Abstract
Background
HLA-DRB1 alleles are major determinants of genetic predisposition to rheumatic diseases. We assessed whether DRB1 alleles are associated with susceptibility to particular clinical features of adult onset Still’s disease (AOSD) in a Japanese population by determining the DRB1 allele distributions.
Methods
DRB1 genotyping of 96 patients with AOSD and 1,026 healthy controls was performed. Genomic DNA samples from the AOSD patients were also genotyped for MEFV exons 1, 2, 3, and 10 by direct sequencing.
Results
In Japanese patients with AOSD, we observed a predisposing association of DRB1*15:01 (p = 8.60 × 10−6, corrected p (Pc) = 0.0002, odds ratio (OR) = 3.04, 95% confidence interval (95% CI) = 1.91–4.84) and DR5 serological group (p = 0.0006, OR = 2.39, 95% CI = 1.49–3.83) and a protective association of DRB1*09:01 (p = 0.0004, Pc = 0.0110, OR = 0.34, 95% CI = 0.18–0.66) with AOSD, and amino acid residues 86 and 98 of the DRβ chain were protectively associated with AOSD. MEFV variants were identified in 49 patients with AOSD (56.3%). The predisposing effect of DR5 was confirmed only in patients with AOSD who had MEFV variants and not in those without MEFV variants. Additionally, DR5 in patients with AOSD are associated with macrophage activation syndrome (MAS) and steroid pulse therapy.
Conclusion
The DRB1*15:01 and DR5 are both associated with AOSD susceptibility in Japanese subjects. A protective association between the DRB1*09:01 allele and AOSD was also observed in these patients. Our data also highlight the effects of DRB1 alleles in susceptibility to AOSD.
Electronic supplementary material
The online version of this article (doi:10.1186/s13075-017-1406-x) contains supplementary material, which is available to authorized users.
Keywords: Adult onset Still’s disease, Autoinflammatory disease, Human leukocyte antigen, Macrophage-activation syndrome, Systemic juvenile idiopathic arthritis
Background
Adult onset Still’s disease (AOSD), manifested by spiking fever, skin rash, and arthritis, is a complex (multigenic) autoinflammatory disease, meaning that its development depends on a combination of genetic and environmental risk factors [1]. The concept of autoinflammation originally emerged from innate immune system activation [2]. Although there are rare monogenic forms of autoinflammatory disease, acquired autoinflammatory diseases in which both innate and adaptive immune abnormalities are implicated are more common [3]; this group includes genetically complex rheumatic diseases, such as AOSD [4]. Complex genetic factors may confer susceptibility to AOSD development under certain environmental conditions [5].
The HLA cluster is one of the most intensively studied genetic factors in AOSD [6]. HLA molecules are linked with adaptive immunity, where they act to present peptide antigens to antigen receptors on T lymphocytes [7]. Currently, there is no consensus on the relationship between AOSD and HLA. Previous studies on the genetic predisposition to AOSD have limitations and have had inconsistent results [8]. This may be caused by the small number of patients included in these studies, due to the rarity of this disease and its heterogeneous clinical manifestations.
Systemic juvenile idiopathic arthritis (sJIA) and AOSD both manifest as systemic arthritis [9]. Recent studies have provided new clues to the genetic underpinning of sJIA. A genome-wide association study of sJIA identified a strong association between sJIA and HLA-DRB1*11 [10]. This study supports a role for DRB1 alleles as a major sJIA risk factor [10]. To determine whether or not genetic variations of DRB1 alleles also influence AOSD risk, we investigated the DRB1 alleles in Japanese patients with AOSD. Previously, we found preliminary evidence suggesting that familial Mediterranean fever (FMF)-related MEFV variants can affect the disease phenotype of AOSD [11]. In this study we evaluated the influence of the MEFV genotype and HLA-DRB1 alleles on AOSD risk.
Methods
Design, setting, patients, and measurements
We retrospectively evaluated 96 patients (mean age ± standard deviation = 50.2 ± 20.2 years, 78 female (81.2%)), who had AOSD and were treated at the Department of Rheumatology of the participating hospital group, between 2010 and 2017. The patients had all been diagnosed with AOSD according to the Yamaguchi criteria [12], after exclusion of infectious, hematologic, and autoimmune diseases. Among 96 patients, 87 patients had undergone laboratory tests, including a complete blood count, liver function tests, urinalysis, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and ferritin. In the remaining nine patients, the demographic and MEFV genotyping data were not available except gender and age. The clinical characteristics of these patients, including age, gender, length of follow up, clinical features, treatments, outcomes, and complications, were evaluated using a standardized form. The study considered three clinical AOSD courses: (1) monocyclic, defined as a single episode that subsequently faded and was followed by persistent good health for 1 year or more of follow up; (2) polycyclic, defined as a complete remission followed by one or more exacerbations; and (3) chronic, defined as persistently active disease, usually associated with polyarthritis [13]. Complicated AOSD was defined as including one or more of the following conditions: liver dysfunction, disseminated intravascular coagulation, and macrophage activation syndrome (MAS) as defined previously [14]. This study was approved by the institutional review board of the Sasebo City Hospital (number 2012-A-22) and participating hospitals.
Genotyping methods
DRB1 allele typing was performed using a Luminex 200 system (Luminex, Austin, TX, USA) and a WAKFlow HLA Typing kit (Wakunaga, Hiroshima, Japan) as described previously [15]. DRB1 alleles were assigned automatically using WAKflow Typing software (Wakunaga). The DR5 serological group consists of DRB1*11:01, *12:01, and *12:02 [16]. Genotyping results for the healthy controls (mean age ± standard deviation = 37.7 ± 11.7 years, 303 male (29.8%)) were previously reported [17].
