Abstract
Objective
In 2015, the U.S. Preventive Services Task Force updated their hypertension recommendations to advise that adults with elevated office blood pressure (BP) undergo out-of-office BP measurement to exclude white-coat hypertension prior to diagnosis. Our goal was to determine the most important barriers to primary care providers’ ordering ambulatory and home BP monitoring in the U.S.
Methods
We enrolled 63 primary care providers into nominal group panels in which participants iteratively listed and ranked barriers to ambulatory and home BP monitoring.
Results
Top ranked barriers to ambulatory BP monitoring were challenges in accessing testing, costs of testing, concerns about the willingness or ability of patients to successfully complete tests, and concerns about the accuracy and benefits of testing. Top ranked barriers to home BP monitoring were concerns about compliance with the correct test protocol, accuracy of tests results, out-of-pocket costs of home BP devices, and time needed to instruct patients on home BP monitoring protocol.
Conclusions
Efforts to increase the use of ambulatory and home BP monitoring by primary care providers in the U.S. should prioritize increasing the financial and personnel resources available for testing and addressing provider concerns about patients’ ability to conduct high quality tests.
Keywords: hypertension, screening, ambulatory blood pressure monitoring, home blood pressure monitoring, implementation science
Introduction
In 2015, the U.S. Preventive Services Task Force (USPSTF) updated their hypertension screening recommendations to advise that patients with elevated office blood pressure (BP) undergo ambulatory (ABPM) or home blood pressure monitoring (HBPM) prior to hypertension diagnosis.1 Several other national and international societies have similarly recommended out-of-office BP testing prior to hypertension diagnosis.2–5 This recommendation is important because approximately one in five adults with elevated office BP has non-hypertensive BP when measured outside of the office setting, a phenomenon known as white-coat hypertension.6 The failure to exclude white-coat hypertension can lead to unnecessary antihypertensive medications, inappropriate labeling with a chronic health condition, and avoidable health care costs.7 Despite the growing consensus for out-of-office BP testing, studies suggest that it is infrequently obtained prior to hypertension diagnosis in U.S. primary care settings.8,9
Hypertension experts have expressed their opinions about barriers to out-of-office BP testing.10,11 Yet, to our knowledge, no one has yet surveyed U.S. primary care providers to learn their perceptions of the barriers to obtaining out-of-office BP testing. Understanding the perceptions of these providers is essential to developing interventions that increase the appropriate use of out-of-office BP testing in clinical practice.
In this study, our goal was to identify the most important barriers to out-of-office BP assessment from the primary care provider’s perspective. We secondarily aimed to compare barriers to ABPM and HBPM as some guidelines, including the one from the USPSTF, suggest that both approaches are acceptable for excluding white-coat hypertension.1,4,5 We surveyed primary care providers from two distinct areas in the U.S., New York City and the South, to learn whether the pattern of barriers varies by geographic region.
Methods
Design
To identify barriers to out-of-office BP testing, we enrolled primary care providers into nominal group panels.12–14 The nominal group technique is a semi-quantitative method in which panelists iteratively list and rank responses to a question, and is ideally suited to efficiently identifying barriers to guideline implementation.14–18 This technique has the advantage of obtaining multiple perspectives, ensuring equal participation throughout the group, prioritizing group cohesiveness, and facilitating interpretability of results. Primary care providers were selected as panelists as these are the providers most often screening patients for hypertension. The institutional review boards of the University of Alabama at Birmingham and Columbia University Medical Center approved this protocol.
Participants
Nominal group panels were comprised of convenience samples of primary care providers (general internists, family practitioners, and nurse practitioners) recruited between April 2015 and February 2016 from clinics in two geographic regions in the United States: Southern states (predominantly Alabama) and New York City. Providers from the South were recruited through emails to lists of primary care physicians affiliated with the Deep South Continuing Medical Education Network and Alabama Practice Based Research Network. Providers in New York City were recruited through emails to primary care providers affiliated with the Ambulatory Care Network of New York-Presbyterian Hospital and Mount Sinai Medical Center. Providers from the South were given an honorarium of $200 for their participation in the nominal groups, and providers from New York City received $150 for participating.
