Abstract
Pregnancy represents a risk factor in the occurrence of vaginal candidosis. The objectives of our study were: to make determination of the microscopic findings of vaginal swab, frequency of Candida species in the culture of pregnant women and patients who are not pregnant, determine the Candida species in all cultures, and to determine the frequency and differences in the frequency of C. albicans and other non-albicans species. In one year study performed during 2006 year, we tested patients of Gynaecology and Obstetrics clinic of the Clinical Centre in Sarajevo and Gynaecology department of the General hospital in Sarajevo. 447 woman included in the study were separated in two groups: 203 pregnant (in the last trimester of pregnancy), and 244 non-pregnant woman in period of fertility. Each vaginal swab was examined microscopically. The yeast, number of colonies, and the species of Candida were determined on Sabouraud dextrose agar with presence of antibiotics. For determination of Candida species, we used germ tube test for detection of C. albicans, and cultivation on the selective medium and assimilation tests for detection of non-albicans species. The results indicated positive microscopic findings in the test group (40,9%), as well as greater number of positive cultures (46,8%). The most commonly detected species for both groups was C. albicans (test group 40.9% and control group 23,0%). The most commonly detected non-albicans species for the test group were C. glabrata (4,2 %) and C. krusei (3,2%), and for the control group were C. glabrata (3,2%) and C. parapsilosis (3,2%). The microscopic findings correlated with the number of colonies in positive cultures. In the test group, we found an increased number of yeasts (64,3%), and the pseudopyphae and blastopores by microscopic examination as an indication of infection. In the control group, we found a small number of yeasts (64,6%), in the form of blastopores, as an indication of the candida colonisation. Our results indicate that gravidity, as the risc factor for incidence of infection, has the significant role in the incidence of vaginal candidosis.
Keywords: vaginal candidosis, pregnancy- risk factor, Candida albicans, non-albicans species
INTRODUCTION
Vaginal candidosis is a vaginal mucosis infection caused by species of the genus Candida. It is one of the most common vaginal infections in women, in the fertile period, and also the most frequent and most important fungal disease of vaginal content (1). Women around the world get diagnosed of vaginal candidosis. It is estimated that 75% of women during the fertile period have at least one episode of vaginal candidosis. Approximately 40-50% of women have repeated infection. Less than 5% of adult female population receives repeated, frequent attacks of recurrent vulvovaginal candidosis. Point-prevalence studies indicate that Candida species may be isolated from the genital tract of approximately 20% (range 10-55%) of asymptomatic, healthy women in the child-bearing age (2). Twenty five to 40% of women who are culture positive for Candida species in the vaginal area are asymptomatic carriers. The natural history of asymptomatic colonization is unknown, although limited human studies suggest that vaginal carriage may continue for several months and perhaps years. In the United States, Candida species is now the second most common cause of vaginal infections, while in Europe it is listed as the primary cause (3). Until recently, the problem of vaginal candidosis was often ignored by medics, or treated as an insignificant problem for the female population. It received more attention only after Herman Gardner said: “Vaginitis can cause more inconvenience than any other gynaecological disease. In addition, many mental and emotional problems are associated with vaginitis “(4). Documented risk factors of vaginal candidosis are pregnancy (30-40%), use of high estrogen content oral contraceptives, antibiotics, steroids, chemotherapeutics, attendence at sexually transmitted diseases clinics and age (5). The increased secretion of reproductive hormones during pregnancy favors the formation of infection (6). High levels of estrogen provide an increased amount of glycogen in the vagina, furthermore providing a good source of carbon needed for candida growth and their germination. These hormones accelerate the formation of yeast pseudopyphae. Vaginal candidosis is rare in postmenopausal women and girls, due to hormonal dependence of vaginal candidosis (1). There is a balance between candida, normal bacterial flora, and immune defence mechanisms. When this balance is disturbed, colonization is replaced by infection. Vaginal candidosis is one of the mucous opportunistic infections, and also one of the most common infections of the genital system. It is still not definitively determined what exactly leads to disruption of the balance and origin of infection. Vaginal candidosis occurs in the presence of factors that increase the virulence of candida, and as a result of the reduction in local defence mechanisms. The exact mechanism by which candida infection occurs is not clear. It is possible that there are multiple mechanisms by which candida can cause cell damage and lead to direct invasion of the infection hyphae in epithelial tissues (6). During vaginal candidosis, vagina is the normal pH range (pH 4,0-4,5), as opposed to mixed infections (bacterial, trichomonas), where pH rises to levels greater than 4,7. Numerous studies around the world show that Candida albicans is responsible for the largest number of symptomatic episodes of vaginal candidosis. Percentage of infection that causes C. albicans was high in the past decades, and varied from 85 to 90% (8, 5). Non-albicans species are most commonly represented by C. glabrata, and C. tropicalis (9, 5). During the 1970s, the incidence of non-albicans species in the United States amounted to 5-10%. The objectives of our study were: to analyze the microscopic findings of vaginal swabs, determine the frequency of Candida species occurrence in cultures of pregnant and non-pregnant women; determine Candida species in all cultures; determine the frequency of C. albicans occurrence, as well as differences in the frequency of C. albicans and other non-albicans species.
