Abstract
Background
Human African trypanosomiasis (HAT), a lethal disease induced by Trypanosoma brucei gambiense, has a range of clinical outcomes in its human host in West Africa: an acute form progressing rapidly to second stage, spontaneous self-cure and individuals able to regulate parasitaemia at very low levels, have all been reported from endemic foci. In order to test if this clinical diversity is influenced by host genetic determinants, the association between candidate gene polymorphisms and HAT outcome was investigated in populations from HAT active foci in Guinea.
Methodology and results
Samples were collected from 425 individuals; comprising of 232 HAT cases, 79 subjects with long lasting positive and specific serology but negative parasitology and 114 endemic controls. Genotypes of 28 SNPs in eight genes passed quality control and were used for an association analysis. IL6 rs1818879 allele A (p = 0.0001, OR = 0.39, CI95 = [0.24–0.63], BONF = 0.0034) was associated with a lower risk of progressing from latent infection to active disease. MIF rs36086171 allele G seemed to be associated with an increased risk (p = 0.0239, OR = 1.65, CI95 = [1.07–2.53], BONF = 0.6697) but did not remain significant after Bonferroni correction. Similarly MIF rs12483859 C allele seems be associated with latent infections (p = 0.0077, OR = 1.86, CI95 = [1.18–2.95], BONF = 0.2157). We confirmed earlier observations that APOL1 G2 allele (DEL) (p = 0.0011, OR = 2.70, CI95 = [1.49–4.91], BONF = 0.0301) is associated with a higher risk and APOL1 G1 polymorphism (p = 0.0005, OR = 0.45, CI95 = [0.29–0.70], BONF = 0.0129) with a lower risk of developing HAT. No associations were found with other candidate genes.
Conclusion
Our data show that host genes are involved in modulating Trypanosoma brucei gambiense infection outcome in infected individuals from Guinea with IL6 rs1818879 being associated with a lower risk of progressing to active HAT. These results enhance our understanding of host-parasite interactions and, ultimately, may lead to the development of new control tools.
Author summary
Human African Trypanosomiasis (HAT) known as sleeping sickness is a lethal neglected disease in West and Central Africa, caused by the parasite Trypanosoma brucei gambiense that is transmitted by tsetse flies Glossina palpalis gambiensis. The disease has long been considered to be invariably fatal, but field studies show that T. b. gambiense infection leads to a wide diversity of clinical outcomes. An acute form progressing rapidly to second stage; spontaneous self-cure and individuals able to control parasitaemia at very low levels (latent infections). In the present study, we test for associations between candidate gene polymorphisms and different HAT phenotypes (HAT confirmed cases, latent infections) and endemic controls, in order to identify relationships between the clinical diversity and host genetic determinants. Our results, based on clinical, serological and parasitological observations, combined with genotypes and association analysis form the most complete study of host genetic determinants and clinical diversity of HAT in Guinea to date. We show that host genes are involved in modulating responses in Trypanosoma brucei gambiense infected individuals. A new association was found between IL6 rs1818879 and a reduced risk of progressing from latent infection to active HAT. These results constitute an important stage toward the identification of the natural human mechanisms involved in T. b. gambiense infection regulation.
Introduction
Human African trypanosomiasis (HAT) known as sleeping sickness is a neglected disease of sub-Saharan Africa caused by two sub-species of trypanosomes, Trypanosoma brucei (T. b.) gambiense (in West and Central Africa) and T. b. rhodesiense (in East and South Africa), with T. b. gambiense causing > 95% of all cases [1]. In West Africa, Guinea is the country with the highest prevalence for HAT, especially on the coast [2], where the vector, the tsetse fly Glossina palpalis gambiensis is abundant [3]. In the active foci of Boffa, Dubreka and Forecariah prevalence in humans is generally around 0.5–1%, but can go up to 5% in some villages [1,3,4]. HAT caused by T. b. gambiense is classically described as a chronic disease with an early haemolymphatic phase (first stage) associated with nonspecific symptoms such as intermittent fevers and headaches, followed by a meningoencephalitic phase (second stage) where the parasite invades the central nervous system (CNS) leading to neurological disorders. In the absence of treatment, HAT is widely assumed to be 100% fatal. However, asymptomatic carriers and spontaneous cure without treatment have been described in old [5] and more recent reports [6], strengthening the evidence for human trypanotolerance / resistance [7–10]. Indeed, a recent long-term longitudinal survey in Côte d’Ivoire found people who were initially diagnosed by microscopy but on follow-up examination, up to 15 years later, had no detectable parasitaemia by microscopy, despite not having received treatment [6]. A drop in antibody titers to seronegative levels was detected in some of these subjects, indicating that they have self-cured. In contrast, others maintained a long-lasting serological response, being Card Agglutination Test for Trypanosomiasis (CATT) and trypanolysis (TL) test positive but had no parasites detectable by microscopy, suggesting that these individuals were able to control blood parasitaemia at very low levels and were considered as asymptomatic carriers of parasites and were classified as latent infections [4,9,11].
Many factors could play a role in this variability of response to infection, and the respective roles of the virulence of the parasite and host susceptibility in this clinical diversity remain unclear [12]. It has been suggested that genetic polymorphism of the parasite could be associated with asymptomatic and very chronic infections [11]. Nevertheless, host genetic factors involved in the control of immunity could regulate infection levels or mortality rates, as has been shown for Trypanosoma congolense infections in experimental models [13,14] and also T. brucei spp in humans [15–20].
Hence, the purpose of the present study was to study the role of single nucleotide polymorphisms (SNPs) in IL4, IL6, IL8, IL10, IFNG, APOL1, TNFA, HPR, HLA-G, HLA-A, HP, and MIF genes on susceptibility/resistance to HAT by means of an association study between HAT cases, seropositive microscopically aparasitaemic subjects with latent infections, and controls in order to explore their possible role in human immunity to this complex disease.
Methods
Informed consent and ethics statement
The study was performed as part of medical survey conducted by the national control program according to the national HAT diagnostic procedures and was approved by the Ministry of Health in Guinea. All participants were informed about the objective of the study in their own language and signed an informed consent form. For participants under 18 year of age, a written informed consent was obtained from the parent. This study is part of a TrypanoGEN project which aims to understand the genetic basis of human susceptibility to trypanosomiasis and samples were archived in the TrypanoGEN Biobank at CIRDES [21] for which approval was obtained from the Guinea National ethics committee (1-22/04/2013).