Data Collection
The nominal groups took place in “virtual” meeting rooms in which providers called into a conference line while being logged onto an internet-connected computer. After introductions, a group moderator reviewed the USPSTF recommendation for out-of-office BP testing as part of hypertension screening. To identify barriers to out-of-office BP testing, providers were told that the goal of the meeting was to understand the challenges primary care providers face in following this recommendation. They were then asked to take five minutes to silently generate answers to the following question: “From your perspective, as a clinician, what are the barriers you and others in your practice face in using ambulatory BP monitoring to exclude white-coat hypertension in your patients?” The moderator then solicited each panelist’s responses, generating a list visible to all providers via a shared website. Subsequent providers were encouraged to generate additional barriers until saturation of ideas was achieved. Providers then anonymously voted on-line for their top five barriers. Top votes were weighted the highest (5 points), and fifth votes the lowest (1 point). Providers then re-voted two additional times with the opportunity to comment and modify the list after each vote was tabulated. After the sessions, providers completed a brief survey assessing demographics, provider type, years in practice, and prior use of ABPM and HBPM. Nominal group sessions were continued until saturation of ideas was obtained for each region.
Data Analysis
Barriers were categorized according to the Theoretical Domains Framework (TDF).19 The TDF represents a synthesis of behavior change theories, and was designed to identify targets or theory-informed behavior change interventions.20 The TDF assesses barriers to behavior change in the following twelve domains: knowledge; cognitive skills; social/professional role and identity; environmental context and resources; social influences; emotion; behavioral regulation; nature of the behavior; capability beliefs; consequences beliefs; motivation and goals; and memory, attention, and decision processes (Table 1).21 In this case, the behavior of interest was the ordering out-of-office blood pressure testing by providers as part of hypertension screening. Two authors independently categorized barriers, and came together with a third author to achieve consensus when there were discrepancies. Capability and consequences beliefs were combined as coders found it challenging to determine which domain was better suited to categorizing concerns about patient compliance with testing. To compare the overall prevalence of barriers to ABPM and HBPM, votes per session were standardized by converting them into percentages.
Table 1.
Theoretical Domains and their Underlying Meaning in the Context of Providers Implementing a Recommended Evidence-Based Clinical Practice*
| Domain | General Description of Barriers within Domain |
|---|---|
| Knowledge | Lack knowledge about the evidence in support of the behavior and in how to implement it |
| Cognitive Skills | Insufficient training in techniques required to implement the guideline |
| Social/professional role and identity | Behavior is not viewed as ‘typical’ for their profession |
| Environmental context and resources | Insufficient time and material resources to do the behavior |
| Social influences | Lack positive social influences to do the behavior |
| Emotion | Doing the behavior is stressful |
| Behavioral regulation | Behavior requires planning and self-monitoring |
| Nature of the behaviors | Behavior is not automatic and requires a change in habit |
| Capability beliefs | Lack confidence in ability to successfully do the behavior |
| Consequence beliefs | Do not believe that the benefits of doing the behavior outweigh the costs |
| Motivation and goals | Lack motivation to do the behavior as behavior does not lead to external rewards or is not a priority compared with other goals |
| Memory, attention, and decision processes | Easy to forget the behavior, and reminders are not in place |
Theoretical domains were derived from Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. 2005;14(1):26–33.
Results
Participants
Twenty-one providers participated in New York (3 groups assessed barriers to ABPM and HBPM; 5, 6, and 10 providers per group), and 42 providers participated in the South (3 groups assessed barriers to ABPM and 3 separate groups assessed barriers to HBPM; 5 to 9 providers per group; 21 providers for ABPM sessions and 21 providers for HBPM sessions). Due in part to a delay in sending surveys to providers to the South, the survey response rate by providers in the South was 55%, whereas the survey response rate in New York was 95%.
Providers from the South were, on average, 10 years older and in practice 9 more years than providers in New York (Table 2). A higher proportion of providers in the South were men. Family practitioners were the most common provider type in the South (65%) whereas general internists were the most common in New York (75%). Few providers in either region (<5%) more than occasionally used ABPM to rule-out white coat hypertension. In contrast, 52% of providers in the South and 20% of providers in New York reported often or always using HBPM to exclude white-coat hypertension.
Table 2.