MEFV gene analysis
Genomic DNA was extracted from whole blood using the Promega Wizard® Genomic DNA Purification Kit (Madison, WI, USA) according to the manufacturer’s instructions. Polymerase chain reaction (PCR) was performed using forward and reverse primers for each exon of the MEFV gene, as described previously [18]. PCR was performed using the forward and reverse primers for each exon (Additional file 1: Figure S1). The resulting PCR products were purified using ExoSAP-IT (GE Healthcare, Tokyo, Japan) and directly sequenced using specific primers and BigDye Terminator v1.1 (Applied Biosystems, Tokyo, Japan). The MEFV genetic analysis was approved by the Ethics Committee of Fukushima Medical University School of Medicine (2016, number 2920).
Statistical analysis
Differences among AOSD characteristics were analyzed by performing the Mann-Whitney U test or chi-squared test using 2 × 2 contingency tables. The association of allele carrier frequencies, haplotype carrier frequencies or amino acid residue carrier frequencies with AOSD was analyzed using Fisher’s exact test with 2 × 2 contingency tables under the dominant model. Adjustment for multiple comparisons was conducted with the Bonferroni method; corrected p (Pc) values were calculated by multiplying the p value by the number of tested alleles or amino acid positions. To examine whether each DRB1 allele independently contributes to AOSD, multiple logistic regression analysis under the additive model was employed and the deviation from 0 was evaluated for coefficients using the Wald test.
Results
Demographic findings of enrolled patients with AOSD
Clinical manifestations of the enrolled patients are shown in Table 1. Among the 87 enrolled patients with AOSD, 69 (79.3%) were women, and the mean age at diagnosis was 49.3 ± 19.9 years. In terms of the disease course, 56 patients (64.3%) had the polycyclic systemic type, 19 (21.8%) had the monocyclic systemic type, and 12 (13.7%) had the chronic articular type of AOSD (Table 1).
Table 1.
Demographics of AOSD patients
| Variable | Value |
|---|---|
| Number | 87 |
| Female, n (%) | 69 (79.3) |
| Age at onset (years) | 49.3 ± 19.9 |
| Ferritin (ng/mL) | 11251.2 ± 16997.9 |
| CRP (mg/dL) | 12.4 ± 8.2 |
| ESR (mm(1 h)) | 71.1 ± 30.1 |
| Liver dysfunction, n (%) | 68 (78.1) |
| MAS, n (%) | 23 (26.4) |
| Initial dose of PSL (mg/day) | 41.8 ± 12.2 |
| Steroid pulse, n (%) | 55 (63.2) |
| Immunosuppressant, n (%) | 51 (58.6) |
| Biologics, n (%) | 26 (29.8) |
| Polycyclic systemic type, n (%) | 56 (64.3) |
| Monocyclic systemic type, n (%) | 19 (21.8) |
| Chronic arthritis type, n (%) | 12 (13.7) |
| Relapse, n (%) | 40 (45.9) |
Mean ± standard deviation or number (percentage) is shown
AOSD adult onset Still’s disease, CRP C-reactive protein, ESR erythrocyte sedimentation rate, MAS macrophage activation syndrome, PSL prednisolone
Association of specific DRB1 alleles with AOSD
Associations of specific DRB1 alleles with AOSD were evaluated in a case-control study consisting of the 96 Japanese patients with AOSD as described previously and 1026 healthy subjects (Table 2). The patients with AOSD had significantly higher frequencies of the DRB1*15:01 allele (p = 8.60 × 10−6, corrected p (Pc) = 0.0002, odds ratio (OR) = 3.04, 95% confidence interval (95% CI) = 1.91–4.84) compared with healthy subjects. Although patients with AOSD appeared to have higher frequencies of DRB1*12:01 allele than healthy subjects, this difference was not statistically significant. However, an association between DR5 serological group and AOSD was observed.
Table 2.
