Abstract
Objective:
To examine rehabilitation therapy utilization for Parkinson disease (PD).
Methods:
We identified 174,643 Medicare beneficiaries with a diagnosis of PD in 2007 and followed them through 2009. The main outcome measures were annual receipt of physical therapy (PT), occupational therapy (OT), or speech therapy (ST).
Results:
Outpatient rehabilitation fee-for-service use was low. In 2007, only 14.2% of individuals with PD had claims for PT or OT, and 14.6% for ST. Asian Americans were the highest users of PT/OT (18.4%) and ST (18.4%), followed by Caucasians (PT/OT 14.4%, ST 14.8%). African Americans had the lowest utilization (PT/OT 7.8%, ST 8.2%). Using logistic regression models that accounted for repeated measures, we found that African American patients (adjusted odds ratio [AOR] 0.63 for PT/OT, AOR 0.63 for ST) and Hispanic patients (AOR 0.97 for PT/OT, AOR 0.91 for ST) were less likely to have received therapies compared to Caucasian patients. Patients with PD with at least one neurologist visit per year were 43% more likely to have a claim for PT evaluation as compared to patients without neurologist care (AOR 1.43, 1.30–1.48), and this relationship was similar for OT evaluation, PT/OT treatment, and ST. Geographically, Western states had the greatest use of rehabilitation therapies, but provider supply did not correlate with utilization.
Conclusions:
This claims-based analysis suggests that rehabilitation therapy utilization among older patients with PD in the United States is lower than reported for countries with comparable health care infrastructure. Neurologist care is associated with rehabilitation therapy use; provider supply is not.
Evidence for the efficacy of rehabilitation therapies in the treatment and management of Parkinson disease (PD) has been expanding, demonstrating improvements in function, activities of daily living, speech volume, and quality of life.1–11 As a result, current American Academy of Neurology (AAN) quality measures for PD treatment advocate for the regular assessment of the need for physical therapy (PT), occupational therapy (OT), and speech therapy (ST).12 Similar guidelines exist globally, motivating research on the utilization of rehabilitation therapies in PD in other countries (e.g., Germany, United Kingdom, the Netherlands). In addition, Medicare policy was changed in 2014 to support continued therapy to prevent or slow further deterioration in neurodegenerative disease so that coverage could not be denied solely for the lack of improvement due to disease progression.
Despite these guidelines and evidence of efficacy, no study to date has examined utilization of these therapies for PD across the United States. To address this gap in knowledge, we studied health care encounter data of 174,643 individuals with Medicare, a government insurance program used by 98% of Americans over the age of 65 years, to achieve the following goals: (1) describe the utilization of PT, OT, and ST for PD in the United States; (2) compare the use of rehabilitation therapies in the United States to that of other developed countries; (3) determine patient and provider factors associated with rehabilitation therapy use; and (4) establish baseline utilization rates, against which the effects of development of quality metrics of care and Medicare coverage policy changes can be measured.
METHODS
Standard protocol approvals, registrations, and patient consents.
This study was approved by the Institutional Review Board at the Perelman School of Medicine, University of Pennsylvania.
Data source.
This study utilized research identifiable files from the Centers for Medicare and Medicaid services (CMS); specifically, (1) Carrier (formerly Part B) files, which contain diagnosis, treatment, and procedure claims from the inpatient and outpatient settings and provider characteristic data (e.g., specialty), and (2) Beneficiary Annual Summary Files, which contain demographic information and comorbid condition (identified by CMS using ICD-9-based algorithms). From these files, a cohort of Medicare beneficiaries with prevalent PD was created and used to identify rehabilitation therapy usage and to examine the associations between patient, clinical, and provider characteristics and receipt of rehabilitation therapies.
Study population.
The study population consisted of adults eligible to receive Medicare by virtue of being age 65 or older who received care for PD in 2007 and were still living on December 31, 2009. Our case identification methods are published elsewhere,13 but briefly, the Carrier (formerly Part B) files were searched to identify beneficiaries with claims containing ICD-9 codes for Parkinson disease (332) or paralysis agitans (332.0). Individuals who also had diagnostic claims for secondary/drug-induced parkinsonism (332.1) or other degenerative diseases of the basal ganglia/atypical Parkinson syndromes (333.0) were excluded because these diseases have a distinct pathophysiology and clinical course, and do not have clinical trial or guideline support for physical therapy. We also excluded individuals who had fewer than 12 months of Medicare data or simultaneous Medicaid or health maintenance organization insurance, because these individuals may not have 100% of their claims submitted to Medicare in a given year. In addition, we extracted individual race (categorized using CMS race codes Caucasian, African American, Hispanic, Asian, Native American, other), sex, age, and state of residence (according to CMS billing information).
Rehabilitation therapies utilization.
Our primary analysis limited our cohort to individuals who received care for PD in 2007, and examined the use of rehabilitation therapies over a 3-year period (2007–2009). We identified all Medicare Carrier billing claims for PT, OT, and ST from January 1, 2007, to December 31, 2009, in our PD cohort using Current Procedural Terminology (CPT) codes. Indicator variables for PT and OT evaluation were generated using distinct evaluation CPT codes. Treatment codes for PT and OT overlap, and were represented by an indicator variable for PT/OT management. ST evaluation and treatment was coded as a single indicator variable.
Care intensity and specialty.