Study population
The study was carried out in three active HAT foci (Dubreka, Boffa, and Forecariah) in the mangrove areas of coastal Guinea. Most of the population is from the Soussou ethnic group and lives in small villages scattered along mangrove channels [1,3]. All subjects included in this study were identified during medical monitoring surveys organized by the National HAT Control Program (NCP) between November 2007 and December 2013, according to the WHO and NCP policies described elsewhere [4]. Blood (5 ml) was collected in heparinized tubes. For individuals who are positive to the CATT (Card Agglutination Test for Trypanosomiasis) serological mass screening test, a twofold plasma dilution series was tested to determine their CATT end titer. All individuals with titers of 1/4 or greater were submitted to microscopic examination of lymph node aspirates whenever swollen lymph nodes were present; 350 ml of buffy coat was then examined by using the mini-anion exchange column (mAECT) test which has shown to have a threshold of detection of 10 trypanosomes ml-1 of blood [3,22]. Samples that were CATT negative, CATT positive with lymph node and/or buffy coat negative for trypanosomes were all subject to the immune trypanolysis test (TL), which is a serological test that is highly specific for T. b. gambiense [23]. 425 individuals were selected according to the study inclusion criteria below.
Phenotype definitions
Samples were classified into three phenotypes: (1) Cases or active HAT patients are defined as subjects presenting as positive on both serological tests (CATT and TL) and parasitological tests (mAECT and/or examination of cervical lymph juice aspirates); (2) latent infections have CATT plasma dilution end titer 1/4 or higher; TL positive and are parasitology negative and maintain this phenotype for at least two years; (3) endemic controls who have serology (CATT and TL) negative and living in the same village as a HAT patient and/or a seropositive subject. All individuals live in the same area and had been exposed to the risk of infection since birth [21].
Study design
This study was one of six studies of populations of HAT endemic areas in DRC, Cameroon, Cote d’Ivoire, Guinea, Malawi and Uganda. The studies were designed to have 80% power to detect odds ratios (OR) >2 for loci with disease allele frequencies of 0.15–0.65 with the 80 SNPs genotyped. The study design included a total of 425 samples: 232 HAT cases, 79 seropositive and 114 uninfected or endemic controls. Power calculations were undertaken using the genetics analysis package gap in r [24].
DNA extraction
DNA was extracted from buffy coat (BC) samples using the Qiagen DNA extraction kit (QIAamp DNA Blood Midi Kit) following the instructions of the manufacturer. The DNA extract was stored at -20°C. After extraction each DNA sample was quantified on a spectrophotometer (NanoDrop).
Single Nucleotide Polymorphisms (SNPs) selection
80 SNP were selected for genotyping using two strategies: 1) specific SNP in IL10, TNFA, HLA-A, HLA-G, APOL1, MIF, HPR and HP had been previously reported to be associated with HAT or 2) IL4, IL8, IL6, HLA-G and IFNG were scanned for sets of linked marker SNP (r2 < 0.5) across each gene. The SNPs in this second group of genes were selected using a merged set of SNP obtained from low fold coverage (8-10x) whole genome shotgun data generated from 230 residents living in regions (Democratic Republic of Congo, Guinea Conakry, Ivory Coast and Uganda) where trypanosomiasis is endemic (TrypanoGEN consortium, European Nucleotide Archive Study Number EGAS00001002482) and 1000 Genomes Project data from African populations, only published SNP with dbSNP identifiers were used in the design. Linkage (r2) between loci was estimated using Plink and sets of SNP that covered the gene were identified. Some SNP loci were excluded during assay development or failed to genotype and were not replaced.
Genotyping
Samples were submitted to Plateforme Genome Transcriptome de Bordeaux at INRA Site de Pierroton. Multiplex design (two sets of 40 SNPs) was performed using Assay Design Suite v2.0 (Agena Biosciences). SNP genotyping was achieved with the iPLEX Gold genotyping kit (Agena Biosciences) for the MassArray iPLEX genotyping assay, following the manufacturer’s instructions. Products were detected on a MassArray mass spectrophotometer and data were acquired in real time with MassArray RT software (Agena Biosciences). SNP clustering and validation was carried out with Typer 4.0 software (Agena Biosciences). APOL1 rs71785313 SNP was genotyped again by LGC Genomics, Hoddesden, United Kingdom, using the PCR based KASP assay [25].
Statistical analysis
Plink v1.9 [26] was used for statistical analysis, allele frequencies were analyzed by simple allele counting and the R 3.3.1 software package was used for data visualization (R Foundation for Statistical Computing, Vienna Austria). For quality control and filtering, SNPs loci with missing genotypes > 10% and individuals with missing loci > 10% were removed. In addition SNPs with Hardy equilibrium (HWE) p < 0.001, minor allele frequency MAF < 0.05, SNPs in linkage with adjacent SNPs (r2 > 0.5) and monomorphic loci were also pruned [27]. 28 SNPs were remaining after filtering and LD pruning and were used to test association with the disease. Association analysis’s were done using pairwise comparison between cases-controls, cases-latent infections and latent infections-controls. The Fisher exact test was used to test for significant differences in allele frequencies between phenotypes. We also tested for association with disease under additive model allowing for non-genetic risk factors “sex and age”. Odds ratio for the minor allele A1, and p-value for association, were adjusted for age and sex. In all analysis, results were adjusted by Bonferroni correction for multiple comparisons. The Bonferroni correction establishes the threshold of significance at α/n. P-values smaller than 0.05/28 = 0.0018 or an adjusted p-value <0.05 were considered significant.
Results
Genes and SNPs selected
In total 12 candidate genes that have known or plausible associations with HAT were identified from the literature. 80 SNPs were identified 17 in HLA-G, 2 in HLA-A, 2 in HPR, 10 in IFNG, 16 in IL4, 12 in IL6, 6 in IL8, 1 in IL10, 8 in MIF, 3 in TNFA, 1 in HP and 2 in APOL1. 28 of these 80 SNPs remained after quality control and linkage pruning and were used for association analysis (Table 1). These SNPs are in HWE, MAF > 5% and LD r2 < 0.5. SNPs with allele frequencies that deviated from HWE were removed. The allelic and minor allele carrier frequencies are shown in Tables 2–4, along with the results of the association test.