HLA-DRB1 allele carrier frequency in the patients with AOSD and in controls
| Cases (n = 96) | Controls (n = 1026) | P | OR | Pc | 95% CI | |
|---|---|---|---|---|---|---|
| DRB1*01:01 | 9 (9.4) | 110 (10.7) | 0.8622 | 0.86 | NS | (0.42–1.76) |
| DRB1*03:01 | 0 (0.0) | 3 (0.3) | 1.0000 | 1.52 | NS | (0.08–29.55) |
| DRB1*04:01 | 0 (0.0) | 22 (2.1) | 0.2486 | 0.23 | NS | (0.01–3.84) |
| DRB1*04:03 | 4 (4.2) | 47 (4.6) | 1.0000 | 0.91 | NS | (0.32–2.57) |
| DRB1*04:04 | 0 (0.0) | 4 (0.4) | 1.0000 | 1.18 | NS | (0.06–22.03) |
| DRB1*04:05 | 21 (21.9) | 243 (23.7) | 0.8014 | 0.90 | NS | (0.54–1.49) |
| DRB1*04:06 | 2 (2.1) | 76 (7.4) | 0.0562 | 0.27 | NS | (0.06–1.10) |
| DRB1*04:07 | 0 (0.0) | 15 (1.5) | 0.6313 | 0.34 | NS | (0.02–5.70) |
| DRB1*04:10 | 4 (4.2) | 32 (3.1) | 0.5413 | 1.35 | NS | (0.47–3.90) |
| DRB1*07:01 | 0 (0.0) | 9 (0.9) | 1.0000 | 0.55 | NS | (0.03–9.61) |
| DRB1*08:02 | 13 (13.5) | 72 (7.0) | 0.0403 | 2.08 | NS | (1.10–3.90) |
| DRB1*08:03 | 16 (16.7) | 153 (14.9) | 0.6544 | 1.14 | NS | (0.65–2.01) |
| DRB1*08:09 | 0 (0.0) | 2 (0.2) | 1.0000 | 2.12 | NS | (0.10–44.55) |
| DRB1*09:01 | 11 (11.5) | 280 (27.3) | 0.0004 | 0.34 | 0.0110 | (0.18–0.66) |
| DRB1*10:01 | 0 (0.0) | 5 (0.5) | 1.0000 | 0.96 | NS | (0.05–17.54) |
| DRB1*11:01 | 6 (6.3) | 41 (4.0) | 0.2837 | 1.60 | NS | (0.66–3.87) |
| DRB1*12:01 | 16 (16.7) | 75 (7.3) | 0.0031 | 2.54 | 0.0896 | (1.41–4.56) |
| DRB1*12:02 | 8 (8.3) | 37 (3.6) | 0.0488 | 2.43 | NS | (1.10–5.38) |
| DRB1*13:01 | 2 (2.1) | 8 (0.8) | 0.2082 | 2.71 | NS | (0.57–12.93) |
| DRB1*13:02 | 5 (5.2) | 163 (15.9) | 0.0040 | 0.29 | 0.1150 | (0.12–0.73) |
| DRB1*14:03 | 7 (7.3) | 44 (4.3) | 0.1941 | 1.76 | NS | (0.77–4.01) |
| DRB1*14:04 | 0 (0.0) | 4 (0.4) | 1.0000 | 1.18 | NS | (0.06–22.03) |
| DRB1*14:05 | 6 (6.3) | 40 (3.9) | 0.2758 | 1.64 | NS | (0.68–3.98) |
| DRB1*14:06 | 2 (2.1) | 29 (2.8) | 1.0000 | 0.73 | NS | (0.17–3.11) |
| DRB1*14:07 | 0 (0.0) | 2 (0.2) | 1.0000 | 2.12 | NS | (0.10–44.55) |
| DRB1*14:54 | 6 (6.3) | 58 (5.7) | 0.8168 | 1.11 | NS | (0.47–2.65) |
| DRB1*15:01 | 31 (32.3) | 139 (13.5) | 8.60 × 10-6 | 3.04 | 0.0002 | (1.91–4.84) |
| DRB1*15:02 | 18 (18.8) | 224 (21.8) | 0.5197 | 0.83 | NS | (0.48–1.41) |
| DRB1*16:02 | 0 (0.0) | 18 (1.8) | 0.3919 | 0.28 | NS | (0.02–4.72) |
| DR5(*11, *12) | 28 (29.2) | 151 (14.7) | 0.0006 | 2.39 | (1.49–3.83) |
Allele carrier frequencies are shown in parentheses (%). Association was tested by Fisher’s exact test using 2 × 2 contingency tables under the dominant model. AOSD adult onset Still’s disease, OR odds ratio, CI confidence interval, Pc corrected p value, NS not significant
Reduced DRB1*09:01 allele carrier frequencies in AOSD
In contrast to the predisposing effects of the DRB1*15:01 allele, DRB1*09:01 was negatively associated with AOSD (Table 2). In fact, although the DRB1*15:01 allele predisposed individuals to AOSD in the absence of DRB1*09:01, the DRB1*15:01 allele was not associated with AOSD in those carrying the DRB1*09:01 allele (Table 3). Thus, the protective effects of DRB1*09:01 can neutralize the AOSD-predisposing effects of the DRB1*15:01 allele. When the allele carrier frequencies of DRB1 alleles in patients with AOSD were compared with age-matched healthy controls, a similar associative tendency was observed (Additional file 2: Table S1). In addition, conditional logistic regression analysis between age, gender, DRB1*09:01, DRB1*15:01, and DR5 in AOSD was performed (Additional file 3: Table S2). The association of DRB1*09:01, DRB1*15:01, and DR5 remained significant, when conditioned on age or gender, and these were independent of each other.
Table 3.
HLA-DRB1 genotype frequencies in the patients with AOSD and in controls
| Cases (n = 96) | Controls (n = 1026) | P | OR | 95% CI | |
|---|---|---|---|---|---|
| *15:01/any alleles | 31 (32.3) | 139 (13.5) | 8.60 × 10-6 | 3.04 | (1.91-4.84) |
| *15:01/*09:01 | 1 (1.0) | 21 (2.0) | 1.0000 | 0.50 | |
| *15:01/alleles other than *09:01 | 30 (31.3) | 118 (11.5) | 1.64 × 10-6 | 3.50 | (2.18-5.61) |
Genotype frequencies are shown in parentheses (%). Association was tested by Fisher’s exact test using 2 × 2 contingency tables. AOSD adult onset Still’s disease, OR odds ratio, CI confidence interval
MEFV variant analysis
All patients with AOSD were successfully genotyped for the MEFV gene. MEFV variants were identified in 49 patients with AOSD (56.3%), and the distributions of MEFV variants in the patients are shown in Table 4. We stratified the patients with AOSD according to the presence of MEFV variants. The predisposing effect of DRB1*15:01 on AOSD development was not changed by the presence or absence of MEFV variants (Table 5). In contrast, the AOSD-predisposing effect of DR5 was confirmed in patients with AOSD with MEFV variants, but DR5 was not associated with AOSD in patients without MEFV variants. Thus, the presence or absence of MEFV variants can affect the AOSD-predisposing effects of DR5.
