Abstract
We have evaluated objectively pain tolerance in transrectal ultrasound-guided prostate biopsy (TRUS) using local periprostatic per rectal anesthesia as compared to the conventional method. From November 2008 to May 2009, 90 patients underwent transrectal ultrasound-guided prostate biopsy at Department of Urology, Clinical Center University Sarajevo. 90 patients who fulfilled the inclusion criteria were randomized into 3 groups of 30 patients each. Group 1 received periprostatic local anesthesia with 2% lidocaine, group 2 received Voltaren supp placed in rectum an hour before biopsy while group 3 received no local anesthesia. Pain scale responses were analyzed for each aspect of the biopsy procedure with a visual analog scale of 0-none to 10-maximal. There was no difference between the 3 groups in pain scores during digital rectal examination, intrarectal injection and probe insertion. The mean pain scores during needle insertion in group 1 receiving periprostatic nerve block and in group 2 receiving Voltaren supp were 3,10 ± 2,32 and 5,15 ± 2,01 respectively. In group 3 (no local anesthesia), mean pain scores were 6,06 ± 2,95 which was found to be significantly different (p < 0,001). However, morbidity after the biopsy was not statistically different between all 3 groups. TRUS-guided prostate biopsy is a traumatic and painful experience, but the periprostatic blockage use is clearly associated with more tolerance and patient comfort during the exam. It is an easy, safe, acceptable and reproducible technique and should be considered for all patients undergoing TRUS biopsy regardless of age or number of biopsies.
Keywords: prostate biopsy, TRUS ultrasonography, local anesthesia and pain score
INTRODUCTION
Transrectal ultrasound-guided prostate biopsy has become essential in diagnostic investigation of patients with clinical suspicion of prostatic neoplasia due to gland alterations resulting from abnormality on the digital rectal examination or rising of the prostatic specific antigen (PSA) (1, 2). Prostatic biopsy indication has been increasing in the last years as a result of the increase in life expectancy, better diagnostic methods, and Public Health Campaigns intensification (3, 4). This procedure is performed by most urologists, in the United States and in England, without any kind of anaesthesia or sedation (5, 6). Apart from the embarrassment and the anxiety, this exam is almost always accompanied by pain sensation, because of TRUS probe introduction, or by biopsy itself (7). Some series show that 11 to 90% of patients have pain during the exam, making the realization of this diagnostic procedure traumatic (8, 9). However, the method of pain measurement by several studies has been subjective, underestimating sometimes the real upset suffered by the patients. Our aim was to randomly compare the use of periprostatic blockage, Voltaren supp. placed in rectum to the conventional prostate biopsy procedure. In order to achieve this, we used objective criteria for pain analysis, considering the importance of pain components related to puncture itself, to the transrectal probe, and evaluating the satisfaction and tolerance facing the possibility of re-biopsy need.
MATERIALS AND METHODS
Between November 2008 to May 2009, 90 consecutive men undergoing TRUS prostate biopsy in the Department of Urology at the University Clinical Centre Sarajevo, were entered into this study. Indications for biopsy included an abnormal digital rectal prostate examination or transrectal ultrasound scan and/or elevated prostate specific antigen (PSA) (> 4 ng/mL). Lidocaine and diclofenac allergy, haemorrhagic diathesis, anticoagulation therapy (users of drugs affecting coagulation), acute prostatitis, inflammatory diseases, or other rectal conditions and an inability to rate a visual analogue scale (VAS) were the exclusion criteria (Figure 1.). Patients received 500 mg ciprofloxacin the night before and two hours prior to the procedure. Once informed consent was obtained, patients were randomized into three groups. All patients were examined in the left lateral decubitus position. The TRUS guided biopsies were performed using a Siemens Sonoline S40 with a 10 MHz probe. In Group 1, local anaesthesia was performed with 4 periprostatic injections of 2,5 ml of 1% lidocaine hydrochloride without epinephrine, TRUS-guided, using a 25 cm x 22-G needle, introduced through the biopsy guide, after the chance of vascular puncture by aspiration has been excluded (Figure 2.). The applications were executed in the neurovascular bundle region (cross-section) and in prostatic apex (longitudinal section), bilaterally TRUS guided. Patients belonging to Group 2 received Voltaren supp. placed in rectum an hour before biopsy. In Group 3 patients received no anesthesia and conventional biopsy was preformed by single intrarectal application of 20 ml of hydrophilic gel lubricant before the procedure. Ten prostatic fragments were removed from: apex, midgland, base, midlateral region and transition zone. Before the examination, patients received a Visual analogica! scale for pain (VAS) which was explained to them. The assessment ranges from 0 (no pain) to 10 (unbearable pain) and was measured during anaesthesia (VAS 1) and immediately after the biopsy procedure (VAS 2). Patients were reviewed by the urologist two weeks after biopsy and data were recorded. Rectal bleeding, gross haematuria, haemospermia, dysuria, fever and any other complication following the biopsy were also noted. Results were analyzed and the differences between the groups in VAS pain score were compared using the Mann-Whitney U test. A p value less than 0,05 were considered statistically significant.