Table 1. SNPs remaining after quality control and LD pruning.
| CHR | Genes | SNPs selected | SNPs pass filtered |
|---|---|---|---|
| 1 | IL10 | 1 | 0 |
| 4 | IL8 | 6 | 4 |
| 5 | IL4 | 16 | 3 |
| 6 | HLAG | 17 | 2 |
| 6 | TNFA | 3 | 2 |
| 6 | HLAA | 2 | 0 |
| 7 | IL6 | 12 | 6 |
| 12 | IFNG | 10 | 5 |
| 16 | HPR | 2 | 0 |
| 16 | HP | 1 | 1 |
| 22 | MIF | 8 | 3 |
| 22 | APOL1 | 2 | 2 |
| Total | 12 | 80 | 28 |
CHR: Chromosome number, SNP: single nucleotide polymorphism
Table 2. Association analysis between HAT cases and controls.
| CHR | Genes | SNP | BP | A1 | A2 | P | BONF | FDR_BH | FRD_BY | OR | CI95 | HWE | FST |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4 | IL8 | rs114259658 | 74605639 | A | T | 0.7973 | 1 | 0.9408 | 1 | 1.08 | 0.59–2.00 | 0.4410 | -0.00361 |
| 4 | IL8 | rs2227307 | 74606669 | T | G | 0.2343 | 1 | 0.5468 | 1 | 0.81 | 0.57–1.15 | 0.1314 | 0.00104 |
| 4 | IL8 | rs2227545 | 74608727 | C | A | 0.1212 | 1 | 0.4848 | 1 | 1.63 | 0.88–3.01 | 1 | 0.00288 |
| 4 | IL8 | rs58478511 | 74610033 | A | G | 0.4888 | 1 | 0.8235 | 1 | 1.14 | 0.78–1.66 | 0.8098 | -0.00218 |
| 5 | IL4 | rs2243261 | 132012806 | T | G | 0.1736 | 1 | 0.4860 | 1 | 0.75 | 0.49–1.14 | 0.4260 | 0.00326 |
| 5 | IL4 | rs2243283 | 132016593 | G | C | 0.5212 | 1 | 0.8235 | 1 | 0.87 | 0.56–1.34 | 0.2041 | -0.00405 |
| 5 | IL4 | rs9282745 | 132014000 | A | T | 0.9918 | 1 | 0.9918 | 1 | 1.00 | 0.57–1.74 | 0.0706 | -0.00265 |
| 6 | HLAG | rs1610696 | 29798803 | G | C | 0.9145 | 1 | 0.9849 | 1 | 0.98 | 0.67–1.44 | 0.0016 | -0.00398 |
| 6 | HLAG | rs2517898 | 29799746 | G | C | 0.6884 | 1 | 0.9178 | 1 | 0.93 | 0.64–1.34 | 0.1739 | -0.00054 |
| 6 | TNFA | rs1800629 | 31543031 | A | G | 0.8156 | 1 | 0.9408 | 1 | 1.06 | 0.66–1.71 | 0.2207 | -0.00108 |
| 6 | TNFA | rs1800630 | 31542476 | A | C | 0.2117 | 1 | 0.5388 | 1 | 1.47 | 0.80–2.67 | 1 | -0.00044 |
| 7 | IL6 | rs1474347 | 22768124 | C | A | 0.0941 | 1 | 0.4393 | 1 | 1.91 | 0.90–4.08 | 1 | 0.00671 |
| 7 | IL6 | rs1548216 | 22769773 | C | G | 0.2988 | 1 | 0.6025 | 1 | 1.28 | 0.81–2.02 | 1 | 0.00392 |
| 7 | IL6 | rs1818879 | 22772727 | A | G | 0.1698 | 1 | 0.4860 | 1 | 0.71 | 0.43–1.16 | 0.4504 | 0.00487 |
| 7 | IL6 | rs2066992 | 22768249 | T | G | 0.5336 | 1 | 0.8235 | 1 | 0.82 | 0.45–1.52 | 1 | -0.00152 |
| 7 | IL6 | rs2069837 | 22768027 | G | A | 0.0871 | 1 | 0.4393 | 1 | 0.64 | 0.38–1.07 | 0.1147 | 0.00977 |
| 7 | IL6 | rs2069855 | 22772624 | C | T | 0.3012 | 1 | 0.6025 | 1 | 1.41 | 0.74–2.70 | 1 | -0.00041 |
| 12 | IFNG | rs2069705 | 68555011 | A | G | 0.9559 | 1 | 0.9913 | 1 | 1.01 | 0.72–1.41 | 0.3431 | -0.00206 |
| 12 | IFNG | rs2069722 | 68548953 | A | G | 0.5588 | 1 | 0.8235 | 1 | 1.25 | 0.59–2.62 | 1 | -0.00184 |
| 12 | IFNG | rs2069728 | 68547784 | T | C | 0.8400 | 1 | 0.9408 | 1 | 1.04 | 0.71–1.51 | 0.3854 | -0.00327 |
| 12 | IFNG | rs2430561 | 68552522 | A | T | 0.1464 | 1 | 0.4860 | 1 | 1.56 | 0.86–2.86 | 0.5307 | 0.00438 |
| 12 | IFNG | rs78554979 | 68554636 | C | T | 0.0449* | 1 | 0.4393 | 1 | 0.55 | 0.31–0.99 | 0.2102 | 0.00940 |
| 16 | HP | rs8062041 | 72088964 | T | C | 0.6853 | 1 | 0.9178 | 1 | 1.07 | 0.76–1.51 | 0.6999 | -0.00300 |
| 22 | APOL1 | rs71785313 | 36661916 | DEL | INSERT | 0.5324 | 1 | 0.8235 | 1 | 1.15 | 0.74–1.79 | 0.3534 | -0.00147 |
| 22 | APOL1 | rs73885319 | 36661906 | G | A | 0.7318 | 1 | 0.9314 | 1 | 0.92 | 0.59–1.45 | 1 | -0.00325 |
| 22 | MIF | rs12483859 | 24234807 | C | T | 0.0807 | 1 | 0.4393 | 1 | 1.38 | 0.96–1.98 | 0.1429 | 0.00610 |
| 22 | MIF | rs34383331 | 24238079 | A | T | 0.0914 | 1 | 0.4393 | 1 | 0.67 | 0.42–1.07 | 1 | 0.00581 |
| 22 | MIF | rs36086171 | 24235455 | G | A | 0.0239* | 0.6697 | 0.4393 | 1 | 1.65 | 1.07–2.53 | 0.3772 | 0.02344 |
CHR: Chromosome number, SNP: single nucleotide polymorphism, BP: Physical position (base-pair in GRCh37), A1: Minor allele name, A2: Major allele name, P: Exact p-value, BONF: Bonferroni corrected p-value, FDR: false discovery rate, OR: Estimated odds ratio (for A1), CI95: 95% confidence interval, HWE: Hardy-Weinberg Equilibrium p-value
* P-value significant; DEL: deletion of 6 base pair; INSER: insertion of 6 base pair.