Table 4.
MEFV genotypes of patients with AOSD
| Mutations | Number of patients (percentage) (n = 87) |
|---|---|
| M694I/normal | 2 (2.3) |
| G632S/E408Q | 1 (1.1) |
| P369S/R408Q | 4 (4.6) |
| E148Q/P369S | 1 (1.1) |
| E148Q/E148Q/P369S/R408Q | 1 (1.1) |
| L110P/E148Q/E148Q/P369S/R408Q | 1 (1.1) |
| E148Q/P369S/R408Q | 2 (2.3) |
| E148Q/R202Q | 1 (1.1) |
| R202Q/normal | 3 (3.4) |
| E148Q/normal | 19 (21.8) |
| E148Q/E148Q | 2 (2.3) |
| L110P/E148Q | 6 (6.9) |
| L110P/E148Q//E148Q | 2 (2.3) |
| L110P/E148Q//R202Q | 1 (1.1) |
| L110P/L110P/E148Q//E148Q | 1 (1.1) |
| E84K/normal | 1 (1.1) |
| E84K/L110P/E148Q | 1 (1.1) |
| Normal | 38 (43.7) |
AOSD adult onset Still’s disease
Table 5.
HLA-DRB1 allele carrier frequency in the patients with AOSD with or without MEFV variants
| AOSD with MEFV variants | AOSD without MEFV variants | Controls | AOSD with MEFV variants vs. controls | AOSD without MEFV variants vs. controls | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 49) | (n = 38) | (n = 1026) | P | OR | Pc | 95% CI | P | OR | Pc | 95% CI | |
| DRB1*15:01 | 17 (34.7) | 13 (34.2) | 139 (13.5) | 0.0002 | 3.39 | 0.0068 | (1.83–6.27) | 0.0013 | 3.32 | 0.0388 | (1.66–6.64) |
| DR5(DRB1*11, *12) | 16 (32.7) | 8 (21.1) | 151 (14.7) | 0.0019 | 2.81 | (1.51–5.23) | 0.2543 | 1.55 | (0.70–3.43) | ||
Allele carrier frequencies are shown in parentheses (%). Association was tested by Fisher’s exact test using 2 × 2 contingency tables under the dominant model. AOSD adult onset Still’s disease, OR odds ratio, CI confidence interval, Pc corrected p value, NS not significant
Association of specific DRB1 alleles and clinical manifestations of AOSD
To evaluate the potential correlation between DRB1 alleles and the clinical manifestations of AOSD, we stratified the patients with AOSD according to the presence of the DRB1*15:01 allele (Table 6). There was no significant difference in the clinical manifestations, including the disease phenotype, between patients with AOSD with and without the DRB1*15:01 allele. We then compared the clinical manifestations between patients with AOSD with or without DR5. Patients with AOSD with DR5 more frequently have macrophage activation syndrome (MAS) and are more frequently treated by steroid pulse therapy than those without DR5 (Table 6).
Table 6.
Comparison of the demographics between patients with AOSD with or without DRB1*15:01 or DR5
| DRB1*15:01 (+) | DRB1*15:01 (-) | P | DR5 (+) | DR5 (-) | P | |
|---|---|---|---|---|---|---|
| Number | 29 | 58 | 23 | 64 | ||
| Female, n (%) | 24 (82.7) | 45 (77.5) | 0.7789 | 20 (86.9) | 49 (77.4) | 0.2912 |
| Age at onset (years) | 46.6 ± 20.3 | 50.6 ± 19.6 | 0.3980 | 50.6 ± 20.5 | 48.1 ± 19.7 | 0.7469 |
| Ferritin (ng/mL) | 12818.5 ± 18292.9 | 10555.5 ± 16284.7 | 0.3657 | 12669.4 ± 16305.9 | 10802.9 ± 17224.9 | 0.3243 |
| CRP (mg/dL) | 11.9 ± 8.2 | 12.7 ± 8.3 | 0.6802 | 12.0 ± 9.2 | 12.6 ± 7.9 | 0.5068 |
| ESR (mm(1 h)) | 59.6 ± 25.3 | 75.4 ± 30.9 | 0.1289 | 67.4 ± 23.0 | 72.5 ± 32.5 | 0.9361 |
| Liver dysfunction, n (%) | 24 (82.7) | 44 (75.8) | 0.4630 | 19 (82.6) | 49 (76.5) | 0.5472 |
| MAS, n (%) | 10 (38.6) | 13 (22.4) | 0.2288 | 10 (43.4) | 13 (20.3) | 0.0307 |
| Initial dose of PSL (mg/day) | 43.8 ± 13.0 | 41.5 ± 11.7 | 0.4379 | 46.1 ± 10.9 | 40.3 ± 12.4 | 0.1184 |
| Steroid pulse, n (%) | 17 (58.6) | 38 (65.5) | 0.4987 | 19 (82.6) | 36 (56.2) | 0.0245 |
| Immunosuppressant, n (%) | 18 (57.6) | 33 (56.8) | 0.6442 | 15 (65.2) | 36 (56.2) | 0.4539 |
| Biologics, n (%) | 10 (38.6) | 16 (27.5) | 0.5077 | 6 (26.0) | 20 (31.2) | 0.6427 |
| Polycyclic systemic type, n (%) | 20 (68.9) | 36 (62.0) | 0.5266 | 18 (78.2) | 38 (59.3) | 0.1048 |
| Monocyclic systemic type, n (%) | 8 (27.5) | 13 (22.4) | 0.5951 | 4 (17.3) | 17 (26.5) | 0.3780 |
| Chronic arthritis type, n (%) | 4 (13.7) | 8 (13.7) | 1.0000 | 2 (8.6) | 10 (15.6) | 0.4085 |
| Relapse, n (%) | 14 (48.2) | 26 (44.8) | 0.7619 | 11 (47.8) | 29 (45.3) | 0.8357 |
Association was tested between patients with adult onset Still’s disease (AOSD) with or without DRB1*15:01 or DR5 analyzed by the chi-squared test using 2 × 2 contingency tables or the Mann-Whitney U test. CRP C-reactive protein, ESR erythrocyte sedimentation rate, MAS macrophage activation syndrome, PSL prednisolone
Amino acid residues in the HLA-DRβ chain are protectively associated with AOSD