MATERIALS AND METHOD
Respondents
This one year study performed during 2006 year. The trial included female patients with Gynaecology-Ob- stetrical Clinics at the University of Sarajevo Clinics Centre, and female patients of the Gynaecology Department at the General Hospital in Sarajevo. Study included total of 447 women, divided into two groups. Test group included 203 pregnant women in the last trimester of pregnancy, while control group included 244 non-pregnant women in the fertile period. In both groups, female patients were handled with clear clinical picture of colpitis, and showed no symptoms that would be indicators of any diseases. Age of female patients in both groups was within the range of 20 to 38. Criteria for inclusion of subjects into the test group was eight or ninth lunar month of pregnancy.
Research Methodology
Sampling
Samples were obtained by vaginal swabs from both experimental groups. Samples were taken by sterile swab, under the gynaecological review. A number of women in both groups exhibited symptoms that indicated a possible existence of vaginal candidosis, while others had no symptoms or indications of other problems.
Microscopie examination
Examination was done at the Institute for Clinical Microbiology, University of Sarajevo Clinics Centre. Each sample of vaginal swab was stained by methylene blue and examined microscopically (40x). Presence of regular blastopores, as well as pseudopyphae and blastopores, was determined by this method.
Yeast isolation
Mycological vaginal cultures were prepared at Institute for Clinical Microbiology, University of Sarajevo Clinics Centre. Each sample of vaginal swab was further cultivated on Sabouraud’s agar, with the addition of antibiotics to prevent growth of bacterial flora. After 48 hours of incubation at 37°C, cultures were separated into positive (growth of yeast) or negative cultures (no yeast growth). Using this approach, we isolated and determined the number of yeast colonies.
Yeast identification
a) Germ tube test
Test proves yeast germination, and it is characteristic for the detection Candida albicans (unless when yeast germination is not characteristic).
b) Cultivation on the selective medium (Chrom agar)
Chrom agar is selective medium, which indicates an increase in the number of non-albicans species based on a colour change. It can be used for identification of individual non-albicans species, as well as C. albicans, if germ tube test was not characteristic. All positive cultures from both experimental groups were cultivated on a Chrom agar. After incubation in the thermostat (48 hours at 37’C), identification of yeast was preformed based on a colony colour. Using this method, we were able to identify the following individual nonalbicans species: C. glabrata (dark pink colonies, wet), C. tropicalis (blue colonies, wet), C. krusei (light pink colonies, dry), and C. albicans (green colonies, wet).
c) Yeast assimilation test (API test)
This test represents the safest identification of non-albi- cans species. Test is based on the ability of yeast to assimilate coal hidra (organic compounds). We used the premade factory tests of high sensitivity and precision (API 20C AUX). It is important to note that this test is performed only with the so-called ‘pure cultures.’ Due to the reliability of this method, we tested all non-albi- cans species using this test, confirming the results obtained by cultivation on Chrom agar. We also tested for other non-albicans species (egg, Candida kefyr, Candida guilliermondii, Candida famata and others).
RESULTS
Results of microscopic examination
From the test group, of the total number samples of test group, 59,1% (120/203) showed negative using the microscopic examination, while 40,9% (83/203) were observed as positive. From the control group, of the total number samples of control group, 76,2% (186/244) of microscopic findings were determined as negative, while 23,8% (58/244) correlated to positive. Positive microscopic findings (Figure 1. and 2.) were more frequent in the test group, as opposed to the control group (Graph 1.). The differences between the two groups is statistically significant (p=0,003; p<0,05).