Table 4. Association analysis between latent infection and controls groups.
| CHR | Genes | SNP | BP | A1 | A2 | P | BONF | FDR_BH | FRD_BY | OR | CI95 | HWE | FST |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4 | IL8 | rs114259658 | 74605639 | A | T | 0.6168 | 1 | 0.9090 | 1 | 1.22 | 0.57–2.62 | 0.4410 | -0.00351 |
| 4 | IL8 | rs2227307 | 74606669 | T | G | 0.0728 | 1 | 0.3402 | 1 | 0.67 | 0.43–1.04 | 0.1314 | 0.01008 |
| 4 | IL8 | rs2227545 | 74608727 | C | A | 0.4602 | 1 | 0.8088 | 1 | 1.31 | 0.64–2.69 | 1 | -0.00240 |
| 4 | IL8 | rs58478511 | 74610033 | A | G | 0.1492 | 1 | 0.5455 | 1 | 1.39 | 0.89–2.17 | 0.8098 | 0.00690 |
| 5 | IL4 | rs2243261 | 132012806 | T | G | 0.2078 | 1 | 0.5818 | 1 | 0.71 | 0.42–1.21 | 0.4260 | -0.00060 |
| 5 | IL4 | rs2243283 | 132016593 | G | C | 0.9907 | 1 | 0.9907 | 1 | 1.00 | 0.59–1.70 | 0.2041 | -0.00552 |
| 5 | IL4 | rs9282745 | 132014000 | A | T | 0.4863 | 1 | 0.8088 | 1 | 0.77 | 0.38–1.59 | 0.0706 | -0.00246 |
| 6 | HLAG | rs1610696 | 29798803 | G | C | 0.6677 | 1 | 0.9337 | 1 | 0.90 | 0.56–1.45 | 0.0016 | -0.00503 |
| 6 | HLAG | rs2517898 | 29799746 | G | C | 0.2517 | 1 | 0.6407 | 1 | 0.76 | 0.48–1.21 | 0.1739 | 0.00193 |
| 6 | TNFA | rs1800629 | 31543031 | A | G | 0.8195 | 1 | 0.9337 | 1 | 1.07 | 0.61–1.87 | 0.2207 | -0.00452 |
| 6 | TNFA | rs1800630 | 31542476 | A | C | 0.8519 | 1 | 0.9337 | 1 | 1.07 | 0.53–2.17 | 1 | -0.00547 |
| 7 | IL6 | rs1474347 | 22768124 | C | A | 0.1617 | 1 | 0.5455 | 1 | 1.87 | 0.78–4.50 | 1 | 0.00398 |
| 7 | IL6 | rs1548216 | 22769773 | C | G | 0.8231 | 1 | 0.9337 | 1 | 1.07 | 0.61–1.86 | 1 | -0.00433 |
| 7 | IL6 | rs1818879 | 22772727 | A | G | 0.0091* | 0.2542 | 0.0636 | 0.2496 | 2.06 | 1.20–3.56 | 0.4504 | 0.02987 |
| 7 | IL6 | rs2066992 | 22768249 | T | G | 0.3577 | 1 | 0.8088 | 1 | 1.39 | 0.69–2.78 | 1 | -0.00258 |
| 7 | IL6 | rs2069837 | 22768027 | G | A | 0.1754 | 1 | 0.5455 | 1 | 0.65 | 0.35–1.21 | 0.1147 | 0.00748 |
| 7 | IL6 | rs2069855 | 22772624 | C | T | 0.8764 | 1 | 0.9337 | 1 | 1.07 | 0.46–2.51 | 1 | -0.00504 |
| 12 | IFNG | rs2069705 | 68555011 | A | G | 0.3858 | 1 | 0.8088 | 1 | 1.21 | 0.78–1.88 | 0.3431 | -0.00064 |
| 12 | IFNG | rs2069722 | 68548953 | A | G | 0.4910 | 1 | 0.8088 | 1 | 0.69 | 0.24–1.97 | 1 | -0.00276 |
| 12 | IFNG | rs2069728 | 68547784 | T | C | 0.7634 | 1 | 0.9337 | 1 | 0.93 | 0.58–1.49 | 0.3854 | -0.00473 |
| 12 | IFNG | rs2430561 | 68552522 | A | T | 0.0729 | 1 | 0.3402 | 1 | 1.89 | 0.94–3.80 | 0.5307 | 0.01195 |
| 12 | IFNG | rs78554979 | 68554636 | C | T | 0.9004 | 1 | 0.9337 | 1 | 0.96 | 0.49–1.89 | 0.2102 | -0.00468 |
| 16 | HP | rs8062041 | 72088964 | T | C | 0.5508 | 1 | 0.8569 | 1 | 0.88 | 0.58–1.33 | 0.6999 | -0.00241 |
| 22 | APOL1 | rs71785313 | 36661916 | DEL | INSERT | 0.0070* | 0.1973 | 0.0636 | 0.2496 | 0.39 | 0.20–0.78 | 0.3534 | 0.02888 |
| 22 | APOL1 | rs73885319 | 36661906 | G | A | 0.0056* | 0.1570 | 0.0636 | 0.2496 | 2.09 | 1.24–3.53 | 1 | 0.03883 |
| 22 | MIF | rs12483859 | 24234807 | C | T | 0.0077* | 0.2157 | 0.0636 | 0.2496 | 1.86 | 1.18–2.95 | 0.1429 | 0.03028 |
| 22 | MIF | rs34383331 | 24238079 | A | T | 0.8246 | 1 | 0.9337 | 1 | 1.06 | 0.62–1.81 | 1 | -0.00513 |
| 22 | MIF | rs36086171 | 24235455 | G | A | 0.4467 | 1 | 0.8088 | 1 | 1.24 | 0.72–2.13 | 0.3772 | -0.00240 |
CHR: Chromosome number, SNP: single nucleotide polymorphism, BP: Physical position (base-pair in GRCh37), A1: Minor allele name, A2: Major allele name, P: Exact p-value, BONF: Bonferroni corrected p-value, FDR: false discovery rate, OR: Estimated odds ratio (for A1), CI95: 95% confidence interval, HWE: Hardy-Weinberg Equilibrium p-value
* P-value significant
DEL: deletion of 6 base pair
INSER: insertion of 6 base pair.
Association study
The APOL1 rs73885319 polymorphism is one part of a two SNP haplotype, with derived alleles designated “G1” composed of two tightly linked coding variants rs73885319 (S342G) and rs60910145 (I384M) non-synonymous in the last exon of APOL1. The derived allele of rs71785313 called APOL1 G2 APOL1 is a 6 base pair deletion, removing amino acids N388 and Y389. Wild type APOL1 is known as G0. APOL1 alleles G1 and G2 are independent [28]. The distribution of APOL1 G1 and APOL1 G2 in the present study were significantly different in latent infections compared to both cases and controls (Tables 3 and 4). The APOL1 G2 allele carriers had a higher risk of developing HAT after infection by T. b. gambiense than the APOL1 G0 individuals (p = 0.0011, OR = 2.70, CI95 = [1.49–4.91], BONF = 0.0301). Subjects carrying the APOL1 G1 (p = 0.0005, OR = 0.45, CI95 = [0.29–0.70], BONF = 0.0129) had an increased risk of developing a latent infection but reduced risk of progressing from latent infection to active HAT than APOL1 G0 (Table 3).
