Abstract
AIM
To study the relation between higher-order aberrations (HOAs) and contrast sensitivity (CS) in normal eyes among a population of laser in situ keratomileusis (LASIK) candidates.
METHODS
In 6629 eyes of 3315 LASIK candidates, CS were measured under dark environment at the spatial frequencies of 1.5, 3, 6, 12 and 18 cycles per degree (c/d), respectively, using an Optec 6500 visual function tester. Meanwhile, ocular HOAs were measured for a 6.0 mm pupil with a Hartmann-Shack wavefront analyzer.
RESULTS
In the study, the subjects with an average spherical equivalent of -4.86±2.07 D were included. HOAs decreased from the third to the sixth order aberrations with predominant aberrations of third-order coma, trefoil and fourth-order spherical aberration. At low and moderate spatial frequencies, CS was negatively correlated with the third-order coma and trefoil aberrations, and decreased with increasing Z31, but increased with increasing Z3−3 and Z5−1. At high spatial frequencies, CS decreased with increasing Z3−3 and increased with increasing Z5−1.
CONCLUSION
At a large pupil size of 6.0 mm, the third-order aberrations, but not the total aberrations, are the main factors affecting CS. Vertical coma is negatively correlated with CS.
Keywords: myopia, contrast sensitivity, higher-order aberrations, coma, spherical aberration
INTRODUCTION
In the past few years, some of the patients had vision degradation with vision blur, glare and halo after laser in situ keratomileusis (LASIK) surgery, and these were considered related to the decrease of contrast sensitivity (CS) after surgery[1]–[4]. It has been proved that wavefront aberration-guided LASIK can improve CS after surgery[5]–[8]. Some researchers have studied the relationship between wavefront aberration and CS in small population (the largest sample contains 196 eyes from 112 patients) and they found negative correlation between high-order aberration (HOA) and CS[9]–[13]. In this study, we studied the relationship between wavefront aberration and CS in a large myopic population (6629 eyes from 3315 patients), our results will provide further evidence to improve wavefront aberration-guide LASIK.
SUBJECTS AND METHODS
The study was approved by the Ethics Committee of Beijing Tongren Hospital. Informed consent was obtained from all individual participants in oral forms and they did not receive pay in this study.
Subjects
The subjects who visited the Myopia Correction Center of Beijing Tongren Hospital between January 2006 and May 2011 and planned to receive LASIK were screened. All subjects should have best corrected visual acuity of 20/20 or better and no history of eye diseases, trauma or surgery. The difference between manifest refraction and cycloplegic refraction spherical equivalent was less than 0.50 D. The subjects either had no history of contact lens wearing or stopped wearing soft contact lenses more than 2wk prior to the ocular examination (or >8wk if rigid gas permeable contact lens were worn).
Ophthalmic Examinations
Both CS and HOAs were measured in one dark room by the same technician. CS was examined using an Optec 6500 visual function tester (Beijing Pratt Medical Instrument Co., Ltd.) with full correction of refractive errors. A night mode with an illumination level of 3 cd/m2 was used. After closing their eyes and resting for 10min, the subjects underwent CS examination at 5 spatial frequencies (1.5, 3, 6, 12 and 18 c/d, respectively) with the best corrected visual acuity. HOAs were measured using a Hartmann-Shack wavefront analyzer (AMO&VISX, USA). After requiring the subjects to blink their eyes, the image acquisition was finished within 3s and was repeated for 3 times. The test results with the best focus on the original picture, the least center deviation, the smallest lower-order aberration, and the best repeatability of HOA images and root mean square (RMS) values at 6.0 mm pupil size were included for analysis.
Statistical Analysis
SPSS 11.5 software was used for data analysis. Multiple regression analysis and independent samples t-test were used to analyze the data. A P value less than 0.05 indicates a statistically significant difference.
