Abstract
Objective
The Centers for Education and Research on Therapeutics convened a workshop to examine the scientific evidence on medication adherence interventions from the patient-centered perspective and to explore the potential of patient-centered medication management to improve chronic disease treatment.
Methods
Patients, providers, researchers, and other stakeholders (N=28) identified and prioritized ideas for future research and practice. We analyzed stakeholder voting on priorities and reviewed themes in workshop discussions.
Results
Ten priority areas emerged. Three areas were highly rated by all stakeholder groups: creating tools and systems to facilitate and evaluate patient-centered medication management plans; developing training on patient-centered prescribing for providers; and increasing patients’ knowledge about medication management. However, priorities differed across stakeholder groups. Notably, patients prioritized using peer support to improve medication management while researchers did not.
Conclusion
Engaging multiple stakeholders in setting a patient-centered research agenda and broadening the scope of adherence interventions to include other aspects of medication management resulted in priorities outside the traditional scope of adherence research.
Practice Implications
Workshop participants recognized the potential benefits of patient-centered medication management but also identified many challenges to implementation that require additional research and innovation.
1. Introduction
More than half of American adults take at least one prescription drug, and 1 of 10 take five or more [1]. As the U.S. population ages and as the number of individuals with multiple chronic conditions increases [2], poor adherence to medication regimens to treat chronic disease will pose a public health challenge of increasing significance. Optimal use of medications to manage chronic conditions can improve patient outcomes and decrease the costs of health care; however, suboptimal medication adherence is pervasive and results in poor health outcomes. An estimated $105 – $290 billion is spent annually in avoidable health care costs related to poor adherence to medication regimens [3–7]. Reasons for low adherence include poor prescribing practices, as well as patient concerns about cost, bothersome side effects, burdensome regimens, absence of chronic disease symptoms, doubts about effectiveness of medications, and low health literacy [8]. Prior work has shown that 20 to 30 percent of prescriptions are never filled. Of those that are filled, about half of medications for chronic disease are not taken as prescribed [9].
The findings on medication adherence are especially disappointing given the vast literature on the topic. Adherence research has largely focused on determinants of successful or unsuccessful medication-taking behavior as well as methods to improve patients’ medication taking. Furthermore, previous research has assumed that prescribers’ recommendations constitute instructions that patients are simply expected to follow—hence the somewhat paternalistic terms “compliance” and “adherence” that predominate the literature [10]. However, the relatively modest progress on improving medication adherence, despite decades of research on the topic, has led researchers, clinicians, patients and other stakeholders to seek additional perspectives. New opportunities to improve medication management could arise by placing the individual patient in the center of decisions [11–15]. Such patient-centered care “is respectful of and responsive to individual patient preferences, needs, and values, and ensure[s] that patient values guide all clinical decisions.”[16] In the context of medication use, a patient-centered approach suggests that improving medication use is not entirely about getting patients to simply follow a provider’s plan, to take more medicines, or to take their medicines more often [17;18]. Instead, efforts should focus on delivering care in a way that incorporates patient beliefs, preferences, goals, practical realities, and concerns into decisions and practices that support appropriate medication prescribing and use [19].
A growing literature explores tailoring medications to patient goals, as well as using shared decision-making in the context of medication therapy for chronic disease [20] to engage patients in prescribing decisions. Two recent systematic reviews of interventions to improve adherence to medications prescribed for chronic conditions found mixed results [21–23]. The most successful interventions were multi-modal, high-intensity, and personalized. The finding that personalized interventions are more effective suggests that patient-centered care may offer a way to further improve medication management. Additional research is needed to determine whether patient-centered medication management can improve health outcomes and whether such management can be accomplished in ways that are feasible, cost-effective, scalable and sustainable.