Table 3. Association analysis between HAT cases and latent infection groups.
| CHR | Genes | SNP | BP | A1 | A2 | P | BONF | FDR_BH | FRD_BY | OR | CI95 | HWE | FST |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 4 | IL8 | rs114259658 | 74605639 | A | T | 0.7133 | 1 | 0.8628 | 1 | 0.89 | 0.47–1.68 | 0.4410 | -0.00384 |
| 4 | IL8 | rs2227307 | 74606669 | T | G | 0.4650 | 1 | 0.7931 | 1 | 1.15 | 0.79–1.66 | 0.1314 | -0.00118 |
| 4 | IL8 | rs2227545 | 74608727 | C | A | 0.5518 | 1 | 0.7931 | 1 | 1.20 | 0.65–2.22 | 1 | -0.00332 |
| 4 | IL8 | rs58478511 | 74610033 | A | G | 0.4429 | 1 | 0.7931 | 1 | 0.86 | 0.59–1.26 | 0.8098 | 0.00058 |
| 5 | IL4 | rs2243261 | 132012806 | T | G | 0.9303 | 1 | 0.9306 | 1 | 0.98 | 0.62–1.55 | 0.4260 | -0.00450 |
| 5 | IL4 | rs2243283 | 132016593 | G | C | 0.5761 | 1 | 0.7931 | 1 | 0.88 | 0.55–1.39 | 0.2041 | -0.00504 |
| 5 | IL4 | rs9282745 | 132014000 | A | T | 0.5372 | 1 | 0.7931 | 1 | 1.24 | 0.63–2.46 | 0.0706 | -0.00376 |
| 6 | HLAG | rs1610696 | 29798803 | G | C | 0.7436 | 1 | 0.8628 | 1 | 1.08 | 0.69–1.69 | 0.0016 | -0.00462 |
| 6 | HLAG | rs2517898 | 29799746 | G | C | 0.5946 | 1 | 0.7931 | 1 | 1.12 | 0.75–1.66 | 0.1739 | -0.00272 |
| 6 | TNFA | rs1800629 | 31543031 | A | G | 0.9306 | 1 | 0.9306 | 1 | 1.02 | 0.61–1.72 | 0.2207 | -0.00388 |
| 6 | TNFA | rs1800630 | 31542476 | A | C | 0.5948 | 1 | 0.7931 | 1 | 1.19 | 0.63–2.23 | 1 | -0.00240 |
| 7 | IL6 | rs1474347 | 22768124 | C | A | 0.7960 | 1 | 0.8628 | 1 | 1.10 | 0.54–2.21 | 1 | -0.00380 |
| 7 | IL6 | rs1548216 | 22769773 | C | G | 0.5169 | 1 | 0.7931 | 1 | 1.17 | 0.72–1.90 | 1 | -0.00117 |
| 7 | IL6 | rs1818879 | 22772727 | A | G | 0.0001* | 0.0034** | 0.004 | 0.0133 | 0.39 | 0.24–0.63 | 0.4504 | 0.08256 |
| 7 | IL6 | rs2066992 | 22768249 | T | G | 0.1921 | 1 | 0.6455 | 1 | 0.66 | 0.36–1.23 | 1 | 0.00583 |
| 7 | IL6 | rs2069837 | 22768027 | G | A | 0.8012 | 1 | 0.8628 | 1 | 1.08 | 0.60–1.93 | 0.1147 | -0.00391 |
| 7 | IL6 | rs2069855 | 22772624 | C | T | 0.3414 | 1 | 0.7931 | 1 | 1.41 | 0.70–2.85 | 1 | -0.00194 |
| 12 | IFNG | rs2069705 | 68555011 | A | G | 0.4609 | 1 | 0.7931 | 1 | 0.87 | 0.61–1.25 | 0.3431 | -0.00382 |
| 12 | IFNG | rs2069722 | 68548953 | A | G | 0.2072 | 1 | 0.6455 | 1 | 1.80 | 0.72–4.50 | 1 | 0.00331 |
| 12 | IFNG | rs2069728 | 68547784 | T | C | 0.7288 | 1 | 0.8628 | 1 | 1.07 | 0.72–1.60 | 0.3854 | -0.00384 |
| 12 | IFNG | rs2430561 | 68552522 | A | T | 0.4592 | 1 | 0.7931 | 1 | 0.81 | 0.47–1.41 | 0.5307 | -0.00261 |
| 12 | IFNG | rs78554979 | 68554636 | C | T | 0.0762 | 1 | 0.4264 | 1 | 0.57 | 0.31–1.06 | 0.2102 | 0.00916 |
| 16 | HP | rs8062041 | 72088964 | T | C | 0.3551 | 1 | 0.7931 | 1 | 1.19 | 0.82–1.73 | 0.6999 | -0.00340 |
| 22 | APOL1 | rs71785313 | 36661916 | DEL | INSERT | 0.0011* | 0.0301** | 0.0100 | 0.0394 | 2.70 | 1.49–4.91 | 0.3534 | 0.04098 |
| 22 | APOL1 | rs73885319 | 36661906 | G | A | 0.0005* | 0.0129** | 0.0065 | 0.0254 | 0.45 | 0.29–0.70 | 1 | 0.05137 |
| 22 | MIF | rs12483859 | 24234807 | C | T | 0.1643 | 1 | 0.6455 | 1 | 0.77 | 0.54–1.11 | 0.1429 | 0.00376 |
| 22 | MIF | rs34383331 | 24238079 | A | T | 0.0673 | 1 | 0.4264 | 1 | 0.64 | 0.40–1.03 | 1 | 0.00985 |
| 22 | MIF | rs36086171 | 24235455 | G | A | 0.2075 | 1 | 0.6455 | 1 | 1.32 | 0.86–2.02 | 0.3772 | 0.00459 |
CHR: Chromosome number, SNP: single nucleotide polymorphism, BP: Physical position (base-pair in GRCh37), A1: Minor allele name, A2: Major allele name, P: Exact p-value, BONF: Bonferroni corrected p-value, FDR: false discovery rate, OR: Estimated odds ratio (for A1), CI95: 95% confidence interval, HWE: Hardy-Weinberg Equilibrium p-value
* P-value significant
** Bonferroni correction significant
DEL: deletion of 6 base pair
INSER: insertion of 6 base pair.
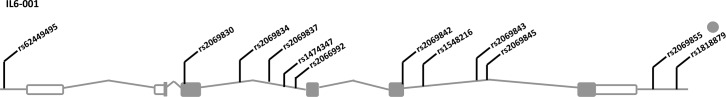
An association was observed at IL6 rs1818879 (Fig 1), indicating that subjects with latent infections carrying the A allele had a lower risk of progressing to active HAT (p = 0.0001, OR = 0.39, CI95 = [0.24–0.63], BONF = 0.0034) (Table 3).