FIGURE 1.
Visual analogical scale for pain
FIGURE 2.
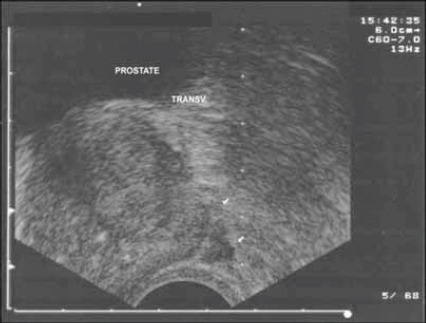
Ecographic (TRUS) image of the prostate base, injection of solution in the periprostatic region
RESULTS
Our study included 90 patients, divided in three groups. Each group consists form 30 patients (Table 1.). Among the 90 men, 30 were randomized to receive periprostatic nerve block-lidocaine (Group 1) and 30 to be infiltrated by Voltaren supp (Group 2). Control group (Group 3), 30 patients received no anaesthesia; conventional biopsy was preformed single intrarectal application of 20 ml of hydrophilic gel lubricant before the procedure. Each patient underwent ten core biopsies (five on each lobe). A lower number of cores were chosen when the diagnosis of prostate cancer was obvious on abnormal DRE and/or by a high PSA level. A higher number of cores were obtained for the patients who had had a previous prostate biopsy. All three groups were similar with respect to age, PSA, prostate volume, findings of the digital rectal examination, previous prostate biopsy, number of cores and pathological findings at needle biopsy. There was no difference between all three groups in pain scores during digital rectal examination, intrarectal injection and probe insertion. Before the examination, patients received a VAS which was explained to them. The assessment ranges from 0 (no pain) to 10 (unbearable pain) and was measured during anaesthesia (VAS 1), and immediately after the biopsy procedure (VAS 2). Patients were reviewed by the urologist three weeks after biopsy and data were recorded.
TABLE 1.
Characteristics of study groups (Group I, II, III)
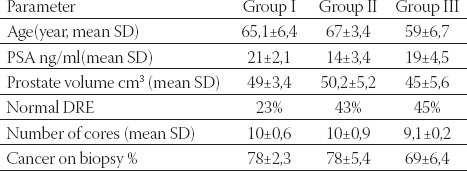
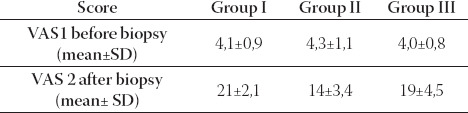
The mean pain scores during needle insertion in Group 1 receiving periprostatic nerve block and in group 2 receiving Voltaren supp were 3,10 ± 2,32 and 5,15±2,01 respectively. In Group 3 (no local anaesthesia), the mean pain scores were 6,06 ± 2,95 and were found to be significantly different (p < 0,001) when compared to Group 1 and 2. However, morbidity after the biopsy was not statistically different between all 3 groups (Figure 3.). Regarding the VAS pain scores, a significant difference existed between the two groups for VAS 1 and VAS 2 in all groups, with an advantage for the control gel group (Table 2.). During the biopsy procedure, the lidocaine injection led to lower pain score values than in Group 2 with statistically significant difference. Mild pain or no pain was experienced by the vast majority of the patients in each group. An advantage in the lidocaine injection group (Group 1) was statistically demonstrated with less pain as indicated by the mean VAS 1 and 2 pain score values, though the mean VAS 2 pain score was lower in all three groups. None of the patients developed any anesthetic complication such as rectal wall haematoma, excessive rectal bleeding or systemic lidocaine toxicity. All patients were examined three weeks after the procedure. Three patients (1%) in Group 1 and four (1,2%) in Group 2 complained of prolonged haematuria. A lengthy haemospermia was noted for four cases (1,2%) in Group 1 and two (0,9%) in Group 3. No other complication was noted. None of the patients complained of acute urinary retention, persistent rectal haemorrhage or fever.
FIGURE 3.
