Abstract
Objectives
Acetaminophen overdoses result in nearly 500 deaths annually and a much larger number of hospitalizations. Suicidal overdoses are exceeded in number in the United States by unintentional overdoses. We evaluated clinical, demographic and psychosocial factors among unintentional and intentional overdose patients whose acetaminophen (APAP) toxicity had resulted in acute liver failure. We hypothesized that APAP overdose patients would be more likely to suffer from behavioral health issues and display higher impulsivity scores than the general population.
Methods
Within 4 days of admission and initial recovery of alertness, we administered a detailed questionnaire that included questions on APAP intake (e.g., dose taken, intent, other substances ingested), the Mini International Neuropsychiatric Interview modules on Depression, Alcohol Use, Substance Use, and Pain Disorders and The Barratt Impulsiveness Scale-11.
Results
The group included 44 intentional (single time point ingestions with the intent to self-harm) and 51 unintentional (multiple time point ingestions to manage pain or other condition) APAP patients enrolled in the Acute Liver Failure Study Group registry between 2007 and 2013. Both groups were characterized by similar frequencies of chronic pain, depressive symptoms at time of ingestion and alcohol and substance use disorders, all at higher rates than the general population. Overall, APAP patients scored higher than the general population for Non-planning aspects of impulsivity, with no apparent differences between other impulsivity scores or between intentional and unintentional APAP patients.
Conclusions
Depression, mismanagement of problematic chronic pain, frequent substance abuse, and increased impulsivity appear to provide the substrate for many APAP overdoses.
Keywords: impulsivity, chronic pain disorder, acute liver failure, acetaminophen
INTRODUCTION
Acetaminophen (APAP)-related overdose is the leading cause of acute liver failure (ALF) in the United States and other Western countries [1–3]. Approximately 46% of patients within the Acute Liver Failure Study Group (ALFSG) registry have ALF thought to be due to APAP overdose, while the next most common etiology (drug-induced liver injury due to prescription or herbal medications) only accounts for 11% of cases [4,5]. The frequent occurrence of APAP ALF is attributed in part to readily available APAP, both in prescription and over-the-counter preparations [6,7] and its reputation of safety and effectiveness when used as directed [6]. Since the first descriptions of cases in the 1980’s, most APAP overdoses are categorized into two groups: intentional (e.g., those that are attempts at self-harm, suicidal, single time point ingestions) and unintentional (e.g., those that occur in the setting of inadequate pain relief, continuing to take excessive doses over several days to weeks) [2]. While the groups differ in some respects, both intentional and unintentional APAP overdose patients use more alcohol, other substances, and anti-depressants on average, compared to the general population. Unintentional APAP overdose patients also are observed to more frequently use APAP-opioid combination products for pain relief [3].
Several UK studies suggest that APAP overdoses typically occur “impulsively,” meaning that APAP is ingested within an hour of initially considering taking the medication [8,9]. There is a paucity of studies which quantify the role of “impulsivity” as a behavioral attribute in the ALF setting. In the US, most of the research to date regarding APAP ALF continues to focus on incidence and other estimates (e.g., developing prognosis models). Although impulsivity [10], depressive disorders [11], alcohol and substance use disorders [12], and pain disorders [13] have all been associated with drug overdosing, there are limited data regarding the psychosocial and behavioral characteristics of the APAP overdose population, since APAP itself is not a substance of abuse. In this study, we examine a cohort of patients admitted to sites participating in the ALFSG with ALF secondary to APAP overdose, using a detailed questionnaire to identify psychosocial and behavioral factors related to overdosing. We hypothesized that APAP overdose patients are more likely to suffer from behavioral health issues and to display higher impulsivity scores compared to the general population. We further examined these characteristics to determine how APAP overdose patients may or may not differ between each other based on intentionality of overdose.
METHODS
Participants
Participants for this study were patients from APAP-related hospitalization that were enrolled at eight different study sites participating in the ALFSG registry (February 2007–June 2013). Patients met established criteria for either Acute Liver Failure (ALF) or Acute Liver Injury (ALI); clinical markers of International Normalized Ratio (INR) ≥ 2.0 and ALT ≥ 10× elevated (irrespective of bilirubin level) were used to identify ALI, while INR ≥ 1.5 and any degree of hepatic encephalopathy were used to identify ALF. A primary diagnosis of APAP hepatotoxicity was determined by site principal investigators, experienced hepatologists, using standard diagnostic criteria: a history of ingestion of APAP compounds, biochemical pattern commonly associated with APAP liver injury (very high aminotransferases and low bilirubin), with or without detectable acetaminophen serum levels at study admission [3]. Diagnoses were also confirmed through patient self-reporting of prior APAP use at the time of the interview. Overdoses were classified into two categories: intentional where the patient admits to self-harm by ingesting significant quantities of APAP at a single time point versus unintentional overdoses, where patients consume excessive quantities of APAP over several days for pain or other related symptom relief [2]. Patients were placed in one of these categories based on self-reporting and chart review at time of admission. In six cases, intentionality was initially marked in the chart as “unknown” by the principal investigator and subsequently clarified through patient self-reporting (1 intentional and 5 unintentional). Patient self-reporting and clinician assessment of intentionality of overdose matched 86% of the time. When cases did not match, we categorized patients based on fit within our working definitions of intentionality. As such, two patients who reported having suicidal thoughts but denied a suicidal gesture were categorized as “unintentional” because they had been using APAP regularly for pain management. Eighteen patients denied a suicidal gesture but since their overdose occurred from a single time point ingestion of APAP we classified them as “intentional.” While it is possible some of these may have indeed been unintentional overdoses, our categorization of these as “intentional” is based on a probable clinical assumption that many of these patients might have had reasons to deny suicidal intent. Other deviations from our working definition included two patients who admitted to a suicide attempt yet consumed APAP over multiple time points within a 24-hour period. These were considered “intentional” due to the patient reporting self-harm. Reported use of APAP-containing compounds in the “unintentional” group denoted daily usage ranging from four days to over five years.