Fig 1. Schematic of single nucleotide polymorphisms of Interleukin-6 selected from 2,000bp up and downstream (5’ and 3’) of the transcript region.
The distribution of the MIF rs36086171 G allele differed between cases and controls (BONF = 0.6697, p = 0.0239, OR = 1.65, CI95 = [1.07–2.53]), and MIF rs12483859 C allele between latent infections and Controls (BONF = 0.2157, p = 0.0077, OR = 1.86, CI95 = [1.18–2.95]) but these did not remain significant after Bonferroni correction (Tables 2 and 4).
No statistically significant differences were observed in allele frequency for the polymorphisms of other genes (IL4, IL8, HLA-G, TNFA, HP, IFNG and MIF) between cases and controls; cases and latent infection or latent infection and controls in all the analyses.
Discussion
Association analysis’s undertaken in this study allow us to investigate genetic associations of candidate genes polymorphisms with HAT in a Guinean population.
The main findings of our study are that the A allele of IL6 rs1818879 and the G allele of APOL1 G1 appear to be associated with a higher risk of developing a latent infection but a lower risk of progressing from latent infection with undetectable parasitaemia to active disease. These alleles thus seem to provide some degree of protection for individuals with latent infections, providing the ability to maintain infection levels that are undetectable by microscopy. However, the APOL1 G2 allele increased the risk of progressing from latent infection to active HAT. The associations with the APOL1 G1 and G2 polymorphisms confirm our previous observations of these SNPs with a more limited sample [20], they were genotyped again in this study as part of the larger multi-country TrypanoGEN consortium study, on an extensive sample from Guinea. Cooper et al. found an association between G2 and HAT and Controls in T. b. rhodesiense in Uganda [20].
APOL1 is a component of the trypanosome lytic factor (TLF) of human serum that confers resistance to T. b. brucei [29,30]. APOL1forms pores in the parasite endolysosomal membranes and triggers lysosome swelling which leads to trypanolysis [31]. APOL1 expression is also induced by T. b. gambiense infection enhancing its lytic activity [32]. African trypanosomes, except T. b. gambiense and T. b. rhodesiense are lysed by APOL1. These two subspecies can resist lysis by APOL1 because they express the serum resistance glycoprotein (TgsGP) and serum resistance-associated protein (SRA), respectively [33–35]. T. b. rhodesiense SRA inhibits APOL1 by direct binding but TgsGP acts by limiting uptake of APOL1. T. b. gambiense (group 1) also can resist TLF-1 killing because coding sequence mutations to the TbgHpHbR, reduce expression of Hp/Hb receptor and limit TLF-1 uptake [36]. The mode of action of G1 is unknown but the G2 mutation limits binding of SRA to APOL1 and should therefore make APOL1 G2 lytic to T. b. rhodesiense but this mechanism could not effect T. b. gambiense, which does not have the SRA gene [28,37]. In this study, we found that the 6 base pair deletion in APOL1 G2 is risk factor for developing an active T. b. gambiense infection from a latent infection.
IL6 rs1818879 A allele carriers had a lower risk of developing the disease. rs1818879 appears to fall within a CCCTC-Binding factor (CTCF) binding site and GTEx reports rs1818879 as an eQTL for AC073072, a novel antisense RNA gene within IL6 on the opposite strand about which little is known [38]. CTCF is a zinc finger protein that can be involved in activation or repression of gene expression and the disruption of this binding site may account for the eQTL associated with AC073072 [39]. Although the mechanism remains unclear, these data suggest that rs1818879 may be a functional polymorphism and not just a marker for differences in response to infection.
It has been shown that IL6 could play a role on the modification of blood brain barrier permeability in vitro together with other pro-inflammatory cytokines such as IL1 and TNFA in blood and/or in CNS [40]. IL6 plasma levels were found to be significantly higher in individuals with latent infection from Guinea as compared to controls or HAT patients [17]. Girard and al. (2005) showed that IL6 synthesis was induced in bone marrow by T. b. gambiense in vitro [41]. Therefore, Il6 appears as an important inflammatory cytokine mediating T. b. gambiense response and suggest that IL6 could play a role in the phenomenon of latent infections without parasitological confirmation. The result obtained with IL6 rs1818879 in our study is consistent with the data from a candidate gene association study in DRC, where rs2069849 in IL6 was shown to be associated with a decreased risk of developing the disease [16].
Our data show that the frequency of the G minor allele of MIF rs36086171 was higher in cases than in controls (uncorrected p = 0.0239, OR = 1.65, CI95 = [1.07–2.53]) and MIF rs12483859 C allele in latent infections than in controls (uncorrected p = 0.0077, OR = 1.86, CI95 = [1.18–2.95]). MIF is an important component of the host response implicated in the antimicrobial response and promotes the secretion and activation of pro-inflammatory cytokines, by immune cells [42,43]. Low expression of MIF has been described as favoring infection and disease progression in leishmaniasis [44]. We did not find a significant difference after correction (BONF = 0.0588), but it is known that this gene can contribute to disease development in a mice experimental model [45].
In conclusion, this study provides further evidence that the clinical diversity of sleeping sickness is partly due to the genetic diversity of the hosts. Our data demonstrate that the outcome of the disease is affected by three polymorphisms (APOL1 G1, G2 and IL6 rs1818879) in the Guinean population. This study was performed in the framework of the TrypanoGEN consortium to systematically investigate the role of host genetics in disease susceptibility and progression across East and West African populations. Further studies need to be conducted to confirm these results and to determine the mechanisms by which these alleles affect disease progression and outcome in HAT and could lead to the discovery of human natural resistance mechanisms and thus to the development of new tools for the control of this neglected tropical disease.
Acknowledgments
We thank subjects who generously donated their specimens and the field workers from the Guinean HAT foci for their dedication in collecting and processing these specimens.
Members of TrypanoGEN group: Hamidou Ilboudo, Harry Noyes, Julius Mulindwa, Magambo Phillip Kimuda, Mathurin Koffi, Justin Windingoudi Kaboré, Bernadin Ahouty, Dieudonne Mumba Ngoyi, Olivier Fataki, Gustave Simo, Elvis Ofon, John Enyaru, John Chisi, Kelita Kamoto, Martin Simuunza, Vincent P. Alibu, Veerle Lejon, Vincent Jamonneau, Annette MacLeod, Mamadou Camara, Bruno Bucheton, Christiane Hertz-Fowler, Issa Sidibe, Enock Matovu.
Data Availability
Genome data has been deposited at the European Genome-phenome Archive (EGA, http://www.ebi.ac.uk/ega/) which is hosted at the EBI, under accession number EGAS00001002602.