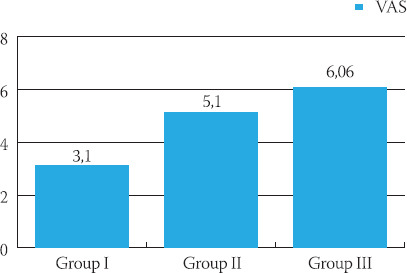
VAS characteristics of study groups (Group Ι, II, III)
TABLE 2.
VAS characteristics of study groups (Group I, II, III) before and after biopsy
DISCUSSION
Recently, various types of local anaesthesia have been proposed to reduce the pain and decrease the discomfort associated with prostate biopsy. Transrectal ultrasound prostatic biopsy has evolved into a standard procedure for diagnosing prostate cancer. Though improvements in the biopsy procedure have been introduced over the years, pain and discomfort still remain the most common side effects. This does not mean that general anaesthesia should be used routinely for TRUS guided prostate biopsy (10, 11, 12). The different attempts have been made to investigate the use of anaesthesia in maintaining a VAS pain score of 0 to 10, which corresponds to a rating of mild pain. In this study, the VAS pain score data appear to be relatively low (less than 4 for the mean data). Complications after anaesthesia or biopsy were the same for all groups (haematuria, anal bleeding, fever, prostatitis) and were rare. As generally described in the literature, no major complication was found, the most common minor complications being haematuria or haemospermia. The obvious necessity of reducing discomfort of TRUS-guided prostate biopsy is represented by the increasing number of recent papers in this field. Collins et al. (13) reported that 20 (22%) of 89 patients had pain during the procedure. Desgrandchamps et al. (14) observed moderate to severe pain in 13 (12%) of 109 patients. Peyromaure et al. (15) reported that only 51 (18.6%) of 275 patients submitted to prostate biopsy with 10 fragments, related no pain or discomfort. However, Aus et al. (16) observed this symptom in only 24 (7%) of 343 patients studied, and one should note that an average of 2,6 biopsies per patient was performed. However, in our study, 73% of patients undergoing prostate biopsy with 10 fragments had moderate to intolerable pain when blindly evaluated by an objective questionnaire. There was an important reduction of pain compared to placebo group (p<0,0001), with no additional complication. Taverna et al. (17) reported that 93 (93%) of 100 patients had from absence of pain to moderate pain with periprostatic blockage performed with 10 ml of 1% lidocaine, compared to the presence of moderate to severe pain in 55 (55%) of 100 patients where no anaesthetic procedure was performed. Of 30 patients in our study submitted to local periprostatic anesthesia with lidocaine, 13 (39%) had mild pain sensation, just 1 (3%) patient complained of moderate pain, and 2 (6%) had severe, but tolerable pain. No patient complained of intolerable pain. The statistical difference observed confirms the periprostatic blockage superiority when compared to conventional biopsy with no analgesic and Voltaren supp. Due to anesthetic blockage of capsular sensitive fibers, there is an important reduction on pain sensation related by patients. As the procedure progresses, the patient feels less anxious and more relaxed, not contracting the pelvic muscles, making the exam more tolerable. Probably there is some degree of systemic drug absorption due to the great absorptive capacity of rectal mucosa (18). There are no doubts that our data show the statistic superiority of periprostatic blockage in this group compared to the placebo group. Biopsy becomes much more soothe and tolerable with Voltaren supp., but local anaesthesia with lidocain is mode of anaesthesia which is safe and effective in reducing discomfort.
CONCLUSION
Periprostatic local anaesthesia promotes significant pain reduction, making the TRUS-guided prostate biopsy well tolerated by the patients. We believe that some analgesia method must be routinely performed during this exam. In this context, the periprostatic anaesthesia is a feasible and low cost option, and can be performed as an outpatient procedure with no additional morbidity.