This study was approved by Institutional Review Boards at each site. To collect initial data for ALF patients enrolled in the ALFSG registry, patients’ next of kin were required to have signed permission, since the ALF patient by definition is encephalopathic and would have impaired judgment. ALI patients were allowed to give consent directly for the registry. After recovery from encephalopathy, enrolled ALF, as well as the ALI patients were approached for participation in the questionnaire study. Patients provided separate signed informed consent for the administration of the questionnaire prior to the start of any research activity. Due to the self-reporting component of the study, the site investigators referred participants to study coordinators once the patients were no longer considered medically or psychiatrically unstable; as a result, these were not consecutive patients but represented those deemed appropriate, having recovered and not requiring further medical support at the time of the questionnaire.
Research coordinators who had agreed to participate at eight of the ALFSG sites selected patients who had made a satisfactory recovery without transplantation to determine whether they were willing to participate in this additional questionnaire study. If they agreed and signed a separate consent, the coordinator then administered a multi-part, structured questionnaire to recovering patients nearing hospital discharge. After initial screening questions to determine whether the overdose was intentional or unintentional, the second part of the questionnaire sought to obtain detailed dosing information–the exact doses taken, circumstances leading up to the overdose, the level of understanding of possible harm from acetaminophen, and patient perspectives on several types of preventive interventions. The next part of the questionnaire consisted of administering the Barratt Impulsiveness Scale 11 (BIS-11) and four modules of the Mini International Neuropsychiatric Interview (M.I.N.I) Plus. The questionnaire administration took place during their recovery process while still in the hospital but near to discharge (median four days after admission).
Measures
The BIS-11 is a 30-item questionnaire that assesses the personality trait of impulsivity using three subscales (Attentional, Non-planning and Motor) and a total score [14]. Impulsivity is defined as “a predisposition toward rapid, unplanned reactions to internal or external stimuli without regard to the negative consequences of these reactions to the impulsive individuals or to others” [15], with the following sub-traits: Attentional (“focusing on the task at hand” and cognitive instability), Non-planning (self-control and cognitive complexity) and Motor (acting without thinking and perseverance) Impulsiveness [14]. Items are scored on a 4-point scale (rarely/never=1, occasionally=2, Often=3, Almost Always/Always=4) without relation to any specific time-period. Higher summed scores for all items indicate higher levels of impulsivity.
The M.I.N.I. Plus 5.0.0 was developed from the M.I.N.I. as an efficient diagnostic interview and is used in clinical as well as research settings [16]. The questionnaire follows DSM-IV and ICD-10 criteria, screening for a number of Axis I diagnoses. For this study, the following modules were used: Major depressive disorders, alcohol use disorders, non-alcohol substance use disorders, and pain disorders. Other relevant modules, such as suicidality and anxiety disorders, were considered but to ensure the questionnaire did not pose excessive burden on the patient, we elected to ask more specifically about history of suicide attempts and to review charts for documented history of anxiety.
Data Analysis
Descriptive statistics (percentage, median and interquartile range (IQR)) for demographic and clinical data within the ALFSG registry were calculated for the intentional and unintentional groups. The primary outcome measures were impulsivity (subscales and total score) and the M.I.N.I. Plus 5.0 scores. Exact 95% binomial confidence intervals were computed for MINI Plus scores for intentional and unintentional groups. Wald 95% confidence intervals were computed for Barratt Impulsivity scores for all APAP patients in our study. Analyses were performed using SAS software.
RESULTS
During the time-period of the study from February 2007 to June 2013, 745 subjects presumed to represent ALF APAP were enrolled in the ALFSG registry (out of 1534 overall enrollments), representing the totality of registry patients impacted by APAP overdose. Of these 745, 515 initially survived across all 23 sites of the ALFSG. At the eight sites participating in the current study, 95 completed the questionnaire (41 ALI and 54 ALF). The group included 51 considered unintentional and 44 intentional cases: none were considered “unknown” type of intentionality by self-report. Demographic and clinical data drawn from the registry are shown in Table 1. The overall median age was 35 years (ranged 28–46). Most overdose patients (76%) were women and Caucasian (87%). Overall, there were few clinical differences found between the unintentional and intentional patient categories (Table 1). As expected, a history of psychiatric disease was present in a considerable percentage of the overall sample (66%), with 77% among intentional overdose patients and in more than half of the unintentional group. Anxiety was slightly more common in the unintentional group (19.6% vs. 9.1%), while depression and bipolar disorder were more common among the intentional group (29.4% vs 47.7%; 13.7% vs 25.0%). However, rates of psychotropic medication usage were similar between both groups (41.2% for unintentional and 50.0% for intentional), with more opioid compounds used by the unintentional patients (60.8% vs. 45.5%) but similar frequencies of selective serotonin reuptake inhibitor (SSRI) anti-depressant use in both groups (37.3% for unintentional and 36.4% for intentional). There were also no demographic differences between the study sample and the overall APAP population of the ALFSG registry (data not shown).
Table 1.