To examine the association between increasing physician visit frequency and physician specialty on the use of rehabilitation therapies, we identified all outpatient office visits per year and extracted physician specialty for each visit. A categorical variable for neurologist visits was generated as follows: none (0 visits), infrequent (1 visit), intermediate (2–3 visits), frequent (4 or more neurologist visits in 1 year). Annual neurologist care was assigned “yes” if there was at least 1 neurologist visit per year.
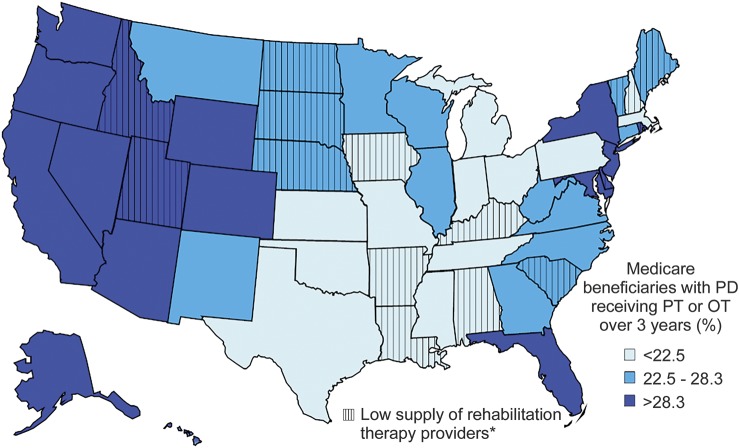
Geographic variation in rehabilitative care.
We examined geographic differences in rehabilitation treatment use and whether these related to therapy availability. The prevalence of rehabilitation services utilization over the 3-year study period was calculated at the state level (number of Medicare patients with PD with a qualifying rehabilitation therapy claim/total number of Medicare beneficiaries treated for PD). Next, we calculated the number of physical, occupational, and speech therapists per 1,000 Medicare beneficiaries in each state using occupational employment statistics data from the US Department of Labor.14 Rehabilitation therapy utilization and the concentration of each type of therapist were categorized into tertiles, with each state categorized as low, medium, or high with regard to rehabilitation therapies use and provider supply. The results were mapped to display regions of the country based on these categories.
Statistical analysis.
Statistical analysis was performed with SAS software (SAS Institute, Cary, NC). All statistical tests were 2-sided. Statistical significance was set at p < 0.05 and normality assumptions were checked where appropriate. Logistic regression models were used to examine the odds of rehabilitation therapy use in PD. The primary outcome was receipt of PT, OT, or ST and covariates included race, age, sex, number of all physician office visits, and number of neurologist visits. Logistic regression models were also used to determine the effects of physician specialty and visit frequency on rehabilitation therapy utilization, controlling for race, age, sex, and number of physician office visits. All logistic regression models accounted for the repeated nature of our longitudinal study design. Spearman correlation coefficient was used to examine the relationship between rehabilitation therapy utilization rates and provider supply, calculated as the number of state-registered PT/OT/ST providers per 1,000 Medicare beneficiaries.
RESULTS
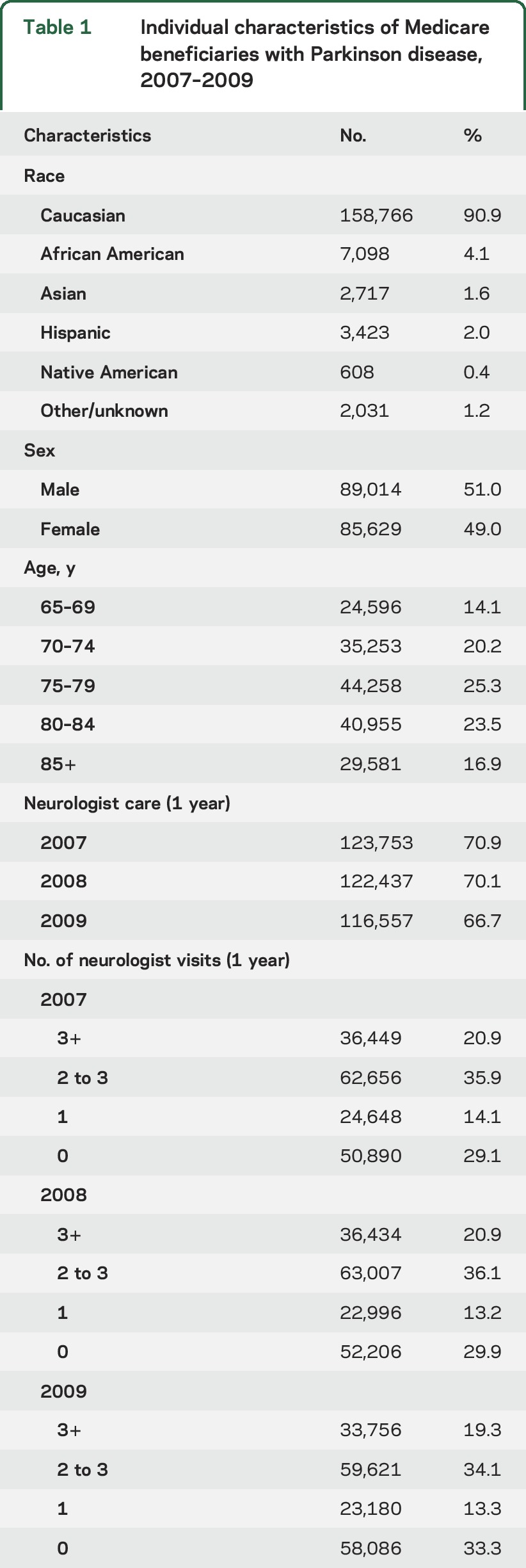
A total of 174,643 unique Medicare beneficiaries were identified who met the inclusion and exclusion criteria (table 1). Over 90% of the patients with PD were Caucasian and two-thirds were ages 75 and older. Sixty-seven percent of patients with PD received neurologist care at least once per year in the 3-year period, the frequency of which is consistent with AAN guidelines and meets the frequency of care we have previously demonstrated is associated with reduced hospitalizations, PD-related illness, and hip fracture.15
Table 1.
