Abstract
Objective
We attempted to clarify the factors related to the aggravation of depression in patients with subacute myelo-optico-neuropathy (SMON) caused by clioquinol intoxication more than 35 years previously.
Methods
We investigated changes in the depressive mental states that occurred with aging in 19 Japanese SMON patients (mean age, 78.3 years; range, 66-89 years) according to their scores on the Japanese version of the Zung Self-rating Depression Scale (SDS), which were obtained 3-10 years previously and their current scores. The depressive state was further evaluated using simultaneous semi-structured interviews.
Results
The depressive mental states of 6 patients, whose current total SDS scores had increased by ≥10% in comparison to the previous score, were considered to have been aggravated with aging. The mean current total SDS score of these six patients was significantly higher than the mean score of the 13 patients whose conditions were not aggravated. Among the 20 SDS questionnaires, the patients whose conditions were aggravated showed significantly higher scores in diurnal variation, sleep disturbance and weight loss. The semi-structured interviews revealed that physical disabilities due to the sequelae of SMON, a lack of acceptance of SMON, and a decline in social activities were important factors in the aggravation of their depressive mental states with aging.
Conclusion
The maintenance of social activities with public support was important for coping among Japanese SMON patients with a depressive mental state, especially those who could not walk independently or who could not go outside freely without assistance.
Keywords: subacute myelo-optico-neuropathy, SMON, Zung Self-rating Depression Scale, depressive mental state, aging
Introduction
Subacute myelo-optico-neuropathy (SMON) is a disease caused by clioquinol intoxication, which occurred in Japan between the 1950s and 1960s. It is characterized by the subacute onset of sensory and motor disturbance in the lower extremities, with visual impairment after abdominal symptoms. The pathological features are characterized by the systemic degeneration of long tracts of the spinal cord combined with polyneuropathy and optic nerve involvement (1).
When the sale of drugs containing clioquinol was banned in Japan in 1970, a sharp decrease (towards zero) in the number of new SMON patients was observed. In 2002, it was estimated that there were approximately 3,000 SMON patients in Japan. The mean age of 1,031 SMON patients was 72.9 years and there was a female predominance (male: female; 1:2.75) (2). In 2013, the number of SMON patients decreased to 1,748 (3), and the mean age was almost 80 years in 2015 (4). Recent reports have indicated that the physical conditions of SMON patients remain severe due to the sequelae of SMON as well as gerontological complications, such as cataracts, orthopedic disorders, malignant disorders and mental diseases (3,4). Almost all of the patients have suffered from characteristic unpleasant dysesthetic sensory disturbances, including pain of the lower extremities (2).
In 2008, our study on the mental states of Japanese SMON patients showed that the incidence of major depressive disorder in SMON patients was seven times higher than that in age-matched healthy individuals (5). The severity of the depressive mental states of SMON patients was the highest among the patients with intractable neurological disorders (6). In this study, we attempted to clarify the factors that may aggravate the depressive mental states of SMON patients with aging. For this purpose, we compared the results of their current and previous Self-rating Depression Scale (SDS) examinations and simultaneously conducted semi-structured interviews. We also attempted to clarify the patient's current clinical symptoms, which may be associated with their mental state.
Materials and Methods
The depressive mental states of 19 SMON patients (mean age, 78.3±6.5 years; range, 66-89 years; male, n=7; female, n=12) living in Kyoto prefecture using the Japanese version (7) of the Zung SDS (8) were evaluated 3-10 years previously (mean interval (±SD): 6.7±1.8 years) and at the time of the present study; semi-structured interviews were conducted simultaneously. The total SDS score is the sum of each score of 20 items associated with the patient's depressive mood. The score for items is graded from 1 to 4. The total SDS scores range from 20 to 80; scores of >40 reflect a depressive mental state (7).
The semi-structured interviews included the following contents; present physical conditions, adaptation to SMON disease, physical complications including gerontological complications and comorbidities of cancer, family support in daily life, leisure and social activities. The patient's current clinical symptoms were evaluated using the records of medical check-ups, which were established by the Japanese SMON Research Committee. The major neurological deficits and symptoms, such as visual impairments, walking conditions and the characteristic dysesthesia, including pain in the lower extremities, were classified into grades according to the severity of deficits and symptoms, as previously described (6). The total Barthel index (9) values (0-100) of all patients were calculated as the sum of ten questionnaires. A total Barthel index score of 100 means that a patient is independent in their daily life. The Barthel index score decreases according to the degree of disability in an individual's daily life. All of the patients in the present study had a mini-mental state examination (MMSE) (10) score of >24 points. None of the patients in the present study were treated with anti-depressants during the study period. This study was approved by the ethics committees of both Gakusai Hospital and Utano National Hospital.
