Abstract
A 66-year-old man presented to his previous physician with epigastric discomfort in 2014. He was then referred to our hospital due to suspected primary malignant melanoma of the esophagus (PMME). A biopsy showed atypical cells containing melanin granules. A diagnosis of PMME was thus made. We investigated the endoscopic findings of the previous physician, which revealed a black point-like pigmentation at the same site since 2009. In 2010, black pigmentation was also observed at the same site. Although esophageal melanosis was suspected, no biopsy was performed. This case demonstrates the process by which esophageal melanomas develop into malignant melanomas.
Keywords: primary malignant melanoma of the esophagus, PMME, malignant melanoma
Introduction
Primary malignant melanoma of the esophagus (PMME) is a rare disease representing from 0.1% to 0.2% of all primary esophageal cancers (1). Due to its rarity, there are few reports on the oncogenesis of PMME. Esophageal melanosis has been suspected to be a precursor lesion of PMME. We herein report a case that supports this notion.
Case Report
A 66-year-old man with epigastric discomfort visited his previous physician in October 2014. Esophagogastroduodenoscopy (EGD) revealed a black uplift in the mid-thoracic esophagus in November. He was then referred to our hospital. He had no pigmentation in the mouth, eyes, anus, rectal mucosa, or anywhere on the skin of his body. His superficial lymph nodes were not palpable. Blood tests were within the normal range. EGD performed in our department showed an elevated lesion of lobulated-black tone in the middle thoracic esophagus, at a site 37-43 cm from the incisors, some of which was accompanied by white moss (Fig. 1A). Endoscopic ultrasonography (EUS) revealed a low echoic lesion, a solid tumor mass, in the esophageal wall (Fig. 1B). An esophageal barium examination showed rising steep ridge tumors that were localized in the chest, in the mid-esophagus (Fig. 1C). Computed tomography revealed a mild, densely stained esophageal tumor in the mid-thoracic esophagus. The diagnosis was made based on the findings of histologic and immunohistochemical examinations. Histologically, the atypical cells containing melanin granules were recognized, that stained positive for HMB45 (Fig. 2). Positron emission computerized-tomography revealed the accumulation of SUVmax16.7 in the mid-thoracic esophagus. In addition, hot spots were identified at the outer portions of the right eighth rib and left fourth rib as well as the left iliac sacroiliac joint surface. They were considered to represent multiple bone metastases.
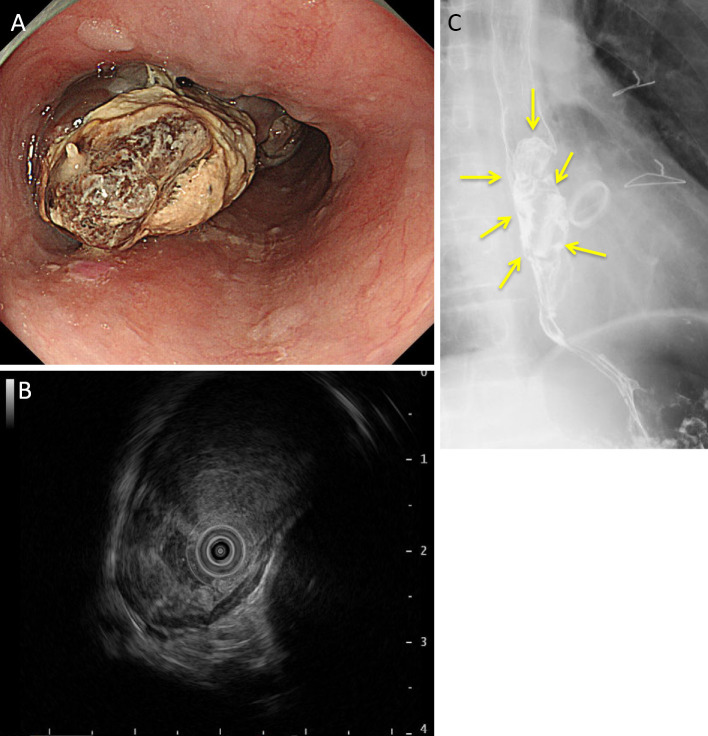
Figure 1.