FIGURE 1.
Positive microscopic findings blastopores in vaginal smear (methylene blue 100 x)
FIGURE 2.
Positive microscopic findings pseudopyphae and blastopores in vaginal smear (methylene blue 100x)
GRAPH 1.
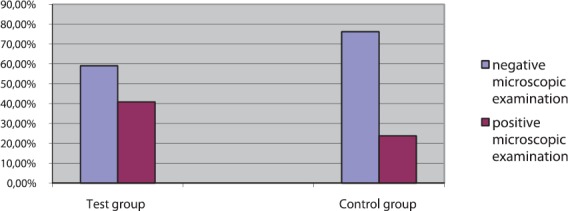
Microscopic examination findings, vaginal smear control (n=244) and test (n=203) groups
Results of isolation
Results growth of Candida species on Sabouraud’s agar Test group showed 46,8% (95/203) positive cultures and 53,2% (108/203) negative cultures. From the control group showed 25,4% (62/244) positive cultures while 74,6% (182/244) correlated to negative cultures. Positive cultures (Figure 3.) were more frequent in the test group, as opposed to the control group (Graph. 2). The difference between the two groups is statistically significant (p=0,028; p<0,05). The results are separated in four groups: the growth of up to 50 yeast colonies, an increase from 50 to 100 colonies, an increase from 100 to 200 colonies, and 200 yeast colonies and more, for both test and control groups. The largest number of colonies was observed in the test group (24,2 %, 95/23), while the lowest number of colonies was observed in the control group (14,5 %, 62/9) (Table 1).
FIGURE 3.

Positive culture of yeast on Sabouraud’s agar
GRAPH 2.
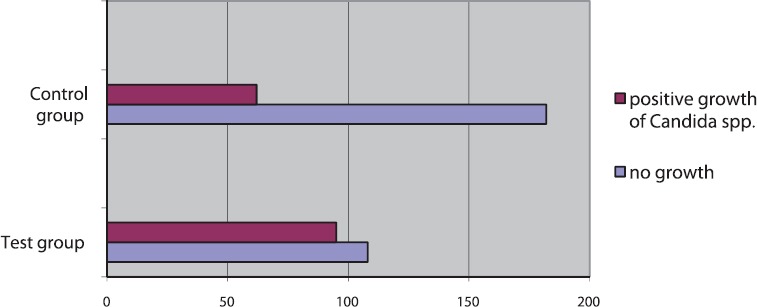
Positive and negative cultures in test (n=203) and control groups (n=244)
TABLE 1.
Number of yeast colonies in positive cultures of test (n=95) and control groups (n=62)

Determination and the frequency of C. albicans; germ tube test
The positive germ tube test (Figure 4) determined a greater number of C. albicans 40,9% (83/203) in the test group, compared to the control group 23,0% (56/244). Germination test for the test group was negative 15,9% (12/203) of sampled subjects, while 2,4% (6/244) turned negative in the control group (Graph 3). The difference between the two groups is statistically significant (p=0,036; p<0,05).
FIGURE 4.

Positive germ tube test (Candida albicans]
GRAPH 3.
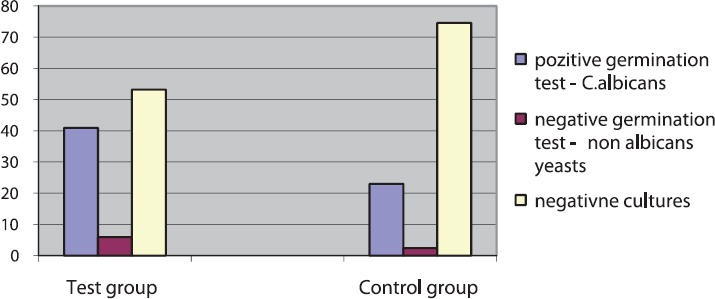
Results of germ tube test in relation to the total number of samples (determination of C. albicans) for test (n=203) and control groups (n=244)
Determination andfrequency of the non-albicans species on selective medium
Experiment shows the number of positive cultures of non-albicans species in test and control groups, elaborated on a selective medium (Chrom agar) (Figure 5.). Cultivation on Chrom agar could not be used for identified of all non-albicans species, therefore, we tested all positive cultures using an API test. In the test group, the most commonly identified species were C. glabrata (4,2 %, 4/95) and C. krusei (3,2 %, 3/95). In the control group, the most commonly detected species were C. glabrata (3,2%, 2/62) and undetermined non-albicans species (3,2%, 2/62) (Table 2). There is no significant difference between the results of identification and frequency to individual non-albicans species in relation to the test and control group (p=0,350; p<0,05).