Characteristics of Primary Care Providers Participating in Nominal Groups*
| Characteristic | South (N= 23 of 42†) | New York (N=20 of 21†) |
|---|---|---|
|
| ||
| Age in years, mean (SD) | 52.9 (10.0) | 43.2 (13.2) |
| Sex | ||
| Female | 8 (34.8%) | 14 (70.0%) |
| Male | 15 (65.2%) | 4 (20.0%) |
| Other | 0 (0%) | 2 (10.0%) |
|
| ||
| Race | ||
| White | 15 (65.2%) | 13 (65.0%) |
| Black | 0 (0%) | 1 (5.0%) |
| Asian | 6 (26.1%) | 6 (30.0%) |
| Other | 2 (8.7%) | 0 (0%) |
|
| ||
| Provider type | ||
| General internist | 7 (30.4%) | 15 (75.0%) |
| Family practitioner | 15 (65.2%) | 0 (0%) |
| Nurse practitioner | 0 (0%) | 5 (25.0%) |
| Other | 1 (4.3%) | 0 (0%) |
|
| ||
| Years in practice, mean (SD) | 21.7 (11.1) years | 13.0 (12.5) years |
|
| ||
| Prior use of ABPM to rule-out white coat hypertension | ||
| Never | 14 (60.9%) | 15 (75.0%) |
| Occasionally | 7 (30.4%) | 5 (25.0%) |
| Often | 1 (4.3%) | 0 (0%) |
| Always | 1 (4.3%) | 0 (0%) |
|
| ||
| Prior use of HBPM to rule-out white coat hypertension | ||
| Never | 2 (8.6%) | 2 (10.0%) |
| Occasionally | 9 (39.1%) | 14 (70.0%) |
| Often | 8 (34.8%) | 4 (20.0%) |
| Always | 4 (17.4%) | 0 (0%) |
Data are presented as N(%) unless otherwise specified.
Characteristics were not collected from nineteen providers in the Southern groups and one provider in the New York groups.
Barriers to ABPM
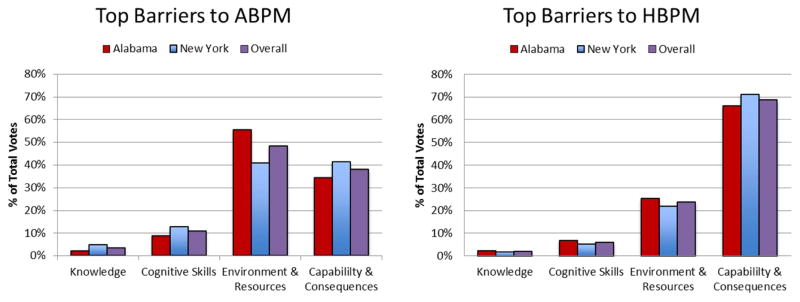
Barriers to ordering ABPM were present in five of the twelve TDF domains. As two domains were combined (capability and consequences beliefs), barriers are presented in four categories (Table 3). The top rated domain, accounting for 48.2% of votes, pertained to environmental resources and context (Figure 1). Barriers in this domain included out-of-pocket costs; challenges in securing insurance coverage for the test; costs of ABPM equipment; staff time to conduct the test; insufficient physician time to implement the ABPM protocol; and inaccessibility of ABPM. The domains that received the second most votes (37.9%) pertained to providers’ beliefs about their capability and beliefs about the consequences of obtaining ABPM data. Providers expressed concerns about patient willingness or ability to comply with the ABPM test protocol due to the discomfort of the procedure, complexity of programming the device in the event of device malfunctions, and the requirement for patients to return the device for data extraction. Providers also expressed concerns that even when testing was completed, the data might be invalid due to patients’ incorrectly following the protocol (e.g., monitoring on the wrong day) or issues with the ABPM device (e.g., using a non-validated ABPM device). Some providers also questioned whether ABPM was superior to office measurement or HBPM. Barriers to ABPM within the cognitive skills domain accounted for 10.7% of votes. In particular, providers identified a need for skills training in how to conduct ABPM, interpret ABPM results, and explain results to patients. Barriers related to the knowledge domain accounted for 3.3% of votes, with a few providers expressing concerns about insufficient knowledge of the recommendations for out-of-office BP testing.
Table 3.
Barriers to Ambulatory Blood Pressure Monitoring Grouped by Domains in the Theoretical Domains Framework
| Domain | Percent of Votes | Top Ranked Barriers |
|---|---|---|
| Environmental context and resources | 48.2% |
|
| Beliefs about capability and beliefs about consequences | 37.9% |
|
| Cognitive Skills | 10.7% |
|
| Knowledge | 3.3% |
|
Figure 1.