Endoscopic image (A), endoscopic ultrasonography (B), and esophageal barium examination (C) of the patient. An elevated lesion with an lobulated-black tone in the mid-thoracic esophagus at a site 37-43 cm from the incisors was revealed, with some areas with a white moss appearance (A). Endoscopic ultrasonography demonstrated a low echoic legion, a solid tumor mass, in the esophageal wall (B). Esophageal barium examination showed rising, steep ridged tumors that were localized in the mid-esophagus of the chest (C).
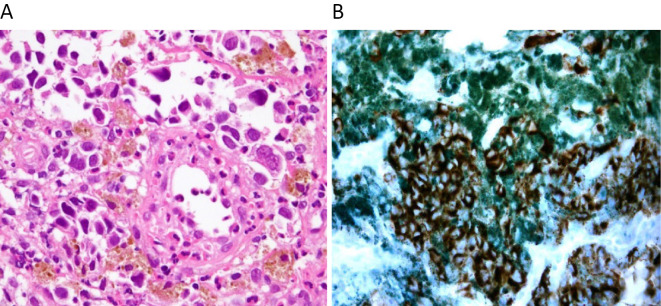
Figure 2.
Histologic image of biopsy specimens. The atypical cells containing melanin granules were identified (A). HMB45 staining was positive (B).
This case was determined to be inoperable. Dacarbazine therapy was started in January 2015, but two courses of this therapy were not effective. The administration of Nivolumab was initiated in March of the same year. However, the occurrence of an adverse reaction of severe diarrhea led to the discontinuation of Nivolumab treatment. The therapeutic strategy was shifted to palliative treatment, and the patient died in August 2015.
This case had been regularly followed up by annual endoscopy from 2009 for a bleeding gastric ulcer. According to the report of the previous physician, a black nodule was recognized in the mid-thoracic esophagus in 2009. The position is considered to be the same site as that of the PMME. It measured 3 mm in size, and the lesion was flat (Fig. 3A). In 2010, a nodule at the same site had grown to 5 mm in size and it had a slightly raised shape. There was a thin mottled black pigmentation around the nodule (Fig. 3B and C). Apart from the features mentioned above, there were no abnormalities in the esophagus. The previous physician suspected the nodule could be esophageal melanosis, but a biopsy was not performed because they could not rule out the possibility of hemangioma. They regarded the lesion as a benign finding and scheduled follow-up EGD a year later. The following year, the patient could not visit his physician due to the Great East Japan Earthquake. Eventually, a PMME tumor developed at the same site in 2014 (Fig. 3D).
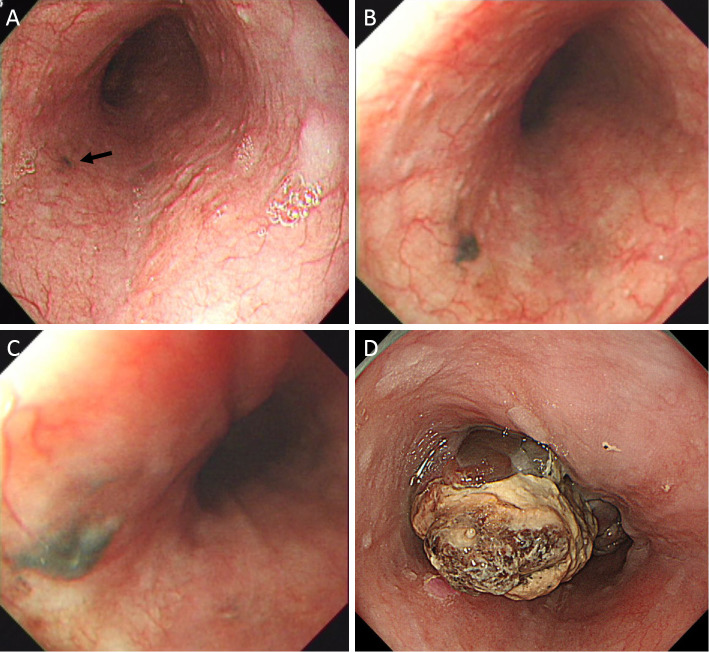
Figure 3.