The statistical analyses included Student's t-test, the Mann-Whitney U test, Spearman's rank correlation and Fisher's exact test were performed as appropriate. The statistical analyses were performed using the SPSS Statistics software program (ver. 17). The p values of <0.05 were considered to indicate statistical significance.
Results
The time course of the total SDS scores of the 19 SMON patients
In order to clarify the factors that were related to the aggravation of the patient's depressive state with aging, the 19 SMON patients were tentatively divided into two groups according to the changes in their total SDS scores. Those whose scores changed by ≥10% were classified into the aggravation group (n=6; male, n=2; female, n=4), while those whose scores changed by <10% were classified into the non-aggravation group (n=13; male, n=5; female, n=8). Six of the 19 patients were unable to walk and used wheelchairs during their daily life due to muscle weakness of both lower extremities due to the sequelae of SMON. None of the patients who used wheelchairs showed an increase in their total SDS scores at the present examinations and 4 out of 6 patients were included in the aggravation group (Figure).
Figure.
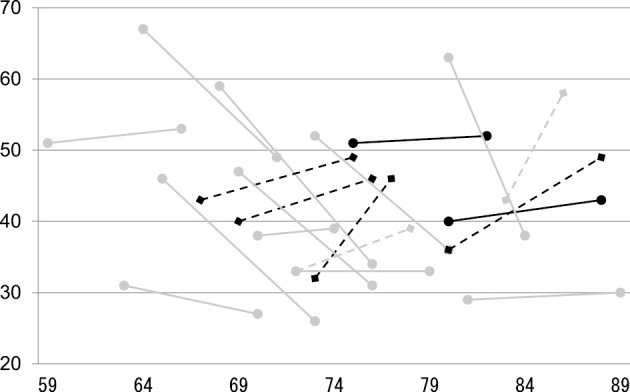
The time course of the total SDS scores in the 19 SMON patients. Dotted lines: Six patients with a ≥10% an increase in their total SDS score (aggravation group). Continuous lines: Thirteen patients in whom the total SDS score decreased or increased by <10% (non-aggravation group). Dark color: Six patients who used wheelchairs during their daily life. Vertical axis: The total SDS scores. Horizontal axis: the age of the patients at the time of the SDS examinations.
The differences in the total SDS scores and the scores of each SDS questionnaire between the aggravation and the non- aggravation groups
In the previous examinations, the mean (±SD) total SDS scores of the aggravation and non-aggravation groups were 37.8±4.9 and 46.6±12.1, respectively. The difference was not statistically significant (Student's t-test). At the current examinations, the mean total SDS scores of the aggravation and non-aggravation groups were 47.5±5.5 and 36.1±9.9, respectively. The mean total SDS score of the aggravation group was significantly higher than that of the non-aggravation group (p<0.019). A Mann-Whitney U test revealed that among the 20 items of the SDS questionnaires, the aggravation group showed significantly higher scores in diurnal variation, sleep disturbance and weight loss (Table 1). Two patients in the aggravation group and one patient in the non-aggravation group complained of severe sensory disturbance (pain and dysesthesia of lower extremities), which disturbed their sleep and caused them to experience a depressive mood in the morning.
Table 1.
The Current Scores of the 19 SMON Patients for Each of the SDS Questionnaires.