Demographic and clinical characteristics by intentionality of overdose from registry.
| Unintentional Patients (Total N=50) |
Intentional Patients (Total N=43) |
Total Patients (Total N=95) |
||||
|---|---|---|---|---|---|---|
| N | Median (IQR) or Number (%) |
N | Median (IQR) or Number (%) |
N | Median (IQR) or Number (%) |
|
| Age | 51 | 34 (28–46) | 44 | 35 (27–46) | 95 | 35 (28–46) |
| Female | 51 | 40 (78.4%) | 44 | 32 (72.7%) | 95 | 72 (75.8%) |
| Caucasian | 51 | 45 (88.2%) | 44 | 38 (86.4%) | 95 | 83 (87.4%) |
| Hispanic or Latino | 51 | 3 (5.9%) | 44 | 4 (9.1%) | 95 | 7 (7.4%) |
| Years Educated | 39 | 12 (10–13) | 37 | 12 (11–14) | 76 | 12 (11–13) |
| Marital Status | ||||||
| Never Married | 28 | 5 (17.9%) | 29 | 14 (48.3%) | 57 | 19 (33.3%) |
| Married | 28 | 13 (46.4%) | 29 | 8 (27.6%) | 57 | 22 (38.6%) |
| Divorced | 28 | 3 (10.7%) | 29 | 6 (20.7%) | 57 | 9 (15.8%) |
| Separated | 28 | 1 (3.6%) | 29 | 1 (3.4%) | 57 | 2 (3.5%) |
| Widowed | 28 | 1 (3.6%) | 29 | 0 (0%) | 57 | 1 (1.8%) |
| Significant Other | 28 | 5 (17.9%) | 29 | 1 (3.4%) | 57 | 6 (10.5%) |
| Psychiatric Disease | 51 | 29 (56.9%) | 44 | 34 (77.3%) | 95 | 63 (66.3%) |
| Anxiety | 51 | 10 (19.6%) | 44 | 4 (9.1%) | 95 | 14 (14.7%) |
| Depression | 51 | 15 (29.4%) | 44 | 21 (47.7%) | 95 | 36 (37.9%) |
| Bipolar | 51 | 7 (13.7%) | 44 | 11 (25.0%) | 95 | 18 (18.9%) |
| Schizophrenia | 51 | 1 (2.0%) | 44 | 1 (2.3%) | 95 | 2 (2.1%) |
| Other | 51 | 6 (11.8%) | 44 | 7 (15.9%) | 95 | 13 (13.7%) |
| Med | ||||||
| SSRI | 51 | 19 (37.3%) | 44 | 16 (36.4%) | 95 | 35 (36.8%) |
| Psych Med | 51 | 21 (41.2%) | 44 | 22 (50.0%) | 95 | 43 (45.3%) |
| Opioid | 51 | 31 (60.8%) | 44 | 20 (45.5%) | 95 | 51 (53.7%) |
| Benzos | 51 | 24 (47.1%) | 44 | 9 (20.5%) | 95 | 33 (34.7%) |
| IDU | 51 | 3 (5.9%) | 44 | 11 (25.0%) | 95 | 14 (14.7%) |
| Amphetamines | 51 | 0 (0%) | 44 | 2 (4.5%) | 95 | 2 (2.1%) |
| Narcotics | 51 | 2 (3.9%) | 44 | 2 (4.5%) | 95 | 4 (4.2%) |
| Cocaine | 51 | 0 (0%) | 44 | 2 (4.5%) | 95 | 2 (2.1%) |
| Other | 51 | 1 (2.0%) | 44 | 2 (4.5%) | 95 | 3 (3.2%) |
| APAP dose per day (mg) | 37 | 6,000 (2,750–13,000) | 32 | 20,000 (7,625–42,500) | 69 | 10,000 (4,000–25,000) |
Overdose Characteristics
In general, the events surrounding the overdose (size, circumstances, reasons, intent and other substances used) that had been obtained on admission to the hospital were corroborated on the patient questionnaire. For example, the dosing information that in many instances had been obtained from a family member, was substantiated by the patient (Figure 1). A strong, positive correlation of 0.737 was observed between the ingested dose reported by the patient in our questionnaire and that found in the ALFSG registry itself. Patients reported slightly lower amounts of APAP taken, regardless of whether the overdose was intentional or unintentional. The median dose ingested by patients with an intentional overdose was 20,000 mg, while the median daily dose ingested by patients with an unintentional overdose was 6,000 mg. It should be noted that we were only able to obtain accurate enough dosing information on 72.6% of our sample. When a clear dose was missing, patients were likely to give too general of a descriptor to approximate (e.g., “a handful” or “many”) or state they could not recall.
Figure 1.
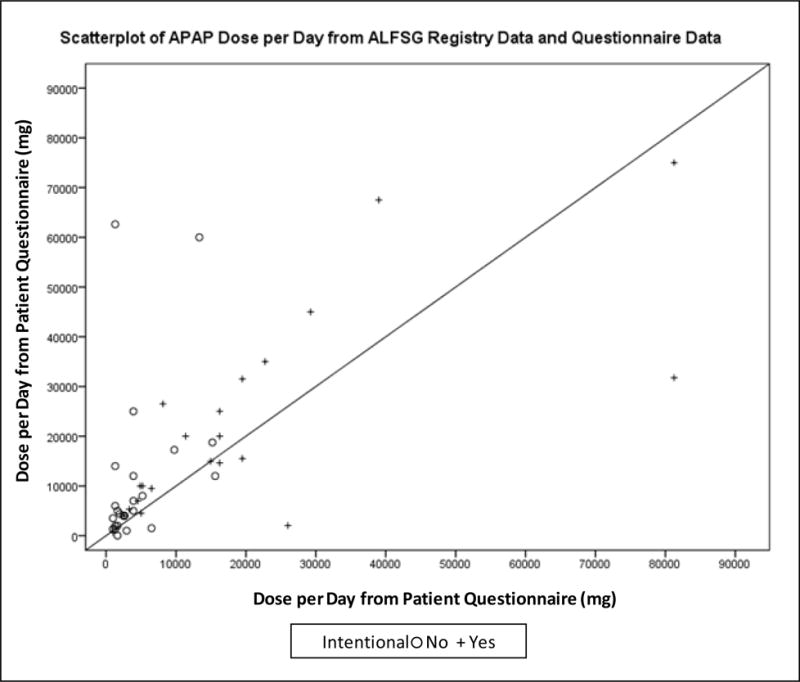
APAP Dose per day from questionnaire data compared to registry.