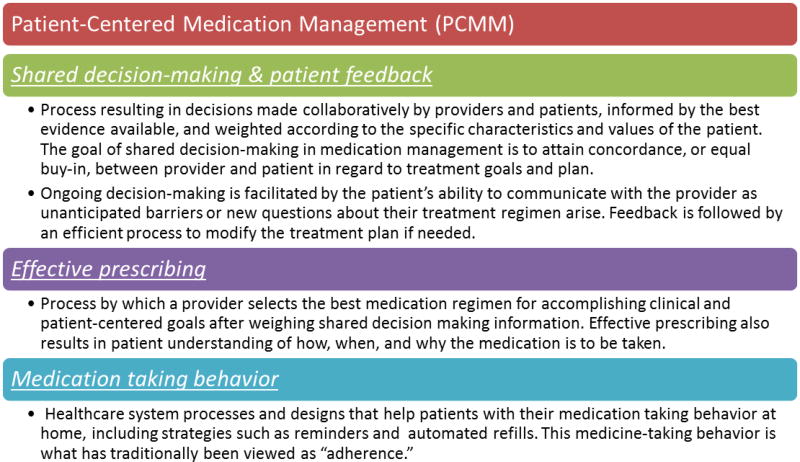
The potential for patient-centered approaches to improve medication outcomes for people with chronic illness prompted a diverse group of therapeutics researchers funded by the Agency for Healthcare Research and Quality (AHRQ)—the Centers for Education and Research on Therapeutics (CERTs)—to convene a two-day workshop in October, 2012 to evaluate how medication adherence interventions could be more patient-centered. An early decision was made to engage other key stakeholders to collaboratively identify and prioritize research and practice needs related to medication adherence. Drawing on the scientific literature (Kuntz et al., manuscript submitted for publication along with this manuscript) and their own expertise in health services research, social science, and analytical methods, conference organizers identified a broad scope of activities for consideration that, in addition to medication-taking behavior (the traditional scope of adherence research), included shared decision-making, methods to enhance effective prescribing, and systems for eliciting and acting upon patient feedback about medication taking and treatment goals (see Figure 1). We refer to this set of activities as patient-centered medication management (PCMM). Next, we convened a workshop at which patients, caregivers, providers, product makers, payers, purchasers of health care, research funders, policymakers, and researchers shared their expertise and perspectives, then collectively identified and prioritized knowledge gaps needing further research and action. This paper reports the key priorities nominated by workshop contributors. We also present themes about PCMM that emerged from qualitative analysis of recordings and transcripts from workshop discussions. Finally, we reflect on our process for engaging diverse stakeholders in shaping patient-centered research.
Figure 1.
2. Methods
2.1. Goal of the workshop
The goal of the workshop was to identify and prioritize opportunities to advance PCMM by convening diverse stakeholders involved in prescribing and/or medication taking.
2.2. Pre-workshop activities
The workshop was planned by a steering group composed of 11 CERTs investigators who have worked on medication adherence from a variety of scientific perspectives (medicine, pharmacy, informatics, epidemiology, and social science) as well as two patient representatives who have personal and advocacy experience with arthritis and juvenile diabetes. The steering group developed definitions of PCMM and its components, and used PCMM to guide a literature review as well as the workshop’s agenda and prioritization process. The steering group also identified potential workshop participants. In alignment with Concannon’s (2012) list of key stakeholders for patient-centered outcomes research, the steering group invited 23 thought leaders representing the following constituencies: patients/patient advocates, caregivers, providers, payers, researchers, funders, product makers, policymakers/consumer advocates, and purchasers of health care. We selected individuals who had been nominated by CERTs researchers from across the United States as experts on patient-centered care and medication management. Fifteen attended the workshop or sent an equally knowledgeable colleague from their organization. In addition, 22 CERTs-affiliated researchers participated in the meeting, including 9 steering group members. Table 1 summarizes self-identified primary stakeholder perspectives (e.g., one workshop attendee identified herself primarily as a researcher, but also as a funder and a patient).
Table 1.
Primary Stakeholder Group Represented by Workshop Participants
| Stakeholder Category | Primary Perspective (n=28*) |
|---|---|
| Patient/Patient Advocate1 | 5 |
| Payer2 | 1 |
| Policy Maker3 | 2 |
| Product Maker4 | 2 |
| Provider5 | 3 |
| Researcher6 | 13 |
| Funder7 | 2 |
Does not include 9 Steering Group members from Center for Health Research, Kaiser Permanente Northwest (8) and Baylor College of Medicine (1)
– Three patients/patient advocates, two caregivers
– Aetna, Inc.
– AARP; National Consumers League
– Surescripts; Merck & Co., Inc.