Barriers to HBPM
The top voted domain (68.5% of votes) for barriers to HBPM pertained to capability and consequences beliefs (Table 4). Barriers relevant to this combined domain pertained to concerns that patients would be unwilling to conduct HBPM due to the intrusiveness and intensity of the HBPM protocol. There were also concerns that patients would incorrectly follow the HBPM protocol due to low health literacy, use of incorrect BP cuff sizes or cuff positioning, non-validated devices, selective recording of desirable BP values, and forgetting to return BP logs. Providers also were concerned patients would record non-representative BP readings (e.g., moments of heightened anxiety or when feeling ill). HBPM barriers related to the environmental context received 23.5% of votes. Within this domain, providers cited costs of home BP devices as well as costs to providers in terms of unreimbursed time for training patients in the HBPM protocol and reviewing test results. Concerns about insufficient cognitive skills received 6% of votes, and pertained to a need for skills in teaching patients the HBPM protocol and analyzing HBPM data. Concerns about insufficient knowledge received 2% of votes.
Table 4.
Barriers to Home Blood Pressure Monitoring Grouped by Domains in the Theoretical Domains Framework
| Domain | Percent of Votes | Top ranked barriers |
|---|---|---|
| Beliefs about capability and consequences | 68.5% |
|
| Environmental context and resources | 23.5% |
|
| Cognitive Skills | 6.0% |
|
| Knowledge | 2.0% |
|
Comparison of Barriers to ABPM and HBPM
Barriers to ABPM and HBPM were present within the same five TDF domains. One major difference was that barriers relevant to environmental context received the highest number of votes for ABPM (48.2%) whereas barriers relevant to beliefs about capability and consequences received the highest number of votes for HBPM (68.5%). Barriers relevant to knowledge and cognitive skills, combined, received a small percentage of votes for ABPM and HBPM (14.0% and 8.0%, respectively).
Comparison of Barriers by Geographic Region
The pattern of barriers to ABPM and HBPM was similar for providers in both regions. One difference is that, for ABPM, providers in the South gave the environmental context a higher percentage of votes (55.4%) than beliefs about capabilities and consequences (34.3%) whereas providers in New York gave a similar number of votes to each of these top two domains (40.9% and 41.5%, respectively).
Discussion
In the current study of primary care providers, the most important barriers to ordering ABPM were related to costs in terms of time, infrastructure, and out-of-pocket expenses, and to inaccessibility of ABPM testing centers. The most important barriers to HBPM related to concerns that patients would not comply with the testing protocol, raising concerns about the validity of HBPM test results. Concerns about insufficient provider skills or knowledge were also ranked for ABPM and HBPM, but these were of secondary importance.
There have been few prior studies assessing barriers to HBPM from the ordering providers’ perspective. The majority of these examined barriers in the setting of hypertension self-management, but not diagnosis.22–26 In a recent survey of providers in the Pacific Northwest, the most important barriers to HBPM as part of hypertension self-management related to affordability of devices, accuracy of BP readings, and technical skill requirements, particularly in older patients.27 A survey of providers in Canada about HBPM identified concerns about the validity of HBPM data and concerns that HBPM would lead patients to become overly preoccupied with BP.23 While concerns about patient anxiety surrounding HBPM testing emerged as a barrier in the current survey, it received only a moderate number of votes, perhaps because these were less important in the context of one-time diagnostic testing.
Few studies have assessed barriers to ordering ABPM from the primary care provider’s perspective. Consistent with the our findings, a survey of 160 primary care providers in Ireland identified low reimbursement, cost, and lack of time as limiting use of ABPM as part of hypertension diagnosis.28 In contrast, accessibility and concerns about patients’ ability to complete testing were not identified as barriers to ABPM in Ireland. This may be due to the fact that ABPM had been recommended by European guidelines for a longer time, ABPM testing centers were more widely available, and providers may have had more success with ABPM.