Individual characteristics of Medicare beneficiaries with Parkinson disease, 2007–2009
Rehabilitation therapy utilization.
In the first year of the study, 9.9% (n = 17,233) of Medicare beneficiaries diagnosed with PD had claims for PT evaluation, 1.3% (n = 2,342) had claims for OT evaluation (table e-1 at Neurology.org), and 14.2% (n = 24,796) had billing codes that may reflect treatment modalities used by either OT or PT, hereafter reported as a combined PT/OT rate (table 2). ST was utilized by 14.6% (n = 25,494) of the cohort in the first year. Rates for all rehabilitative therapy modalities showed a small decline from 2007 to 2009.
Table 2.
Rehabilitation therapy utilization among Medicare beneficiaries with Parkinson disease, 2007–2009
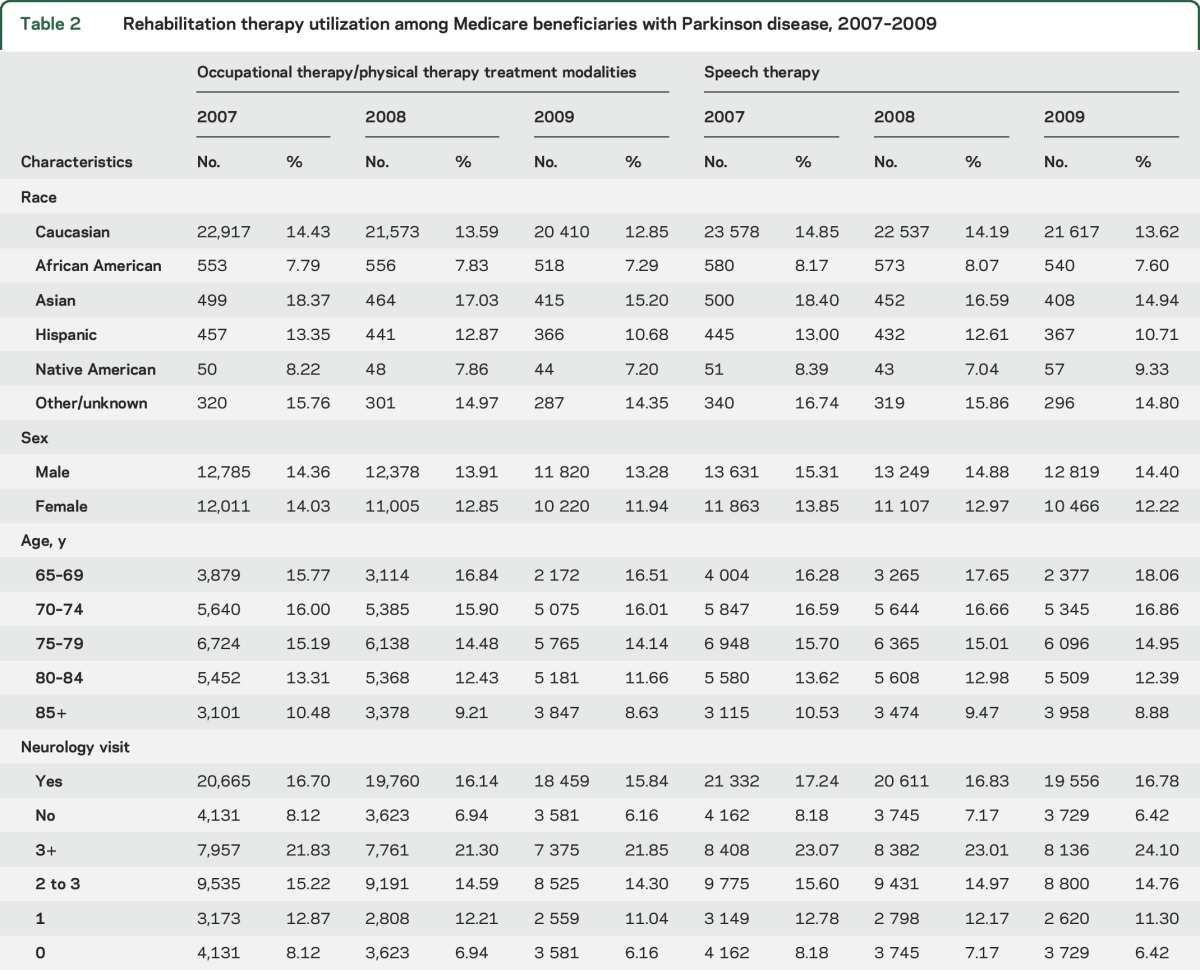
PT/OT and ST treatment for PD varied by demographic characteristics. As shown in table 2, Asian patients with PD were the highest users of PT/OT (18.4%) and ST (18.4%), followed by Caucasian patients with PD (PT/OT, 14.4%; ST, 14.9%). PT/OT and ST were least often utilized by African American patients with PD (PT/OT, 7.8%; ST, 8.2%) and Native American patients with PD (PT/OT, 8.2%; ST, 8.4%). PT/OT use was similar between men and women, but men had higher utilization rates for ST than women (table 2).