FIGURE 5.
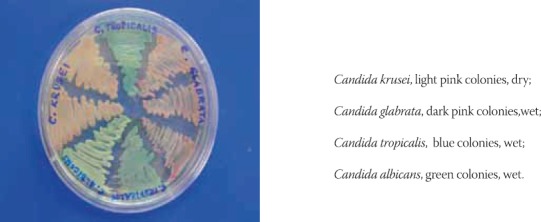
Determination of Candida species on Chrom agar medium
TABLE 2.
Results of identification of Candida species on selective medium of positive cultures for test (n=95) and control groups (n=62)

Determination and the frequency non-albicans species using assimilation test (API test)
Analysis of all positive cultures from the test group (n=95) yielded detection of C. glabrata in 4 samples (4,2%), C. krusei in 3 samples (3,2%), C. tropicalis 2 in samples (2,1%), C. parapsilosis in 2 samples (2,1 %), and C. guilliermondii in 1 sample (1,1%). Analysis of all positive cultures from the control group (n=62) yielded detection of C. glabrata in 2 samples (3,2%), C. parapsilosis in 2 samples (3,2%), C. krusei in 1 sample (1,6 %), and C. tropicalis in 1 sample (1,6 %), while C. guilliermondii was not detected, as was the case with the test group (Graph 4). There is no significant difference between the results of identification and frequency to individual non-albicans species in relation to test and control groups (p=0,378; p>0,05).
GRAPH 4.
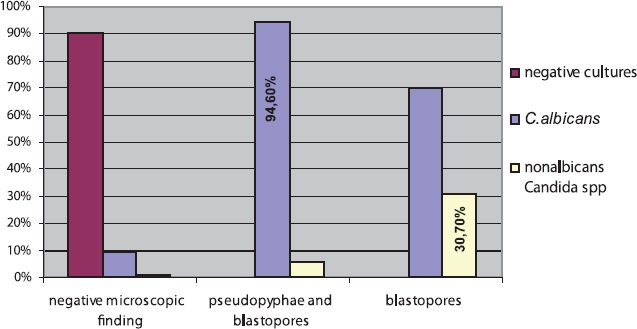
Correlation the results of Candida species and microscopic examination of test group
Correlation between the results of germ tube test and the microscopic findings (only blastospores or blastospores with pseudomycelium) of vaginal swab
In the test group, the maximum frequency of pseudopyphae and blastopores, established at C. albicans in 94,6% (53/56), and blastopores, at non-albicans species in 30,7% (8/27) of the samples. (Table 3, Graph. 5). In the control group, the maximum frequency of pseudopyphae and blastopores, established at non-albicans species in 15,0% (3/56), and blastopores, at C. albicans in 97,3% (36/37) of the samples (Table 4, Graph. 6). There is a significant difference between determined Candida species and microscopic examination for both groups (p=0,0001; p<0,05).
TABLE 3.
Correlation the results of Candida species and microscopic examination of test group

GRAPH 5.
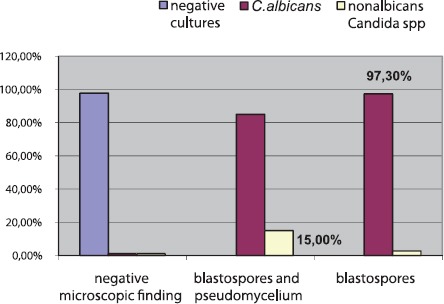
Correlation the results of Candida spp. and microscopic examination of control group
TABLE 4.