– Brigham & Women’s Hospital; Duke Cardiology; Group Health Cooperative
– Partners Healthcare; Indiana University School of Medicine; Cincinnati Children’s Hospital Medical Center (2); Department of Veterans Affairs; Duke University School of Medicine; Northwestern University; Rutgers University (2); University of Alabama at Birmingham (2); University of North Carolina at Chapel Hill; University of Illinois at Chicago
– Patient-Centered Outcomes Research Institute; Agency for Healthcare Research and Quality
2.3. Workshop activities
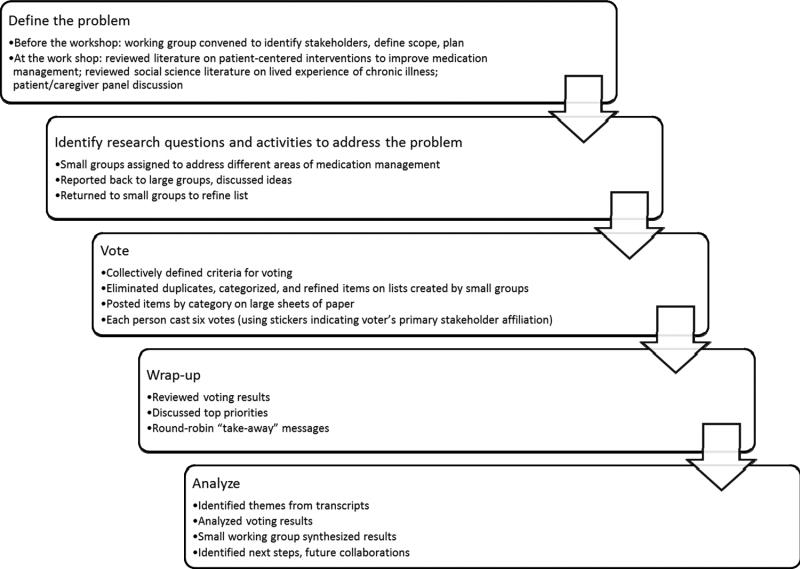
The workshop combined presentations and group discussions on pre-selected topics, followed by a period of voting to establish research and practice priorities (Figure 2). We modeled the workshop on approaches to consensus building, data collection, and analysis described elsewhere [24–26]. On the first day of the workshop, there were three presentations: 1) a review of the current literature on patient-centered interventions to improve medication management (Kuntz et al., manuscript submitted for publication, in parallel); 2) a review of social science research about the lived experience of chronic illness [19;27–29]; and 3) a discussion by a panel of five patients, caregivers, and patient advocates about how to improve medication management. The presentations were followed by small-group discussions with reports back to the entire group. Small groups designed to achieve diverse stakeholder perspectives were assigned one or two of four PCMM areas, matched to participants’ areas of expertise as much as possible: 1) shared decision-making and patient feedback, 2) effective prescribing, and 3) medication-taking behavior. At the end of the day, each group produced a list of research questions or activities in its content area that might advance research and practice related to PCMM.
Figure 2.
The following day, conference organizers reviewed the lists, eliminated duplicate items, refined wording and categorized the lists into broad, cross-cutting domains (i.e., methods and measures, policy, and education). Items in each domain were written on large sheets of paper and were posted around the conference room. Attendees used stickers, with colors indicating their stakeholder perspective, to place a total of 6 votes on the agenda items they prioritized. Nine members of the CERTs coordinating center did not participate in the voting but did participate actively in other aspects of the workshop. Attendees were permitted to vote more than once for a single item to indicate a priority they felt was very important. Day 2 continued with a discussion of the priorities with the most votes overall and differences in stakeholder group priorities. The meeting concluded with each attendee providing his or her “takeaway” messages about the workshop. During the workshop, large-group discussions were tape-recorded, and small-group session recommendations were captured on large sheets of paper.
2.4. Data analysis
2.4.1. Stakeholder voting results
We asked attendees to list their primary perspective as stakeholders, in addition to other perspectives that shaped their contributions to the workshop. For example, someone whose primary contributions reflected the research perspective could acknowledge a secondary perspective as a provider. We tabulated votes according to each voter’s primary stakeholder perspective. We edited the wording of items for clarity and brevity and grouped some very similar items under more general headings. For example, three very specific items relating to the need for more epidemiologic knowledge about long-term medication use were combined under the more general heading of “improve epidemiologic knowledge of long-term medication-taking behavior.”
2.4.2. Theme analysis
We transcribed and analyzed digital recordings. Using a grounded theory approach to theme identification, we created a list of all discussion topics [30]. We reviewed and consolidated the list of topics into more than 100 themes. Each theme was noted as an individual row in a spreadsheet, and the first author led a multidisciplinary team in a virtual card-sort exercise over the course of several webinars. We grouped similar themes and then assigned names to the groups of themes. The sorting process resulted in a three-part taxonomy of considerations for advancing PCMM in research and practice.
3. Results
3.1. Stakeholder voting results
Ten categories of priorities emerged from the workshop. These are listed in Table 2, ranked according to total number of votes for each priority. Table 2 also includes the number of votes for each priority by stakeholder group and a representative selection of items in each category. Table 3 shows the rank order of each priority according to stakeholder group: researchers, patients, and all other stakeholders. We deemed the top four ranked priorities within each group as “high priority.” Accordingly, three priorities were highly rated by all types of stakeholders: 1) creating tools and systems to facilitate and evaluate patient-centered medication management plans; 2) developing patient-centered prescribing curricula for providers (physicians, physician assistants, and nurses); and 3) increasing patient knowledge about medication management to improve health outcomes. Other priorities rated highly were: changing the culture of health care to focus on creating and maintaining health as opposed to treating disease; defining patient-centered goals and measures; and involving peers, family and social networks in PCMM.
Table 2.