Other characteristics of the overdose group we examined included reasons for taking APAP and whether alcohol was involved. In all cases of intentional overdoses, suicide was the primary purpose for consuming APAP. Primary reasons for unintentional overdoses were pain-related, specifically including orthopedic pain, toothache, or headache. One-third reported consuming alcohol prior to their overdose. Patients in the intentional category were more likely to report drinking alcohol within 48 hours prior to their overdose (47.5% for intentional vs. 19.0% for unintentional).
M.I.N.I Plus 5
Results of the M.I.N.I Plus 5 are reported in Table 2. A greater portion of the intentional cases reported experiencing more major depressive episodes in the past as well as currently (past: 55.6% vs. 50.0%, current: 41.0% vs. 28.6%), though these differences were not statistically significant (95% confidence intervals overlap). Other types of mood disorders were not common in either group. The intentional overdose patients also reported more problems with alcohol and other substance use disorders, lifetime (substance dependence: 35.0% vs. 28.0%) and current (alcohol abuse or dependence: 39.0% vs. 28.6%, substance abuse or dependence: 38.5% vs. 28.0%). Current pain disorder associated with psychosocial factors and general medical condition was present in both groups of patients (26.0% in unintentional and 10.5% in intentional overdoses). Chronic pain disorder was similarly present in both groups of patients (28.0% vs. 10.5%). While rates of pain disorders were generally low in both groups, the perception of problematic chronic pain was relatively high for both groups (70.5% and 46.3%). For all psychiatric conditions mentioned above, both groups demonstrated higher rates than what is commonly found in the general population.
Table 2.
MINI results by intentionality
| Unintentional Cases (Total N=51) |
Intentional Cases (Total N=44) |
|||||||
|---|---|---|---|---|---|---|---|---|
| N | N events |
% events |
95% CI* for % events |
N | N events |
% events |
95% CI* for % events |
|
| Major Depressive Episode (Current) | 49 | 14 | 28.6 | 16.6–43.3 | 39 | 16 | 41.0 | 25.6–57.9 |
| Major Depressive Episode (Past) | 40 | 20 | 50.0 | 33.8–66.2 | 36 | 20 | 55.6 | 38.1–72.1 |
| Mood Disorder (Current) | 49 | 2 | 4.1 | 0.01–14.0 | 38 | 0 | 0.0 | 0.0–9.3 |
| Mood Disorder (Past) | 42 | 1 | 2.4 | 0.1–12.6 | 37 | 0 | 0.0 | 0.0–9.5 |
| Substance Induced Mood Disorder (Current) | 49 | 1 | 2.0 | 0.1–10.9 | 38 | 2 | 5.3 | 0.6–17.8 |
| Substance Induced Mood Disorder (Past) | 42 | 2 | 4.8 | 0.6–16.2 | 36 | 2 | 5.6 | 0.7–18.7 |
| Alcohol Dependence/Abuse (Current) | 49 | 14 | 28.6 | 16.6–43.3 | 41 | 16 | 39.0 | 24.2–55.5 |
| Substance Dependence (Lifetime) | 50 | 14 | 28.0 | 16.2–42.5 | 40 | 14 | 35.0 | 20.6–51.7 |
| Substance Dependence/Abuse (Current) | 50 | 14 | 28.0 | 16.2–42.5 | 39 | 15 | 38.5 | 23.4–55.4 |
| Pain Disorder Associated with Psychosocial Factors (Current) | 50 | 1 | 2.0 | 0.1–10.7 | 38 | 0 | 0.0 | 0.0–9.3 |
| Pain Disorder Associated with Psychosocial Factors and General Medical Condition (Current) | 50 | 13 | 26.0 | 14.6–40.4 | 38 | 4 | 10.5 | 2.9–24.8 |
| Chronic Pain Disorder | 50 | 14 | 28.0 | 16.2–42.5 | 38 | 4 | 10.5 | 2.9–24.8 |
| Problematic Chronic Pain | 44 | 31 | 70.5 | 54.8–83.2 | 41 | 19 | 46.3 | 30.7–62.6 |
Exact binomial CI’s
Barratt Impulsiveness Scale
Impulsivity as measured by the BIS-11 was assessed for the three sub-traits and total score. The sub-trait and total scores for the BIS-11 by each APAP overdose group are shown in Figure 2. The distribution of Attentional score was similar for both groups. Whereas the median Motor scores were similar for the intentional and unintentional groups, there was slightly more variability within the unintentional group. Likewise, the median Non-planning scores were similar for the intentional and unintentional groups, and there was slightly more variability between patients within the unintentional overdose group compared to the intentional group.
Figure 2.