RESULTS
Total 3315 young subjects were included in this study. These LASIK candidates consisted of 611 males (1222 eyes) and 2704 females (5407 eyes) aging from 18 to 40y (25.95±5.35y). The spherical equivalent ranged from -1.02 D to -10.37 D (-4.86±2.07 D), and the cylinder from -0.05 to -1.96 D (-0.66±0.47 D).
Higher-order Aberrations
At 6.0 mm pupil size, the RMS of the total HOAs ranged from 0.03 to 1.13 µm, with an average of 0.3977±0.0910 µm. Among the HOAs, the third- to sixth-order aberrations decreased with increasing orders. The predominant HOAs were coma (Z3−1-Z31), trefoil (Z3−3-Z33) and fourth-order spherical aberrations (Z40) (Table 1).
Table 1. RMS of the various HOAS.
| RMS | Mean±SD (µm) | Range (µm) |
| HOAs | 0.3977±0.0910 | 0.03-1.13 |
| 3rd order (R3) | 0.2100±0.0960 | 0.05-0.48 |
| 4th order (R4) | 0.151±0.0790 | 0.02-0.37 |
| 5th order (R5) | 0.0655±0.0310 | 0.03-0.27 |
| 6th order (R6) | 0.0418±0.0297 | 0.02-0.19 |
Contrast Sensitivity
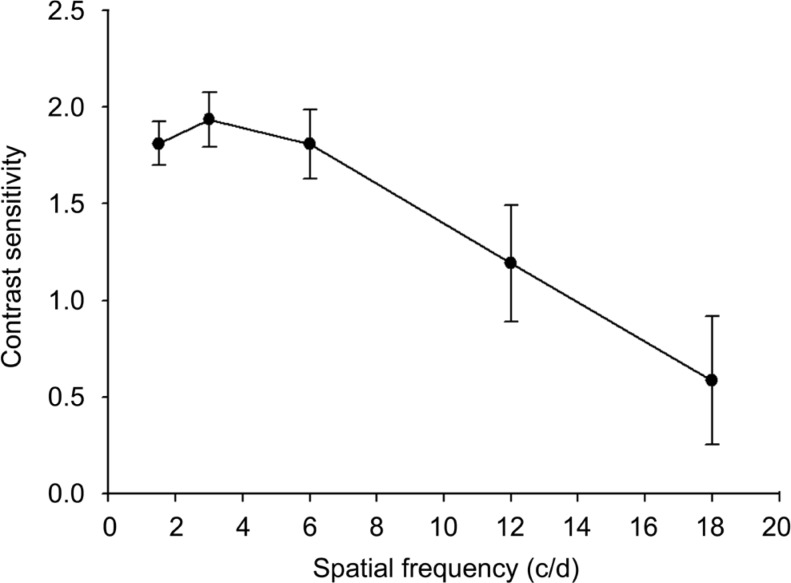
At the night mode, CS had the maximum of 1.9362±0.1397 at the low spatial frequency of 3 c/d, followed by the medium spatial frequencies of 1.5 c/d (1.8108±0.1130) and 6 c/d (1.8100±0.1789), and then the high spatial frequencies of 12 c/d (1.1922±0.3000) and 18 c/d (0.5859±0.3300), respectively (Figure 1).
Figure 1. Contrast sensitivity (mean±SD) of the myopes at different spatial frequencies.
Relation Between Contrast Sensitivity and Various Orders of Higher-order Aberrations
In these five spatial frequencies (Table 2), we did multiple regression analysis between CS and HOAs. When the spatial frequency was 1.5 c/d, the regression is CS=1.7259-0.377R3 (P<0.05). When the spatial was 3 c/d, CS=1.7971-0.7238R3 (P<0.05). When spatial frequency is 6 c/d, CS=2.0638-0.2215R3 (P<0.05). These results showed CS decreases when third order aberration increased when the spatial frequencies were 1.5 c/d, 3 c/d and 6 c/d respectively. At high spatial frequencies (12 c/d and 18 c/d), CS was not associated with the 3rd to 6th order aberrations.