The use of a theoretical framework to categorize barriers enabled us to consider theory-derived interventions that could be tested to increase out-of-office testing.20 Implementation scientists have linked the barriers identified by the TDF with evidence-based behavior change strategies (e.g., education, persuasion, incentivization, enablement, modeling, environmental restructuring) and policy recommendations that can increase the adoption of evidence-based recommendations.29–31 Policy changes that increase incentives for out-of-office testing may be needed, especially for ABPM which is not currently accessible to many primary care providers in the U.S. To overcome provider concerns about insufficient time to teach patients how to conduct HBPM, allied health professionals could be trained to teach patients. Barriers related to beliefs about capabilities and consequences could be targeted through persuasion by prominent primary care providers using case-based curricula including grand rounds or continuing medical education presentations. These barriers might also be addressed by educating providers about the high rate of successful completion of ABPM when available, and on the substantial evidence in support of out-of-office testing. Barriers related to knowledge of the recent USPSTF recommendations and how to order ABPM testing could be overcome by decision support tools embedded in the electronic health record that prompt providers to recall the guidelines and facilitate test ordering.32
Our provider survey demonstrated that ABPM was infrequently obtained, suggesting that the ordering of ABPM represents a change in the usual practice of diagnosing hypertension for many providers. Thus, we expected that the need for providers to establish a new routine in clinical practice would have been nominated as an important barrier to conducting ABPM, at least until ABPM become part of the routine, automatic thought process of primary care providers during hypertension screening.33 Yet, none of the providers identified this as an important barrier. Future studies should explicitly ask providers about this potential barrier as unique interventions such as computerized clinical decision support tools that match patient-specific information (e.g., elevated office BP) to evidence-based knowledge in real-time (e.g., in-visit recommendation to order out-of-office BP testing) may be helpful should this barrier be present.34–36
There were several strengths of the approach used in the current study. We used an evidence-based theoretical framework to organize barriers. The inclusion of providers from two regions in the U.S. enhanced the generalizability of the findings. The use of the nominal group technique allowed for a semi-quantitative understanding of the relative importance of groups of barriers. There were also limitations. We did not systematically assess each of the domains in the TDF and may have missed opportunities to identify important barriers. We did not assess provider preferences for ABPM versus HBPM, and thus cannot infer which form of testing has more barriers. We enrolled a convenient sample of primary care providers, and the representativeness of their perspectives is unknown. We were missing responses on provider characteristics, and any attribution of differences in barriers by provider type or region must be made with caution. As providers in the two regions ranked barriers similarly, however, these barriers may be broadly representative.
In conclusion, we identified several major barriers to increasing the use of ABPM and HBPM as part of diagnosis of hypertension in the U.S. context. Environmental context and resources was the major barrier to ABPM. Concerns about being capable of successfully obtaining valid data were the most important barriers to HBPM. Future efforts are needed to overcome these barriers and increase the adoption of evidence-based hypertension screening recommendations.
Highlights.
ABPM and HBPM are rarely conducted before hypertension diagnosis in the US
Barriers to ABPM and HBPM were identified by surveying primary care providers
Top barriers to ABPM were inaccessible testing centers and costs of testing
Top barriers to ABPM were concerns about patient compliance with testing protocol
Acknowledgments
This worked was supported by the Agency for Healthcare Research and Quality (R01-HS024262). Additionally, Dr. Kronish was supported by grant UL1-TR001873 from the National Center for Advancing Translational Sciences; Dr. Shimbo was supported by grant K24-HL125704 from the National Heart, Lung, and Blood Institute (NHLBI); Dr. Kent was supported by grant T32-HL00745733 from NHLBI; and Dr. Muntner was supported by 15SFRN2390002 from the American Heart Association.
Footnotes
Prior presentations: Abstract presenting the New York City data, alone, using a different framework for organizing barriers was presented at the 2016 meeting of the American Society of Hypertension. Reference: Kronish IM, Safford M, Kent S, Sullivan A, Muntner P, Shimbo D. Barriers to incorporating ambulatory and home blood pressure monitoring into clinical practice: the primary care perspective. American Society of Hypertension Annual Scientific Meeting, New York, NY. May 2016.
