Abstract
Background
Transition from at-risk state to full syndromal mental disorders is underexplored for unipolar and bipolar disorders compared with psychosis.
Aims
Prospective, trans-diagnostic study of rates and predictors of early transition from sub-threshold to full syndromal mental disorder.
Method
One-year outcome of 243 consenting youth aged 15–25 years with a sub-syndromal presentation of a potentially severe mental disorder. Survival analysis and odds ratio (OR) for predictors of transition identified from baseline clinical and demographic ratings.
Results
About 17% (n=36) experienced transition to a major mental disorder. Independent of syndromal diagnosis, transition was significantly more likely in individuals who were NEET (not in education, employment or training), in females and in those with more negative psychological symptoms (e.g. social withdrawal).
Conclusions
NEET status and negative symptoms are modifiable predictors of illness trajectory across diagnostic categories and are not specific to transition to psychosis.
Declaration of interest
I.B.H. has been a Commissioner in Australia’s National Mental Health Commission since 2012. He was a board member of headspace: National Youth Mental Health Foundation until January 2012. He has led a range of community-based and pharmaceutical industry-supported depression awareness and education and training programmes. He has led projects for health professionals and the community supported by governmental, community agency and pharmaceutical industry partners (Wyeth, Eli Lilly, Servier, Pfizer, AstraZeneca) for the identification and management of depression and anxiety. He has received honoraria for presentations of his own work at educational seminars supported by a number of non-government organisations and the pharmaceutical industry (including Servier, Pfizer, AstraZeneca and Eli Lilly). He is a member of the Medical Advisory Panel for Medibank Private and also a board member of Psychosis Australia Trust. He leads an investigator-initiated study of the effects of agomelatine on circadian parameters (supported in part by Servier) and has participated in a multicentre clinical trial of the effects of agomelatine on sleep architecture in depression and a Servier-supported study of major depression and sleep disturbance in primary care settings.
Copyright and usage
© The Royal College of Psychiatrists 2017. This is an open access article distributed under the terms of the Creative Commons Non-Commercial, No Derivatives (CC BY-NC-ND) license.
Depression, psychosis and bipolar disorders are three of the four most burdensome conditions in young people aged under 25 years.1 Furthermore, these three major mental disorders all demonstrate a peak age at onset of between 15 and 25 years.2 Evidence clearly indicates that individuals at clinical high risk of developing full syndromal mental disorders often report sub-syndromal depressive, hypomanic or psychotic-like presentations in the months or even years prior to the first illness episode that meets diagnostic criteria for a specific, major mental disorder.3,4 Early intervention services that initially targeted those at risk of psychosis afforded an opportunity to undertake a number of prospective studies in populations with sub-threshold symptoms. This research, alongside several recent meta-analyses, highlights that over the course of 1 year, transition to a psychotic episode meeting diagnostic criteria occurs in about 10–20% of individuals presenting with a range of sub-syndromal symptoms (usually referred to as an ultra-high risk state).5,6 Furthermore, some (but not all) treatment studies suggest transitions may be delayed or prevented by biopsychosocial interventions with a high benefit-to-risk ratio.7
The philosophy underpinning early intervention for psychosis (EIP) also fostered the adoption of clinical staging models in psychiatry. These are an accepted element of research and clinical practice in general medicine, especially for the diagnosis and treatment of chronic disorders. Importantly, clinical staging determines where an individual is ‘located’ on a continuum from an asymptomatic but ‘at-risk’ state (stage 0) through to end-stage disease (stage 4). In mental health, presentations meeting diagnostic criteria for a specific disorder are usually classified as stage 2, whilst sub-syndromal presentations (such as ultra-high risk states, attenuated psychotic symptoms or sub-threshold manic symptoms) are usually classified as stage 1b. Research in youth mental health services8 has demonstrated that staging models are not only useful to the study of the evolution of the early stages of psychosis but can also be applied to youth with sub-threshold syndromes of unipolar or bipolar disorders in addition to psychotic disorders.9–11
A major gap in knowledge, however, is what factors predict which individuals across all high-risk groups will progress to discrete syndromal-level major mental disorders, and over what time periods such transitions will occur. This information is key to improved targeting of interventions, as well as clarifying whether any predictors of transition are specific to any type of disorder. Recent meta-analyses suggest that the prediction of transition to psychosis on the basis of psychotic-like symptoms alone may be less robust than models that incorporate baseline assessment of other symptoms (such as depression, distress or disorganisation),12 social adjustment or functioning,12 or employment13–16 or NEET status (not in education, employment or training).17 However, these publications focus only on risk of transition to psychosis. Although this is undoubtedly an important group, such cases actually constitute a minority of the help-seeking adolescents and young adults who present to youth mental health services.9,18
Given recent findings that youth with emerging mood disorders are highly impaired and often experience outcomes similar to those of recent-onset psychosis, this study examines trans-diagnostic transitions from sub-threshold (stage 1b) to threshold caseness (stage 2) for individuals with sub-syndromal unipolar, bipolar and psychotic disorders. The study hypothesises that social as well as clinical characteristics of individuals presenting to youth mental health services for the first time (e.g. demography, symptom severity, functional impairment and NEET status) can help to predict the likelihood of and time to early transition across diagnostic groups and that the predictors of transition identified in studies of individuals at clinical high risk of developing psychosis will also predict disease progression in unipolar and bipolar disorders.