The time course for tumor progression from a black nodule to PMME. A black nodule was recognized in the mid-thoracic esophagus in 2009 (A). In 2010, a nodule at the same site had grown to 5 mm in size with a slightly raised profile (B), and there was thin mottled black pigmentation around the nodule (C). PMME was confirmed in the mid- thoracic esophagus in 2014 (D).
Discussion
PMME occurs predominantly in males, with a 2.02:1 male-to-female ratio, and the prevalent age is 60.5 years old. It is most commonly located in the middle and lower third of the esophagus. Most patients complain of dysphagia (2).
EGD is useful for the diagnosis of PMME. Using EGD, an elevated and pigmented tumor can be found, sometimes accompanied by ulcers. Although the black tone is a well-known characteristic of PMME, some have various colors such as purple, brown and white (3). Melanin spots and a submucosal tumor-like lesion around the tumor sometimes indicate intramural metastasis, which can contribute to the diagnosis. Endoscopic ultrasonography has been reported to demonstrate an iso-hypoechoic lesion (4).
The diagnosis in this case was based on the pathological histology. However, biopsies obtained by EGD are difficult to diagnose because more than 50% of the primary lesions of PMME are present in the submucosal layer (5). Immunohistochemical staining leads to a definitive diagnosis of PMME. S-100 protein, melan A and HMB 45 are positive indicators (3). In this case, HMB 45 was positive. Although the risk of seeding by biopsy has been feared, there has so far been no report of this (6).
Esophageal melanosis is observed 7.7% of healthy populations (7); it is more commonly observed in men and tends to be present in the middle and lower third of the esophagus (8). The gender differences and preferential site of esophageal melanosis are consistent with PMME. In addition to these common characteristics, 25-30% of PMME are accompanied by esophageal melanosis (9,10). These findings indicate that esophageal melanosis is a precursor lesion of PMME. However, only one case has so far been reported in which melanosis progressed to PMME (11). In the current case, melanosis was observed in the middle esophagus 5 years earlier and it eventually progressed to PMME at an inoperable stage. Therefore, this is only the second known case report. What is common in these two cases is that the melanosis has grown over time. Indeed, a growing melanosis is considered to be a sign of malignancy. Ohashi et al. noted that hyperplastic changes, acanthosis and chronic esophagitis are involved in this growth. For instance, chronic stimulation by acid regurgitation may cause hyperplastic changes and chronic inflammation in the mucosal membrane, leading to melanosis growth and progression to a precursor lesion of PMME (11).
Biopsies from the black spot were not taken by the previous physician in this patient in both 2009 and 2010, hence, the diagnosis of melanosis was not histologically confirmed in this case. However, the typical black pigmentation is a well-recognized characteristic feature of esophageal melanosis (8), hence histological confirmation of small black pigmentation is not a general procedure that is carried out when making a diagnosis of melanosis. On the other hand, a lack of histological examination prior to PMME development could raise the possibility that PMME had already existed in the initial small black pigmentation rather than a transformation from melanosis to PMME during the 5 year observation period. However, we believe that such a scenario seems unlikely because it is reported that the survival time for patients with PMME rages from 10 to 15 months once the malignant neoplasia develops (12). Esophageal melanosis is a very common finding in ordinary endoscopic examinations, hence we think that it is not practical to routinely take biopsies from all sites of black pigmentation at every follow-up EGD. Nevertheless, taking biopsies is required to detect PMME at an early stage when morphological changes are observed at the follow-up EGD. We retrospectively considered that biopsies should have been taken at the second EGD (2010) in this case since the size of the melanosis seemed to have slightly increased compared with that observed one year previously (2009).