Correlation the results of Candida species and microscopic examination of control group

DISCUSSION
Candida species in the vaginal mucosa was found in 35% of healthy women (10). Numerous studies worldwide show that Candida albicans are responsible for the greatest number of symptoms associated with the vaginal candidosis. It is important to emphasize that in the past three decades there has been an increasing percentage of infections caused by non-albicans species. These non-albicans species are often resistant to conventional therapy (11). In the he microscopic specimens, simple blastopores are usually detected. There is a delicate balance between Candida species, normal bacterial flora, and immune defence mechanisms. When this balance is disturbed, colonization usually results in the occurrence of vaginal candidosis. It is one of the mucous opportunistic infections, and also one of the most common infections of the genital system. Mechanisms that lead to the disruption of this balance are still unclear, and origins of the infection remain uncertain (5). Disorders of immune systems and host defence mechanisms contribute to the colonization of the genital system by yeast, which is then transformed into the manifest form of vaginal candidosis. This condition is accompanied by appropriate symptoms, clinical features and mycological findings. Blastopores stretch, and hyfe become formed and carried out the invasion of tissue. Vaginal candidosis is the infection of women in the reproductive age, and it is very rare in postmenopausal women and girls, which indicates the hormone dependence of infection (12). Hamad at al. (13) examined the ability of estrogens to induce of vaginal candidosis in the case when there is no infection, or if it already exists. The obtained results clearly indicate that estrogens are able to disrupt the relationship between Candida species and host and lead to infection. During pregnancy, which is listed as a risk factor, vagina is more sensitive, and the infections occur significantly more often. This is especially true in the last trimester of pregnancy, due to the increased amount of glycogen in the vagina and high levels of hormones (with estrogens being the most important). It provides a good source of carbon, which favours the growth of Candida species Fidel at al. (14) demonstrated the effect of reproductive hormones on experimental vaginal candidosis, and put forward the hypothesis that despite high levels of progesterone during pregnancy, the high incidence of vaginitis pregnant women is related to levels of estrogens, which is in turn considered the primary factor for the occurrence of infection. Vaginal candidosis usually has pronounced symptoms in women in the last trimester of pregnancy, and infection is often repeated. Our results clearly demonstrate significantly increased the number of positive microscopic findings in pregnant women (40,9%, 83/203), compared to 23,8% (58/244) in non-pregnant women. Newmann at al. (15) investigated two groups of respondents, pregnant (n=251) and non-pregnant (n=232) women, in a similar way, using the microscopic preparation. Their results indicated a greater representation of the positive microscopic findings in the test group (36,7%), compared to the control group (19,9%), and their values corresponded with our findings. When we speak of the candida existence in vaginal swab, and possibility features that give saprophyte the ability to change forms and cause an infection, it is necessary to have insight into the mycological findings at the culture of Candida species. Our results of cultivation and isolation of yeast on a selective medium Sabouraud’s agar, showed fewer positive cultures (25,4%, 62/244) in non-pregnant women, compared to pregnant women (46,8%, 95/203). Holland at al. (16) investigated a number of vaginal swab samples (n=5802) over the course of two months in 2000, and obtained the results similar to ours. The number of positive cultures in their study was 1221 (21%). In the study where they examined women (n=442), the number of positive cultures was 180 (42%). Their results were similar to ones obtained by our group, given that the number of tested subjects was different than ours. Other authors obtained similar results in their studies. Eckert at al. (17) examined the vaginal swabs in two groups. Their control group contained women who were on a regular gynaecological control (n=774), and the number of positive cultures in this group was 201 (25,9%). The test group contained a number of risk factor pregnant women (n=545), and number of positive cultures in this group was elevated (52,8%). These results are consistent with our studies. The results of Enweani at al. (18) showed a greater percentage of the vaginal yeast detected in pregnant women (51,5%, 203/394), compared to non-preg- nant women (40,6%, 43/106). This study showed a significant statistical difference in the results between the two examined groups, which is fully consistent with our findings and proves that pregnancy, as a risk factor, increases the possibility of vaginal candidosis. Nyirsey at al. (19) tested 300 women in fertile age in period between 1991 and 1993. The number of positive cultures was 77 (25,6%), which is again consistent with our results. Positive results of microscopic findings of vaginal swab and the number of colonies is also an indicator of colonization or vaginal candidosis. Therefore, numerous studies indicate that pregnancy is indeed a risk factor, and favours the formation of infection and its higher frequency (20). Mycological diagnosis of vaginal candidosis is complex due to the fact that Candida