Method
Sample
With ethics approval from The University of Sydney Human Ethics Board, we obtained written consent from participants (or their guardians for those under 18 years) to collect their de-identified assessment details in a database for use in a series of linked research studies. All patients aged 15–25 years who presented to headspace19 Campbelltown, a specialised, primary-level early intervention youth mental health service in outer metropolitan Sydney, Australia, participated in this study. Young people and their families can self-refer, which results in initial presentations across the spectrum of mental-ill health. Some of these young people require immediate referral to higher tier mental health services, and others continue to be managed within the service. Around 1200 young people were managed between January 2014 and June 2015, and all were approached to be included in the database.
To be included in this study, the individual was required to meet the criteria at baseline assessment for a sub-syndromal presentation of a potentially severe mental disorder (clinical stage 1b) as described in detail in Hickie et al.18 To briefly summarise the procedure, allocation of a case to a particular clinical stage is undertaken at regular multidisciplinary clinical consensus meetings involving senior mental health professionals (consultant psychiatrists or senior clinical psychologists). Stage 1b criteria identify young people with attenuated, ambiguous, sub-threshold or sub-syndromal presentations that do not meet current traditional diagnostic criteria for a psychotic or severe mood disorder, but who are deemed to be at clinical high-risk for the development of a major depressive, bipolar or psychotic disorder. No other exclusion criteria applied. Of all who met the criteria for study inclusion (n=255), only 15 declined participation and they were provided with the same level of clinical care and treatment as those who consented.
Baseline assessment
Baseline data included current age, gender and an estimate of the time since onset of any symptoms or psychological problems (age at current presentation minus self-reported age at first-ever onset of self-reported psychological symptoms determined at the initial clinical assessment). Two measures were used to assess current symptom levels: the 10-item version of Kessler Scale for the assessment of psychological distress20 (K-10 scores range from 10 to 50, with 10 indicating no distress and 50 indicating severe distress) and the expanded version of the Brief Psychiatric Rating Scale (BPRS), completed by a psychiatrist or clinical psychologist. The latter comprises of six subscales21 with scores reflecting the main forms of psychopathology observed in mental disorders, namely BPRS-affect (anxiety, guilt, depression, somatic; score range: 4–28), BPRS-positive symptoms (thought content, conceptual disorganisation, hallucinations, grandiosity; score range: 4–28), BPRS-negative symptoms (blunted affect, emotional withdrawal, motor retardation; score range: 4–28), BPRS-resistance (hostility, uncooperativeness, suspiciousness; score range: 3–21), BPRS-activation (excitement, tension, mannerisms-posturing; score range: 3–21) and BPRS-suicidality (score range 1–7). Higher scores on each subscale indicated higher levels of symptoms. Two measures of social functioning were included: the observer-rated Social and Occupational Functioning Assessment Scale22 (SOFAS, with scores ranging from 0 to 100 and higher scores indicating better functioning) and an objective measure of current education or employment engagement, namely NEET status (NEET= not in employment, education or training) asking young people if they were employed/unemployed or if they were attending school or other educational or training courses or if they were not engaged in education or training.