Vote Totals for Research Questions and Actions to Advance Patient-Centered Medication Management, by Self-Identified Stakeholder Group (see Table 1). (Each participant had six votes)
| Category and illustrative research questions included within each category: | Total (N=168) n (%) |
Researchers (N=78) n (%) |
Patients (N=30) n (%) |
Others (N=60) n (%) |
|---|---|---|---|---|
Create Tools and Systems to Facilitate and Evaluate Patient-Centered Medication Plans
|
38 (22.6) | 21 (26.9) | 5 (16.7) | 12 (20.0) |
Develop Patient-Centered Prescribing Curricula
|
24 (14.3) | 9 (11.5) | 6 (20.0) | 9 (15.0) |
Increase Patient Knowledge about Medication Management to Improve Health Outcomes
|
22 (13.1) | 10 (12.8) | 6 (20.0) | 6 (10.0) |
Improve Epidemiology of Long-term Medication-taking Behavior
|
20 (11.9) | 12 (15.4) | 3 (10.0) | 5 (8.3) |
Patient-Centered Medication Management Requires Change in the Culture of Health Care
|
17 (10.2) | 8 (10.3) | 3 (10.0) | 6 (10.0) |
Define Patient-Centered Goals and Measures in Research and Practice
|
14 (8.3) | 5 (6.4) | 1 (3.3) | 8 (13.3) |
Involve Peers, Family and Social Networks in the Solution
|
14 (8.3) | 3 (3.9) | 5 (16.7) | 6 (10.0) |
Incorporate Patient Feedback into Medication Management
|
10 (6.0) | 6 (7.7) | 1 (3.3) | 3 (5.0) |
Incorporate the Patient Experience of Medications into Research and Practice
|
4 (2.4) | 3 (3.9) | 0 (0) | 1 (1.7) |
Target Interventions by Prioritizing Populations and Allocating Resources
|
3 (1.8) | 1 (1.3) | 0 (0) | 2 (3.3) |
| Other | 2 (1.2) | 0 (0) | 0 (0) | 2 (3.3) |
Table 3.
Rank Order of Voting by Stakeholder Category (Researchers, Patients, and Other Stakeholders). Shaded cells show top 4 priorities for each group.
| Researchers | Patients | Other Stakeholders* |
|
|---|---|---|---|
| Create Tools and Systems to Facilitate and Evaluate Patient-Centered Medication Plans | 1 | 3 (tie) | 1 |
| Develop Patient-Centered Prescribing Curricula | 4 | 1 (tie) | 2 |
| Increase Patient Knowledge about Medication Management to Improve Health Outcomes | 3 | 1 (tie) | 4 (tie) |
| Improve Epidemiology of Long-term Medication-taking Behavior | 2 | 5 (tie) | 7 |
| Patient-Centered Medication Management Requires Change in the Culture of Health Care | 5 | 5 (tie) | 4 (tie) |
| Define Patient-centered Goals and Measures in Research and Practice | 7 | 7 (tie) | 3 |
| Involve Peers, Family, and Social Networks in the Solution | 8 (tie) | 3 (tie) | 4 (tie) |
| Incorporate Patient Feedback into Medication Management | 6 | 7 (tie) | 8 |
| Incorporate the Patient Experience of Medications into Research and Practice | 8 (tie) | 10 | |
| Target Interventions by Prioritizing Populations and Allocating Resources | 10 | 9 |
Two votes could not be categorized.
We found notable differences among stakeholder groups. As shown in Table 3, researchers’ second-ranked priority—“improve epidemiologic knowledge of long-term medication-taking behavior”—was ranked as relatively unimportant by the other two groups: fifth by patients and seventh by other stakeholders. A group composed mostly of individuals engaged in the business of delivering health care ranked the category “define patient-centered goals and measures” as its third-highest priority. In contrast, patients and researchers ranked this category seventh. Finally, as Table 2 shows, while patients cast 17% of their total votes for efforts to incorporate peers, family, and social networks into medication management efforts, only 4% of researchers cast votes for this category.
3.2. Theme analysis: Workshop discussion topics
Our thematic analysis of transcripts and notes from workshop discussions revealed a wide range of issues to consider in research and implementation of PCMM. We clustered these topics into three overarching themes:
What is patient-centered health care?
Why is PCMM needed? (See Table 4);
How can we develop, evaluate and implement PCMM?
Table 4.
Why Patient-Centered Medication Management is Needed: Themes from Workshop Discussions
| Providing information that makes sense to patients |
|
|
| “Give patients a fighting chance: talk to them; inform them." (Patient advocate) |
|
|
|
|
|
| Enhancing patient/provider communication and building trust |
|
|
| “When providers connect with patients, magic happens. But this happens when the patient stays for a long time and there is time to get to know the patient.” (Patient advocate) |
|
|
|
|
|
| Prescribing to treat a whole person, not a disease |
|
|
| “I could not do any of the things I used to … as a young adult. The symptoms of my disease affected my identity.” (Patient advocate) |
| “I think I take [my medicines] because of my loss of identity. If I take my meds, I look a little less like a patient.” (Patient advocate) |
|
|
|
|
|
| Creating a health care system that is more supportive of patients |
|
|
| “Thousands of dollars’ worth of drugs and procedures that took hundreds of thousands of dollars of medical personnel to administer to me and the whole thing, the entire enterprise, rested on a skinny scared adolescent. … I was just in awe how much responsibility is now “ours” in order to make our care successful.” (Patient advocate) |
|
|
|
|
|
| Understanding the challenges of evidence-based prescribing |
|
|
| “A peer has experience with medication, so you trust that. Much more than you would the provider … who is basing the info on literature and statistics.” (Patient advocate) |
|
|
|
3.2.1. What is patient-centered health care?
Workshop participants, especially patients, emphasized that engaging them in health care (and health care improvement) is a critical component of medication adherence. One patient advocate stated:
“Patient-centeredness means patients have the support to do what we need to do to care for ourselves and use health care as a tool for us to live as well as we can for as long as we can.”