Logistic regression models that included race, age, and sex, while also adjusting for the number of physician office visits and neurologist care, demonstrated an association between race and receipt of PT/OT or ST (table 3). Compared to Caucasian patients, African American patients had lower odds of any PT/OT (AOR 0.63, 0.59–0.67) or ST (AOR 0.63, 0.59–0.67). Hispanic patients similarly were less likely to have ST services (AOR 0.91, 0.85–0.98). Asian American patients with PD were 31% more likely to receive PT/OT (AOR 1.31, 1.21–1.41).
Table 3.
Odds of rehabilitation therapy use according to characteristics of patients with Parkinson disease
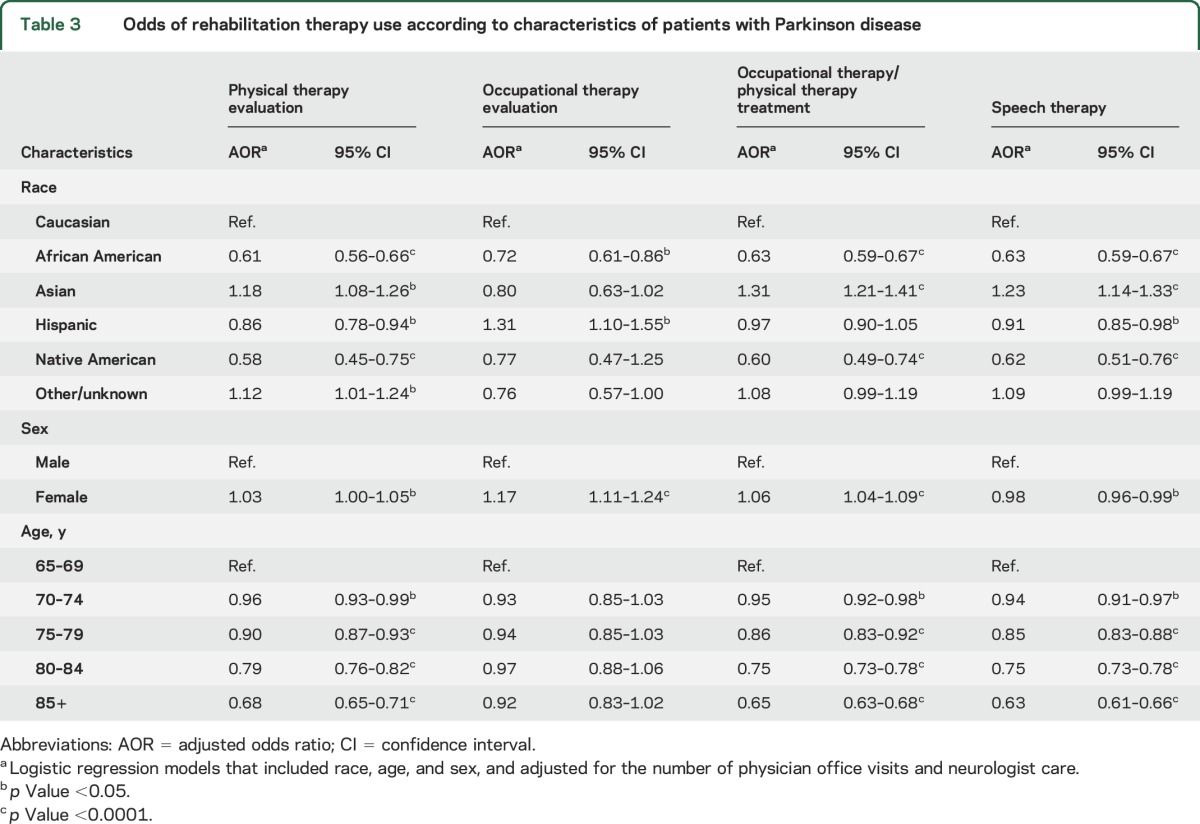
Neurologist care and rehabilitation therapies utilization.
