Abstract
Natural killer/T-cell lymphomas are extremely rare and carry high mortality rates. Epidemiologically, these cancers tend to affect mainly Asian and South American patients and are associated with Epstein-Barr virus seropositivity. This report details a 78-year-old Vietnamese woman who presented initially with vitritis of unknown cause, but later developed proptosis and conjunctival involvement as her disease spread. Biopsies of the orbit, ethmoid sinus, and conjunctiva were found to be significant for natural killer/T-cell lymphoma. The case highlights the diagnostic difficulty of this tumor given its rarity and ability to mimic other disorders.
Most lymphomas involving the orbit and globe are non-Hodgkin's B-cell lymphomas (1). Only about 2% of intraocular lymphomas are non–B-cell tumors, and those expressing natural killer (NK) cell markers are typically highly aggressive and carry a poor prognosis (2). Since they arise primarily from the nasal mucosa, NK/T-cell lymphomas have the ability to invade the orbit and globe (2). Herein we present a case of NK/T-cell lymphoma in a 78-year-old Vietnamese woman who initially presented with vision problems and was successfully treated with chemotherapy.
CASE REPORT
A 78-year-old Vietnamese woman with a past medical history of coronary artery disease, hyperlipidemia, and hypothyroidism presented with a 6-month history of blurred vision in the left eye associated with sporadic pressure-like pain in that eye. On exam, vision in the left eye was 20/50, and there was no improvement with pinhole testing. Her intraocular pressure in the left eye was 10 mm Hg. The patient demonstrated mild vitritis and periphlebitis with vascular sheathing in the temporal periphery on the left. She also manifested a pigmented chorioretinal scar in the superonasal periphery of the same eye. The remainder of the exam, including pupils and extraocular movements, was normal.
The patient was initially diagnosed with uveitis and treated with a dexamethasone intravitreal implant; however, she developed recurrence of symptoms after implant dissolution. Serologic workup was performed that included tests for antineutrophil cytoplasmic antibody, toxoplasma IgM and IgG, rapid plasma reagin, QuantiFERON tuberculosis, and Lyme antibodies, all of which were negative. The patient also demonstrated a normal erythrocyte sedimentation rate, C-reactive protein level, and angiotensin-converting enzyme level. Magnetic resonance imaging with contrast demonstrated a metallic foreign body in the preseptal upper lid but was otherwise unremarkable and notably negative for any mass lesions, including central nervous system lymphoma, and an anterior chamber paracentesis failed to yield diagnostic results.
Two months later, the patient returned with an inflamed salmon-colored lesion within the medial conjunctiva of the left eye and markedly decreased visual acuity on the left to 20/200. Examination demonstrated supra-, infra-, and abduction deficits on the left with mechanical ptosis, as well as 5 mm of proptosis and mild resistance to retropulsion.
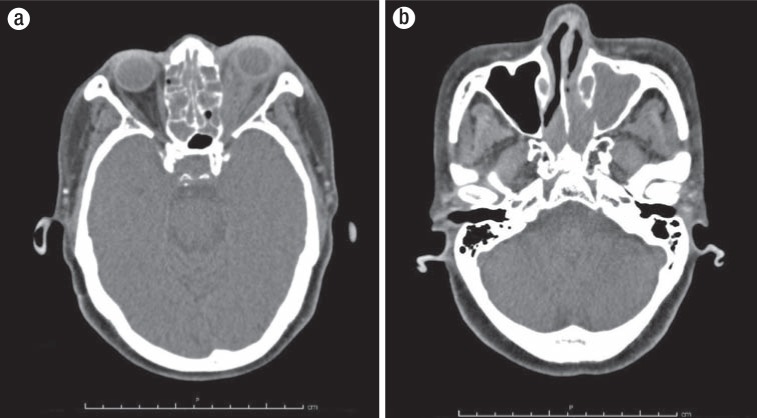
Due to the presence of a metallic foreign body, a contrast-enhanced computed tomography (CT) scan of the head was substituted for magnetic resonance imaging. This scan demonstrated extensive opacification of the left maxillary and ethmoid sinuses, as well as an invasive pattern of hyperdense material filling the majority of the left intraconal space, which extended anteriorly, causing protrusion of the subcutaneous tissue of the inferior eyelid (Figure 1).