List of Abbreviations
DRE -digital rectal examination
PSA -prostate-specific antigen
TRUS -transrectal ultrasound
VAS -visual analogical scale
REFERENCES
- 1.Irani J, Fournier F, Bon D. Patient tolerance of transrectal ultrasound-guided biopsy of the prostate. Br. J. Urol. 1997;79:608–610. doi: 10.1046/j.1464-410x.1997.00120.x. [DOI] [PubMed] [Google Scholar]
- 2.Hodge KK, McNeal JE, Terris M.K. Random systematic versus directed ultrasound guided transrectal core biopsies of the prostate. J. Urol. 1989;142:71–76. doi: 10.1016/s0022-5347(17)38664-0. [DOI] [PubMed] [Google Scholar]
- 3.Soloway MS, Obek C. Periprostatic local anesthesia before ultrasound guided prostate biopsy. J Urol. 2000;163:172–173. [PubMed] [Google Scholar]
- 4.Machado MT, Simardi L.H, Pinto MA, Eiger A, Freitas JPA, Borelli M, Wroclawski ER. 1st Prostate Health Campaign of ABC Medical School. Pathologic results of needle biopsy. Arq. Med. ABC. 2000;23:12–17. [Google Scholar]
- 5.Crundwell MC, Cooke PW, Wallace DMA. Patients’ tolerance of transrectal ultrasound-guided prostatic biopsy: an audit of 104 cases. BJU Int. 1999;83:792–795. doi: 10.1046/j.1464-410x.1999.00011.x. [DOI] [PubMed] [Google Scholar]
- 6.Soloway MS, Öbek C. Periprostatic local anesthesiabefore ultra-sound guided prostate biopsy. J. Urol. 2000;163:172–173. [PubMed] [Google Scholar]
- 7.Naughton CK, Ornstein DK, Smith DS, Catalona WJ. Pain and morbidity of transrectal ultrasound guided prostate biopsy: A prospective randomized trial of 6 versus 12 cores. J. Urol. 2000;163:160–171. [PubMed] [Google Scholar]
- 8.Nash PA, Bruce JE, Indudhara R, Shinohara K. Transrectal ultrasound guided prostatic nerve blockade eases systematic needle biopsy of the prostate. J. Urol. 1996;155:607–609. [PubMed] [Google Scholar]
- 9.Al-Ghazo MA, Ghalayini IF, Matalka II. Ultrasound-guided transrectal extended prostate biopsy: a prospective study. Asian J Androl. 2005;7:165–169. doi: 10.1111/j.1745-7262.2005.00019.x. [DOI] [PubMed] [Google Scholar]
- 10.Melzack R, Torgenson WS. On the language of pain. Anesthesiology. 1971;34:50–59. doi: 10.1097/00000542-197101000-00017. [DOI] [PubMed] [Google Scholar]
- 11.Benoit G, Merlaud L, Meduri G, Moukarzel NM, Quillard J, Ledroux M, Giuliano F, Jardin A. Anatomy of the prostatic nerves. Surg. Radiol Anat. 1994;16:23–29. doi: 10.1007/BF01627917. [DOI] [PubMed] [Google Scholar]
- 12.Leibovici D, Zisman A, Siegel YI, Sella A, Kleinmann J, Lindner A. Local anesthesia for prostate biopsy by periprostatic lidocaine injection: a double-blind placebo controlled study. J. Urol. 2002;167:563–565. doi: 10.1016/S0022-5347(01)69086-4. [DOI] [PubMed] [Google Scholar]
- 13.Collins GN, Lloyd SN, Hehir M, Mckelevie GB. Multiple transrectal ultrasound-guided prostatic biopsies-true morbidity and patient acceptance. British J Urol. 1993;71:460–463. doi: 10.1111/j.1464-410x.1993.tb15993.x. [DOI] [PubMed] [Google Scholar]
- 14.Desgrandchamps F, Meria P, Irani J, Desgrippes A, Teillac P, Le Duc A. The rectal administration of lidocaine gel and tolerance of transrectal ultrasonography-guided biopsy of the prostate: A pro-spective randomized placebo-controlled study. BJU Int. 1999;83:1007–1009. doi: 10.1046/j.1464-410x.1999.00080.x. [DOI] [PubMed] [Google Scholar]
- 15.Peyromaure M, Ravery V, Messas A, Toublanc M, BocconGidob L. Pain and morbidity of an extensive prostate 10-biopsy protocol: a prospective study in 289 patients. J. Urol. 2002;167:218–221. [PubMed] [Google Scholar]
- 16.Aus G, Damber JE, Hugosson J. Prostate biopsy and anaesthesia: an overview. Scand. J. Urol. Nephrol. 2005;39:124–129. doi: 10.1080/00365590510007784. [DOI] [PubMed] [Google Scholar]
- 17.Taverna G, Maffezzini M, Benetti A, Seveso M, Giusti G, Graziotti P. A single infection of lidocaine as local anesthesia for ultrasound guided neddle biopsyof the prostate. J. Urol. 2002;167:222–223. [PubMed] [Google Scholar]
- 18.Yun TJ, Lee HJ, Kim SH, Lee SE, Cho JY, Seong CK. Does the intrarectal instillation of lidocaine gel before periprostatic neurovascular bundle block during transrectal ultrasound guided prostate biopsies improve analgesic efficacy? A prospective, randomized trial. J Urol. 2007;178:103–106. doi: 10.1016/j.juro.2007.03.047. [DOI] [PubMed] [Google Scholar]