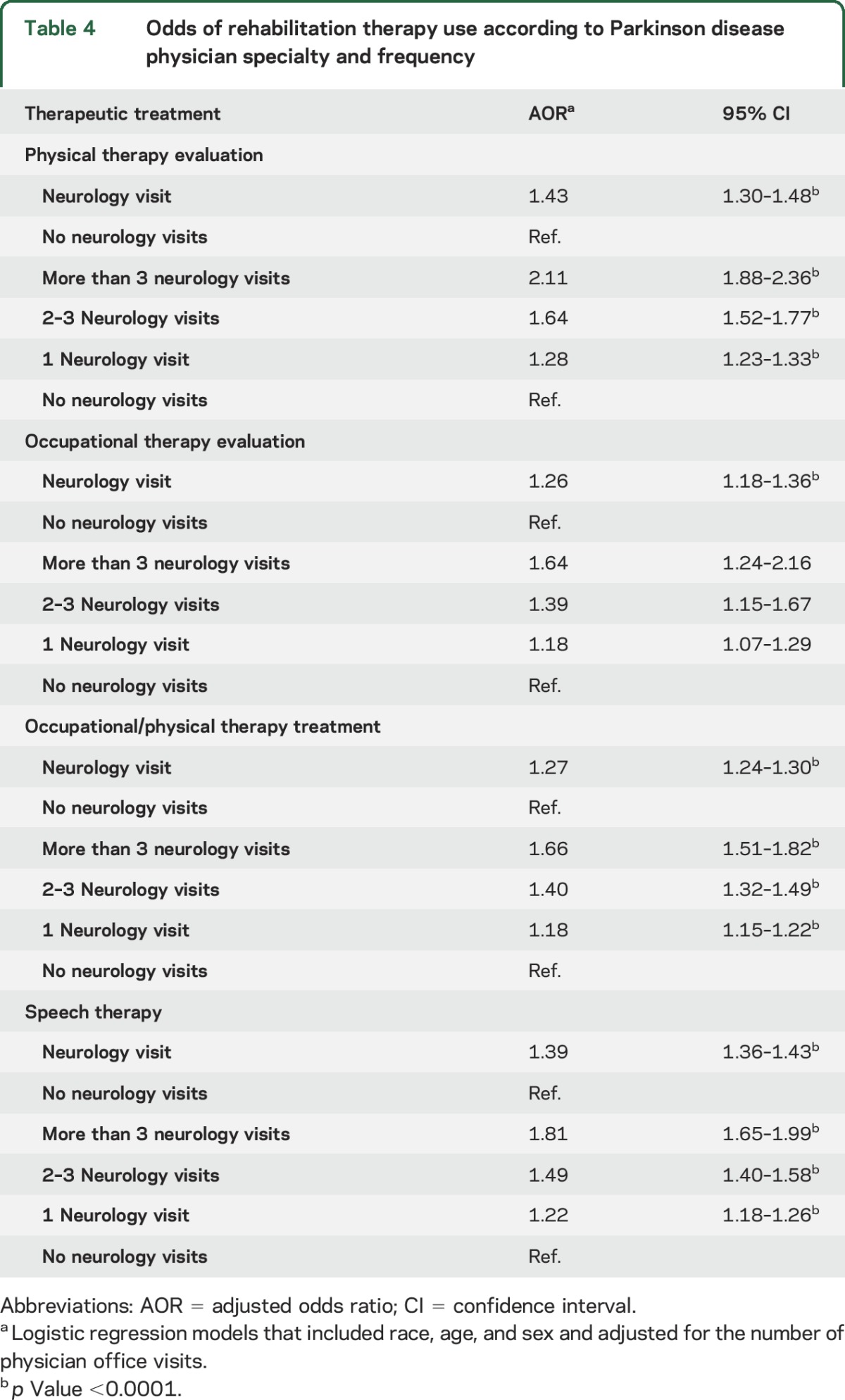
Patients with PD with at least 1 neurologist visit were 43% more likely to receive an evaluation for PT compared to those without neurologist care (AOR 1.43, 1.30–1.48). This relationship was similar for ST, OT evaluation, and PT/OT treatment (table 4). There were incremental increases in the odds of all outcomes with increasing levels of neurologist participation in PD care, even after adjusting for patient race, sex, age and the number of physician office visits. For patients with more than 3 neurology visits per year, the odds of PT evaluation were the highest (AOR 2.11, 1.88–2.36), followed by ST evaluation (AOR 1.81, 1.65–1.99), OT evaluation (AOR 1.64, 1.24–2.16), and PT/OT (AOR 1.27, 1.24–1.30).
Table 4.
Odds of rehabilitation therapy use according to Parkinson disease physician specialty and frequency
State-level differences in utilization.
There were geographic differences in rehabilitation therapy use, although no state had greater than 40% therapy utilization for PD over the 3-year study period. Only Idaho, Utah, Delaware, New Jersey, California, New York, Arizona, and Wyoming had utilization rates ≥35% (figure). There were no significant correlations between provider supply and evaluation for PT (correlation coefficient −0.045, p = 0.75), OT (correlation coefficient 0.175, p = 0.23), or ST (correlation coefficient −0.017, p = 0.91).
Figure. Receipt of rehabilitation therapies by state.
The prevalence of physical therapy (PT) and occupational therapy (OT) utilization over 3 years is shown by state. *Low supply of rehabilitation therapy providers indicates the state was in the lowest tertile for provider supply. PD = Parkinson disease.
DISCUSSION
In this study, we present the first national data on the utilization of outpatient rehabilitation services for patients with PD in the United States. Using data from 174,643 older adults, we found that 75% of Medicare beneficiaries diagnosed with PD did not receive rehabilitative therapies over a 36-month period. While it is not clear what the appropriate utilization rate should be, utilization among patients with PD in the Netherlands and the United Kingdom greatly exceeds what we found in the United States: at least 57% and 54%, respectively.16,17 In this study, predictors of higher (but still low) rates of therapy utilization included PD care by a neurologist, Asian or Caucasian race, and geographic location.