We also analyzed the association between amino acid residues in the HLA-DRβ chain and AOSD. Glycine at position 86 (86G, p = 7.88 × 10-7, OR = 0.24, Pc = 2.68 × 10-5, 95% CI 0.15–0.41) and glutamic acid at position 98 (98E, p = 2.80 × 10-5, OR = 0.40, Pc = 0.0010, 95% CI 0.26–0.62) in the DRβ chain showed a protective association with AOSD (Fig. 1, open circle).
Fig. 1.
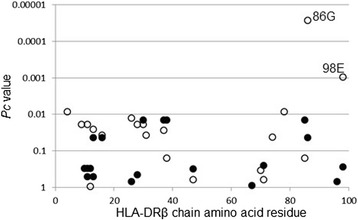
Association between amino acid residues in the DRβ chain and adult onset Still’s disease. Differences in amino acid residue carrier frequencies were analyzed by Fisher’s exact test using 2 × 2 contingency tables. Corrected p (Pc) values were calculated by multiplying the p value by the number of amino acid residues tested. Predisposing association is indicated by filled circles and protective association by open circles
Discussion
AOSD is an inflammatory disorder of uncertain etiology characterized by spiking fever, rash, and arthritis that is accompanied by high ferritin levels [19]. Both sJIA and AOSD are considered to be autoinflammatory diseases with a dysregulated innate immune system [20]. However, this characterization is limited by the fact that dysfunctions of the innate and adaptive immune systems are not mutually exclusive, even in monogenic forms of autoinflammatory disease [21].
Certain HLA alleles have been reported to confer a predisposition to rheumatic diseases [22]. Although no hereditary trend has been reported in AOSD, some studies have reported the associations between HLA-DR and AOSD. Pouchot et al. described a strong association between AOSD and HLA-DR2 [23]. Wouters et al. found an association between DRB1*04 and AOSD and reported that DR6 (DRB1*13, *14) was more frequent in cases with axial joint involvement [24]. Miller et al. reported a frequent association between AOSD and HLA-DR7 [6]. Fujii et al. evaluated the major histocompatibility complex (MHC) class II alleles in 30 Japanese patients with AOSD and reported that DRB1*15:01 and DRB1*12:01 were more frequently detected in subjects with chronic articular forms of AOSD than in healthy controls [25]. Additionally, a Korean study showed that patients with AOSD more frequently had DRB1*12 and *15, and less frequently had DRB1*04 than control subjects [26]. However, controversies remain on the association between HLA-DR molecules and AOSD.
Recent studies have provided new clues to the genetic predispositions for developing systemic arthritis. A genome-wide association study of sJIA patients identified a strong association between sJIA and DRB1*11 [10]. Interestingly, Ombrello et al. raised the new idea that the MHC may act not as an antigen-presenting molecule but rather as a direct activator of MHC class-expressing macrophages or dendritic cells [10]. Our data show that both DRB1*15:01 and DR5 are associated with AOSD in Japanese patients. DRB1*15:01 is the HLA allele that was most strongly associated with AOSD in our study, and these results are consistent with those of previous studies in Japanese or Korean patients [25, 26]. Conversely, the DRB1*09:01 allele had a significantly deceased frequency in patients with AOSD when compared with that in control subjects as reported in multiple sclerosis [27, 28]. However, this negative association of AOSD with the DRB1*09:01 allele needs to be confirmed in the other ethnic populations because the distribution of HLA alleles is different between Japanese and other ethnic populations. Notably, extensive heterogeneity is observed in the clinical manifestations of AOSD, suggesting that AOSD may actually be a heterogeneous subset of disorders [29]. Our results suggest that DRB1 alleles may play a role in the occurrence of AOSD; however, it is possible that there are transcriptional changes for other HLA loci that are co-inherited with DRB1, and these haplotypes may also contribute to the AOSD risk.
It was found that amino acid residues 86 and 98 of the DRβ chain were protectively associated with AOSD (Fig. 1). The DRB1*09:01 allele includes these two amino acid residues, suggesting the predominant protective effects of DRB1*09:01 on AOSD. Amino acid residues 85, 86, 89, and 90 form the HLA-DR peptide-binding groove for peptide position 1 [30], suggesting the involvement of peptide antigens bound to the specific HLA-DR molecule to prevent AOSD.