Table 2. The regression equation between CS at various spatial frequencies and various HOAs.
| Spatial frequency (c/d) | Regression equation | F | P |
| 1.5 | CS=1.7300-0.4828Z31+0.5097Z3−3 +0.5586 Z5−1 | 5.554 | 0.000 |
| 3 | CS=1.0042-0.2133 Z31+0.3486 Z3−3 | 6.486 | 0.021 |
| 6 | CS=1.7996-0.5962 Z31+0.2254 Z3−3+0.2988 Z5−1+0.0226 Z6−2 | 8.884 | 0.000 |
| 12 | CS=1.2142-0.1022 Z3−3+0.4577 Z5−1 | 4.861 | 0.047 |
| 18 | CS=1.6034-0.3442 Z3−3 | 5.487 | 0.039 |
Relation Between Contrast Sensitivity and Various Modes of High-order aberrations
Further multiple regression analysis between CS and various modes of HOAs showed that CS decreased with the increase of Z31 and increased with the increase of Z3−3 and Z5−1 at the medium (1.5 c/d and 3 c/d) and low (6 c/d) spatial frequencies. At the high (12 c/d and 18 c/d) spatial frequencies, CS decreased with the increase of Z3−3 and increased with the increase of Z5−1. The regression equations were examined by F-test and all the P values were less than 0.05 (Table 2).
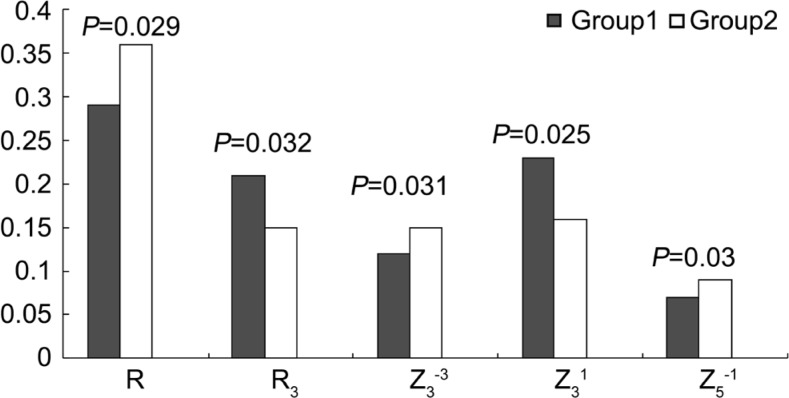
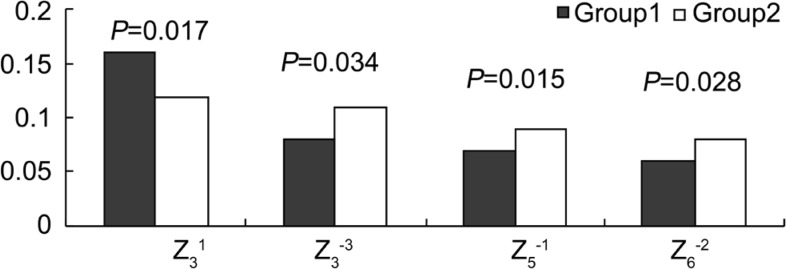
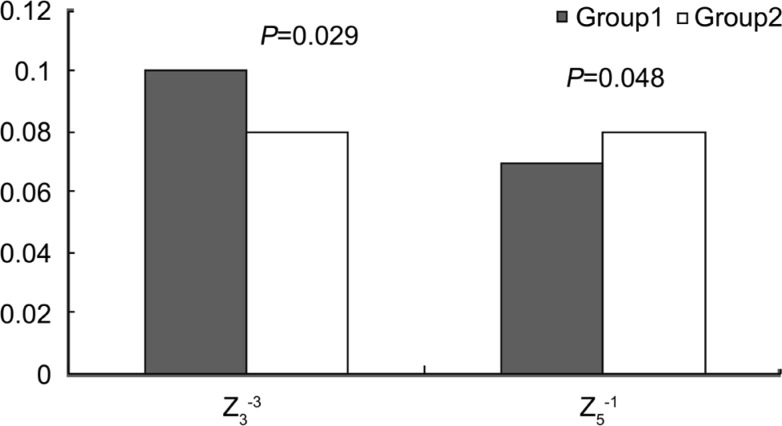
Comparisons of Aberrations Between the High and Low Contrast Sensitivity Group
The subjects were divided into two groups according to the mean CS at each spatial frequency. Group 1 included subjects whose CS was lower than the mean value, and Group 2 with CS higher than the mean value. The total aberration, total HOAs, and third-order to sixth-order aberrations were compared between the two groups. The results showed that, when the spatial frequency was 1.5 c/d and 3 c/d, the total aberration (R), R3, Z3−3, Z31 and Z5−1 were significantly different between the high and low CS groups (P<0.05). R was lower in Group 1 than in Group 2. R3 and Z31 were higher in Group 1 than that in Group 2, while Z3−3 and Z5−1 were lower in Group 1 than that in Group 2 (Figure 2). When the spatial frequency was 6 c/d, Z31, Z3−3, Z5−1, and Z6−2 were significantly different between the two groups (P<0.05). Z31 was higher in Group 1 than that in Group 2, while Z3−3, Z5−1 and Z6−2 were lower (Figure 3). When the spatial frequency was 12 c/d and 18 c/d, Z3−3 and Z5−1 were significantly different between the two groups (P<0.05). Z3−3 was higher in Group 1 than that in Group 2 while Z5−1 was lower (Figure 4).