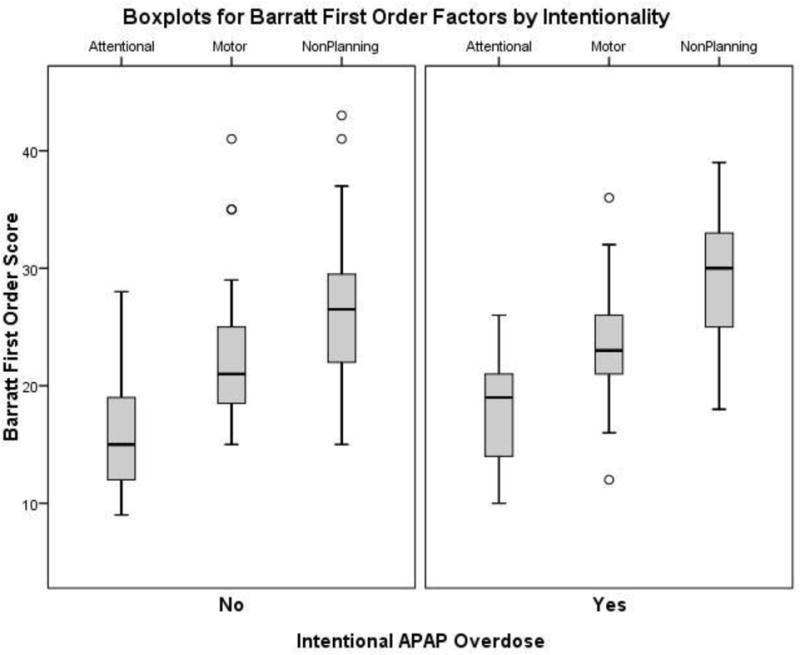
First order BIS scores by intentionality
Both intentional and unintentional patients showed overall higher impulsivity Non-planning and total scores compared to the general population (Table 3) [14]. Although there were no significant differences for the APAP ALF group and general population for the Attentional and Motor subscales (overlapping confidence intervals), those in the study group were significantly more likely to have increased total impulsivity scores that were largely the result of increases in the Non-planning component when compared to the general population.
Table 3.
BIS results by intentionality
| APAP Cases (Intentional and Unintentional) (N =95) |
Normal Population15 (N=1577) |
|||
|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | |
| Attentional | 16.8 | 15.6–18.1 | 16.7 | 16.5–16.9 |
| Motor | 22.1 | 20.8–23.5 | 22.0 | 21.8–22.2 |
| Non-planning | 26.9 | 25.4–28.4 | 23.6 | 23.4–23.8 |
| Total | 65.9 | 62.2–69.5 | 62.3 | 61.8–62.8 |
DISCUSSION
We examined the clinical features surrounding severe acetaminophen overdoses using patient recall data via a detailed questionnaire format, to describe both psychosocial and behavioral factors surrounding these events. ALFSG registry data provided some information for identifying common factors relevant to APAP overdosing, such as intentionality and substance use. While ALI patients provided medical and social histories directly to the clinician, ALF patients demonstrating altered mental status (by definition) required history intake via family members or friends. Thus, initial clinician assessments of APAP overdose and intentionality were based at least in part on second hand accounts. For our project, the questionnaire provided a mechanism to confirm the extent and factors surrounding the overdose through self-reporting, once the patients had fully recovered mental functioning. In general, the questionnaire confirmed the prior clinical assessment of dose and intentionality, the latter matching 86% of the time, and clarified the 6% initially marked as unknown. The remaining 8% mismatch in self-report and initial clinician assessment reflects a need for a more nuanced understanding of the clinical categorization of overdose patients provided by the added information obtained well after the initial patient intake.
Our working definitions of “intentional” and “unintentional” draw from the work from Schiodt et al. [2] that clearly demarcated two distinct categories. Yet, nearly two decades later, the groups appear more similar than different in several ways. While intentional overdose patients reported more depressive episodes, current and past, the difference between this group and the unintentional overdose group was not statistically significant. Moreover, both groups had similar rates for usage of SSRI and other psychotropic medications, per medical history. Both groups also reported similar rates of substance dependence (lifetime), with only slightly higher rates of current alcohol and substance use disorders present in the intentional group. Major depressive episodes [17,18], alcohol and substance use disorders [12,18] have all been associated with suicidal behavior. These similarities call attention to the dysfunctional nature of individuals susceptible to unintentional overdosing: chronic pain, depression, and substance abuse all may predispose to impulsivity, in continuing to seek pain relief beyond the bounds of rational behavior, such as limitation of daily intake of medication of any type. It should be noted that patients with chronic pain may be prescribed psychotropic drugs including serotonin-norepinephrine reuptake inhibitors, such as duloxetine that specifically carry indications for pain, making it hard to distinguish depression management from pain management in the unintentional group.
Unintentional overdosing may be considered a result of mismanaged chronic pain, while intentional overdosing is typically viewed in terms of a behavioral health issue [19]. While only a quarter of the patients with an unintentional overdose had a diagnosable chronic pain disorder, approximately 70% perceived their chronic pain as problematic. This perception may have behavioral health implications as patients find ways to cope with their pain, such as self-medicating with increased dosages of APAP. Moreover, high rates of suicidal ideation and gestures have been found in patients suffering from chronic pain [20]. Our data indicate problematic chronic pain might also play a role in almost half of intentional overdosing, further suggesting similar motivations between the two groups. Thus, the distinction between intentional and unintentional becomes less clear, making the entire overdose population in many ways resemble each other. Moreover, the high rates of perceived problematic chronic pain in both groups warrant further examination to better inform clinical pain management practices. While acetaminophen (paracetamol) overdoses in the United Kingdom have been considered almost exclusively related to suicide attempts, more recently unintentional overdoses have been recognized and seen to carry a worse prognosis, confirming the early data from 1997 [2]. While the definitions used are similar to our studies, the additional term ‘staggered overdose’ has been proposed; however, whether intentional self-harm can follow a multi-day pattern still remains unclear [19,21].