Follow-up assessments
Baseline measures were repeated every 3 months for 1 year. The primary outcome measure was clinical stage at follow-up (e.g. persistent stage 1b representing attenuated or sub-threshold caseness; development of a syndrome meeting diagnostic criteria for a stage 2 unipolar, bipolar or psychotic disorder as determined by the consensus method outlined above). Time to transition to stage 2 was also recorded.
Statistical analyses
Analysis was performed using SPSS 22.0, with statistical significance set at P<0.05 for all analyses.
First, we assessed missing values. There was a small amount of random missing data from the baseline assessments (<5%). Given the low level of missing values, items were replaced with the sample mean scores. If NEET status was not recorded, we assumed the individual was not NEET (as our previous research indicates that this is the most common reason for exclusion of recording this information17,23). If no information was recorded to indicate progression to stage 2 illness and no date of transition was provided, we assumed the individual had remained at stage 1b throughout the 1-year follow-up.
Survival analysis was undertaken to determine time to transition to stage 2 and to identify variables associated with transition by 12 months. Cox’s time-dependant regression analysis of survival time was employed, with age, gender (reference category: male) and sub-threshold group (categorised as stage 1b depressive, bipolar or psychotic disorder) included at step one of the model to allow us to first take into account the possible influence on survival time of demographic factors and putative diagnosis/illness trajectory. Symptom ratings (K-10 and BPRS subscale scores), SOFAS score and NEET status (reference category: not NEET) were then entered into the model to enable us to explore the combination of key clinical and social functioning variables that best classified individuals into groups according to outcome (stage 1b v. stage 2). The final model is reported using odds ratios (ORa) and 95% confidence intervals (95% CIa) for variables included at the last step in the analysis.
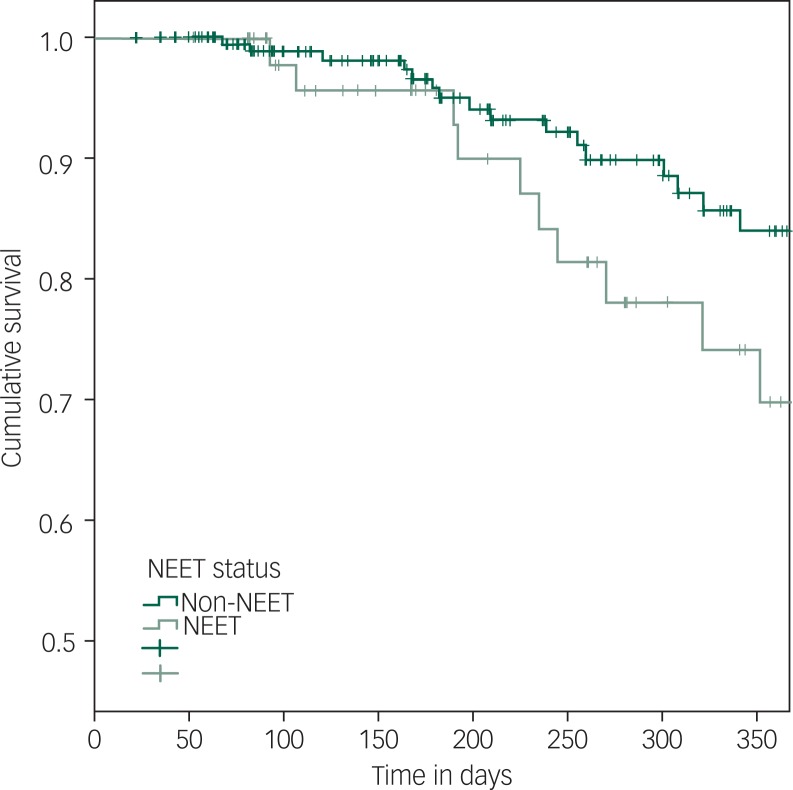
As we were also interested in the potential importance of NEET status to risk of transition, we undertook a planned, subsidiary analysis of the median time to transition in groups defined by NEET status (NEET v. non-NEET). A Kaplan–Meier survival curve demonstrates time to transition according to NEET status at baseline.
In a post hoc analysis of the identified predictor variables, we compared baseline measures of the predictors across the three sub-syndromal groups (stage 1b depressive, bipolar and psychotic disorders) using one-way analysis of variance (ANOVA) of scores on the BPRS-negative symptoms subscale and chi-squared tests for gender and NEET status.