Figure 2. Comparison of CS (1.5 c/d and 3 c/d) between Group 1 and Group 2.
Figure 3. Comparison of CS (6 c/d) between Group 1 and Group 2.
Figure 4. Comparison of CS (12 c/d and 18 c/d) between Group 1 and Group 2.
DISCUSSION
With the development of refractive surgery, people focused more and more on the visual quality rather than the naked eye vision only, CS is an important criterion for measuring visual quality. Human eye is a complicate optical system with different aberrations and these aberrations are some of the limiting factors of visual quality[14]–[17]. Traditional LASIK surgery can improve naked eye vision but there are some problems after surgery, including decrease of CS, night glare and decrease of low contrast vision. Recent studies[1],[18]–[20] have proved these problems are related to HOAs after surgery. Therefore, wavefront aberration-guided customized ablation is becoming the hot topic of the corneal refractive surgery[5],[21]–[22]. Researchers have tried to minimize HOA, improve visual quality and CS by using customized surgery. However the results show very limited visual quality improvement[23]–[25]. To solve this problem, we need to understand the relationship between CS and HOA.
In the present study, we chose CS as an indicator of visual quality. The subjects were examined with the best corrected visual acuity then HOAs are relatively dominant. Multiple regression analysis between CS at five spatial frequencies and various order aberrations showed that CS at low and medium frequencies decreased with increasing 3rd order aberrations, but not the total HOAs. It meant that 3rd order aberrations are the main factor affecting CS at low and medium frequencies. Multiple regression analysis between CS at five spatial frequencies and various modes HOAs showed that Z31, Z3−3, and Z5−1 were the main components of HOAs affecting CS. At low to medium frequencies, CS decreased with the increase in Z31 and increased with the increases in Z3−3 and Z5−1. At high frequencies, Z3−3 and Z5−1 also affected CS but with a reversal negative effects of Z3−3. The other component Z5−1 had consistent positive effects on CS at high frequencies, similar to its effects on CS at low frequencies. It seems that different components of 3rd order aberrations played different roles in affecting CS at different spatial frequencies and their combined effects deteriorate CS.