Of further interest, both groups demonstrated similar degrees of impulsivity, per the BIS. Once again, the intentional and unintentional overdoses did not appear to be significantly different from each other; however, both groups were more impulsive than the general population, particularly for Non-planning impulsivity. This finding suggests that clinicians should consider patients with unintentional overdoses more like an intentional overdose than the general population, which has implications for medication regimens and transplant listing. Impulsivity is a personality trait of particular importance in relation to certain maladaptive behaviors and has been associated with antisocial behavior [22], irritability and reactive aggression [23], severity of substance abuse [24], and suicidal behavior [24–26]. Non-planning, characterized by the failure to problem solve and plan ahead, was distinguished from motor and attentional factors in a study of 433 prisoners, suggesting that Non-planning is the strongest indicator of serious dysfunctional impulsivity [27].
Impulsivity is often compounded by alcohol and substance use, further increasing the potential for risky behaviors [28]. In our cohort, a quarter of the unintentional group and slightly over half of the intentional group reported using alcohol at the time of APAP overdose. It is well documented that nearly half of those who present to the emergency room following self-harm, reportedly consumed alcohol immediately preceding or as part of the episode [29–31]. Our findings support these studies, yet differ somewhat from other specific research on intentional and unintentional APAP overdoses. In the case of intentional APAP overdoses, Simkin et al. [8] found only a third of patients reported consuming alcohol prior to their overdose. Craig et al. [19] found that patients with unintentional overdoses were more likely to have consumed alcohol immediately prior to their ALF episode in comparison to the intentional group. The connection between alcohol and ALF in general is not fully understood and is being examined further through another ancillary study of the ALFSG.
While the current study did not reveal statistically significant differences in the psychiatric conditions tested between the two overdose categories, differences may be found in a future study with a larger sample size. M.I.N.I results showed that both groups of patients were vulnerable to psychiatric comorbidities such as depression at the time of ingestion and far exceeded rates found in the general population. Medical histories also indicate high rates of bipolar disorder among the intentional group and anxiety disorder among the unintentional group. Future psychosocial studies may be further corroborated with genetic testing. Correlations between certain personality factors and high-risk behavior, such as drug overdosing are recognized and may have a genetic basis. Impulsivity and substance use disorder appear closely linked and share a number of specific genes within the hypothalamus-pituitary-adrenal axis that create abnormal stress responses that lead to drug use behavior [32,33]. Indeed, in a study from our group, DNA from 229 APAP overdose patients was interrogated for 19 single nucleotide polymorphisms associated with impulsivity and substance use disorder with the finding of two SNPs enriched in the study population [34]. There was no difference observed in the frequency between the intentional and unintentional groups. Further exploring both behavioral and genetic characteristics influencing impulsivity and psychiatric comorbidities that impact drug overdose behavior should help inform interventions to prevent ALF from APAP overdoses in patients seeking pain management.
Limitations
While the ALFSG registry is nationally representative of the US population [5], the current findings are limited to a small patient sample from eight registry sites. The small sample size may have limited statistical power to detect differences between groups. A post hoc power analysis, using GPower [35], revealed that on the basis of the mean, between-groups comparison effect size observed in the present study (d=0.45), an n of approximately 154 would be needed to obtain statistical power at the standard .80 level. However, demographics of our study sample were remarkably similar to those of the entire registry population, providing support for its generalizability to the US population. These data may have limited applicability in international populations. While this study examined impulsivity, depressive symptoms, and other risk behaviors, these are not the totality of risk behaviors. Future studies could explore other relevant psychosocial dynamics such as lack of social support or other maladaptive behaviors, as well as other psychiatric conditions such as anxiety or borderline personality disorders. We also did not measure to what extent chronic pain and other psychiatric conditions were being managed by a specialist, and more research is necessary to determine appropriate clinical interventions. Finally, the use of hepatologists, who were caring for the patients through their critical illness, to determine psychiatric stability may have precluded some patient participation if they were transferred to psychiatric services prior to initiating the research protocol. Patients excluded would likely have had more severe psychiatric conditions than those considered suitable for the study.
Conclusions
APAP overdoses remain the leading cause of ALF. Conditions such as depression, alcohol use disorder, substance use disorder and chronic pain are strongly associated with risk of APAP-related ALF and ALI. While chronic pain disorder was present in some of the unintentional overdoses, the perception of a problematic chronic pain may be an exceedingly important condition to address for both intentional and unintentional APAP overdoses. Impulsivity also appeared to impact both intentional and unintentional APAP ALF and ALI. In-depth assessments of behavior and attempts at behavior modification may lead to new strategies to address the increasing problem of APAP overdose.
Highlights.
APAP ALF and psychosocial and behavioral conditions are strongly correlated.
Intentional and unintentional APAP overdoses are more similar than previously known.
Chronic pain disorder plays a considerable role in APAP ALF.
Impulsivity also plays a significant role in APAP ALF.
Acknowledgments
This study was funded by National Institutes of Health grant (DK U-01 58369) for the Acute Liver Failure Study Group provided by the National Institute of Diabetes and Digestive and Kidney Diseases.
