Historically, sedation for routine gastrointestinal (GI) endoscopy has been directed by the endoscopist (generally with short-acting opioids and benzodiazepines). In recent years, use of monitored anesthesia care (MAC) for GI endoscopy has been increasing, with rates increasing to 47.6%and 53.0%, respectively, in Medicare and commercially insured patients in 2013.1 Monitored anesthesia care requires the presence of an anesthesiology professional and typically involves administration of propofol, leading to a deeper level of sedation. It is estimated that use of MAC for esophagogastroduodenoscopy (EGD) and colonoscopy resulted in additional national expenditures of more than $1 billion for Medicare and commercially insured patients in20092 and is associated with higher rates of 30-day endoscopy-related complications compared with standard sedation.3 Current guidelines recommend considering MAC for patients with anticipated intolerance of standard sedatives or certain comorbidities, but caution that MAC is not cost-effective for average-risk patients undergoing routine procedures.4 Yet, more than half of MAC appears to be used for routine endoscopy in low-risk patients, suggesting widespread guideline-discordant use that may in part be driven by financial incentives.1
To better understand the extent to which increasing MAC use might be driven by financial incentives vs other factors, we assessed trends in MAC use in the Veterans Health Administration (VHA), an integrated health care delivery system with a capitated payment model.
Methods
The institutional review board of the VA Ann Arbor Healthcare System approved this study. The requirement of informed consent was waived due to the retrospective nature of the study. This was a retrospective cohort study using data obtained through the VA Corporate Data Warehouse. The study population consisted of veterans who underwent outpatient EGD and/or colonoscopy at a VHA facility in fiscal years (FY) 2000 through 2013. Cases were identified via Current Procedural Terminology (CPT) codes for colonoscopy and EGD. Cases were identified as having been performed with MAC when one of the relevant procedure codes occurred on the same day as anesthesia CPT codes 00810 or 00740. A cross-sectional validation study found MAC CPT codes to be accurate (sensitivity = 81%, specificity = 93%, κ = 0.74) compared with manual record review. Descriptive statistics were used for data analysis.
Results
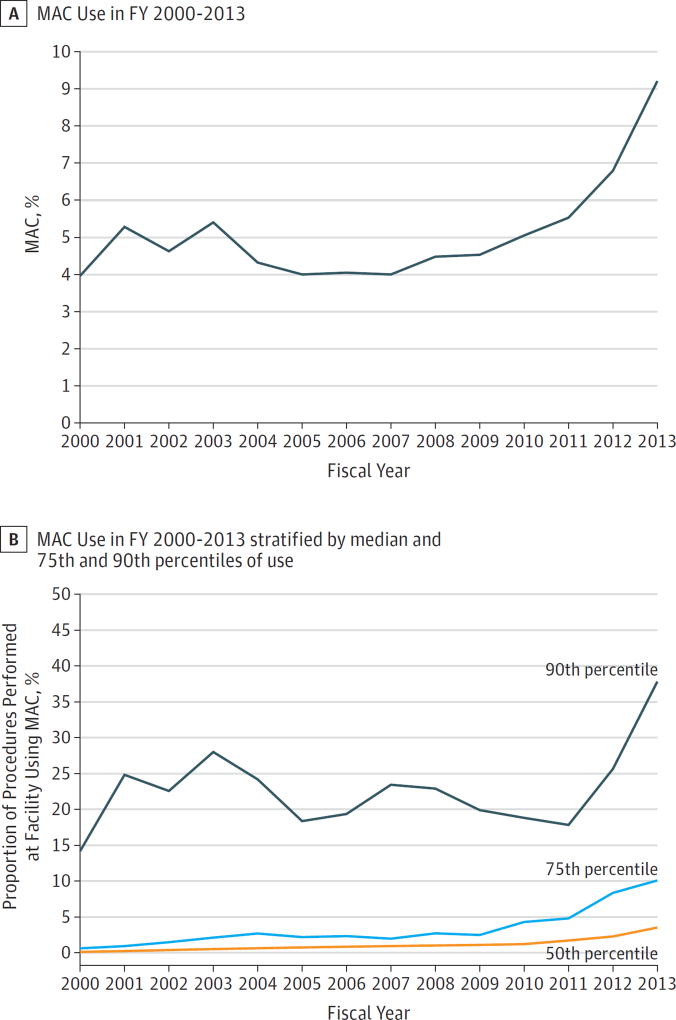
A total of 3 564 085 procedures in 2 091 590 veterans were performed during the study period (Table). Of these, 5.2% (185 910 procedures) used MAC. The percentage of procedures using MAC more than doubled from 4.0% in FY 2000 to 9.3% in FY 2013, with a steady increase in use starting around 2008 (Figure, A). Median facility use of MAC in FY 2000 was 0.11% (interquartile range, 0.00%–0.62%), compared with 3.52% in FY 2013 (interquartile range, 1.13%–10.12%). Facilities varied widely in their overall use of MAC, particularly in the later years of the study period (Figure, B).
Table.