species is an integral part of normal vaginal flora. Microscopic evidence of candida in the vaginal swab and positive cultures on Sabouraud’s agar are not necessarily an indicator of the infection. Therefore, attention should be paid to the number of colonies of candida in culture, as well as their morphological form (blastopores or pseudopyphae and blastopores) in vaginal swab. However, there is controversy as to whether one of these two criteria is indeed a reliable indicator of infection, and is correlated with clinical signs and symptoms (21). During the pregnancy, high levels of reproductive hormones provide a greater amount of glycogen in the vagina, further providing a good source of carbon candida growth. It was demonstrated that estrogens increases the affinity for the vaginal epithelial cell adherence of candida and yeast cytosol receptor or system to connect to reproductive hormones. These hormones also increase the formation of yeast blastopores, as their morphological form (12). Results of our germ tube test show that C. albicans was detected in 40,9% (83/203) sampled individuals from the test group, and 23% (56/244) sampled individuals in the control group. Using cultivation on a selective basis, and identifying colonies based on different colour and consistency, we were able to detect three nonalbicans species: C. glabrata, C. tropicalis and C. krusei. Assimilation test of Candida species (API test) confirmed these findings, and also determined the other non-albicans spp. (C. parapsilosis and C. guilliermondii). Based on these results, we can conclude that the most common non-albicans species, in tested samples, were C. glabrata, 4.2% (4/95) and C. krusei 3,2% (3/95), while most common species in the control samples were C. glabrata 3,2% (2/62) and C. parapsilosis 3,2% (2/95). There are differences in results regarding the representation of C. albicans compared to non-albicans species between the individual studies. In most studies, 80-90% of vaginal isolates were C. albicans. Incidence of candidal vulvovaginitis caused by non-albicans species increased during the last decade (22). In a study done by Polish researchers (23), wich was examined genital candidiasis; C. albicans was detected in 89% of positive cultures. The most commonly detected non-albicans species were C. glabrata and C. tropicalis. These results are very similar to the results that we obtained in our study. Holland at al. (16) showed was slightly lower percentage of C. albicans detected in the positive cultures of vaginal swabs in pregnant women (82% instead of 89%) but the difference has no statistical significance. Our results correlate to results of mentioned studies. Most commonly detected non-albicans species in both experimental groups were C. glabrata (7,5%), C. parapsilosis, C. krusei, and C. tropicalis. Rihter at al. (24) showed in their 2004 study that the C. albicans was the most commonly detected vaginal yeast (70,8%). It should be emphasized that the number of non-albicans species has been growing, according to the recent studies. Results of the last two studies show the increase in the frequency of non-albicans species by up to 20%, as potential causes of vaginal candidosis. Based on previous research, as well as our research, C. glabrata is the most commonly detected non-albicans species. Sobel at al. (20) indicated that a number of risk factors enhance the ability of non-albicans species to cause infections. These include the uncontrolled use antifungal agents, and incomplete and prolonged use antifungal agents in the prevention of candida infections. According to Odds (25) and Horowitz (26), occurrence of VVC attributed to non-albicans species increased from 9,9% in the 1970s, to 20,3% in the 1980s. C. glabrata, C. tropicalis, and C. krusei are listed as the most frequently detected species. It is believed that the occurrence of these species is associated with chronic vaginal candidosis. Research indicates that determination of the candida species is important for determation of the appropriate therapy (27). In our investigations, we looked at the correlation of detected candida species and the microscopic findings. For the test group, the presence of pseudopyphae and blastopores were detected in 94,6% of determined C. albicans. This is in contrast with the control group studies, where only the regular blastopores were found in 97,3% of determined C. albicans. Candidal vulvovaginitis is very rare in postmenopausa! women and girls. This fact highlights hormonal dependence of candidal vulvovaginitis. Increased secretion of sexual hormones in pregnant women favours the formation of infection. During pregnancy, the vagina is more sensitive and the result is a higher frequency of colonization and symptomatic vaginal candidosis (20). The frequency of vaginal candidosis, which is accompanied by clinical manifestations, particularly increases during the last trimester of pregnancy, and repeated infections become more often. High levels of reproductive hormones provide an increased amount of glycogen in the vaginal environment, and subsequently a good source of carbon needed for growth of Candida species and their germination (28). The mechanism is quite complex, and there is an indication that estrogens increases the affinity of vaginal epithelial cells for the adherence of candida, coupling yeast cytosol receptor with a binding system for female reproductive hormones. These hormones also increase the occurrence yeast pseudopyphae (25). In these circumstances there is a balance of candida and other protective bacterial flora in relation to other local defence mechanisms (29).