Results
Sample characteristics
Table 1 outlines the baseline characteristics of the 243 individuals who were recruited to the study. The sample was predominantly female (n=155; 64%) with a mean age of about 18 years, and most individuals self-reported that their first ever symptoms or problems occurred at about 13 years of age; 77 individuals (32%) met criteria for being NEET at baseline. Nearly four-fifths of the sample (n=196) was classified as stage 1b depression, 27 as stage 1b bipolar disorder and 20 as stage 1b psychosis (proportions that reflect the general make-up of referrals to the local and national headspace youth mental health services in Australia9,19). Mean scores for the K-10 (mean 31.14), SOFAS (mean 61.13) and four BPRS subscales (means: affect 12.59, negative symptoms 4.29, resistance 5.39 and suicidality 2.16) showed moderate levels of severity. SOFAS scores at baseline were significantly lower for those classified as NEET than for those classified as non-NEET (F[1, 242]=16.24; P<0.001).
Table 1. Baseline characteristics of the sample of 243 individuals.
| Mean (s.d.) unless specified | |
|---|---|
| Current age in years | 18.12 (3.03) |
| % Male | 36% |
| % NEET | 32% |
| Age of first self-reported symptoms or problems | 13.0 (3.12) |
| 10-item Kessler Scale (K10) | 31.14 (8.86) |
| SOFAS | 61.13 (8.76) |
| SOFAS for NEETs | 56.93 (8.42) |
| SOFAS for non-NEETs | 62.52 (8.53) |
| BPRS-affect | 12.59 (3.78) |
| BPRS-positive symptoms | 5.04 (1.93) |
| BPRS-negative symptoms | 4.29 (2.23) |
| BPRS-resistance | 5.39 (2.55) |
| BPRS-activation | 4.02 (1.53) |
| BPRS-suicidality | 2.16 (1.29) |
Percentage are given to the nearest whole number.
NEET, not in education, employment or training; SOFAS, Social and Occupational Functioning Assessment Scale; BPRS, Brief Psychiatric Rating Scale.
Survival analysis
Transition from stage 1b to stage 2 occurred in 36 individuals (16.8%) by the end of the follow-up period. Of the 36 who transitioned, just over 60% (n=22) were stage 1b depression, 8 were stage 1b psychosis and 6 were stage 1b bipolar disorder. Eleven per cent (11%) of sub-syndromal depressive cases, 40% of individuals with sub-syndromal psychosis and 22% of individuals with sub-syndromal bipolar disorder transitioned to stage 2.
The Cox regression model was statistically significant (χ2=27.72; d.f.=14; P=0.02) and included three variables as shown in Table 2: gender (OR 0.09, 95% CI: 0.012, 0.74; i.e. more females than males demonstrated transition), NEET status (being NEET was associated with transition: OR 5.19, 95% CI: 1.06, 15.32) and BPRS-negative symptoms (more negative symptoms were associated with transition: OR 1.45, 95% CI: 1.12, 1.87). Sub-threshold group (depression, bipolar disorder, psychosis trajectory); prior duration of symptoms; and scores on the SOFAS, K-10 and all other BPRS subscales did not predict transition. Post hoc analyses showed that the sub-threshold groups did not differ at baseline on gender or BPRS-negative symptoms. The groups differed only on two baseline measures with the psychosis group recording higher mean scores for BPRS-positive symptoms (psychosis 7.5 v. depression 4.9 v. bipolar 4.2; F=13.76; d.f.=3.239; P=0.001) and BPRS-activation symptoms (psychosis 4.4 v. depression 4.1 v. bipolar 3.3; F=2.97; d.f.=3.239; P=0.03).