Over the last few decades, a substantial amount of public (NIH) and private funds have been invested in the study of rehabilitation therapies in PD. Physical therapy has been well-studied in randomized controlled trials, and efficacy in PD has been documented by systemic reviews and meta-analyses.1,4,6,10 Furthermore, exercise has been shown to improve both motor and nonmotor symptoms in patients with PD.4,6,8,11 PT can serve as a means to be physically active, but with supervision, alleviating perceived or actual injury risks that could come with nonsupervised exercise in patients with PD. While PT makes up a large portion of rehabilitation therapies use in patients with PD, studies on the efficacy of OT and ST in the treatment and management of PD have also been done, showing improvements in quality of life, dysarthria, and hypophonia.2,3,7,9 Up to 89% of patients with PD have speech disorders, yet in this study, only 14.6% received ST consultation or treatment.18 Likewise, falls are a common indication for PT referral, and occur in up to 68% of patients with PD,19 but only 14.2% of our cohort received PT/OT. Our data highlight the US gap between PD research and implementation, and may provide an evidence base for investment in dissemination and implementation research for PD in the United States.
Possible explanations as to why rehabilitation therapies, particularly PT, are so underutilized among patients with PD in the United States are wide-ranging. One possibility may be related to uncertainty over the clinical significance of published outcomes. A Cochrane review found no particular form of physical therapy to be superior, and although many categories of motor function did improve for patients with PD using PT, improvements in most categories were small.10 Both clinicians and patients may see these small gains as difficult to justify, given the time, cost, and travel required for PT sessions. Physicians may instead be recommending independent, home-based exercise programs for PD and patients may be seeking out other exercise modalities including dance, tai chi, and boxing that are not currently covered by Medicare.20 Finally, previous Medicare policy required that individuals demonstrate a treatment response in order to continue PT beyond the annual dollar-amount payment cap at the time these data were gathered. This policy resulted in the denial of regular PT or OT for individuals with chronic neurologic diseases in the absence of functional improvements. In 2014, this policy was changed to support continued PT with the goal to maintain current functional status or prevent decline in function as long as additional documentation is provided. This may remove some of the barrier for physical therapy utilization in patients with PD in the United States, and future studies will be needed to determine the extent to which this policy change affects utilization rates.
Primary care practitioners are the primary managers for 50% of people diagnosed with PD in the United States and may not read subspecialty journals or guidelines for PD,15 possibly reducing the likelihood of referral for rehabilitation therapies. This is supported by our finding that patients with PD with at least 1 neurologist visit were more likely to receive a PT evaluation compared to those without neurologist care. Similar results were found for OT and ST evaluation and incremental increases in neurologist care improved the odds of receiving therapies. Neurologists also tend to see patients with more severe disease, which may explain the increase in utilization. Despite the higher disease severity, neurologist-treated patients with PD have been shown to have better outcomes.15,21
Several PD organizations have a mission focus on patient care.22–25 These organizations identify and support clinics and academic centers that have specialty trained PD providers. However, the 50% of patients with diagnosed PD who do not see a neurologist early in disease (most often women, minorities, and rural-dwelling patients) would have little benefit.15 Geography-based approaches, such as ParkinsonNet, may be worth considering. The ParkinsonNet care model was devised and first implemented in the Netherlands and aimed to improve access to comprehensive care for patients with PD, including access to rehabilitation therapists with PD-specific expertise.26
Limitations of this study consist of those that accompany retrospective design, i.e., selection bias or misclassification of outcome or exposure variables, as well as those that are associated with Medicare administrative datasets: coding errors (which may be random or systemic, and affect the validity of our PD diagnosis), coding variability practices by different providers, case mixing, and disease severity confounding. In addition, we only had access to Medicare Carrier claims, and thus our utilization estimates do not include patients (1) receiving rehabilitation services exclusively in home health by virtue of being homebound or in acute inpatient rehabilitation or in skilled nursing settings under Medicare Part A and also (2) receiving rehabilitative services exclusively from providers who do not bill for services under Medicare Part B. We also do not have data for patients who do not use insurance for rehabilitation services, such as those who pay out of pocket or belong to a community or patient organization–sponsored fitness program, nor do we have data for those participating in other organized modalities of therapy and group exercise directed at patients for PD (e.g., dance, boxing, tai chi, BIG & LOUD)1,27–30 that are not currently covered by Medicare. Patient-reported use of rehabilitation services in a National Parkinson Foundation Center of Excellence study was higher (PT 47%, OT 20%, and ST 21%), perhaps reflecting the diversity of rehabilitation and rehabilitation-like service use among academic medical center study patients.31 Therefore, our data do not necessarily imply that patients with PD are not receiving appropriate care; they may have been receiving care outside of the Medicare system. In addition, this study only includes patients 65 years or older, so the results may not be generalizable to younger patients with PD. The percentage of men and women in the PD group were similar, which at first may seem to be at odds with the known association of PD with male sex.32 It is important to note that the sex differences in PD relate to incidence (number with disease/total number at risk of disease), which bears no relation to the sex distribution within an all-PD cohort. Women have greater longevity and increased survival after PD diagnosis, thus it is not surprising to observe similar numbers of women and men in a prevalence cohort.