MEFV variants are commonly found in the Japanese population [31]. Although the significance of MEFV variants is controversial, some studies have suggested that they can influence the phenotypes of inflammatory disorders [32]. Here, we found that the DR5-associated risk for AOSD was not detected in Japanese Patients with AOSD without MEFV variants, whereas the DR5-associated risk was preserved in Japanese patients with MEFV gene variants. These finding suggest a possible interaction between DRB1 and MEFV in AOSD development or in the AOSD disease phenotype. Furthermore, these findings imply that differences between susceptible and non-susceptible DR5 alleles are complemented by MEFV variants in Japanese patients with AOSD, which could be explained by the broad involvement of pyrin, the MEFV encoded protein, in the regulation of the inflammasome and inflammatory processes.
Rheumatic diseases are likely on the spectrum between autoimmunity and autoinflammation [33]. It was suggested that a pathogenic model in which autoinflammatory processes beget an autoimmune condition, sJIA, is a prototype of AOSD [34]. A genome-wide association study on sJIA identified a strong association between sJIA and DRB1*11 alleles. DR5 is a broad-antigen serotype that is further split into HLA-DR11, which includes DRB1*11:01, and HLA-DR12 [17]. In our study, patients with DR5 were more frequently associated with AOSD with macrophage activation syndrome (MAS), which has some similarities to the clinical features of sJIA. These findings are consistent with the reports by Ombrello et al. that demonstrate an association between sJIA and DRB1*11 alleles [11]. From a pathogenic point of view, most autoinflammatory and autoimmune diseases share a chronic aberrant activation of the immune system, which leads to tissue inflammation and/or damage [35].]. In contrast to autoimmune diseases, “autoinflammatory diseases” present with inflammation in the absence of either high-titer autoantibodies or autoreactive T cells. Although the evidence for autoimmunity in AOSD is scant, there are some data that support a role for T cells in its pathogenesis [36]. Additionally, class II HLA molecules have a role in innate immunity and in the regulation of macrophages, including antigen-presenting cells. For example, super-antigen-engaged antigen-presenting cells induce proinflammatory cytokines [37].
There are limitations in our study. Control subjects were younger than the patients. AOSD is a rare disorder offsetting any potential bias due to development of AOSD later in life by a younger control. Another limitation is that all of our study subjects were Japanese because too few patients from other racial/ethnic backgrounds were available for analysis. Also, the number of patients with AOSD was modest and a larger study would be needed.
Conclusion
Our study provides evidence that DRB1*15:01 and DR5 confer a risk for AOSD. A protective association between the DRB1*09:01 allele and AOSD was also observed in this study. Specifically, our data demonstrate that DR5 is associated with AOSD complicated with MAS, in a Japanese population. Additional studies are needed to determine the specific mechanism through which the HLA-DRB1 influences the risk of AOSD.
Additional files
Primers and polymerase chain reaction conditions. (JPG 171 kb)
HLA-DRB1 allele carrier frequency in the patients with AOSD and age-matched healthy controls (1:2). (PDF 57 kb)
Conditional logistic regression analysis between the protective HLA alleles in AOSD. (PDF 43 kb)
Acknowledgements
Not applicable.
Funding
The study was supported by the Practical Research Project for Rare/Intractable Diseases from the Japan Agency for Medical Research and Development, AMED.
Availability of data and materials
Not applicable.
Abbreviations
- AOSD
adult onset Still’s disease
- HLA
human leukocyte antigen
- MAS
macrophage-activation syndrome
- MHC
Major histocompatibility class
- Pc
Corrected p value
- sJIA
systemic juvenile idiopathic arthritis
Authors’ contributions
FH, KE, KY, AK, and KM carried out the molecular genetic studies, participated in the sequence alignment and drafted the manuscript. HF carried out the genetic assays and revised the manuscript. TA, FH, MY, and KM participated in the sequence alignment and drafted the manuscript. MA, YJ, and HK participated in the design of the study, performed the statistical analysis and helped to revise the manuscript. TA, SS, HK, HW, FS, TI, YU, DK, NI, YI, KF, SY, TN, TK, TS, MU, EN, and YU collected the clinical data, and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Ethical approval for this study (number 21003) was provided by the Ethics Committee of Nagasaki Medical Center and written informed consent was obtained from each individual.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1186/s13075-017-1406-x) contains supplementary material, which is available to authorized users.
Contributor Information
Tomoyuki Asano, Email: asanovic@fmu.ac.jp.
Hiroshi Furukawa, Email: furukawa-tky@umin.org.
Shuzo Sato, Email: shuzo@fmu.ac.jp.
Makiko Yashiro, Email: myashiro@fmu.ac.jp.
Hiroko Kobayashi, Email: hkoba@fmu.ac.jp.
Hiroshi Watanabe, Email: chiehiro@fmu.ac.jp.
Eiji Suzuki, Email: azsuzuki@ohta-hp.or.jp.
Tomoyuki Ito, Email: itotomo@nagaoka.jrc.or.jp.
Yoshifumi Ubara, Email: ubara@toranomon.gr.jp.
Daisuke Kobayashi, Email: joifa602@hotmail.com.
Nozomi Iwanaga, Email: n.iwanaga@nagasaki-mc.com.
Yasumori Izumi, Email: yizumi@nagasaki-mc.com.
Keita Fujikawa, Email: keitafj@gmail.com.
Satoshi Yamasaki, Email: syama@hiroshima-u.ac.jp.
Tadashi Nakamura, Email: nakamura@k-shinto.or.jp.