It is interesting that not all HOAs reduced CS on human eye. Some components of HOAs, such as Z3−3 and Z5−1, may improve CS at least at low to medium spatial frequencies. It indicates that the effects of individual aberrations might be different from the combined effects of individual aberrations. Various components of HOAs interact with one another[26]. Overall, Z31 and Z3−3 play a major role in affecting CS. That result is consistent with Feizi and Karimian[9] report that when the dark-adapted pupil was large, the third-order coma aberration was the main factor affecting CS.
Comparative analysis of the aberrations in the high and low CS groups showed that the total aberration of the two groups was significantly different at low spatial frequencies, and that the total aberration in the low CS group was lower than that in the high CS group. Our results were consistent with Lu et al's[13] study results, but differed from some other reports in the literature[27]–[29] showing that the greater the aberrations, the lower the CS. The third-order aberrations Z3−3, Z31 and Z5−1 were significantly different between the two groups when the specific components of aberrations were compared. The aberration component Z31 that can decrease CS was significantly higher in the low CS group than in the high CS group, leaving the aberration components Z3−3 and Z5−1 that can increase CS significantly lower than those in the high CS group. The total third-order aberrations that mainly affect CS at low frequencies were also higher than in the high CS group. Therefore, although the total aberration in the low CS group was small, aberrations contained relatively higher numbers of components that can decrease CS; thus, CS was low.
At medium and high spatial frequencies, although there was no significant difference between the two groups in the total aberration, the total aberration in the low CS group tended to be higher than that in the high CS group. At medium spatial frequencies, Z31, Z3−3, Z5−1 and Z6−2 were significantly different between the two groups, and in the low CS group the aberration component Z31 that can decrease CS was nonetheless significantly higher than in the high CS group, leaving the aberration components Z3−3, Z5−1 and Z6−2 that can increase CS significantly lower. At high spatial frequencies, Z3−3 and Z5−1 were significantly different between the two groups. Z3−3 can reduce CS, and therefore Z3−3 was significantly higher in the low CS group than in the high CS group, leaving the aberration component Z5−1 that can increase CS lower in the low CS group than in the high CS group.
Thus, the total aberration is not a main factor determining the level of CS. Significant total aberration does not necessarily mean CS will be low; and the composition of aberration plays a key role. This also suggests that we should not blindly pursue reduction of the total aberration during wavefront aberration-guided individualized ablation. Instead, we should choose to reduce the aberration components that can decrease CS, such as third-order coma and fifth-order higher-order coma.
In summary, the relationship between HOAs and CS is complex. Third-order aberrations are the main factors affecting CS, and the third-order coma can reduce both CS and visual quality. We cannot simply assume that all aberrations will lower CS and that elimination of aberrations will improve visual quality. The total aberration is not the main factor determining the level of CS. The various components of HOAs may have individual effects different from their combined effects. Some aberrations may counteract one another. Simple reduction of some aberrations may break this “balance” among them, reducing visual quality instead.
Acknowledgments
Conflict of Interest: Zhao PF, None; Li SM, None; Lu J, None; Song HM, None; Zhang J, None; Zhou YH, None; Wang NL, None.