Table 2. Cox regression analysis of survival: baseline variables associated with transition from sub-syndromal to syndromal caseness during the 12-month follow-up period.
| Variable | Sig. | Exp(B) | 95% CI for Exp(B) | |
|---|---|---|---|---|
| Lower | Upper | |||
| NEET status | 0.042 | 5.190 | 1.06 | 15.32 |
| BPRS-negative symptoms | 0.005 | 1.446 | 1.12 | 1.87 |
| Gender | 0.024 | 0.09 | 0.012 | 0.74 |
Figure 1 shows the time to transition for NEET v. non-NEET individuals over 12 months. As can be seen, no group demonstrated a transition rate of 50%. At the end of the follow-up period, 26% of those who were categorised as NEET at baseline versus 16% of those who were not NEET had reached threshold caseness (stage 2). Furthermore, the estimated time for 10% of the NEET group to make a transition to stage 2 was about 225 days, and for 10% of the non-NEET group, the equivalent transition rate was not reached until about 300 days.
Fig. 1. Kaplan–Meier curve representing time to transition in groups defined by NEET (not in education, employment or training) status at baseline.
Discussion
The rate of transition (17%) from sub-syndromal (stage 1b) to syndromal (stage 2) unipolar, bipolar or psychotic disorders observed in this study of young people is consistent with that observed in other studies of transition to psychosis (most of which include both affective and non-affective psychosis).5,7 Consistent with studies in ultra-high risk of psychosis cohorts,24 we did not find that baseline assessment of psychological distress as measured by the K-10 or other common psychiatric symptoms or positive symptoms as measured by the BPRS were predictors of transition over 12 months. By contrast, negative symptoms were predictive of early transition to any of the three disorder pathways, a finding that is consistent with previous psychosis risk research.12,15 Importantly, negative symptoms were not specific to the sub-syndromal psychosis groups, but were a trans-diagnostic phenomenon, being equally common in those at risk of early transition to syndromal mood disorder. Baseline social and occupational functioning as measured by the SOFAS did not appear in the final step of the regression model. Although this finding is at odds with some previous research that suggests a link between the SOFAS and similar measures of functioning and later transition to psychosis,12 our study found a link between NEET status and early transition in this trans-diagnostic cohort. As NEET status and social and functional impairment are linked phenomena, our findings may indicate that NEET status is a more potent marker of impairment in daily living skills or a useful proxy indicator that the level of impaired functioning reported by an individual is reaching a critical level. Females were also more likely to transition from stage 1b to stage 2 in this study. This was somewhat unexpected, but may be related to the over-representation of females in help-seeking youth attending headspace services, or the fact that previous studies that have focused solely on transition to psychosis, which is more common in males, rather than to major mood and psychotic disorders.
The percentage of young people with NEET status in this study is higher than to those reported elsewhere in similar clinical settings (19%)23 and is much higher than the rate observed in the general population in Australia (11%)23 and in the OECD (13%).25 The relatively high NEET rate in this study may be because of a combination of factors, including clinical characteristics, such as level of symptomatic impairment at baseline increasing the likelihood that patients were already disengaging from participation in education or employment, but also demography, namely the location of the clinic in an area of greater socio-economic disadvantage (so that the population base rate for NEET status was higher than the national average). Although we cannot disentangle cause and effect in this study, the findings of an association between NEET status and increased likelihood of transition in this trans-diagnostic cohort are similar to recent studies of transition to psychosis.14,15 Importantly, we found that NEET status appears to serve as a trans-diagnostic marker for progression to full syndromal episodes of major mental disorder, independent of either the presumed diagnostic sub-type or symptom severity. This reinforces that attention to NEET status is important as baseline unemployment has been shown to translate to poor functioning up to 6 years later in young people.17,26 Furthermore, even if NEET status is a consequence of developing mental and substance-use problems,25 treating earlier, sub-syndromal presentations of potentially severe mental disorders may reduce the risk of becoming NEET, which may in turn reduce transition risk. From a pragmatic viewpoint, NEET status is a simple objective marker that general practitioners or non-specialist clinicians could record and use as an additional criterion (alongside mental state) to identify a subgroup of youth who may benefit from ongoing monitoring, early referral and/or more intensive interventions by specialists in youth mental health. From an intervention perspective, supporting young people to re-engage in employment, education or training may prove as or even more productive than the traditional focus on symptom reduction alone.23 Indeed, there is increasing support for the notion that this kind of support should be provided to all help-seeking young people who require it regardless of their ‘high-risk’ status and/or transition outcomes.15 This study cannot determine whether NEET status is a marker of the degree of functional deterioration secondary to an underlying illness process or whether it is a risk factor for transition or whether being non-NEET is a protective factor against transition (or all the three). However, the findings emphasise that clinicians, service providers and government agencies need to consider how to access and identify individuals with sub-threshold clinical syndromes from within NEET populations.