Tomohiro Koga, Email: tkoga@nagasaki-u.ac.jp.
Toshimasa Shimizu, Email: toshimasashimizu2000@yahoo.co.jp.
Masataka Umeda, Email: masataka_0807@yahoo.co.jp.
Fumiaki Nonaka, Email: bunyomona0921@yahoo.co.jp.
Michio Yasunami, Email: yasunami@nagasaki-u.ac.jp.
Yukitaka Ueki, Email: yuku5056@yahoo.co.jp.
Katsumi Eguchi, Email: keguchi0630@yahoo.co.jp.
Koh-ichiro Yoshiura, Email: kyoshi@nagasaki-u.ac.jp.
Atsushi Kawakami, Email: atsushik@nagasaki-u.ac.jp.
Kiyoshi Migita, Phone: +81-24-547-2055, Email: migita@fmu.ac.jp.
References
- 1.Gerfaud-Valentin M, Jamilloux Y, Iwaz J, Sève P. Adult-onset Still’s disease. Autoimmun Rev. 2014;13(7):708–22. doi: 10.1016/j.autrev.2014.01.058. [DOI] [PubMed] [Google Scholar]
- 2.Park H, Bourla AB, Kastner DL, Colbert RA, Siegel RM. Lighting the fires within: the cell biology of autoinflammatory diseases. Nat Rev Immunol. 2012;12(8):570–80. doi: 10.1038/nri3261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rigante D, Vitale A, Lucherini OM, Cantarini L. The hereditary autoinflammatory disorders uncovered. Autoimmun Rev. 2014;13(9):892–900. doi: 10.1016/j.autrev.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Castañeda S, Blanco R, González-Gay MA. Adult-onset Still’s disease: Advances in the treatment. Best Pract Res Clin Rheumatol. 2016;30(2):222–38. doi: 10.1016/j.berh.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 5.Guilpain P, Le Quellec A. About the complexity of adult onset Still's disease… advances still required for its management. BMC Med. 2017;15(1):5. doi: 10.1186/s12916-016-0769-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller ML, Aaron S, Jackson J, et al. HLA gene frequencies in children and adults with systemic onset juvenile rheumatoid arthritis. Arthritis Rheum. 1985;28(2):146–50. doi: 10.1002/art.1780280207. [DOI] [PubMed] [Google Scholar]
- 7.Heemst J, Huizinga TJ, van der Woude D, Toes RE. Fine-mapping the human leukocyte antigen locus in rheumatoid arthritis and other rheumatic diseases: identifying causal amino acid variants? Curr Opin Rheumatol. 2015;27(3):256–61. doi: 10.1097/BOR.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 8.Efthimiou P, Georgy S. Pathogenesis and management of adult-onset Still’s disease. Semin Arthritis Rheum. 2006;36(3):144–52. doi: 10.1016/j.semarthrit.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 9.Vastert SJ, Kuis W, Grom AA. Systemic JIA: new developments in the understanding of the pathophysiology and therapy. Best Pract Res Clin Rheumatol. 2009;23(5):655–64. doi: 10.1016/j.berh.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ombrello MJ, Remmers EF, Tachmazidou I, et al. HLA-DRB1*11 and variants of the MHC class II locus are strong risk factors for systemic juvenile idiopathic arthritis. Proc Natl Acad Sci USA. 2015;112(52):15970–5. doi: 10.1073/pnas.1520779112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nonaka F, Migita K, Jiuchi Y, et al. Increased prevalence of MEFV exon 10 variants in Japanese patients with adult-onset Still’s disease. Clin Exp Immunol. 2015;179(3):392–7. doi: 10.1111/cei.12463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yamaguchi M, Ohta A, Tsunematsu T, et al. Preliminary criteria for classification of adult Still’s disease. J Rheumatol. 1992;19(3):424–30. [PubMed] [Google Scholar]
- 13.Cush JJ, Thomas A, et al. Adult-onset Still’s disease. Arthritis Rheum. 1987;30(2):186–94. doi: 10.1002/art.1780300209. [DOI] [PubMed] [Google Scholar]
- 14.Grom AA, Mellins ED. Macrophage activation syndrome: advances towards understanding pathogenesis. Curr Opin Rheumatol. 2010;22(5):561–6. doi: 10.1097/01.bor.0000381996.69261.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ikeda N, Kojima H, Nishikawa M, et al. Determination of HLA-A, -C, -B, -DRB1 allele and haplotype frequency in Japanese population based on family study. Tissue Antigens. 2015;85(4):252–9. doi: 10.1111/tan.12536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tilanus MG, Hongming F, van Eggermond MC, et al. An overview of the restriction fragment length polymorphism of the HLA-D region: its application to individual D-, DR- typing by computerized analyses. Tissue Antigens. 1986;28(4):218–27. doi: 10.1111/j.1399-0039.1986.tb00486.x. [DOI] [PubMed] [Google Scholar]
- 17.Furukawa H, Oka S, Kawasaki A, et al. Human leukocyte antigen and systemic sclerosis in Japanese: the sign of the four independent protective alleles, DRB1*13:02, DRB1*14:06, DQB1*03:01, and DPB1*02:01. PLoS One. 2016;11(4):e0154255. doi: 10.1371/journal.pone.0154255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Migita K, Agematsu K, Yazaki M, et al. Familial Mediterranean fever: genotype-phenotype correlations in Japanese patients. Medicine (Baltimore) 2014;93(3):158–64. doi: 10.1097/MD.0000000000000029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Putte LB, Wouters JM. Adult-onset Still’s disease. Baillieres Clin Rheumatol. 1991;5(2):263–75. doi: 10.1016/S0950-3579(05)80283-3. [DOI] [PubMed] [Google Scholar]