The authors would like to acknowledge Jaime Speiser in the development of this manuscript. Members and institutions participating in the Acute Liver Failure Study Group 1998–2016 are as follow: William M. Lee, M.D. (Principal Investigator), The University of Texas Southwestern Medical Center, Dallas, TX; Anne M. Larson, M.D., Iris Liou, M.D., University of Washington, Seattle, WA; Timothy Davern, M.D., University of California, San Francisco, CA (current address: California Pacific Medical Center, San Francisco, CA), Oren Fix, M.D., University of California, San Francisco; Michael Schilsky, M.D., Mount Sinai School of Medicine, New York, NY (current address: Yale University, New Haven, CT); Timothy McCashland, M.D., University of Nebraska, Omaha, NE; J. Eileen Hay, M.B.B.S., Mayo Clinic, Rochester, MN; Natalie Murray, M.D., Baylor University Medical Center, Dallas, TX; A. Obaid S. Shaikh, M.D., University of Pittsburgh, Pittsburgh, PA; Andres Blei, M.D., Northwestern University, Chicago, IL (deceased), Daniel Ganger, M.D., Northwestern University, Chicago, IL; Atif Zaman, M.D., University of Oregon, Portland, OR; Steven H.B. Han, M.D., University of California, Los Angeles, CA; Robert Fontana, M.D., University of Michigan, Ann Arbor, MI; Brendan McGuire, M.D., University of Alabama, Birmingham, AL; Raymond T. Chung, M.D., Massachusetts General Hospital, Boston, MA; Alastair Smith, M.B., Ch.B., Duke University Medical Center, Durham, NC; Robert Brown, M.D., Cornell/Columbia University, New York, NY; Jeffrey Crippin, M.D., Washington University, St Louis, MO; Edwyn Harrison, Mayo Clinic, Scottsdale, AZ; Adrian Reuben, M.B.B.S., Medical University of South Carolina, Charleston, SC; Santiago Munoz, M.D., Albert Einstein Medical Center, Philadelphia, PA; Rajender Reddy, M.D., University of Pennsylvania, Philadelphia, PA; R. Todd Stravitz, M.D., Virginia Commonwealth University, Richmond, VA; Lorenzo Rossaro, M.D., University of California Davis, Sacramento, CA; Raj Satyanarayana, M.D., Mayo Clinic, Jacksonville, FL; and Tarek Hassanein, M.D., University of California, San Diego, CA. The University of Texas Southwestern Administrative Group included Grace Samuel, Ezmina Lalani, Carla Pezzia, Corron Sanders, Ph.D., Nahid Attar, Linda S. Hynan, Ph.D. and Angela Bowling and the Medical University of South Carolina Data Coordination Unit included Valerie Durkalski, Ph.D., Wenle Zhao, Ph.D., Catherine Dillon, Holly Battenhouse, Tomoko Goddard, Lynn Patterson, Jaime Speiser and Caitlyn Nicole ‘Ellerbe Program Directors from the National Institute of Diabetes and Digestive and Kidney Diseases included Patricia Robuck, Ph.D., Edward Doo, M.D., and Averell Sherker, M.D.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have nothing to disclose.
References
- 1.Seeff L, Cuccerini BA, Zimmerman HJ, Adler E, Benjamin SB. Acetaminophen hepatotoxicity in alcoholics A therapeutic misadventure. Ann Intern Med. 1986;104:399–404. doi: 10.7326/0003-4819-104-3-399. [DOI] [PubMed] [Google Scholar]
- 2.Schiødt FV, Rochling FJ, Casey DL, Lee WM. Acetaminophen toxicity in an urban county hospital. N Engl J Med. 1997;337:1112–17. doi: 10.1056/NEJM199710163371602. [DOI] [PubMed] [Google Scholar]
- 3.Larson AM, Fontana RJ, Davern TJ, Polson J, Lalani EK, Hynan LS, Reisch JS, Schiødt FV, Ostapowicz G, Shakil AO, Lee WM. Acetaminophen-Induced acute liver failure: Results of a United States multicenter, prospective study. Hepatology. 2005:1364–1372. doi: 10.1002/hep.20948. [DOI] [PubMed] [Google Scholar]
- 4.Reuben A, Koch DG, Lee WM, Acute Liver Failure Study Group Drug-induced acute liver failure: Results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–2076. doi: 10.1002/hep.23937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reuben A, Tillman H, Fontana RJ, Davern T, McGuire B, Stravitz RT, et al. Outcomes in adults with acute liver failure between 1998 and 2013: An observational cohort study. Ann Intern Med. 2016;164:724–32. doi: 10.7326/M15-2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee WM. Acetaminophen and the US Acute Liver Failure Study Group: lowering the risks of hepatic failure. Hepatology. 2004;40:6–9. doi: 10.1002/hep.20293. [DOI] [PubMed] [Google Scholar]
- 7.Lee WM. Acetaminophen hepatotoxicity: Changing perceptions of a social/medical issue. Hepatology. 2007;46:966–70. doi: 10.1002/hep.21926. [DOI] [PubMed] [Google Scholar]
- 8.Simkin S, Hawton K, Kapur N, Gunnell D. What can be done to reduce mortality from paracetamol overdoses? A patient interview study. QJM. 2012;105:41–51. doi: 10.1093/qjmed/hcr135. [DOI] [PubMed] [Google Scholar]
- 9.Hawton K, Ware C, Mistry H, Hewitt J, Kingsbury S, Roberts D, Weitzel H. Paracetamol self-poisoning characteristics, prevention and harm reduction. Brit J Psych. 1996;168:43–48. doi: 10.1192/bjp.168.1.43. [DOI] [PubMed] [Google Scholar]