CONCLUSION
There is a clear correlation between the frequency of positive microscopic findings and positive cultures in vaginal swabs, in both pregnant and non-pregnant women. Greater frequency of positive cultures and microscopic findings was established in pregnant compared to non-pregnant women. The number of colonies and pseudopyphae and blastopores in microscopical findings, were found in the vaginal swabs of pregnant women. It is characteristic for infection. Identification of species showed that the most common isolated candida, of the pregnant and non-pregnant women was Candida albicans. Frequency of detection C. albicans was greater in pregnant, compared to non-pregnant women. The most commonly identified non-alibcans species, in both groups, were C. glabrata, C. parapsilosis, and C. tropicalis. Correlation between C. albicans and microscopic specimens showed that the C. albicans was mostly commensal for the control group, but for the test group mostly caused a vaginal candidosis. Correlation between non-albicans spp. and microscopic specimens showed, non-albicans spp. were mostly caused a vaginal candidosis for the control group, but for the test group, were commensally.
List of Abbreviations
API 20C AUX - Yeast identification kit
VVC - Vulvovaginal candidosis
REFERENCES
- 1.Sobel JD. Candidal vulvovaginitis. Seminars in Dermatology. 1996;15(1):17–28. doi: 10.1016/s1085-5629(96)80014-9. [DOI] [PubMed] [Google Scholar]
- 2.Sobel JD. Genital candidiasis. In: Brodey GP, editor. Candidiasis. 2nd ed. New York: Raven Press; 1992. p. 225. [Google Scholar]
- 3.Kaufman RN, Freidrich EG, Garden HL. Benign diseases of the vulva and vagina. 3rd ed. Chicago: Year Book Medical Publishers; 1989. pp. 361–418. [Google Scholar]
- 4.Sobel JD, Faro S, Force RW, Foxman B, Ledger WJ, Nyersey PR, Reed BD, Summers R. Vulvovaginal candidiasis: Epidemiologic, diagnostic and therapeutic considerations. Am. J. Obstet. Gynecol. 1998;178(2):203–211. doi: 10.1016/s0002-9378(98)80001-x. [DOI] [PubMed] [Google Scholar]
- 5.Odds FC. Candidosis of genitalia. In: Odds FC, editor. Candida and candidosis. 2nd ed. London: Balliere Tindall; 1988. pp. 124–135. [Google Scholar]
- 6.Sobel JD. Epidemiology and pathogenesis of recurrent vulvovaginal candidiasis. Am. J. Obstet. Gynecol. 1985;152:924. doi: 10.1016/s0002-9378(85)80003-x. [DOI] [PubMed] [Google Scholar]
- 7.Numanović F, Hukić M, Nurkić M, Gegić M, Delibegović Z, Imamović A, Pasić S. Importance of isolation and biotypization of Gardnarella vaginalis in diagnosis of bacterial vaginosis. Bosn. J. Basic. Med. Sci. 2008;8(3):270–276. doi: 10.17305/bjbms.2008.2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Babic-Cemalovic M, Ozegovic L, Subasic Đ, Zvizdic A, Seremet M. Morphotypization and genotypization of candida albicans during two attacs of reccurent vaginitis at pregnant woman. Ibernoam. Micologia. 2001:153. [Google Scholar]
- 9.Horowitz BJ, Edelstein SW, Lippman L. Candida tropicalis vulvovginitis, Obstet. Gynecol. 1985;66:229–232. [PubMed] [Google Scholar]
- 10.Goldacre MJ, Watt B, Loudon N, Milne LJ, Loudon JD, Vessey MP. Vaginal microbial flora in normal young women. Br. Med. J. 1979;(1:1450–1455. doi: 10.1136/bmj.1.6176.1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Babic-Cemalovic M, Babić M, Hukić M, Ožegović L, Arapčić S. Examing of yeasts from Candida species on influence of fluconasole. Micologia. 2004:111. [Google Scholar]