| Difference | Age | Gender | Total SDS scores |
1 | 2* | 3 | 4* | 5 | 6 | 7* | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 15 | 86 | M | 58 | 3 | 4 | 2 | 4 | 4 | 4 | 3 | 1 | 3 | 2 | 3 | 2 | 2 | 2 | 2 | 2 | 3 | 4 | 4 | 4 |
| 14 | 77 | M | 46 | 2 | 3 | 2 | 2 | 1 | 4 | 4 | 2 | 4 | 4 | 4 | 4 | 1 | 1 | 3 | 1 | 1 | 1 | 1 | 1 |
| 13 | 88 | F | 49 | 3 | 4 | 1 | 3 | 2 | 4 | 2 | 2 | 1 | 1 | 2 | 2 | 3 | 2 | 3 | 1 | 4 | 4 | 1 | 4 |
| 6 | 75 | F | 49 | 3 | 4 | 1 | 3 | 3 | 4 | 3 | 3 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 2 | 4 | 4 | 3 | 4 |
| 6 | 76 | F | 46 | 3 | 2 | 3 | 3 | 2 | 4 | 1 | 1 | 1 | 2 | 2 | 3 | 3 | 1 | 3 | 2 | 2 | 2 | 3 | 3 |
| 6 | 78 | F | 39 | 1 | 4 | 1 | 3 | 1 | 4 | 3 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 4 | 3 | 1 | 3 |
| 3 | 88 | F | 43 | 2 | 3 | 2 | 1 | 4 | 4 | 1 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 3 | 3 | 3 | 1 | 2 | 1 |
| 2 | 66 | F | 53 | 2 | 1 | 2 | 2 | 1 | 4 | 2 | 1 | 2 | 2 | 1 | 1 | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
| 1 | 82 | M | 52 | 2 | 3 | 1 | 3 | 3 | 4 | 1 | 3 | 1 | 1 | 3 | 3 | 3 | 4 | 3 | 1 | 4 | 4 | 1 | 4 |
| 1 | 89 | M | 30 | 1 | 1 | 1 | 1 | 1 | 4 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 3 | 1 | 3 | 1 | 2 | 1 | 2 |
| 1 | 74 | M | 39 | 3 | 1 | 3 | 1 | 1 | 4 | 2 | 3 | 2 | 1 | 4 | 1 | 3 | 2 | 3 | 1 | 1 | 1 | 1 | 1 |
| 0 | 79 | F | 33 | 1 | 3 | 1 | 2 | 1 | 4 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 2 | 3 | 1 | 1 | 4 | 1 |
| -4 | 70 | M | 27 | 1 | 2 | 1 | 1 | 1 | 3 | 1 | 2 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 3 | 1 | 1 | 1 | 1 |
| -16 | 76 | F | 31 | 2 | 3 | 1 | 1 | 1 | 4 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 2 | 2 | 1 | 2 |
| -16 | 80 | F | 36 | 1 | 1 | 1 | 3 | 1 | 4 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 2 | 3 | 3 | 3 | 1 | 3 |
| -18 | 71 | F | 49 | 3 | 4 | 2 | 2 | 1 | 4 | 2 | 1 | 2 | 2 | 3 | 3 | 1 | 2 | 1 | 4 | 2 | 4 | 2 | 4 |
| -20 | 73 | M | 26 | 1 | 1 | 2 | 1 | 1 | 4 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 |
| -25 | 76 | F | 34 | 2 | 3 | 2 | 1 | 1 | 4 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 2 | 1 | 1 | 3 | 1 | 3 |
| -25 | 84 | F | 38 | 2 | 3 | 2 | 2 | 1 | 4 | 1 | 1 | 1 | 1 | 1 | 2 | 3 | 2 | 3 | 3 | 1 | 2 | 1 | 2 |
The patients were arranged according to the degree of difference between their previous and current total SDS scores (top to bottom). The total SDS scores of the upper six patients increased by ≥10% in comparison to the previous examinations. The depressive mental states of these patients were considered to be aggravated. The remaining 13 patients in whom the total SDS scores increased by <10% were classified into the non- aggravation group. The numbers of the uppermost line indicate the 20 SDS questionnaires (8): 1: depressed affect, 2*: diurnal variation, 3: crying spells, 4*: sleep disturbance, 5: decreased appetite, 6: decreased libido; 7*: weight loss, 8: constipation, 9: tachycardia, 10: fatigue, 11: confusion, 12: psychomotor retardation, 13: psychomotor agitation, 14: hopelessness, 15: irritability, 16: indecisiveness, 17: personal devaluation, 18: emptiness, 19: suicidal rumination, 20: dissatisfaction. The asterisks indicate the items in which significant differences were observed between two groups of patients (Mann-Whitney U test).
The results of the semi-structured interviews
The content of the semi-structured interviews was summarized into five categories as follows: walking condition, acceptance of SMON disease, medical complications such as cancer, assistance of family members and involvement in various social activities. The mean age of the patients in the aggravation group (80.0±5.5 years) was greater than that of the patients in the non-aggravation group (77.5±7.0 years); however, the difference was not statistically significant.
The percentages of patients in each of the categories are shown in Table 2. Asterisks indicate the categories for which a significant difference between the two groups was identified by Fisher's exact test. Regarding the physical condition in relation to walking, 4 (67%) of the 6 patients in the aggravation group used a wheelchair, while 11 (85%) of the 13 patients in the non-aggravation group could walk without assistance. A significantly larger percentage of the patients in the aggravation group were wheelchair-dependent (Table 2).
Table 2.