Other patient representatives reported that engagement should involve recognizing patients’ expertise, being sensitive to the diversity of patients’ preferences, and understanding how outcomes that matter to patients can differ from those that matter to clinicians. In terms of prescribing, participants noted that therapeutic goals should be attainable by patients given their specific circumstances, and that a patient-centered health care system should seek out and actively remove barriers to accessing health care and successful medication-taking. Another discussion topic explored the importance of teaching people how to become informed and engaged patients, perhaps even as part of primary or secondary school education.
3.2.2. Why is PCMM needed?
Extensive discussions highlighted several justifications for a broad, patient-centered approach to medication management: 1) to provide information that makes sense to patients; 2) to enhance patient-provider communication and to build trust; 3) to understand the differences between disease-oriented prescribing and person-oriented prescribing; 4) to create a health care system that is more supportive of patients; and 5) to better understand and overcome the challenges of evidence-based prescribing. More details about these reasons for PCMM are noted in Table 4.
3.2.3. How can we develop, evaluate, and implement PCMM?
Participants offered several policy-relevant insights to guide implementation of PCMM. First, there is a need to find opportunities for alignment between the often conflicting goals of standardized and personalized health care; finding a balance can be challenging at both the system and provider-patient level. Patient-centered care requires incorporating individual goals and preferences into care, but implementing such variability may burden providers and health systems. Workshop participants recognized the challenge of generalizing individualized patient care on a broader scale. For example, one provider commented:
“Providers in the fee for service world are even just struggling to identify who’s had a recent ER visit, and why [the patient came in]… So for me, as a provider [questions like] how are you doing on your medication today? Are you doing okay? What information do you need from me? How can I help you? Those are things that are not on the trigger list as far as looking at you medically in a patient centered fashion.”
Innovative solutions, including those that make use of information technology and new forms of communication, are needed. Indeed, interventions at the health system or provider level may be as important as those that focus on patients or provider-patient communication. As one participant noted,
“Not everything we discussed as being patient-centered is directly aimed at the patient.” (Researcher)
Participants also emphasized the need to recognize heterogeneity in health care contexts, such as differences between fee-for-service and integrated health systems. Integrated systems that combine medical care, health education, case management, and pharmacy services potentially offer easier entry points to advancing PCMM, but for PCMM to have real impact we will need to test interventions in fee-for-service, mail-order pharmacy, retail pharmacy, and other contexts.
4. Discussion and Conclusion
4.1. Discussion
In an effort to rethink medication taking in the context of chronic disease from a patient-centered perspective, we considered processes outside of the traditional purview of medication adherence, including shared decision-making and incorporation of patient feedback in therapeutic plans, and effective prescribing. Multiple stakeholders gathered to create a research agenda and call for action to advance PCMM.
Priorities that received strong overall endorsements from all stakeholders were: create tools and systems to facilitate and evaluate PCMM plans; develop patient-centered prescribing curricula; and increase patient knowledge about medication management. A majority of the workshop participants deemed the latter two critically important. The suggestion to incorporate patient-centered training into providers’ training and continuing education in order to enable them to be patient-centered prescribers is consistent with the American Association of Medical Colleges’ 2008 recommendation that improvements are necessary to train physicians in safe and effective prescribing practices [31;32]. Consensus on some priorities may be difficult to achieve, as reflected in the differences in prioritization across stakeholder groups. Among stakeholders who were not patients or researchers, the perceived need for tools to identify and measure patient-centered goals may reflect the challenges of implementing customized processes in large-scale health care operations, which are less salient for researchers and patients. Also, while patients and “other” stakeholders prioritized using social networks to advance PCMM, researchers did not rate this area as high priority. This suggests that the promise of interventions that use social networks and peer support represent is being overlooked by researchers. Finally, researchers’ second-rated priority, improving epidemiologic knowledge of long-term medication taking behavior, was not highly ranked by other stakeholder groups (Table 3) and may reflect the dominance of quantitative pharmacoepidemiologists among the workshop participants.
The fact that a top priority of researchers was not highly ranked by others illustrates that an agenda that results from engaging multiple stakeholders—and not only patient stakeholders—is likely to differ substantially from an agenda set solely by researchers. The results of this workshop demonstrate a concrete, feasible process for actively engaging patients and non-researcher stakeholders to ensure integration of their needs into research.