Complete excision by surgical resection is the standard treatment. Its prognosis is low, with a 1-year survival rate of 74.1% and 5-year survival rate of 30.7% (2). Although chemotherapy, chemoradiotherapy, and endocrine therapy are reported as other therapies, there has been no report that such therapies extended either the overall survival or progression-free survival. However, expectations for Nivolumab immunotherapy have recently been increasing. Although it had to be discontinued due to negative side effects in this case, Nivolumab administered to cutaneous malignant melanoma improved both the overall survival and progression-free survival better than conventional chemotherapy (13). There are no reports regarding the administration of Nivolumab to PMME cases, so further investigations are required.
Currently, no effective treatment has been established for advanced PMME. Thus, an early diagnosis and timely treatment are desirable, and as esophageal melanosis is considered to be a precursor lesion of PMME, it should be observed by EGD with regularity (namely, at least an annual follow-up EGD). In particular, melanosis with chronic inflammation and mucosal hypertrophy of the background mucosa, melanosis of the lower esophagus exposed to a stimulus, and melanosis which grows over time requires careful observation with histological examinations when appropriate.
Conclusion
We examined the case of a precursor lesion of PMME that was confirmed by endoscopy. Esophageal melanosis should therefore be monitored during follow-up as it may develop into PMME.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Bisceglio M, Perri F, Tucci A, et al. Primary malignant melanoma of the esophagus: a clinicopathologic study of a case with comprehensive literature review. Adv Anat Pathol 18: 235-252, 2011. [DOI] [PubMed] [Google Scholar]
- 2. Sabaanathan S, Eng J, Pradhan GN. Primary malignant melanoma of the esophagus. Am J Gastroenterol 84: 1475-1481, 1989. [PubMed] [Google Scholar]
- 3. Joob AW, Haines GK 3rd, Kies MS, et al. Primary malignant melanoma of the esophagus. Ann Thorac Surg 60: 217-222, 1995. [PubMed] [Google Scholar]
- 4. Namiento T, Koito K, Ambo T, et al. Primary malignant melanoma of the esophagus: diagnostic value of endoscopic ultrasonography. Am Surg 62: 716-718, 1996. [PubMed] [Google Scholar]
- 5. Dematos P. Primary malignant melanoma of the esophagus. J Surg Oncol 66: 201-206, 1997. [DOI] [PubMed] [Google Scholar]
- 6. Kato N, Kamio K, Yamashita T, et al. Primary malignant melanoma of the esophagus. Gan No Rinsho 32: 1459-1465, 1986. (in Japanese, Abstract in English). [PubMed] [Google Scholar]
- 7. Ohashi K, Kato Y, Knanno J, et al. Melanocytes and melanosis of the oesophagus in Japanese subjects: analysis of factors effecting increase. Virchows Arch A Pathol Anat Histopathol 417: 137-143, 1990. [DOI] [PubMed] [Google Scholar]
- 8. Chang F, Deere H. Esophageal melanocytosis morphologic features and review of the literature. Arch Pathol Lab Med 130: 552-557, 2006. [DOI] [PubMed] [Google Scholar]
- 9. Volpin E, Sauvanet A, Couvelard A, et al. Primary malignant melanoma of the esophagus: a case report and review of the literature. Dis Esophagus 15: 244-249, 2002. [DOI] [PubMed] [Google Scholar]
- 10. Lohmann CM, Hwu WJ, Iverson K, et al. Primary malignant melanoma of the oesophagus: a clinical and pathological study with emphasis on the immunophenotype of the tumours for melanocyte differentiation markers and cancer/testis antigens. Melanoma Res 13: 595-601, 2003. [DOI] [PubMed] [Google Scholar]
- 11. Oshiro T, Shimoji H, Matsuura F, et al. Primary malignant melanoma of the esophagus arising from a melanotic lesion: report of a case. Surg Today 37: 671-675, 2007. [DOI] [PubMed] [Google Scholar]
- 12. Herman J, Duda M, Lovecek M, et al. Primary malignant melanoma of the esophagus treated by endoscopic ablation and interferon therapy. Dis Esophagus 14: 239-240, 2001. [DOI] [PubMed] [Google Scholar]
- 13. Robert C, Long GV, Brady B, et al. Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med 372: 320-330, 2015. [DOI] [PubMed] [Google Scholar]