A Summary of the Semi-structured Interviews.
| Number of patients |
Age (mean±SD) |
Wheelchair | Acceptance of SMON disease |
Comorbidity of cancer |
Single life |
Social activity |
|
|---|---|---|---|---|---|---|---|
| Aggravation group | 6 | 80.0±5.5 | 67%* | 50%* | 33% | 33% | 33%* |
| Non-aggravation group | 13 | 77.5±7.0 | 15% | 100% | 31% | 15% | 92% |
Asterisks indicate a significant difference between the aggravation and non-aggravation groups (Fisher’s exact test).
Regarding the acceptance of SMON disease, all of the non-aggravation patients had changed their minds and had been able to overcome their anger toward the government in relation to the harmful effects and the sequelae caused by clioquinol intoxication in order to live with the disease. In contrast, most of the patients in the aggravation group continued to feel anger towards the Japanese Government and the responsible pharmaceutical companies.
Regarding physical complications, patients in both groups complained equally of a decrease in their physical and mental strength, and were worried about an increase in their physical disability with aging. Patients in both groups were undergoing treatment for hypertension, bone fracture or other orthopedic pain. Two patients (33%) in the aggravation group and 4 patients in the non-aggravation group (31%) had suffered from or were suffering from cancer (Table 2). The patients in the aggravation group complained that they could not go outside freely without assistance and were anxious about living alone. They also worried about their future lifestyle and were concerned that they might require more help in the near future. Although a larger percentage of the patients in the aggravation group was living alone (33%), the percentage of patients in the non-aggravation group (15%) was not significantly different (Table 2). One patient in the non-aggravation group reported that the concerns about living alone were overcome by spending time with relatives. Another patient in the non-aggravation group reported that their depressive mental state was related to the hardship they experienced in association with the various symptoms of SMON and that they felt guilty for depending on their family members for daily physical support.
Most of the patients in both groups hoped to maintain their present physical conditions without further aggravation and to receive greater economic support from the government to support the costs of daily life. Twelve patients (92%) in the non-aggravation group engaged in work or attended social activities. In contrast, only two patients (33%) in the aggravation group attended social activities; the difference was statistically significant (Table 2).
The correlations between the total SDS scores and the current clinical parameters
Among the current clinical parameters, the total SDS scores were not correlated with the severity of visual acuity disturbance, age or the age at the onset of SMON. The total Barthel index score, the going outdoors score and the severity of walking disturbance showed a significant negative correlation with the total SDS scores (Spearman's rank correlation coefficient; Table 3). These results suggested that physical disabilities that affected a patient's ability to go outside freely were closely related with a depressive mental state. Although the degree of unpleasant dysesthetic sensory symptoms of the lower extremities (dysesthesia of legs) was not correlated with the total SDS scores (γs=-0.121), a subanalysis of the female patients revealed that the degree of unpleasant sensory disturbance was significantly correlated with the total SDS score (γs=-0.603).
Table 3.
The Spearman’s Rank Correlation Coefficients (γs) between the Current Clinical Parameters and the Total SDS Scores of the 19 SMON Patients.
| Present clinical parameters | γs | |
|---|---|---|
| Barthel index score | -0.602 | ** |
| Gait disturbance | -0.553 | * |
| Going outdoors | -0.639 | ** |
| Visual impairment | -0.216 | |
| Dysesthesia of legs | -0.121 | |
| Age | 0.103 | |
*: p<0.05, **: p<0.01
In summary, most of the patients in the aggravation group used wheelchairs, found it difficult to accept SMON and had less opportunity to participate in social activities due to the lack of both independent walking and the ability to go outside freely.
Discussion
The depressive mental states of 6 out of 19 SMON patients were aggravated. Since the total SDS values and the mean scores of each of the 20 SDS questionnaires decreased after the treatment of depressive disorders (8), the SDS is considered to be a valid and sensitive measure of the clinical severity of depression (11). The same decrement of the total SDS scores after treatment was observed when the Japanese version of the SDS (7) was used. Thus, it is appropriate to define an increase in the total SDS scores as an aggravation of the depressive mental state.
Semi-structured interviews were conducted with all patients to clarify the factors that were associated with the aggravation of their depressive mental state that occurred with aging. Based on these interviews, three categories were frequently observed in the patients of the aggravation group: the restriction of their daily activities because they required the use of a wheelchair, difficulty in accepting SMON disease, and a lack of social activities through work or hobbies. The correlation study between the patient's current clinical conditions and the total SDS scores showed that their dependence on assistance for walking and the decreased frequency of outdoor activities due to their physical disabilities were also closely associated with high total SDS scores. The characteristic findings of this study were that none of the patients who required wheelchairs due to their physical disabilities showed an improved depressive state with aging, and that the depressive state of some of these patients was aggravated with aging. The reasons why the depressive states of some patients improved without anti-depressant treatment were not clear in this study. The sharing of the individual mental problems that were observed in this study with medical doctors and psychological therapists, who have a good understanding SMON disease, might have helped to soften their hard feelings and in its turn ameliorate their depressive mental state.