- 20.Cimaz R. Systemic-onset juvenile idiopathic arthritis. Autoimmun Rev. 2016;15(9):931–4. doi: 10.1016/j.autrev.2016.07.004. [DOI] [PubMed] [Google Scholar]
- 21.Ombrello MJ. Advances in the genetically complex autoinflammatory diseases. Semin Immunopathol. 2015;37(4):403–6. doi: 10.1007/s00281-015-0498-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sparks JA, Costenbader KH. Genetics, environment, and gene-environment interactions in the development of systemic rheumatic diseases. Rheum Dis Clin North Am. 2014;40(4):637–57. doi: 10.1016/j.rdc.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pouchot J, Sampalis JS, Beaudet F, et al. Adult Still’s disease: manifestations, disease course, and outcome in 62 patients. Medicine (Baltimore) 1991;70(2):118–36. doi: 10.1097/00005792-199103000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Wouters JM, Reekers P, van de Putte LB. Adult-onset Still’s disease. Disease course and HLA associations. Arthritis Rheum. 1986;29(3):415–8. doi: 10.1002/art.1780290316. [DOI] [PubMed] [Google Scholar]
- 25.Fujii T, Nojima T, Yasuoka H, et al. Cytokine and immunogenetic profiles in Japanese patients with adult Still’s disease. Association with chronic articular disease. Rheumatology (Oxford) 2001;40(12):1398–404. doi: 10.1093/rheumatology/40.12.1398. [DOI] [PubMed] [Google Scholar]
- 26.Joung CI, Lee HS, Lee SW, et al. Association between HLA-DR B1 and clinical features of adult onset Still’s disease in Korea. Clin Exp Rheumatol. 2003;21(4):489–92. [PubMed] [Google Scholar]
- 27.Qiu W, James I, Carroll WM, Mastaglia FL, Kermode AG. HLA-DR allele polymorphism and multiple sclerosis in Chinese populations: a meta-analysis. Mult Scler. 2011;17(4):382–8. doi: 10.1177/1352458510391345. [DOI] [PubMed] [Google Scholar]
- 28.Isobe N, Matsushita T, Yamasaki R, et al. Influence of HLA-DRB1 alleles on the susceptibility and resistance to multiple sclerosis in Japanese patients with respect to anti-aquaporin 4 antibody status. Mult Scler. 2010;16(2):147–55. doi: 10.1177/1352458509355067. [DOI] [PubMed] [Google Scholar]
- 29.Mahroum N, Mahagna H, Amital H. Diagnosis and classification of adult Still’s disease. J Autoimmun. 2014;48-49:34–7. doi: 10.1016/j.jaut.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 30.Jardetzky TS, Brown JH, Gorga JC, et al. Three-dimensional structure of a human class II histocompatibility molecule complexed with superantigen. Nature. 1994;368:711–8. doi: 10.1038/368711a0. [DOI] [PubMed] [Google Scholar]
- 31.Sugiura T, Kawaguchi Y, Fujikawa S, et al. Familial Mediterranean fever in three Japanese patients, and a comparison of the frequency of MEFV gene mutations in Japanese and Mediterranean populations. Mod Rheumatol. 2008;18(1):57–9. doi: 10.3109/s10165-007-0003-2. [DOI] [PubMed] [Google Scholar]
- 32.Rabinovich E, Livneh A, Langevitz P, et al. Severe disease in patients with rheumatoid arthritis carrying a mutation in the Mediterranean fever gene. Ann Rheum Dis. 2005;64(7):1009–14. doi: 10.1136/ard.2004.029447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hedrich CM. Shaping the spectrum - from autoinflammation to autoimmunity. Clin Immunol. 2016;165:21–8. doi: 10.1016/j.clim.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 34.Nigrovic PA. Autoinflammation and autoimmunity in systemic juvenile idiopathic arthritis. Proc Natl Acad Sci USA. 2015;112(52):15785–6. doi: 10.1073/pnas.1521837113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Kempen TS, Wenink MH, Leijten EF, Radstake TR, Boes M. Perception of self: distinguishing autoimmunity from autoinflammation. Nat Rev Rheumatol. 2015;11(8):483–92. doi: 10.1038/nrrheum.2015.60. [DOI] [PubMed] [Google Scholar]
- 36.Chen DY, Chen YM, Lan JL, Lin CC, Chen HH, Hsieh CW. Potential role of Th17 cells in the pathogenesis of adult-onset Still’s disease. Rheumatology (Oxford) 2010;49(12):2305–12. doi: 10.1093/rheumatology/keq284. [DOI] [PubMed] [Google Scholar]
- 37.Krogman A, Tilahun A, David CS, et al. HLA-DR polymorphisms influence in vivo responses to staphylococcal toxic shock syndrome toxin-1 in a transgenic mouse model. HLA. 2017;89(1):20–8. doi: 10.1111/tan.12930. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Primers and polymerase chain reaction conditions. (JPG 171 kb)
HLA-DRB1 allele carrier frequency in the patients with AOSD and age-matched healthy controls (1:2). (PDF 57 kb)
Conditional logistic regression analysis between the protective HLA alleles in AOSD. (PDF 43 kb)
Data Availability Statement
Not applicable.