Thematic analysis of workshop discussions highlighted: 1) what patient-centered health care is, 2) why PCMM is needed, and 3) how to develop, evaluate, and implement PCMM. Each of these issues is relevant for current policy debates, and workshop discussions emphasized the centrality of medication management for improving health care quality.
Including patients in the pre-workshop planning substantively informed the workshop and also the development of the innovative, expanded PCMM framework that extends beyond patients’ medication-taking behavior. Including patients in the planning and conceptualization of priority-setting activities should be replicated in future similar efforts.
Participants made several observations about the workshop process that are worth noting. They recognized the complexity of medication management and the benefits of engaging multiple stakeholders to improve it. Participants were energized by the productive debate and insights they gained because many types of stakeholders were present, and they recognized the strength of the multiple-stakeholder approach. Despite their disciplinary and experiential differences, workshop participants were open to new ways of conceptualizing medication adherence and were able to communicate well in workshop discussions. Participants also affirmed efforts such as those initiated by the Patient-Centered Outcomes Research Institute (PCORI; www.pcori.org) and AHRQ’s Effective Healthcare Program (www.effectivehealthcare.ahrq.gov) that are changing the process of determining health policy, quality improvement efforts, and research priorities by including the voices of patients and other stakeholders. Our experience showed that a diverse-stakeholder workshop is both feasible and important. The workshop composition and process could be considered as a model for similar health-related priority setting efforts.
Participants also noted several significant challenges with the workshop process and its results. First, a solid conceptual framework for PCMM is lacking. The proceedings revealed that the framework developed in preparation for the workshop was less than optimal, in part because the boundaries between PCMM activities and their inter-relationships were unclear. For example, the framework did not specify the boundary between shared decision-making and effective prescribing, or show the flow of activities from one PCMM component to the next. Second, multiple stakeholder engagement is resource-intensive. Providers, patients, advocates, and community leaders have limited time, energy, and financial resources to dedicate to agenda-setting activities. Third, patients’ expertise needs to be recognized in discussions and processes that have traditionally been limited to clinical and scientific experts. Neglecting the value of patient experiences and expertise in all phases of research can result in failure to identify and advance patient-centered research. Fourth, progress can be slow. Participants in our workshop reflected on the high energy generated by a presentation that questioned the validity of medication adherence as a concept and shared social science approaches to medication taking and their direct relevance to patient experience. But they also observed that when it was time to generate research questions, participants retreated to more familiar territory. At the end of the conference, many participants were somewhat disappointed by the “mainstream” research questions that were generated in the prioritization exercise. This was a very important outcome of the workshop — the recognition of how challenging it will be to move away from familiar and comfortable paradigms toward new ways of conceptualizing, researching and delivering health care.
4.1.1. Limitations
The workshop outcomes suggest areas for future research and action, but they represent only a first step in reframing medication adherence so that it is patient-centered. The workshop attendees raised many questions and suggested activities that were not fully formulated. Further work will be required to delineate, generate consensus and add specificity to the issues raised and to take appropriate next steps. The guiding framework we developed to describe PCMM will also need refinement.
It should be noted that, while we aimed to represent the viewpoints of diverse stakeholders in our work, we found it difficult to find payers who were available to attend the workshop, and some representatives of funding agencies were precluded from participating due to government travel restrictions. In addition to patients or patient advocates, we also would have benefited from including additional consumer advocates, who aim to ensure a fair health-care marketplace, transparency of information, product safety and other consumer protections, rather than having direct experience with a disease or condition, per se. Both patient advocate and consumer advocate perspectives are valuable and needed, and probably should be distinguished rather than collapsed into one category. Methodologically, the workshop’s process was less formal than a traditional Delphi approach to drawing consensus, which could have generated different results. A different set of stakeholders could have also reached different conclusions. Further efforts to elicit perspectives from these constituencies would be warranted.
4.2. Policy Implications
Our results have implications for policy efforts to address a significant public health problem: poor medication adherence in the context of chronic disease treatment. There are currently a number of policy initiatives aimed at improving adherence. These include: Medicare star ratings, patient-centered medical homes, meaningful use of health information technology (HIT), medication therapy management, and risk-sharing incentives by accountable care organizations (ACOs). None of these initiatives, with the exception of the patient-centered medical home, puts patient-centered care at the core.