- 12.Howard L, Kent MD. Epidemiology of vaginitis. Am. J. Obstet. Gynecol. 1991;165(4):1168–1176. doi: 10.1016/s0002-9378(12)90722-x. [DOI] [PubMed] [Google Scholar]
- 13.Hamad M. Estrogen-dependent induction of persistent vaginal candidosis in naive mice. Mycoses. 2004;47(7):304–306. doi: 10.1111/j.1439-0507.2004.00994.x. [DOI] [PubMed] [Google Scholar]
- 14.Fidel PL, Cutright J, Steel C. Effect of reproductive hormones on experimental vaginal candidiasis. Infection and Immun. 2000;68(2):651–657. doi: 10.1128/iai.68.2.651-657.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newman G, Kaben U. Blastomycoid flora of the urogenital tract in non-pregnant and pregnant patients. Zentralbl. Gynakol. 1975;97(6):372–378. [PubMed] [Google Scholar]
- 16.Holland J, Young ML. Vulvovaginal carriage of yeasts other than Candida albicans. Sex. Transm. Infect. 2003;79:249–250. doi: 10.1136/sti.79.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eckert LO, Hawes SE. Vulvovaginal candidiasis: clinical manifestations, risk factors, management algorithm. Obstet. Gynecol. 1998;92(5):757. doi: 10.1016/s0029-7844(98)00264-6. [DOI] [PubMed] [Google Scholar]
- 18.Enweani IB, Gugnani HC, Okobia R, Ojo SB. Effect of contraceptives on the prevalence of vaginal colonization with Candida species in Endo State, Nigeria. Rev. Iberoam. Micol. 2001;18:171. [PubMed] [Google Scholar]
- 19.Nyirsey P. Chronic focal vaginitis: The value of cultures. Am. J. Obstet. Gynecol. 1995;173(3):820. doi: 10.1016/0002-9378(95)90347-x. [DOI] [PubMed] [Google Scholar]
- 20.Sobel JD, Sabastian F, et al. Vulvovaginal candidiasis: Epidemiologic, diagnostic and therapeutic considerations. Am. J. Obstet. Gynecol. 1998;178(2):203–211. doi: 10.1016/s0002-9378(98)80001-x. [DOI] [PubMed] [Google Scholar]
- 21.Evans EG. Diagnostic laboratory techniques in vaginal candidosis. Br. J. Clin. Pract. Suppl. 1990;71:70–72. [PubMed] [Google Scholar]
- 22.Kent HL. Epidemiology of vaginitis. Am. J. Obstet. Gynecol. 1991;165(4):1168–1176. doi: 10.1016/s0002-9378(12)90722-x. [DOI] [PubMed] [Google Scholar]
- 23.Kwasniewska J, Jaskolowska A, Choczaj-Kukula A. Candidosis of genitalorgans in sexual partners. Mikologia lekarska. 2005;12(4):237–241. [Google Scholar]
- 24.Rihter S, et al. Antifungal susceptibilities of Candida species causing vulvovaginitis and epidemiology of reccurent cases. J. Clin. Microbiol. 2005;43(5):2155–2162. doi: 10.1128/JCM.43.5.2155-2162.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Odds FC. Candida and Candidosis. 2nd ed. London: BaillièTindall; 1988. p. 220. [Google Scholar]
- 26.Horowitz BJ. Mycotic vulvovaginitis. Am. J. Obstet. Gynecol. 1991;165(4):1189–1192. doi: 10.1016/s0002-9378(12)90725-5. [DOI] [PubMed] [Google Scholar]
- 27.Osmanaglaoglu O, et al. Identification of different Candida species isolated in various various hospitals in Ankara by fungichrom test kit and their differentiation by SDS-Page. Turk. J. Med. Sci. 2000;30:355–358. [Google Scholar]
- 28.Evans EG. Diagnostic laboratory techniques in vaginal candidosis. Br. J. Clin. Pract. Suppl. 1990;71:70–72. [PubMed] [Google Scholar]
- 29.Fidel PL. Distinct protective host defenses against oral and vaginal candidiasis. Med. Mycol. 2002;40:359. [PubMed] [Google Scholar]