Figure 1.
A CT scan taken after the development of left-sided proptosis shows (a) hyperdense material filling the left intraconal space and protruding into the inferior eyelid and (b) prominent maxillary and ethmoid sinus opacification.
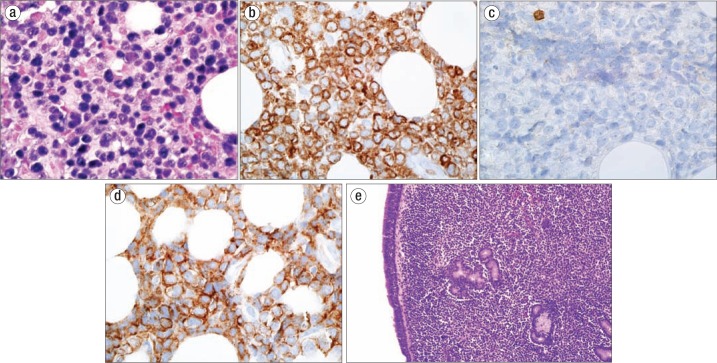
The patient underwent orbitotomy with biopsy of the abnormal tissue in the left orbit and ethmoid sinus as well as a conjunctival biopsy. Pathology results revealed intermediate- to large-sized neoplastic CD2+, CD56+, CD5+ lymphoid cells, highlighting an atypical prominent population of true NK cells (Figure 2). In situ hybridization for Epstein-Barr virus was strongly and diffusely positive in neoplastic cells. The diagnosis of extranodal NK/T-cell lymphoma nasal type was made, and the patient underwent tumor staging. A positron emission tomography (PET) scan demonstrated extensive metabolically active disease, indicating a stage IVA diagnosis. The patient received three of six planned cycles of gemcitabine, oxaliplatin, and L-asparaginase (GELOX) chemotherapy. Her therapy was suspended due to severe treatment-induced debilitation; however, she remains in complete remission by both CT and PET scan as of her most recent follow-up 10 months following her initial oncologic consultation.
Figure 2.
Pathology results confirming the diagnosis of natural killer/T-cell lymphoma: (a) in situ hybridization for Epstein Barr virus on orbital tissue showing intermediate- to large-sized neoplastic cells with nuclear irregularities that stain strongly positive (1000×); (b) CD3 immunohistochemical stain of orbital tissue (1000×); (c) CD5 immunohistochemical stain of orbital tissue (1000×); (d) CD56 immunohistochemical stain of orbital tissue (1000×); (e) sinonasal mucosa with an abnormal lymphoid infiltrate displaying some nuclear irregularity underlying normal respiratory epithelium (200×).
DISCUSSION
NK/T-cell lymphoma is a rare and aggressive subtype most common in Asian and South American populations and associated with EBV (3). While most ocular and orbital lymphomas are of the non-Hodgkin's B-cell variety, the nasal type NK/T-cell lymphoma does occasionally invade the globe or ocular adnexa and represents approximately 1% to 3% of all lymphoproliferative lesions in these locations (4). Over 70% of these cancers localize to the nasopharynx with inflammation and local tissue destruction (5); however, angioinvasion allows widespread dissemination to the gastrointestinal tract (6), skin (7), and central nervous system (8). A recent review that included 24 patients with primary nasal or nasopharyngeal NK/T-cell lymphoma identified six patients (25% of the study population) who suffered vision-threatening complications that stemmed from uveitis/vitritis and/or orbital inflammation (5). Intraocular and orbital presentations of the malignancy have been confused with a range of diagnoses, including orbital cellulitis (9, 10), nonspecific orbital inflammation (6), conjunctivitis, anterior uveitis, and optic neuritis (11).