There are a number of adherence-oriented coalitions, campaigns, and research groups—NIH Adherence Research Network [33], the National Consumers League Script Your Future campaign [34], the Medication Adherence Alliance [35], the National Council on Patient Information and Education (NCPIE) [36], nonprofits such as NEHI [37], the Office of the Surgeon General [38], and Prescriptions for a Healthy America [39]. Only some of these groups were represented at the workshop (National Consumers League, Medication Adherence Alliance). To follow up on the workshop recommendations, the CERTs sponsored a meeting in Rockville, MD, in March 2014. More than 60 diverse stakeholders (including most of the national medication adherence initiatives listed above, as well as patients and researchers) attended the two-day meeting to discuss patient-centered approaches to appropriate medication use. Specific topics ranged from the role of health information technology to health literacy. The goals of the meeting were to: foster a patient-centered perspective on medication use; share perspectives on needed innovations in terms of policy, intervention, and research, as well as available resources; identify key priorities for action; and determine interest in continued collaboration. A number of these initiatives incorporate patient perspectives in their efforts, and our process and findings suggest promising areas of continued policy and advocacy work.
4.3. Conclusion
The priorities and considerations identified in our multi-stakeholder workshop, as well as the process we used for engaging multiple stakeholders’ perspectives, suggest a roadmap for multiple stakeholders to engage, educate, and support patients in addressing chronic disease management.
Acknowledgments
Acknowledgments/Financial Support
This project was supported by grant number U19HS021107 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. We extend special acknowledgments to the late Jessie Gruman, who, as president and founder of the Center for Advancing Health provided a strong, articulate voice at the workshop. Her contributions as a patient representative brought focus and urgency to the issue of patient-centered medication management; she will be missed.
References
- 1.Gu Q, Dillon CF, Burt VL. Prescription drug use continues to increase: U.S. prescription drug data for 2007–2008. NCHS Data Brief. 2010;42:1–8. [PubMed] [Google Scholar]
- 2.Wu S, Green A. Projection of Chronic Illness Prevalence and Cost Inflation. Santa Monica, CA: RAND Health; 2000. [Google Scholar]
- 3.New England Healthcare Institute. Thinking Outside the Pillbox. Retrieved from: http://www.nehi.net/publications/44/thinking_outside_the_pillbox_a_systemwide_approach_to_improving_patient_medication_adherence_for_chronic_disease.
- 4.IMS Institute for Healthcare Informatics. An updated reference/report from IMS Instutive for Healthcare Informatics called Avoidable Costs in U.S. Healthcare: The $200 Billion Opportunity from Using Medicines More Responsibly estimated $105 billion in annual avoidable healthcare costs do to medication nonadherence. Retrieved from: http://www.imshealth.com/deployedfiles/imshealth/Global/Content/Corporate/IMS%20Institute/RUOM-2013/IHII_Responsible_Use_Medicines_2013.pdf.
- 5.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–30. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 6.Roebuck MC, Liberman JN, Gemmill-Toyama M, Brennan TA. Medication adherence leads to lower health care use and costs despite increased drug spending. Health Aff. 2011;30:91–9. doi: 10.1377/hlthaff.2009.1087. [DOI] [PubMed] [Google Scholar]
- 7.DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40:794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Briesacher BA, Gurwitz JH, Soumerai SB. Patients at-risk for cost-related medication nonadherence: a review of the literature. J Gen Intern Med. 2007;22:864–71. doi: 10.1007/s11606-007-0180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peterson AM, Takiya L, Finley R. Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm. 2003;60:657–65. doi: 10.1093/ajhp/60.7.657. [DOI] [PubMed] [Google Scholar]
- 10.Trostle JA. Medical compliance as an ideology. Soc Sci Med. 1988;27:1299–308. doi: 10.1016/0277-9536(88)90194-3. [DOI] [PubMed] [Google Scholar]
- 11.Dwamena F, Holmes-Rovner M, Gaulden CM, Jorgenson S, Sadigh G, Sikorskii A, Lewin S, Smith RC, Coffey J, Olomu A. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev. 2012;12 doi: 10.1002/14651858.CD003267.pub2. CD003267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peikes D, Zutshi A, Genevro JL, Parchman ML, Meyers DS. Early evaluations of the medical home: building on a promising start. Am J Manag Care. 2012;18:105–16. [PubMed] [Google Scholar]
- 13.Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR. Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetologia. 2012;55:1577–96. doi: 10.1007/s00125-012-2534-0. [DOI] [PubMed] [Google Scholar]
- 14.Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2013;70:351–79. doi: 10.1177/1077558712465774. [DOI] [PubMed] [Google Scholar]