REFERENCES
- 1.Yamane N, Miyata K, Samejima T, Hiraka T, Kiuchi T, Okamoto F, Hirohara Y, Mihashi T, Oshika T. Ocular higher-order aberrations and contrast sensitivity after conventional laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2004;45(11):3986–3990. doi: 10.1167/iovs.04-0629. [DOI] [PubMed] [Google Scholar]
- 2.Zhang J, Zhou YH, Li R, Tian L. Visual performance after conventional LASIK and wavefront-guided LASIK with iris-registration: results at 1 year. Int J Ophthalmol. 2013;6(4):498–504. doi: 10.3980/j.issn.2222-3959.2013.04.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Loukotova V, Vlkova E, Horackova M, Tokosova E, Pirnerova L, Hlinomazova Z, Dvorakova D, Nemec J. Changes of higher order aberrations and contrast sensitivity after standard photorefractive keratectomy. Cesk Slov Oftalmol. 2009;65(5):176–181. [PubMed] [Google Scholar]
- 4.Oshika T, Tokunaga T, Samejima T, Miyata K, Kawana K, Kaji Y. Influence of pupil diameter on the relation between ocular higher-order aberration and contrast sensitivity after laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2006;47(4):1334–1338. doi: 10.1167/iovs.05-1154. [DOI] [PubMed] [Google Scholar]
- 5.Jahadi Hosseini SH, Abtahi SM, Khalili MR. Comparison of higher order aberrations after wavefront-guided LASIK and PRK: one year follow-up results. J Ophthalmic Vis Res. 2016;11(4):350–357. doi: 10.4103/2008-322X.194069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marcos S. Aberrations and visual performance following standard laser vision correction. J Refract Surg. 2001;17(5):S596–601. doi: 10.3928/1081-597X-20010901-19. [DOI] [PubMed] [Google Scholar]
- 7.Ang RE, Reyes KB, Hernandez JA, Tchah H. Wavefront-guided epithelial laser in situ keratomileusis with mitomycin-C for myopia and myopic astigmatism: flap-on versus flap-off technique. J Cataract Refract Surg. 2011;37(6):1133–1139. doi: 10.1016/j.jcrs.2010.12.052. [DOI] [PubMed] [Google Scholar]
- 8.Hatch BB, Moshirfar M, Ollerton AJ, Sikder S, Mifflin MD. A prospective, contralateral comparison of photorefractive keratectomy (PRK) versus thin-flap LASIK: assessment of visual function. Clin Ophthalmol. 2011;5:451–457. doi: 10.2147/OPTH.S18967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feizi S, Karimian F. Effect of higher order aberrations on contrast sensitivity function in myopic eyes. Jpn J Ophthalmol. 2009;53(4):414–419. doi: 10.1007/s10384-009-0677-4. [DOI] [PubMed] [Google Scholar]
- 10.Oshika T, Okamoto C, Samejima T, Samejima T, Tokunaga T, Miyata K. Contrast sensitivity function and ocular higher-order wavefront aberrations in normal human eyes. Ophthalmology. 2006;113(10):1807–1812. doi: 10.1016/j.ophtha.2006.03.061. [DOI] [PubMed] [Google Scholar]
- 11.Tanabe T, Miyata K, Samejima T, Hirohara Y, Mihashi T, Oshika T. Influence of wavefront aberration and corneal subepithelial haze on low-contrast visual acuity after photorefractive keratectomy. Am J Ophthalmol. 2004;138(4):620–624. doi: 10.1016/j.ajo.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 12.Seiler T, Kaemmerer M, Mierdel P, Krinke HE. Ocular optical aberrations after photorefractive keratectomy for myopia and myopic astigmatism. Arch Ophthalmol. 2000;118(1):17–21. doi: 10.1001/archopht.118.1.17. [DOI] [PubMed] [Google Scholar]
- 13.Lu Jing, Zhou Yuehua, Zheng Yan. Influence of wavefront aberration on contrast sensitivity inmyopic eyes. Rec Adv Ophthalmol. 2007;27(9):682–684. [Google Scholar]
- 14.Schwiegerling J. Scaling pseudo-Zernike expansion coefficients to different pupil sizes. Opt Lett. 2011;36(16):3076–3078. doi: 10.1364/OL.36.003076. [DOI] [PubMed] [Google Scholar]