This study provides data on what was billed for through Medicare and does not capture what was discussed during visits. A recent study reviewed adherence with the AAN quality measure guidelines from 2010 and found that rehabilitation therapies were reviewed annually in only 7.5% of cases.33 Although we found no correlation between rehabilitation therapy provider supply and utilization rates, the distance from and accessibility of care for the individual patients in this study is unknown and plausibly plays a role. Administrative data are subject to coding errors or bias, which may be random or systemic. Despite these limitations, this study provides important data on rehabilitation therapies use in the largest segment of the US PD population prior to the introduction of the AAN quality measurement set and may serve as a benchmark for future research following the implementation of these guidelines. Our data may also inform US research priorities and policies aimed at increasing the delivery of proven therapies for PD.
Supplementary Material
GLOSSARY
- AAN
American Academy of Neurology
- AOR
adjusted odds ratio
- CMS
Centers for Medicare and Medicaid Services
- CPT
Current Procedural Terminology
- ICD-9
International Classification of Diseases–9
- OT
occupational therapy
- PD
Parkinson disease
- PT
physical therapy
- ST
speech therapy
Footnotes
Supplemental data at Neurology.org
AUTHOR CONTRIBUTIONS
Michelle Fullard: interpretation of data, drafting manuscript. Dylan P. Thibault: analysis and interpretation of data, study design. Andrew Hill: interpretation of data. Joellyn Fox: revision of manuscript for intellectual content. Danish E. Bhatti: revision of manuscript for intellectual content. Michelle A. Burack: revision of manuscript for intellectual content. Nabila Dahodwala: revision of manuscript for intellectual content. Elizabeth Haberfeld: revision of manuscript for intellectual content. Drew S. Kern: revision of manuscript for intellectual content. Olga S. Klepitskava: revision of manuscript for intellectual content. Enrique Urrea-Mendoza: revision of manuscript for intellectual content. Phillip Myers: revision of manuscript for intellectual content. Jay Nutt: revision of manuscript for intellectual content. Miriam R. Rafferty: revision of manuscript for intellectual content. Jason M. Schwalb: revision of manuscript for intellectual content. Lisa M. Shulman: revision of manuscript for intellectual content. Allison W. Willis: study concept and design, acquisition of data, interpretation of data, revision of manuscript for intellectual content.
STUDY FUNDING
This study was funded by NIH K23NS081087 and T32NS061779-07.
DISCLOSURE
M. Fullard is funded by NIH training grant T32NS061779-07. D. Thibault, A. Hill, and J. Fox report no disclosures relevant to the manuscript. D. Bhatti is on a speaker panel for Teva Neurosciences and ACCADIA Pharmaceuticals. A. Burack reports no disclosures relevant to the manuscript. N. Dahodwala is funded by the NIH, National Parkinson Foundation, Parkinson Counsil, Biotie, and AbbVie. E. Haberfeld reports no disclosures relevant to the manuscript. D. Kern has served as an advisor for Michael J. Fox Foundation and AbbVie Pharmaceutics; has received honorarium from Merz Pharma, AbbVie Pharmaceutics, and SAI-Med Partners, LLC; and has received grants from the Parkinson's Society of Canada and University of Colorado Skin Disease Research Center. O. Klepitskaya received consulting fees from Acadia Pharmaceuticals. E. Urrea-Mendoza received honorarium from Great Lakes NeuroTechnologies. P. Myers reports no disclosures relevant to the manuscript. J. Nutt serves as a consultant for Neuroderm Ltd., Merck, Elan Pharmaceuticals, Lundbeck Inc., ONO Pharma, SynAgile Crop., Prexa Inc., and US World Med, and has received honoraria from the American Academy of Neurology. M. Rafferty reports no disclosures relevant to the manuscript. J. Schwalb receives research funding from Medtronic. L. Shulman is funded by the NIH for research and clinical trials, as well as the Fox Foundation, The Veteran's Administration Medical Center, PCORI, The Rosalyn Newman Foundation, The Brin Family, and Biotie Therapies. A. Willis received research support from the NIH (K23NS081087), the Patient-Centered Outcomes Research Institute (PCORI), the St. Louis Chapter of the American Parkinson Disease Association, the University of Pennsylvania, Walter and Connie Donius, and The Robert Renschen Fund. Go to Neurology.org for full disclosures.