- 15.Berwick DM. What 'patient-centered' should mean: confessions of an extremist. Health Aff. 2009;28:w555–65. doi: 10.1377/hlthaff.28.4.w555. [DOI] [PubMed] [Google Scholar]
- 16.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. The National Academies Press; 2001. [PubMed] [Google Scholar]
- 17.Schiff GD, Galanter WL, Duhig J, Lodolce AE, Koronkowski MJ, Lambert BL. Principles of conservative prescribing. Arch Intern Med. 2011;171:1433–40. doi: 10.1001/archinternmed.2011.256. [DOI] [PubMed] [Google Scholar]
- 18.Heisler M, Hogan MM, Hofer TP, Schmittdiel JA, Pladevall M, Kerr EA. When more is not better: treatment intensification among hypertensive patients with poor medication adherence. Circulation. 2008;117:2884–92. doi: 10.1161/CIRCULATIONAHA.107.724104. [DOI] [PubMed] [Google Scholar]
- 19.Lambert BL, Levy NA, Winer J. Keeping the Balance and Monitoring the Self-System Towards a More Comprehensive Model of Medication Management in Psychiatry. In: Brashers DE, Goldsmith DJ, editors. Communicating to Manage Health and Illness. Routledge/Taylor and Francis Group; 2009. pp. 179–211. [Google Scholar]
- 20.Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. N Engl J Med. 2012;366:780–1. doi: 10.1056/NEJMp1109283. [DOI] [PubMed] [Google Scholar]
- 21.Viswanathan M, Golin C, Jones C, Ashlok M, Blalock S, Wines R, Coker-Schwimmer E, Grodensky C, Rosen D, Sista P, Lohr K. Medication Adherence Interventions: Comparative Effectiveness. Closing the Quality Gap: Revisiting the State of the Science. Evidence Report No. 208. (Prepared by RTI International-University of North Carolina Evidence-based Practice Center under Contract No. 290-2007-10056-I.) AHRQ Publication No. 12-E010-EF September 2012. Retrieved from: http://www.ncbi.nlm.nih.gov/books/NBK114350/pdf/TOC.pdf. [PMC free article] [PubMed]
- 22.Viswanathan M, Golin CE, Jones CD, Ashok M, Blalock SJ, Wines RC, Coker-Schwimmer EJ, Rosen DL, Sista P, Lohr KN. Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann Intern Med. 2012;157:785–95. doi: 10.7326/0003-4819-157-11-201212040-00538. [DOI] [PubMed] [Google Scholar]
- 23.Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008 doi: 10.1002/14651858.CD000011.pub3. CD000011. [DOI] [PubMed] [Google Scholar]
- 24.Yasnoff WA, Overhage JM, Humphreys BL, LaVenture M. A national agenda for public health informatics: summarized recommendations from the 2001 AMIA Spring Congress. J Am Med Inform Assoc. 2001;8:535–45. doi: 10.1136/jamia.2001.0080535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. J Amer Med Assoc. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 26.Ash JS, Stavri PZ, Kuperman GJ. A consensus statement on considerations for a successful CPOE implementation. J Am Med Inform Assoc. 2003;10:229–34. doi: 10.1197/jamia.M1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lambert BL, Street RL, Cegala DJ, Smith DH, Kurtz S, Schofield T. Provider-Patient Communication, Patient-Centered Care, and the Mangle of Practice. Health Communication. 1997;9:27–43. [Google Scholar]
- 28.Viswanathan H, Lambert BL. An inquiry into medication meanings, illness, medication use, and the transformative potential of chronic illness among African Americans with hypertension. Res Social Adm Pharm. 2005;1:21–39. doi: 10.1016/j.sapharm.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 29.Corbin JM, Strauss A. Unending work and care: Managing chronic illness at home. Jossey-Bass; 1988. [Google Scholar]
- 30.Ryan GW, Bernard HR. Techniques to Identify Themes. Field Methods. 2003;15:85–109. [Google Scholar]
- 31.Bernabeo E, Holmboe ES. Patients, providers, and systems need to acquire a specific set of competencies to achieve truly patient-centered care. Health Aff. 2013;32:250–8. doi: 10.1377/hlthaff.2012.1120. [DOI] [PubMed] [Google Scholar]
- 32.Association of American Medical Colleges. Medical School Objectives Project. Report X: Contemporary Issues in Medicine : Education in Safe and Effective Prescribing Practices. Association of American Medical Colleges; 2008. [Google Scholar]
- 33.Office of Behavioral and Social Sciences Research. Adherence Research Network. Retrieved from: http://obssr.od.nih.gov/scientific_areas/health_behaviour/adherence/adherenceresearchnetwork.aspx.
- 34.National Consumers League. Script Your Future. Retrieved from: http://www.scriptyourfuture.org.
- 35.Bosworth HB, Granger BB, Mendys P, Brindis R, Burkholder R, Czajkowski SM, Daniel JG, Ekman I, Ho M, Johnson M, Kimmel SE, Liu LZ, Musaus J, Shrank WH, Whalley BE, Weiss K, Granger CB. Medication adherence: a call for action. Am Heart J. 2011;162:412–24. doi: 10.1016/j.ahj.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.National Council on Patient Information and Education. Educate before you medicate. Retrieved from: http://www.talkaboutrx.org/
- 37.NEHI (Network for Excellence in Health Innovation) How Can We Fix Health and Health Care in the US? Retrieved from: http://www.nehi.net/
- 38.U.S. Department of Health & Human Services. SurgeonGeneral.gov. Retrieved from: http://www.surgeongeneral.gov/
- 39.National Council on Patient Information and Education. Prescriptions for a Healthy America. Retrieved from: http://www.talkaboutrx.org/