There were a number of limitations in this study. The most important was that the sub-syndromal psychosis and bipolar groups only comprised a minority of the sample. This case mix reflects the ‘stage 1b’ help-seeking population presenting to youth early intervention clinics. Furthermore, the actual proportion of transitions in each of these two groups was 2–4 times that seen in the stage 1b depression group. However, the small subgroup sizes mean that we cannot exclude the possibility that disorder-specific predictors of transition were not identified. Furthermore, although the OR for transition in NEET group compared to non-NEET group was high (OR>5), the 95% confidence intervals were wide, indicating again the limitations of the study and the analyses. A longer follow-up period with larger samples is required to fully explore predictors in youth mental health settings, especially because other studies have demonstrated ongoing risk of transition beyond 12 months, and in some cases up to 10 years.6 Lastly, measurement occurred 3-monthly in this study, which may have limited the sensitivity of the timing of the transitions and the associated changes in symptoms and functioning.
Overall, this preliminary study of trans-diagnostic transition from sub-syndromal to syndromal major mental disorders demonstrated that complex relationships exist between negative symptoms, NEET status and potentially with gender. The finding that NEET status and negative symptoms are important in transitions to later clinical stages in mood as well as psychotic disorders is important as it emphasises the need to better understand which risk factors are disorder-specific and which represent generic markers or risk for disease progression across a range of disorders. Furthermore, the finding that two of the three predictors of early transition are potentially modifiable (NEET status and negative symptoms) may inform the development of both age- and stage-specific interventions that reduce symptoms, improve functioning and delay or prevent the risk of transition to the three most burdensome severe mental disorders in young people.
References
- 1.Gore FM, Bloem PJN, Patton GC, Ferguson J, Joseph V, Coffey C, et al. Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet 2011; 377: 2093–102. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustun TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry 2007; 20: 359–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hickie I, Scott J, McGorry P. Clinical staging for mental disorders: a new development in diagnostic practice in mental health. Med J Aust 2013; 198: 461–2. [DOI] [PubMed] [Google Scholar]
- 4.Scott J, Leboyer M, Hickie I, Berk M, Kapczinski F, Frank E, et al. Clinical staging in psychiatry: a cross-cutting model of diagnosis with heuristic and practical value. Br J Psychiatry 2013; 202: 243–5. [DOI] [PubMed] [Google Scholar]
- 5.Hartmann JA, Yuen HP, McGorry PD, Yung AR, Lin A, Wood SJ, et al. Declining transition rates to psychotic disorder in “ultra-high risk” clients: investigation of a dilution effect. Schizophr Res 2016; 170: 130–6. [DOI] [PubMed] [Google Scholar]
- 6.Simon AE, Velthorst E, Nieman DH, Linszen D, Umbricht D, de Haan L. Ultra high-risk state for psychosis and non-transition: a systematic review. Schizophr Res 2011; 132: 8–17. [DOI] [PubMed] [Google Scholar]
- 7.Simon AE, Borgwardt S, Riecher-Rössler A, Velthorst E, de Haan L, Fusar-Poli P. Moving beyond transition outcomes: meta-analysis of remission rates in individuals at high clinical risk for psychosis. Psychiatry Res 2013; 209: 266–72. [DOI] [PubMed] [Google Scholar]
- 8.Cross SP, Hermens DF, Scott EM, Ottavio A, McGorry PD, Hickie IB. A clinical staging model for early intervention youth mental health services. Psychiatr Serv 2014; 65: 939–43. [DOI] [PubMed] [Google Scholar]
- 9.Cross SP, Hermens DF, Hickie IB. Treatment patterns and short-term outcomes in an early intervention youth mental health service. Early Interv Psychiatry 2014. [DOI] [PubMed] [Google Scholar]