Funding Statement
This work was funded through the Wellcome Trust (study number 099310/Z/12/Z) awarded to the TrypanoGEN Consortium, members of H3Africa (099310). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Camara M, Kaba D, KagbaDouno M, Sanon JR, Ouendeno FF, et al. (2005) [Human African trypanosomiasis in the mangrove forest in Guinea: epidemiological and clinical features in two adjacent outbreak areas]. Med Trop (Mars) 65: 155–161. [PubMed] [Google Scholar]
- 2.Simarro PP, Diarra A, Ruiz Postigo JA, Franco JR, Jannin JG (2011) The human African trypanosomiasis control and surveillance programme of the World Health Organization 2000–2009: the way forward. PLoS Negl Trop Dis 5: e1007 doi: 10.1371/journal.pntd.0001007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kagbadouno MS, Camara M, Rouamba J, Rayaisse JB, Traore IS, et al. (2012) Epidemiology of sleeping sickness in Boffa (Guinea): where are the trypanosomes? PLoS Negl Trop Dis 6: e1949 doi: 10.1371/journal.pntd.0001949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ilboudo H, Jamonneau V, Camara M, Camara O, Dama E, et al. (2011) Diversity of response to Trypanosoma brucei gambiense infections in the Forecariah mangrove focus (Guinea): perspectives for a better control of sleeping sickness. Microbes Infect 13: 943–952. doi: 10.1016/j.micinf.2011.05.007 [DOI] [PubMed] [Google Scholar]
- 5.Checchi F, Filipe JA, Barrett MP, Chandramohan D (2008) The natural progression of Gambiense sleeping sickness: what is the evidence? PLoS Negl Trop Dis 2: e303 doi: 10.1371/journal.pntd.0000303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jamonneau V, Ilboudo H, Kabore J, Kaba D, Koffi M, et al. (2012) Untreated human infections by Trypanosoma brucei gambiense are not 100% fatal. PLoS Negl Trop Dis 6: e1691 doi: 10.1371/journal.pntd.0001691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bucheton B, MacLeod A, Jamonneau V (2011) Human host determinants influencing the outcome of Trypanosoma brucei gambiense infections. Parasite Immunol 33: 438–447. doi: 10.1111/j.1365-3024.2011.01287.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garcia A, Courtin D, Solano P, Koffi M, Jamonneau V (2006) Human African trypanosomiasis: connecting parasite and host genetics. Trends Parasitol 22: 405–409. doi: 10.1016/j.pt.2006.06.011 [DOI] [PubMed] [Google Scholar]
- 9.Checchi F, Filipe JA, Haydon DT, Chandramohan D, Chappuis F (2008) Estimates of the duration of the early and late stage of gambiense sleeping sickness. BMC Infect Dis 8: 16 doi: 10.1186/1471-2334-8-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sternberg JM, Maclean L (2010) A spectrum of disease in human African trypanosomiasis: the host and parasite genetics of virulence. Parasitology 137: 2007–2015. doi: 10.1017/S0031182010000946 [DOI] [PubMed] [Google Scholar]
- 11.Jamonneau V, Ravel S, Garcia A, Koffi M, Truc P, et al. (2004) Characterization of Trypanosoma brucei s.l. infecting asymptomatic sleeping-sickness patients in Côte d'Ivoire: a new genetic group? Ann Trop Med Parasitol 98: 329–337. doi: 10.1179/000349804225003406 [DOI] [PubMed] [Google Scholar]
- 12.Jamonneau V, Garcia A, Ravel S, Cuny G, Oury B, et al. (2002) Genetic characterization of Trypanosoma brucei gambiense and clinical evolution of human African trypanosomiasis in Cote d'Ivoire. Trop Med Int Health 7: 610–621. [DOI] [PubMed] [Google Scholar]
- 13.Iraqi F, Clapcott SJ, Kumari P, Haley CS, Kemp SJ, et al. (2000) Fine mapping of trypanosomiasis resistance loci in murine advanced intercross lines. Mamm Genome 11: 645–648. [DOI] [PubMed] [Google Scholar]
- 14.Kemp SJ, Iraqi F, Darvasi A, Soller M, Teale AJ (1997) Localization of genes controlling resistance to trypanosomiasis in mice. Nat Genet 16: 194–196. doi: 10.1038/ng0697-194 [DOI] [PubMed] [Google Scholar]
- 15.Courtin D, Argiro L, Jamonneau V, N'Dri L, N'Guessan P, et al. (2006) Interest of tumor necrosis factor-alpha -308 G/A and interleukin-10–592 C/A polymorphisms in human African trypanosomiasis. Infect Genet Evol 6: 123–129. doi: 10.1016/j.meegid.2005.03.002 [DOI] [PubMed] [Google Scholar]
- 16.Courtin D, Milet J, Jamonneau V, Yeminanga CS, Kumeso VK, et al. (2007) Association between human African trypanosomiasis and the IL6 gene in a Congolese population. Infect Genet Evol 7: 60–68. doi: 10.1016/j.meegid.2006.04.001 [DOI] [PubMed] [Google Scholar]
- 17.Ilboudo H, Bras-Goncalves R, Camara M, Flori L, Camara O, et al. (2014) Unravelling human trypanotolerance: IL8 is associated with infection control whereas IL10 and TNFalpha are associated with subsequent disease development. PLoS Pathog 10: e1004469 doi: 10.1371/journal.ppat.1004469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Courtin D, Milet J, Sabbagh A, Massaro JD, Castelli EC, et al. (2013) HLA-G 3' UTR-2 haplotype is associated with Human African trypanosomiasis susceptibility. Infect Genet Evol 17: 1–7. doi: 10.1016/j.meegid.2013.03.004 [DOI] [PubMed] [Google Scholar]
- 19.Ilboudo H, Jamonneau V, Koffi M, Kabore J, Amoussa R, et al. (2016) Trypanosome-induced Interferon-gamma production in whole blood stimulation assays is associated with latent Trypanosoma brucei gambiense infections. Microbes Infect 18: 436–440. doi: 10.1016/j.micinf.2016.03.002 [DOI] [PubMed] [Google Scholar]
- 20.Cooper A, Ilboudo H, Alibu VP, Ravel S, Enyaru J, et al. (2017) APOL1 renal risk variants have contrasting resistance and susceptibility associations with African trypanosomiasis renal risk variants have contrasting resistance and susceptibility associations with African trypanosomiasis. Elife 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ilboudo H, Noyes H, Mulindwa J, Kimuda MP, Koffi M, et al. (2017) Introducing the TrypanoGEN biobank: A valuable resource for the elimination of human African trypanosomiasis. PLoS Negl Trop Dis 11: e0005438 doi: 10.1371/journal.pntd.0005438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Camara M, Camara O, Ilboudo H, Sakande H, Kabore J, et al. (2010) Sleeping sickness diagnosis: use of buffy coats improves the sensitivity of the mini anion exchange centrifugation test. Trop Med Int Health 15: 796–799. doi: 10.1111/j.1365-3156.2010.02546.x [DOI] [PubMed] [Google Scholar]