- 15.Zhao PF, Zhou YH, Wang NL, Zhang J. Study of the wavefront aberrations in children with amblyopia. Chin Med J (Engl) 2010;123(11):1431–1435. [PubMed] [Google Scholar]
- 16.Serrao S, Lombardo G, Ducoli P, Lombardo M. Long-term corneal wavefront aberration variations after photorefractive keratectomy for myopia and myopic astigmatism. J Cataract Refract Surg. 2011;37(9):1655–1666. doi: 10.1016/j.jcrs.2011.03.046. [DOI] [PubMed] [Google Scholar]
- 17.Jungnickel H, Babovsky H, Kiessling A, Gebhardt M, Grein HJ, Kowarschik R. Effects on vision with glare after correction of monochromatic wavefront aberrations. J Refract Surg. 2011;27(8):602–612. doi: 10.3928/1081597X-20110317-02. [DOI] [PubMed] [Google Scholar]
- 18.Liu TX, Chen YT, Dan TT, Shi R, Linghu SR, Li HX. Four-year follow-up of corneal aberrations and visual functions of myopic patients after laser in situ keratomileusis. Pak J Med Sci. 2015;31(6):1453–1456. doi: 10.12669/pjms.316.8338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Khan MS, Humayun S, Fawad A, Ishaq M, Arzoo S, Mashhadi F. Effect of wavefront optimized LASIK on higher order aberrations in myopic patients. Pak J Med Sci. 2015;31(5):1223–1226. doi: 10.12669/pjms.315.7683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chan JW, Edwards MH, Woo GC, Woo VC. Contrast sensitivity after laser in situ keratomileusis. one-year follow-up. J Cataract Refract Surg. 2002;28(10):1774–1779. doi: 10.1016/s0886-3350(02)01499-2. [DOI] [PubMed] [Google Scholar]
- 21.Moussa S, Dexl AK, Krall EM, Arlt EM, Grabner G, Ruckhofer J. Visual, aberrometric, photic phenomena, and patient satisfaction after myopic wavefront-guided LASIK using a high-resolution aberrometer. Clin Ophthalmol. 2016;10:2489–2496. doi: 10.2147/OPTH.S108002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ye MJ, Liu CY, Gu ZY, Zhao BY, Liao Y. SMILE and wavefront-guided LASIK out-compete other refractive surgeries in ameliorating the induction of high-order aberrations in anterior corneal surface. J Ophthalmol. 2016;10:870–876. doi: 10.1155/2016/8702162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Phusitphoykai N, Tungsiripat T, Siriboonkoom J, Vongthongsri A. Comparison of conventional versus wavefront-guided laser in situ keratomileusis in the same patient. J Refract Surg. 2003;19:217–220. doi: 10.3928/1081-597X-20030302-08. [DOI] [PubMed] [Google Scholar]
- 24.Mrochen M, Kaemmerer M, Seiler T. Wavefront guided laser in situ keratomileusis: early results in three eyes. J Refract Surg. 2000;16(2):116–121. doi: 10.3928/1081-597X-20000301-03. [DOI] [PubMed] [Google Scholar]
- 25.Vongthongsri A, Phusitphoykai N, Nariphapan P. Comparison of wavefront-guided customized ablation vs.conventional ablation in laser in situ keratomileusis. J Refract Surg. 2002;18(3 Suppl):332–335. doi: 10.3928/1081-597X-20020502-09. [DOI] [PubMed] [Google Scholar]
- 26.Applegate RA, Sarver EJ, Khemsara V. Are all aberrations equal? J Refract Surg. 2002;18(5):556–562. doi: 10.3928/1081-597X-20020901-12. [DOI] [PubMed] [Google Scholar]
- 27.Sakata N, Tokunaga T, Miyata K, Oshika T. Changes in contrast sensitivity function and ocular higher order aberration by conventional myopic photorefractive keratectomy. Jpn J Ophthalmol. 2007;51(5):347–352. doi: 10.1007/s10384-007-0467-9. [DOI] [PubMed] [Google Scholar]
- 28.Hiraoka T, Okamoto C, Ishii Y, Kakita T, Oshika T. Contrast sensitivity function and ocular higher-order aberrations following overnight orthokeratology. Invest Ophthalmol Vis Sci. 2007;48(2):550–556. doi: 10.1167/iovs.06-0914. [DOI] [PubMed] [Google Scholar]
- 29.Stoimenova BD. The effect of myopia on contrast thresholds. Invest Ophthalmol Vis Sci. 2007;48(5):2371–2374. doi: 10.1167/iovs.05-1377. [DOI] [PubMed] [Google Scholar]