Patient Characteristics and Procedure Type
| Characteristic | Value |
|---|---|
| Age, mean (SD), y | 62.8 (11.0) |
| BMI, mean (SD) | 29.3 (6.1) |
| Sex, No. (%) | |
| Male | 3 376 417 (94.7) |
| Female | 187 664 (5.3) |
| Type of procedure, No. (%) | |
| EGD | 580 005 (16.3) |
| Colonoscopy | 1 939 036 (54.4) |
| Bidirectional endoscopy (EGD and colonoscopy) | 1 045 044 (29.3) |
Abbreviations: BMI, body mass index, calculated as weight in kilograms divided by height in meters squared; EGD, esophagogastroduodenoscopy.
Figure. Use of Monitored Anesthesia Care (MAC).
A, Rate of MAC use for outpatient esophagogastroduodenoscopy and/or colonoscopy in fiscal year (FY) 2000 to 2013. Use of MAC in the Veterans Health Administration more than doubled from 4.0% in FY 2000 to 9.3% in FY 2013. A steady increase in MAC use was noted starting around 2008. B, Trends in overall facility MAC use over time: stratified by facilities at the median, 75th, and 90th percentiles of MAC use nationally. Facilities varied widely in their overall use of MAC, particularly in the later years of the study period.
Discussion
In this study, we sought to better characterize trends in MAC use in a non–fee-for-service environment in which financial incentives are largely absent. While our results demonstrate that MAC use did indeed increase in the VHA over the study period, the overall rate of MAC use in the VHA is substantially lower than that observed in fee-for-service environments, further supporting the existence of prominent financial drivers in the growing use outside the VHA.1
This finding raises important questions, however. If not financial incentives, what other factors are contributing to this observed increase in MAC use? Changes in patient characteristics, such as increased veteran comorbidities or use of prescription opioids (which may confer intolerance to standard sedatives), could perhaps help explain this trend. However, organizational factors influencing health care delivery, including practice culture, patient preference for MAC,5 and increased availability of MAC in the VHA, may also contribute substantially to the increase in VHA MAC use.6 Understanding the presence and degree of inappropriate use of MAC inside and outside the VHA will help promote efficient use of resources and ensure delivery of high-value care.
Acknowledgments
Funding/Support: Dr Adams was supported by National Institutes of Health 5 T32 DK 62708-12 during this research. Dr Krein is supported by a VA Health Services Research and Development Research Career Scientist Award (RCS 11-222). This study was also supported by the Veterans Health Administration’s Office of Informatics and Analytics.
Role of the Funder/Sponsor: The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Adams had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Adams, Prenovost, Kerr, Krein, Rubenstein.
Acquisition, analysis, or interpretation of data: Adams, Prenovost, Dominitz, Kerr, Saini, Rubenstein.
Drafting of the manuscript: Adams, Prenovost.
Critical revision of the manuscript for important intellectual content: Prenovost, Dominitz, Kerr, Krein, Saini, Rubenstein.
Statistical analysis: Adams, Prenovost.
Obtained funding: Kerr.
Administrative, technical, or material support: Kerr.
Supervision: Saini, Rubenstein.
Conflict of Interest Disclosures: None reported.
Disclaimer: The opinions are those of the authors and do not represent those of the Department of Veterans Affairs.
Additional Contributions: We acknowledge the assistance of Robert G. Holleman, MPH, Center for Clinical Management Research, Department of Veterans Affairs, VA Ann Arbor Healthcare System, in data acquisition. He was not compensated for his contributions.
References
- 1.Predmore Z, Nie X, Main R, Mattke S, Liu H. Anesthesia service use during outpatient gastroenterology procedures continued to increase from 2010 to 2013 and potentially discretionary spending remained high. Am J Gastroenterol. 2016 doi: 10.1038/ajg.2016.266. [DOI] [PubMed] [Google Scholar]
- 2.Liu H, Waxman DA, Main R, Mattke S. Utilization of anesthesia services during outpatient endoscopies and colonoscopies and associated spending in 2003–2009. JAMA. 2012;307(11):1178–1184. doi: 10.1001/jama.2012.270. [DOI] [PubMed] [Google Scholar]
- 3.Cooper GS, Kou TD, Rex DK. Complications following colonoscopy with anesthesia assistance: a population-based analysis. JAMA Intern Med. 2013;173(7):551–556. doi: 10.1001/jamainternmed.2013.2908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lichtenstein DR, Jagannath S, Baron TH, et al. Standards of Practice Committee of the American Society for Gastrointestinal Endoscopy. Sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2008;68(5):815–826. doi: 10.1016/j.gie.2008.09.029. [DOI] [PubMed] [Google Scholar]
- 5.Agrawal D, Rockey DC. Propofol for screening colonoscopy in low-risk patients: are we paying too much? JAMA Intern Med. 2013;173(19):1836–1838. doi: 10.1001/jamainternmed.2013.8417. [DOI] [PubMed] [Google Scholar]
- 6.Adams MA, Saleh A, Rubenstein JH. A systematic review of factors associated with utilization of monitored anesthesia care for gastrointestinal endoscopy. Gastroenterol Hepatol (N Y) 2016;12(6):361–370. 20. [PMC free article] [PubMed] [Google Scholar]