REFERENCES
- 1.Alves Da Rocha P, McClelland J, Morris ME. Complementary physical therapies for movement disorders in Parkinson's disease: a systematic review. Eur J Phys Rehabil Med 2015;51:693–704. [PubMed] [Google Scholar]
- 2.Atkinson-Clement C, Sadat J, Pinto S. Behavioral treatments for speech in Parkinson's disease: meta-analyses and review of the literature. Neurodegenerative Dis Manag 2015;5:233–248. [DOI] [PubMed] [Google Scholar]
- 3.Azevedo LL, Souza IS, Oliveira PM, Cardoso F. Effect of speech therapy and pharmacological treatment in prosody of parkinsonians. Arq Neuropsiquiatr 2015;73:30–35. [DOI] [PubMed] [Google Scholar]
- 4.Dibble LE, Addison O, Papa E. The effects of exercise on balance in persons with Parkinson's disease: a systematic review across the disability spectrum. J Neurol Phys Ther 2009;33:14–26. [DOI] [PubMed] [Google Scholar]
- 5.Gisbert R, Schenkman M. Physical therapist interventions for Parkinson disease. Phys Ther 2015;95:299–305. [DOI] [PubMed] [Google Scholar]
- 6.Goodwin VA, Richards SH, Taylor RS, Taylor AH, Campbell JL. The effectiveness of exercise interventions for people with Parkinson's disease: a systematic review and meta-analysis. Mov Disord 2008;23:631–640. [DOI] [PubMed] [Google Scholar]
- 7.Saint-Hilaire M. Occupational therapy for Parkinson's disease: increasing awareness. Lancet Neurol 2014;13:527–529. [DOI] [PubMed] [Google Scholar]
- 8.Smidt N, de Vet HC, Bouter LM, et al. Effectiveness of exercise therapy: a best-evidence summary of systematic reviews. Aust J Physiother 2005;51:71–85. [DOI] [PubMed] [Google Scholar]
- 9.Sturkenboom IH, Graff MJ, Hendriks JC, et al. Efficacy of occupational therapy for patients with Parkinson's disease: a randomised controlled trial. Lancet Neurol 2014;13:557–566. [DOI] [PubMed] [Google Scholar]
- 10.Tomlinson CL, Patel S, Meek C, et al. Physiotherapy versus placebo or no intervention in Parkinson's disease. Cochrane Database Syst Rev 2012;7:Cd002817. [DOI] [PubMed] [Google Scholar]
- 11.van der Kolk NM, King LA. Effects of exercise on mobility in people with Parkinson's disease. Mov Disord 2013;28:1587–1596. [DOI] [PubMed] [Google Scholar]
- 12.Cheng EM, Tonn S, Swain-Eng R, Factor SA, Weiner WJ, Bever CT Jr. Quality improvement in neurology: AAN Parkinson disease quality measures: report of the Quality Measurement and Reporting Subcommittee of the American Academy of Neurology. Neurology 2010;75:2021–2027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wright Willis A, Evanoff BA, Lian M, Criswell SR, Racette BA. Geographic and ethnic variation in Parkinson disease: a population-based study of US Medicare beneficiaries. Neuroepidemiology 2010;34:143–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bureau of Labor Statistics. State & Area Data: Occupational Employment Statistics (OES). Available at: bls.gov/. Accessed August 22, 2016. [Google Scholar]
- 15.Willis AW, Schootman M, Evanoff BA, Perlmutter JS, Racette BA. Neurologist care in Parkinson disease: a utilization, outcomes, and survival study. Neurology 2011;77:851–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keus SH, Bloem BR, Verbaan D, et al. Physiotherapy in Parkinson's disease: utilisation and patient satisfaction. J Neurol 2004;251:680–687. [DOI] [PubMed] [Google Scholar]
- 17.Parkinson's UK. Life with Parkinson's Today: Room for Improvement. London: Parkinson's UK; 2007. [Google Scholar]
- 18.Scott S, Caird FI. Speech therapy for Parkinson's disease. J Neurol Neurosurg Psychiatry 1983;46:140–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wood BH, Bilclough JA, Bowron A, Walker RW. Incidence and prediction of falls in Parkinson's disease: a prospective multidisciplinary study. J Neurol Neurosurg Psychiatry 2002;72:721–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ellis T, Boudreau JK, DeAngelis TR, et al. Barriers to exercise in people with Parkinson disease. Phys Ther 2013;93:628–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Willis AW, Schootman M, Tran R, et al. Neurologist-associated reduction in PD-related hospitalizations and health care expenditures. Neurology 2012;79:1774–1780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parkinson's Disease Foundation. Available at: pdf.org/. Accessed October 18, 2016.
- 23.American Parkinson Disease Foundation. Available at: apdaparkinson.org/. Accessed October 18, 2016.
- 24.National Parkinson Disease Foundation. Available at: parkinson.org/. Accessed October 18, 2016.
- 25.Parkinson Study Group. Available at: parkinson-study-group.org/. Accessed October 18, 2016.
- 26.ParkinsonNet. Available at: parkinsonnet.info/. Accessed October 18, 2016.
- 27.Combs SA, Diehl MD, Chrzastowski C, et al. Community-based group exercise for persons with Parkinson disease: a randomized controlled trial. NeuroRehabilitation 2013;32:117–124. [DOI] [PubMed] [Google Scholar]
- 28.Fox C, Ebersbach G, Ramig L, Sapir S. LSVT LOUD and LSVT BIG: behavioral treatment programs for speech and body movement in Parkinson disease. Parkinsons Dis 2012;2012:391946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McKay JL, Ting LH, Hackney ME. Balance, body motion, and muscle activity after high-volume short-term dance-based rehabilitation in persons with Parkinson disease: a pilot study. J Neurol Phys Ther 2016;40:257–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhou J, Yin T, Gao Q, Yang XC. A meta-analysis on the efficacy of tai chi in patients with Parkinson's disease between 2008 and 2014. Evid Based Complement Altern Med 2015;2015:593263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hassan A, Wu SS, Schmidt P, et al. The profile of long-term Parkinson's disease survivors with 20 years of disease duration and beyond. J Parkinsons Dis 2015;5:313–319. [DOI] [PubMed] [Google Scholar]
- 32.Van Den Eeden SK, Tanner CM, Bernstein AL, et al. Incidence of Parkinson's disease: variation by age, gender, and race/ethnicity. Am J Epidemiol 2003;157:1015–1022. [DOI] [PubMed] [Google Scholar]
- 33.Baek WS, Swenseid SS, Poon KY. Quality care assessment of Parkinson's disease at a tertiary medical center. Int J Neurosci 2013;123:221–225. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.