Conflicts of Interest: Dr. Shimbo receives support as a consultant to Abbott Vascular and Novartis Pharmaceuticals Corporation.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Siu AL Force USPST. Screening for High Blood Pressure in Adults: U.S. Preventive Services Task Force Recommendation Statement. Annals of internal medicine. 2015;163(10):778–786. doi: 10.7326/M15-2223. [DOI] [PubMed] [Google Scholar]
- 2.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Journal of hypertension. 2013;31(7):1281–1357. doi: 10.1097/01.hjh.0000431740.32696.cc. [DOI] [PubMed] [Google Scholar]
- 3.Pickering TG, White WB American Society of Hypertension Writing G. ASH Position Paper: Home and ambulatory blood pressure monitoring. When and how to use self (home) and ambulatory blood pressure monitoring. Journal of clinical hypertension. 2008;10(11):850–855. doi: 10.1111/j.1751-7176.2008.00043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krause T, Lovibond K, Caulfield M, McCormack T, Williams B Guideline Development G. Management of hypertension: summary of NICE guidance. Bmj. 2011;343:d4891. doi: 10.1136/bmj.d4891. [DOI] [PubMed] [Google Scholar]
- 5.Daskalopoulou SS, Rabi DM, Zarnke KB, et al. The 2015 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. The Canadian journal of cardiology. 2015;31(5):549–568. doi: 10.1016/j.cjca.2015.02.016. [DOI] [PubMed] [Google Scholar]
- 6.Pickering TG, James GD, Boddie C, Harshfield GA, Blank S, Laragh JH. How common is white coat hypertension? Jama. 1988;259(2):225–228. [PubMed] [Google Scholar]
- 7.Piper MA, Evans CV, Burda BU, Margolis KL, O'Connor E, Whitlock EP. Diagnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: a systematic review for the U.S. Preventive Services Task Force. Annals of internal medicine. 2015;162(3):192–204. doi: 10.7326/M14-1539. [DOI] [PubMed] [Google Scholar]
- 8.Shimbo D, Kent ST, Diaz KM, et al. The use of ambulatory blood pressure monitoring among Medicare beneficiaries in 2007–2010. Journal of the American Society of Hypertension : JASH. 2014;8(12):891–897. doi: 10.1016/j.jash.2014.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kent ST, Shimbo D, Huang L, et al. Rates, amounts, and determinants of ambulatory blood pressure monitoring claim reimbursements among Medicare beneficiaries. Journal of the American Society of Hypertension : JASH. 2014;8(12):898–908. doi: 10.1016/j.jash.2014.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shimbo D, Abdalla M, Falzon L, Townsend RR, Muntner P. Role of Ambulatory and Home Blood Pressure Monitoring in Clinical Practice: A Narrative Review. Annals of internal medicine. 2015;163(9):691–700. doi: 10.7326/M15-1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bloch MJ, Basile JN. UK guidelines call for routine 24-hour ambulatory blood pressure monitoring in all patients to make the diagnosis of hypertension--not ready for prime time in the United States. Journal of clinical hypertension. 2011;13(12):871–872. doi: 10.1111/j.1751-7176.2011.00551.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Safford MM, Shewchuk R, Qu H, et al. Reasons for not intensifying medications: differentiating “clinical inertia” from appropriate care. Journal of general internal medicine. 2007;22(12):1648–1655. doi: 10.1007/s11606-007-0433-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shewchuk R, O'Connor SJ. Using cognitive concept mapping to understand what health care means to the elderly: an illustrative approach for planning and marketing. Health Mark Q. 2002;20(2):69–88. doi: 10.1300/J026v20n02_05. [DOI] [PubMed] [Google Scholar]
- 14.Levine DA, Saag KG, Casebeer LL, Colon-Emeric C, Lyles KW, Shewchuk RM. Using a modified nominal group technique to elicit director of nursing input for an osteoporosis intervention. J Am Med Dir Assoc. 2006;7(7):420–425. doi: 10.1016/j.jamda.2006.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pena A, Estrada CA, Soniat D, Taylor B, Burton M. Nominal group technique: a brainstorming tool for identifying areas to improve pain management in hospitalized patients. Journal of hospital medicine. 2012;7(5):416–420. doi: 10.1002/jhm.1900. [DOI] [PubMed] [Google Scholar]
- 16.Harvey N, Holmes CA. Nominal group technique: an effective method for obtaining group consensus. Int J Nurs Pract. 2012;18(2):188–194. doi: 10.1111/j.1440-172X.2012.02017.x. [DOI] [PubMed] [Google Scholar]
- 17.Van de Ven AH, Delbecq AL. The nominal group as a research instrument for exploratory health studies. Am J Public Health. 1972;62(3):337–342. doi: 10.2105/ajph.62.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hickling JA, Nazareth I, Rogers S. The barriers to effective management of heart failure in general practice. Br J Gen Pract. 2001;51(469):615–618. [PMC free article] [PubMed] [Google Scholar]