In the female SMON patients, the unpleasant dysesthetic sensory disturbance of the lower extremities was significantly correlated with high total SDS scores. This is in line with our previous results using Beck's Depression Inventory Questionnaires (5). The peculiar dysesthetic sensory disturbance, including constant pain in the lower extremities that continues throughout day and night is a characteristic symptom of SMON and is observed in almost all patients (97.6%) (2). The lack of correlation between sensory symptoms and the total SDS scores in male patients might be due to the small number of male SMON patients. It is conceivable that the unpleasant sensory symptoms in SMON patients could cause sleep disturbance and other depressive symptoms, since physical health impairments (including pain) have already reported to be associated with the depressive mental states of elderly individuals (12). In addition to physical impairments, a lack of social activities was found to be an important factor for the aggravation of the depressive state in the SMON patients.
The degree of depression was most severe among SMON patients with similar physical disabilities who suffered from various intractable nervous diseases, such as multiple sclerosis, amyotrophic lateral sclerosis, multiple system atrophy and Parkinson disease (6). An investigation of the strategies that some SMON patients employed for coping with their depressive mental state through discussions with medical staff who have a good understanding of the disease and an analysis of the individual mental and physical backgrounds would also be helpful in the treatment of depressive patients with other intractable diseases. Since many causes of depression exist in individual SMON patients, further studies that include a greater number of SMON patients will be necessary to clarify the factors that aggravate their depressive mental states.
The authors state that they have no Conflict of Interest (COI).
Financial Support
This study was supported by a Grant-in-Aid from the Ministry of Health, Labor and Welfare, Japan, for Research on Intractable Diseases.
References
- 1. Sobue I. Clinical aspects of subacute myelo-optico-neuropathy (SMON). In: Intoxications of the Nervous System: Part 2. Handbook of Clinical Neurology, Vol. 37. Vinken PJ, et al. , Eds. North-Holland, Amsterdam, 1979: 115-139. [Google Scholar]
- 2. Konagaya M, Matsumoto A, Takase S, et al. Clinical analysis of longstanding subacute myelo-optico-neuropathy: sequelae of clioquinol at 32 years after its ban. J Neurol Sci 218: 85-90, 2004. [DOI] [PubMed] [Google Scholar]
- 3. Konagaya M. SMON: toxicity of clioquinol and the status quo. Brain Nerve 67: 49-62, 2015. [DOI] [PubMed] [Google Scholar]
- 4. Konagaya M. Present conditions of Japanese SMON patients from the annual medical checkup in 2015. In: Annual Report of SMON Research Committee in 2016. Konagaya M, Ed. SMON Research Committee supported by the Ministry of Health, Labor and Welfare of Japan, Nagoya, 2016: 25-47. [Google Scholar]
- 5. Konishi T, Hayashi K, Hayashi M, et al. Depression in patients with subacute myelo-optico-neuropathy (SMON). Intern Med 47: 2127-2131, 2008. [DOI] [PubMed] [Google Scholar]
- 6. Konishi T, Fujita M, Hayashi K. Depressive mental states in SMON patients. In comparison with various intractable nervous diseases and healthy people. J Kyoto Medical Association 64: 75-79, 2017. [Google Scholar]
- 7. Fukuda K, Kobayashi S. Japanese version of SDS (self-rating depression scale). Sankyobo, Kyoto, 1983. [Google Scholar]
- 8. Zung WWK. A self-rating depression scale. Arch Gen Psychiatry 12: 63-70, 1965. [DOI] [PubMed] [Google Scholar]
- 9. Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J 14: 61-65, 1965. [PubMed] [Google Scholar]
- 10. Tombaugh TN, McIntyre NJ. The mini-mental state examination:a comprehensive review. J Am Geriatr Soc 40: 922-935, 1992. [DOI] [PubMed] [Google Scholar]
- 11. Biggs JT, Wylie LT, Ziegler VE. Validity of the Zung Self-rating Depression Scale. Br J Psychiatry 132: 381-385, 1978. [DOI] [PubMed] [Google Scholar]
- 12. Blazer D. Williams CD: Epidemiology of dysphoria and depression in an elderly population. Am J Psychiatry 137: 439-444, 1980. [DOI] [PubMed] [Google Scholar]