- 10.Cross SPM, Hermens DF, Scott J, Salvador-Carulla L, Hickie IB. Differential impact of current diagnosis and clinical stage on attendance at a youth mental health service. Early Interv Psychiatry 2017; 11: 255–62. [DOI] [PubMed] [Google Scholar]
- 11.Fusar-Poli P, Yung AR, McGorry P, van Os J. Lessons learned from the psychosis high-risk state: towards a general staging model of prodromal intervention. Psychol Med 2014; 44: 17–24. [DOI] [PubMed] [Google Scholar]
- 12.Valmaggia L, Stahl D, Yung A, Nelson B, Fusar-Poli P, McGorry P, et al. Negative psychotic symptoms and impaired role functioning predict transition outcomes in the at-risk mental state: a latent class cluster analysis study. Psychol Medicine 2013; 43: 2311–25. [DOI] [PubMed] [Google Scholar]
- 13.Yung AR, Phillips LJ, Yuen HP, Francey SM, McFarlane CA, Hallgren M, et al. Psychosis prediction: 12-month follow up of a high-risk (“prodromal”) group. Schizophr Res 2003; 60: 21–32. [DOI] [PubMed] [Google Scholar]
- 14.Dragt S, Nieman DH, Veltman D, Becker HE, van de Fliert R, de Haan L, et al. Environmental factors and social adjustment as predictors of a first psychosis in subjects at ultra high risk. Schizophr Res 2011; 125: 69–76. [DOI] [PubMed] [Google Scholar]
- 15.Fusar-Poli P, Byrne M, Valmaggia L, Day F, Tabraham P, Johns L, et al. Social dysfunction predicts two years clinical outcome in people at ultra high risk for psychosis. J Psychiatr Res 2010; 44: 294–301. [DOI] [PubMed] [Google Scholar]
- 16.Ising H, Ruhrmann S, Burger N, Rietdijk J, Dragt S, Klaassen R, et al. Development of a stage-dependent prognostic model to predict psychosis in ultra-high-risk patients seeking treatment for co-morbid psychiatric disorders. Psychol Med 2016; 46: 1839–51. [DOI] [PubMed] [Google Scholar]
- 17.Scott J, Fowler D, McGorry P, Birchwood M, Killackey E, Christensen H, et al. Adolescents and young adults who are not in employment, education, or training. BMJ 2013; 347: f5270. [DOI] [PubMed] [Google Scholar]
- 18.Hickie IB, Scott EM, Hermens DF, Naismith SL, Guastella AJ, Kaur M, et al. Applying clinical staging to young people who present for mental health care. Early Interv Psychiatry 2013; 7: 31–43. [DOI] [PubMed] [Google Scholar]
- 19.McGorry P, Tanti C, Stokes R, Hickie I, Carnell K, Littlefield L, et al. headspace: Australia’s National Youth Mental Health Foundation – where young minds come first. Med J Aust 2007; 187: S68–70. [DOI] [PubMed] [Google Scholar]
- 20.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002; 32: 959–76. [DOI] [PubMed] [Google Scholar]
- 21.Shafer A. Meta-analysis of the brief psychiatric rating scale factor structure. Psychol Assess 2005; 17: 324–35. [DOI] [PubMed] [Google Scholar]
- 22.Goldman H, Skodol A, Lave T. Revising axis V for DSM-IV: a review of measures of social functioning. Am J Psychiatry 1992; 149: 1148–56. [DOI] [PubMed] [Google Scholar]
- 23.O’Dea B, Glozier N, Purcell R, McGorry PD, Scott J, Feilds K-L, et al. A cross-sectional exploration of the clinical characteristics of disengaged (NEET) young people in primary mental healthcare. BMJ Open. 2014; 4: e006378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O’Connor K, Nelson B, Lin A, Wood SJ, Yung A, Thompson A. Are UHR patients who present with hallucinations alone at lower risk of transition to psychosis? Psychiatry Res 2015; 235: 177–96. [DOI] [PubMed] [Google Scholar]
- 25.Baggio S, Iglesias K, Deline S, Studer J, Henchoz Y, Mohler-Kuo M, et al. Not in education, employment, or training status among young Swiss men. Longitudinal associations with mental health and substance use. J Adolesc Health 2015; 56: 238–43. [DOI] [PubMed] [Google Scholar]
- 26.Brandizzi M, Valmaggia L, Byrne M, Jones C, Iwegbu N, Badger S, et al. Predictors of functional outcome in individuals at high clinical risk for psychosis at six years follow-up. J Psychiatr Res 2015; 65: 115–23. [DOI] [PubMed] [Google Scholar]