The prognosis of extranodal NK/T-cell lymphomas is worse than that of their B-cell counterparts (12). While early stage, localized disease is highly curable, metastatic disease and refractory cases carry a 5-year survival rate of <10% (13). Treatment for localized disease (stage I/II) includes chemotherapy and radiotherapy; however, disseminated disease is treated with combination chemotherapy (14). Furthermore, expression of P-glycoprotein (an active drug-export mechanism) on NK/T-cell lymphoma cells confers multidrug resistance (15), so regimens such as cyclophosphamide, doxorubicin, vincristine, and prednisolone have largely been replaced with methotrexate- and ifosfamide-containing regimens (16). L-asparaginase is another crucial component of the chemotherapeutic regimen, and phase II studies of dexamethasone, methotrexate, ifosfamide, etoposide, and L-asparaginase (SMILE) therapy have shown 1-year overall survival and progression-free survival rates of 45% and 45%, respectively (17). This patient was treated with GELOX, which in one prospective study showed a 2-year overall survival rate of 86% and a progression-free survival rate of 86%, with a local relapse rate of 15% and systemic relapse rate of 11% (18).
It is important to consider the diagnosis of NK/T-cell lymphoma in patients complaining of orbital swelling, especially those with concomitant findings of ocular inflammation or other systemic complaints. Orbital biopsy should be considered in cases of chronic uveitis with nondiagnostic vitreous biopsy and orbital imaging findings. When diagnosed early, treatment with radio- and chemotherapy can be effective for regional sino-orbital NK/T-cell lymphoma.
References
- 1.Choi KH, Lee SJ, Suh YL, Kim YD. Nasal-type natural killer/T-cell lymphoma of the orbit. J Korean Ophthalmol Soc. 2004;45:2145–2150. [Google Scholar]
- 2.Cimino L, Chan C-C, Shen D, Masini L, Ilariucci F, Masetti M, Asioli S, Sartori A, Cappuccini L. Ocular involvement in nasal natural killer T-cell lymphoma. Int Ophthalmol. 2009;29(4):275–279. doi: 10.1007/s10792-008-9220-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aozasa K, Zaki MA. Epidemiology and pathogenesis of nasal NK/T-cell lymphoma: a mini-review. Sci World J. 2011;11:422–428. doi: 10.1100/tsw.2011.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coupland SE, Foss HD, Assaf C, Auw-Haedrich C, Anastassiou G, Anagnostopoulos I, Hummel M, Karesh JW, Lee WR, Stein H. T-cell and T/natural killer-cell lymphomas involving ocular and ocular adnexal tissues: a clinicopathologic, immunohistochemical, and molecular study of seven cases. Ophthalmology. 1999;106(11):2109–2120. doi: 10.1016/S0161-6420(99)90492-X. [DOI] [PubMed] [Google Scholar]
- 5.Hon C, Kwok AK, Shek TW, Chim JC, Au WY. Vision-threatening complications of nasal T/NK lymphoma. Am J Ophthalmol. 2002;134(3):406–410. doi: 10.1016/s0002-9394(02)01520-9. [DOI] [PubMed] [Google Scholar]