- 19.Michie S, Johnston M, Abraham C, et al. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. 2005;14(1):26–33. doi: 10.1136/qshc.2004.011155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Phillips CJ, Marshall AP, Chaves NJ, et al. Experiences of using the Theoretical Domains Framework across diverse clinical environments: a qualitative study. J Multidiscip Healthc. 2015;8:139–146. doi: 10.2147/JMDH.S78458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implementation science : IS. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheng C, Studdiford JS, Diamond JJ, Chambers CV. Primary care physician beliefs regarding usefulness of self-monitoring of blood pressure. Blood Press Monit. 2003;8(6):249–254. doi: 10.1097/00126097-200312000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Logan AG, Dunai A, McIsaac WJ, Irvine MJ, Tisler A. Attitudes of primary care physicians and their patients about home blood pressure monitoring in Ontario. Journal of hypertension. 2008;26(3):446–452. doi: 10.1097/HJH.0b013e3282f2fdd4. [DOI] [PubMed] [Google Scholar]
- 24.Parati G, Hernandez-Hernandez R, Velasco M. Home blood pressure monitoring in general practice: expectations and concerns. J Hypertens. 2006;24(9):1699–1701. doi: 10.1097/01.hjh.0000242390.76978.1a. [DOI] [PubMed] [Google Scholar]
- 25.Tirabassi J, Fang J, Ayala C. Attitudes of primary care providers and recommendations of home blood pressure monitoring--DocStyles, 2010. J Clin Hypertens (Greenwich) 2013;15(4):224–229. doi: 10.1111/jch.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steinmann WC, Chitima-Matsiga R, Bagree S. What are specialist and primary care clinicians' attitudes and practices regarding home blood pressure monitoring for hypertensive patients? Mo Med. 2011;108(6):443–447. [PMC free article] [PubMed] [Google Scholar]
- 27.Robins LS, Jackson JE, Green BB, Korngiebel D, Force RW, Baldwin LM. Barriers and facilitators to evidence-based blood pressure control in community practice. J Am Board Fam Med. 2013;26(5):539–557. doi: 10.3122/jabfm.2013.05.130060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Flynn E, Flavin A. General practitioner's reported use of clinical guidelines for hypertension and ambulatory blood pressure. Irish medical journal. 2012;105(3):89–91. [PubMed] [Google Scholar]
- 29.Francis JJ, O'Connor D, Curran J. Theories of behaviour change synthesised into a set of theoretical groupings: introducing a thematic series on the theoretical domains framework. Implementation science : IS. 2012;7:35. doi: 10.1186/1748-5908-7-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dyson J, Lawton R, Jackson C, Cheater F. Development of a theory-based instrument to identify barriers and levers to best hand hygiene practice among healthcare practitioners. Implementation science : IS. 2013;8:111. doi: 10.1186/1748-5908-8-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.French SD, McKenzie JE, O'Connor DA, et al. Evaluation of a theory-informed implementation intervention for the management of acute low back pain in general medical practice: the IMPLEMENT cluster randomised trial. PloS one. 2013;8(6):e65471. doi: 10.1371/journal.pone.0065471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Michie S, Atkins L, West R. The Behaviour Change Wheel: A Guide to Designing Interventions. Kingston-upon-Thames, Great Britain: Silverback Publishing; 2014. [Google Scholar]
- 33.Michie S, Johnston M, Francis J, Hardeman W, Eccles M. From theory to intervention: Mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol-Int Rev. 2008;57(4):660–680. [Google Scholar]
- 34.Teich JM, Osheroff JA, Pifer EA, Sittig DF, Jenders RA Panel CDSER. Clinical decision support in electronic prescribing: recommendations and an action plan: report of the joint clinical decision support workgroup. Journal of the American Medical Informatics Association : JAMIA. 2005;12(4):365–376. doi: 10.1197/jamia.M1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garg AX, Adhikari NK, McDonald H, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. Jama. 2005;293(10):1223–1238. doi: 10.1001/jama.293.10.1223. [DOI] [PubMed] [Google Scholar]
- 36.Roshanov PS, Fernandes N, Wilczynski JM, et al. Features of effective computerised clinical decision support systems: meta-regression of 162 randomised trials. Bmj. 2013;346:f657. doi: 10.1136/bmj.f657. [DOI] [PubMed] [Google Scholar]