Abstract
Heerfordt-Waldenström syndrome is a rare subacute variant of sarcoidosis, characterized by enlargement of the parotid or salivary glands, facial nerve paralysis and anterior uveitis. Granulomas with a peripheral lymphocyte deficit are found in the anatomic pathology of affected organs. It is normally self-limiting, with cure achieved between 12 and 36 months, but some prolonged cases have been reported. Diagnosis of the syndrome is clinical, and treatment depends on the degree of systemic impairment. Oral corticosteroids represent the first line treatment option. The mortality rate ranges between 1 and 5% of cases.
Keywords: Uveoparotid fever, Parotid gland, Facial Paralysis, Sarcoidosis, Uveitis
CASE REPORT
A 36-year-old female patient reported having right peripheral facial paralysis, with no apparent cause. She was treated with prednisone (40 mg/day) until clinical improvement occurred. One year later, left peripheral facial paralysis was diagnosed, and the previous treatment was successfully instituted. After three months, the patient developed a cough, chest pain and dyspnea and was admitted for investigation. Chest tomography revealed a large number of small bilateral parenchymal nodules and intense mediastinal adenomegaly. During this period, bilateral uveitis appeared, along with erythematous papules on the back, cervical region and face, which had the appearance of apple jelly on diascopy (Figures 1 and 2). A biopsy of the facial lesion was performed, and the histopathology results revealed sarcoid granulomas on the dermis (Figure 3). Tests for fungal and alcohol acid-fast bacilli were negative. The dermatology team opted for treatment with methotrexate (10mg/week) and prednisone (20mg/day), which resulted in clinical improvement.
Figure 1.

Papule on the forehead, with a translucent appearance and red-brownish color
Figure 2.

Conjunctival hyperemia secondary to uveitis
Figure 3.
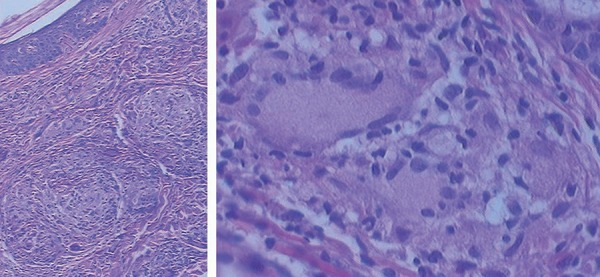
Sarcoidal granulomas on the dermis (left photo, hematoxylin and eosin, X100). Presence of multinucleated cells in the granuloma (right photo, hematoxylin and eosin, X400)
DISCUSSION
Heerfordt-Waldenström syndrome (HWS) is a rare subacute variant of sarcoidosis, characterized by enlargement of the parotid glands, facial nerve paralysis and anterior uveitis.1,2 When two of its symptoms occur, it is considered incomplete HWS.3 The disease was first described in 1909 by Heerfordt and Waldenström, and its association with sarcoidosis was noted in 1937.4,5
In approximately 6% of sarcoidosis cases, parotid gland enlargement occurs, which is caused by a granulomatous inflammatory reaction.3,4 Nervous system impairment occurs in 5% of patients, and facial nerve paralysis due to epineural and perineural granulomas is the most common manifestation.3,4
Anterior uveitis is a classic ocular manifestation, especially in African-Americans (70% to 75%), and includes photophobia, blurred vision and tearing. Posterior uveitis is more frequent in Caucasians (65% to 83%).1 Asymptomatic conjunctival nodules, representing epithelioid granulomas, may be present.4,6
A study of 1,000 sarcoidosis patients showed a significant correlation between the HLA-DRB1*04 allele and HWS. Three patients had the full form, 13 had the incomplete form, and all had uveitis.1
The diagnosis of HWS is clinical.4 The lesion's anatomic pathology includes so-called "naked granulomas", an expression coined because they are surrounded by few lymphocytes.6 These granulomas produce angiotensin-converting enzyme, but the levels do not always correlate with disease activity (10% false positives and 40% false negatives).4
Complementary test results include hypercalcemia, which results in the secretion of 1,25-dihydroxyvitamin D3 by the alveolar macrophages and occurs in up to 40% of cases.6 The Kveim-Siltzbach test is positive in up to 80% of acute forms, but its positivity decreases as disease duration increases.6
Treatment depends on the severity of systemic impairment. Oral corticosteroids represent the first line treatment option. Prednisone dosages of 20 to 40 mg/day (the dosage may be up to 80 mg/day in some cases) are prescribed over six to 12 months.6 Artificial tears are useful when facial paralysis with lagophthalmos is present. The likelihood of permanent paralysis increases in patients who are not treated with corticosteroids.4
The prognosis of sarcoidosis varies according to disease duration, severity and the organs affected. It is usually a self-limiting disease, with cure achieved within 12 to 36 months. Some prolonged cases have been reported. The mortality rate varies between 1% and 5%.6
Footnotes
Conflict of interest: none.
The work was conducted in the Hospital do Servidor Público Estadual de São Paulo - São Paulo (SP), Brazil.
Financial support: none.
REFERENCES
- 1.Darlington P, Tallstedt L, Padyukov L, Kockum I, Cederlund K, Eklund A, et al. HLA-DRB1 alleles and symptoms associated with Heerfordt's syndrome in sarcoidosis. Eur Respir J. 2011;38:1151–1157. doi: 10.1183/09031936.00025011. [DOI] [PubMed] [Google Scholar]
- 2.Fischer T, Filimonow S, Petersein J, Zimmer C, Beyersdorff D, Guski H. Diagnosis of Heerfordt's syndrome by state-of-the-art ultrasound in combination with parotid biopsy: a case report. Eur Radiol. 2002;12:134–137. doi: 10.1007/s003300100879. [DOI] [PubMed] [Google Scholar]
- 3.Yagi T, Hattori H, Ohira M, Nakamichi K, Takayama-Ito M, Saijo M, et al. Progressive multifocal leukoencephalopathy developed in incomplete Heerfordt syndrome, a rare manifestation of sarcoidosis, without steroid therapy responding to cidofovir. Clin Neurol Neurosurg. 2010;112:153–156. doi: 10.1016/j.clineuro.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Denny MC, Fotino AD. The Heerfordt-Waldenström syndrome as an initial presentation of sarcoidosis. Proc (Bayl Univ Med Cent) 2013;26:390–392. doi: 10.1080/08998280.2013.11929014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glocker FX, Seifert C, Lücking CH. Facial palsy in Heerfordt's syndrome: electrophysiological localization of the lesion. Muscle Nerve. 1999;22:1279–1282. doi: 10.1002/(sici)1097-4598(199909)22:9<1279::aid-mus18>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 6.Daldon PEC, Arruda LHF. Granulomas não-infecciosos: sarcoidose. An Bras Dermatol. 2007;82:559–571. [Google Scholar]