- 6.Mo ZY, Wang P, Yang HW, Li WB, Liang QL. Esophageal metastasis secondary to extranodal nasal-type natural killer/T-cell lymphoma: a case report. Mol Clin Oncol. 2016;5(1):207–209. doi: 10.3892/mco.2016.861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sandner A, Helmbold P, Winkler M, Gattenlöhner S, Müller-Hermelink H-K, Holzhausen HJ. Cutaneous dissemination of nasal NK/T-cell lymphoma in a young girl. Clin Exp Dermatol. 2008;33(5):615–618. doi: 10.1111/j.1365-2230.2008.02777.x. [DOI] [PubMed] [Google Scholar]
- 8.Romero-Guadarrama MB, Aguilar-Martínez E. Extranodal nasal NK/T-cell lymphoma with dissemination to the central nervous system: a case report. Acta Cytol. 2010;54(5 Suppl):993–997. [PubMed] [Google Scholar]
- 9.Kim JW, An JH. Extranodal natural killer/T-cell lymphoma, nasal type, of the orbit mimicking recurrent orbital cellulitis. J Craniofac Surg. 2014;25(2):509–511. doi: 10.1097/SCS.0000000000000677. [DOI] [PubMed] [Google Scholar]
- 10.Ely A, Evans J, Sundstrom JM, Malysz J, Specht CS, Wilkinson M. Orbital involvement in extranodal natural killer T cell lymphoma: an atypical case presentation and review of the literature. Orbit. 2012;31(4):267–269. doi: 10.3109/01676830.2011.605506. [DOI] [PubMed] [Google Scholar]
- 11.Abe RY, Pinto RDP, Bonfitto JFL, Lira RPC, Arieta CEL. Ocular masquerade syndrome associated with extranodal nasal natural killer/T-cell lymphoma: case report. Arq Bras Oftalmol. 2012;75(6):430–432. doi: 10.1590/s0004-27492012000600013. [DOI] [PubMed] [Google Scholar]
- 12.Cheung MM, Chan JK, Lau WH, Foo W, Chan PT, Ng CS, Ngan RK. Primary non-Hodgkin's lymphoma of the nose and nasopharynx: clinical features, tumor immunophenotype, and treatment outcome in 113 patients. J Clin Oncol. 1998;16(1):70–77. doi: 10.1200/JCO.1998.16.1.70. [DOI] [PubMed] [Google Scholar]
- 13.Au WY. Current management of nasal NK/T-cell lymphoma. Oncology (Williston Park) 2010;24(4):352–328. [PubMed] [Google Scholar]
- 14.Tse E, Kwong YL. Diagnosis and management of extranodal NK/T cell lymphoma nasal type. Expert Rev Hematol. 2016;9(9):861–871. doi: 10.1080/17474086.2016.1206465. [DOI] [PubMed] [Google Scholar]
- 15.Yamaguchi M, Kita K, Miwa H, Mishii K, Oka K, Ohno T, Shirakawa S, Fukumoto M. Frequent expression of P-glycoprotein/MDR1 by nasal T-cell lymphoma cells. Cancer. 1995;76(11):2351–2356. doi: 10.1002/1097-0142(19951201)76:11<2351::aid-cncr2820761125>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 16.Tse E, Kwong YL. Management of advanced NK/T-cell lymphoma. Curr Hematol Malig Rep. 2014;9(3):233–242. doi: 10.1007/s11899-014-0216-3. [DOI] [PubMed] [Google Scholar]
- 17.Yamaguchi M, Kwong YL, Kim WS, Maeda Y, Hashimoto C, Suh C, Izutsu K, Ishida F, Isobe Y, Sueoka E, Suzumiya J, Kodama T, Kimura H, Hyo R, Nakamura S, Oshimi K, Suzuki R. Phase II study of SMILE chemotherapy for newly diagnosed stage IV, relapsed, or refractory extranodal natural killer (NK)/T-cell lymphoma, nasal type: the NK-Cell Tumor Study Group study. J Clin Oncol. 2011;29(33):4410–4416. doi: 10.1200/JCO.2011.35.6287. [DOI] [PubMed] [Google Scholar]
- 18.Wang L, Wang ZH, Chen XQ, Li YJ, Wang KF, Xia YF, Xia ZJ. First-line combination of gemcitabine, oxaliplatin, and L-asparaginase (GELOX) followed by involved-field radiation therapy for patients with stage IE/IIE extranodal natural killer/T-cell lymphoma. Cancer. 2013;119(2):348–355. doi: 10.1002/cncr.27752. [DOI] [PubMed] [Google Scholar]