- 10.Hayaki J, Stein MD, Lassor JA, Herman DS, Anderson BJ. Adversity among drug users: relationship to impulsivity. Drug Alcohol Depend. 2005;78:65–71. doi: 10.1016/j.drugalcdep.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Tobin MK, Latkin CA. The relationship between depressive symptoms and nonfatal overdose among a sample of drug users in Baltimore, Maryland. J Urban Health. 2003;80:220–9. doi: 10.1093/jurban/jtg025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug alcohol depend. 2004;76:S11–9. doi: 10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Dunn KM, Saunders KW, Rutter CM, Banta-Green CJ, Merrill JO, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152:85–92. doi: 10.1059/0003-4819-152-2-201001190-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psych. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 15.Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. Amer J Psych. 2001;158:1783–93. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- 16.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:S22–33. [PubMed] [Google Scholar]
- 17.Malone KM, Haas GL, Sweeney JA, Mann JJ. Major depression and the risk of attempted suicide. J Affect Disorders. 1995;34:173–85. doi: 10.1016/0165-0327(95)00015-f. [DOI] [PubMed] [Google Scholar]
- 18.Dumais A, Lesage AD, Alda M, Rouleau G, Dumont M, Chawky N, et al. Risk factors for suicide completion in major depression: a case-control study of impulsive and aggressive behaviors in men. Amer J Psych. 2005;162:2116–24. doi: 10.1176/appi.ajp.162.11.2116. [DOI] [PubMed] [Google Scholar]
- 19.Craig DG, Bates CM, Davidson JS, Martin KG, Hayes PC, Simpson KJ. Staggered overdose pattern and delay to hospital presentation are associated with adverse outcomes following paracetamol-induced hepatotoxicity. Brit J Clin Pharmacol. 2012;73:285–294. doi: 10.1111/j.1365-2125.2011.04067.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheatle MD. Depression, chronic pain, and suicide by overdose: On the edge. Pain Med. 2011;(Suppl 2):S43–48. doi: 10.1111/j.1526-4637.2011.01131.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Craig DGN, Bates CM, Davidson JS, Martin KG, Hayes PC, Simpson KJ. Overdose pattern and outcome in paracetamol-induced acute severe hepatotoxicity. Brit J Clin Pharmacol. 2010;71:283–92. doi: 10.1111/j.1365-2125.2010.03819.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luengo MA, Carrillo-de-la-Pena MT, Otero JM, Romero E. A short-term longitudinal study of impulsivity and antisocial behavior. J Personal Social Psychol. 1994;66:542–548. doi: 10.1037//0022-3514.66.3.542. [DOI] [PubMed] [Google Scholar]
- 23.Seroczynski AD, Bergeman CS, Coccaro EF. Etiology of the impulsivity/aggression relationship: Genes or environment? Psych Res. 1999;86:41–57. doi: 10.1016/s0165-1781(99)00013-x. [DOI] [PubMed] [Google Scholar]
- 24.Moeller FG, Dougherty DM, Barratt ES, Schmitz JM, Swann AC, Grabowski J. The impact of impulsivity on cocaine use and retention in treatment. J Subst Abuse Treat. 2001;21:193–198. doi: 10.1016/s0740-5472(01)00202-1. [DOI] [PubMed] [Google Scholar]
- 25.Apter A, Plutchik R, van Praag HM. Anxiety, impulsivity and depressed mood in relation to suicidal and violent behavior. Acta Psychiatrica Scandinavica. 1993;87:1–5. doi: 10.1111/j.1600-0447.1993.tb03321.x. [DOI] [PubMed] [Google Scholar]
- 26.Kaslow NJ, Price AW, Wyckoff S, Bender Grall M, Sherry A, Young S, et al. Person factors associated with suicidal behavior among African American women and men. Cultural Divers Ethnic Minority Psychol. 2004;10:5–22. doi: 10.1037/1099-9809.10.1.5. [DOI] [PubMed] [Google Scholar]
- 27.Haden SC, Shiva A. Trait impulsivity in a forensic inpatient sample: an evaluation of the Barratt Impulsivity Scale. Behav Sci Law. 2008;26:675–690. doi: 10.1002/bsl.820. [DOI] [PubMed] [Google Scholar]
- 28.Lejuez CW, Read JP, Kahler CW, Richards JB, Ramsey SE, Stuart GL, et al. Evaluation of a behavioral measure of risk taking: the Balloon Analogue Risk Task (BART) J Exper Psychol Applied. 2002;8:75. doi: 10.1037//1076-898x.8.2.75. [DOI] [PubMed] [Google Scholar]
- 29.Hawton K, Bergen H, Casey D, Simkin S, Palmer B, Cooper J, et al. Self-harm in England: a tale of three cities. Soc Psychiatry Psych Epidemiol. 2007;42:513–521. doi: 10.1007/s00127-007-0199-7. [DOI] [PubMed] [Google Scholar]
- 30.Horrocks J, Price S, House A, Owens D. Self-injury attendances in the accident and emergency department: Clinical database study. British J Psych. 2003;183:34–39. doi: 10.1192/bjp.183.1.34. [DOI] [PubMed] [Google Scholar]
- 31.Merrill J, Milner G, Owens J, Vale A. Alcohol and attempted suicide. Brit J Addict. 1992;87:83–89. doi: 10.1111/j.1360-0443.1992.tb01903.x. [DOI] [PubMed] [Google Scholar]
- 32.Kreek MJ, Nielsen DA, Butelman ER, LaForge KS. Genetic influences on impulsivity, risk taking, stress responsivity and vulnerability to drug abuse and addiction. Nature Neuroscience. 2005;8:1450–7. doi: 10.1038/nn1583. [DOI] [PubMed] [Google Scholar]
- 33.Verdejo-García A, Lawrence AJ, Clark L. Impulsivity as a vulnerability marker for substance-use disorders: review of findings from high-risk research, problem gamblers and genetic association studies. Neurosci Biobehavior Rev. 2008;32:777–810. doi: 10.1016/j.neubiorev.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 34.Randesi M, Levran O, Correa da Rosa J, Hankins J, Rule J, Kreek MJ, Lee WM. Association of variants of arginine vasopressin and arginine vasopressin receptor 1A, with severe acetaminophen liver injury. Cell Mol Gastroenterol Hepatol. 2017;3:500–505. doi: 10.1016/j.jcmgh.2017.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]