- 23.Van Meirvenne N, Magnus E, Buscher P (1995) Evaluation of variant specific trypanolysis tests for serodiagnosis of human infections with Trypanosoma brucei gambiense. Acta Trop 60: 189–199. [DOI] [PubMed] [Google Scholar]
- 24.Zhao JH (December 2007) Genetic Analysis Package. Journal of Statistical Software 23: 1–18. [Google Scholar]
- 25.Semagn K, Babu R, Hearne S, Olsen M (2014) Single nucleotide polymorphism genotyping using Kompetitive Allele Specific PCR (KASP): overview of the technology and its application in crop improvement. Molecular Breeding 33: 1–14. [Google Scholar]
- 26.Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, et al. (2007) PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet 81: 559–575. doi: 10.1086/519795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anderson CA, Pettersson FH, Clarke GM, Cardon LR, Morris AP, et al. (2010) Data quality control in genetic case-control association studies. Nat Protoc 5: 1564–1573. doi: 10.1038/nprot.2010.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Genovese G, Friedman DJ, Ross MD, Lecordier L, Uzureau P, et al. (2010) Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science 329: 841–845. doi: 10.1126/science.1193032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Perez-Morga D, Vanhollebeke B, Paturiaux-Hanocq F, Nolan DP, Lins L, et al. (2005) Apolipoprotein L-I promotes trypanosome lysis by forming pores in lysosomal membranes. Science 309: 469–472. doi: 10.1126/science.1114566 [DOI] [PubMed] [Google Scholar]
- 30.Vanhamme L, Paturiaux-Hanocq F, Poelvoorde P, Nolan DP, Lins L, et al. (2003) Apolipoprotein L-I is the trypanosome lytic factor of human serum. Nature 422: 83–87. doi: 10.1038/nature01461 [DOI] [PubMed] [Google Scholar]
- 31.Vanwalleghem G, Fontaine F, Lecordier L, Tebabi P, Klewe K, et al. (2015) Coupling of lysosomal and mitochondrial membrane permeabilization in trypanolysis by APOL1. Nat Commun 6: 8078 doi: 10.1038/ncomms9078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ilboudo H, Berthier D, Camara M, Camara O, Kabore J, et al. (2012) APOL1 expression is induced by Trypanosoma brucei gambiense infection but is not associated with differential susceptibility to sleeping sickness. Infect Genet Evol 12: 1519–1523. doi: 10.1016/j.meegid.2012.05.010 [DOI] [PubMed] [Google Scholar]
- 33.Vanhollebeke B, Pays E (2010) The trypanolytic factor of human serum: many ways to enter the parasite, a single way to kill. Mol Microbiol 76: 806–814. doi: 10.1111/j.1365-2958.2010.07156.x [DOI] [PubMed] [Google Scholar]
- 34.Cuypers B, Lecordier L, Meehan CJ, Van den Broeck F, Imamura H, et al. (2016) Apolipoprotein L1 Variant Associated with Increased Susceptibility to Trypanosome Infection. MBio 7: e02198–02115. doi: 10.1128/mBio.02198-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pays E (2006) The variant surface glycoprotein as a tool for adaptation in African trypanosomes. Microbes Infect 8: 930–937. doi: 10.1016/j.micinf.2005.10.002 [DOI] [PubMed] [Google Scholar]
- 36.Kieft R, Capewell P, Turner CMR, Veitch NJ, MacLeod A, et al. (2010) Mechanism of Trypanosoma brucei gambiense (group 1) resistance to human trypanosome lytic factor. Proc Natl Acad Sci U S A 107: 16137–16141. doi: 10.1073/pnas.1007074107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lecordier L, Vanhollebeke B, Poelvoorde P, Tebabi P, Paturiaux-Hanocq F, et al. (2009) C-terminal mutants of apolipoprotein L-I efficiently kill both Trypanosoma brucei brucei and Trypanosoma brucei rhodesiense. PLoS Pathog 5: e1000685 doi: 10.1371/journal.ppat.1000685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Consortium TG (2015) The Genotype-Tissue Expression (GTEx) pilot analysis: Multitissue gene regulation in humans. Science (New York, NY) 348: 648–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim S, Yu NK, Kaang BK (2015) CTCF as a multifunctional protein in genome regulation and gene expression. Exp Mol Med 47: e166 doi: 10.1038/emm.2015.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Vries HE, Blom-Roosemalen MC, van Oosten M, de Boer AG, van Berkel TJ, et al. (1996) The influence of cytokines on the integrity of the blood-brain barrier in vitro. J Neuroimmunol 64: 37–43. [DOI] [PubMed] [Google Scholar]
- 41.Girard M, Giraud S, Courtioux B, Jauberteau-Marchan MO, Bouteille B (2005) Endothelial cell activation in the presence of African trypanosomes. Mol Biochem Parasitol 139: 41–49. doi: 10.1016/j.molbiopara.2004.09.008 [DOI] [PubMed] [Google Scholar]
- 42.Calandra T, Froidevaux C, Martin C, Roger T (2003) Macrophage migration inhibitory factor and host innate immune defenses against bacterial sepsis. J Infect Dis 187 Suppl 2: S385–390. [DOI] [PubMed] [Google Scholar]
- 43.Renner P, Roger T, Calandra T (2005) Macrophage migration inhibitory factor: gene polymorphisms and susceptibility to inflammatory diseases. Clin Infect Dis 41 Suppl 7: S513–519. [DOI] [PubMed] [Google Scholar]
- 44.de Jesus Fernandes Covas C, Cardoso CC, Gomes-Silva A, Santos Oliveira JR, Da-Cruz AM, et al. (2013) Candidate gene case-control and functional study shows macrophage inhibitory factor (MIF) polymorphism is associated with cutaneous leishmaniasis. Cytokine 61: 168–172. doi: 10.1016/j.cyto.2012.09.012 [DOI] [PubMed] [Google Scholar]
- 45.Stijlemans B, Leng L, Brys L, Sparkes A, Vansintjan L, et al. (2014) MIF contributes to Trypanosoma brucei associated immunopathogenicity development. PLoS Pathog 10: e1004414 doi: 10.1371/journal.ppat.1004414 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Genome data has been deposited at the European Genome-phenome Archive (EGA, http://www.ebi.ac.uk/ega/) which is hosted at the EBI, under accession number EGAS00001002602.