Abstract
OBJECTIVES:
The objective of the study was to assess the availability of human and nonhuman resources for emergency medical services (EMSs) at the primary health care (PHC) level.
MATERIALS AND METHODS:
A cross-sectional study with mixed research methods (quantitative and qualitative) was carried out in governmental PHC centers in Dammam, Eastern Province of Saudi Arabia, between September 2014 and January 2015. Using systematic random sampling technique, 13 out of 26 PHC centers were included in the study. The study consisted of two main parts: The first involved the completion of an observational checklist to assess the availability and adequacy of human and nonhuman resources (workforce, emergency infrastructure, equipment, drugs and supporting facilities). The second part involved face-to-face interviews with key informants of nurses from the emergency room (ER) in the sampled centers.
RESULTS:
Analysis of the checklist showed that the total number of physicians “actually” present ranged from 2 to 8 per center and nurses actually present were 4–11 whereas the officially assigned number was 3–12 physicians and 8–17 nurses per center. Only 2 out of 13 (15.4%) centers had a place reserved for EMS in each male and female section. Only 4 (30.8%) PHC centers had a male ER located on the ground floor, near the entrance, and with a separate ramp. None of the centers had the emergency drugs such as metergotamine, calcium chloride, and naloxone. Regarding ER equipment, none of the studied centers had cervical collars, mouth gags, or a tracheostomy sets. Only one (7.6%) center had a functioning fully equipped ambulance. Five (38.46%) centers were equipped with electrocardiogram and X-ray machines. In the interviews, the informants confirmed the deficiencies identified in the checklist.
CONCLUSION:
Resources for EMS at Dammam PHC centers were deficient in infrastructure and supporting facilities.
Keywords: Check list, emergency services, human and nonhuman resources, primary health care center
Introduction
Primary health care (PHC) was defined by the World Health Organization (WHO) in 1978 as essential health care based on practical, scientifically sound, and socially acceptable methods and technology made universally accessible to all individuals in the community.[1] In accordance with the Alma-Ata declaration,[1] the need of PHC development was recognized by health-care authorities in the Kingdom of Saudi Arabia (KSA).[2,3] In KSA, the Ministry of Health (MOH) offers health services at three levels: primary, secondary, and tertiary. PHC centers provide primary care services including promotive, preventive, curative (including emergency services) and rehabilitative services and refer only those cases that require more advanced care to public hospitals, which provide secondary and tertiary levels of care.[4]
Medical emergency is defined as a serious, unexpected, and often dangerous situation requiring immediate action.[5] It is recognized worldwide that the goal of an effective emergency medical system (EMS) is to provide universal emergency care to those in need with rapid assessment, timely provision of appropriate interventions, and rapid transportation to the nearest suitable medical institution by the best means possible to enhance survival, control morbidity, and prevent disability. Consequently, emergency services need to be well planned and supported at all levels: national, provincial, and community.[6,7,8,9,10,11]
However, overutilization of the hospital emergency room (ER) services by nonurgent patients or inappropriate referrals results in a waste of resources, increased pressure on ER staff, and a delay in the care of patients needing urgent attention as reported by many national[12,13,14] and international studies.[8,9,15,16,17,18,19,20,21] Establishment and utilization of emergency services at the PHC level have been recommended by numerous studies as a means of decreasing the load on hospital ER.[8,9,12,13,14,15,16,17,18,19,20,21] The question is whether PHC centers have well-organized emergency services. Much international research[10,22,23,24,25,26,27,28] has consistently reported the lack of preparedness of EMS in PHC centers in terms of available emergency drugs, equipment, and supporting facilities.
In KSA, a huge country with many regions and outlying PHC services, some variation in the organization of care in the numerous PHC centers is expected. Therefore, it is essential to assess the services in each of these PHC centers and ensure that there is uniformity in the quality and standard of service. To the authors' knowledge, only one national study has been published that assessed the preparedness of PHC centers to deal with emergency cases. This study was conducted in 2003 in Asir in all thirty PHC centers of Abha district, both rural and urban, which revealed some deficiencies mainly in infrastructure and support facilities in the emergency services.[14]
Emergency medical services (EMSs) in all PHC centers should be organized well enough to provide optimal care for patients in a safe, appropriate, efficient, and compassionate manner.[7,14,29] To the authors' knowledge, the EMS at the PHC level in Dammam city, Eastern Region of Saudi Arabia, has not been evaluated. The aim of the current study was to assess the preparedness of EMS in PHC centers in Dammam in terms of the suitability of the design of the infrastructure, adequacy of workforce, emergency drugs, equipment, and support facilities.
Materials and Methods
A cross-sectional study using both quantitative and qualitative methods was conducted in MOH PHC centers in Dammam, Eastern Province, KSA.
The study was carried out from September 2014-January 2015. Thirteen out of the 26 PHC centers in Dammam were selected by systematic random sampling as follows; all 26 centers were ordered in a descending manner according to the size of their catchment population. Then, all PHC centers corresponding to the odd order numbers in this list were selected and included in the study for an assessment of their EMS delivery.[30]
Data collection was done using two main tools: the first tool was the completion of an observational checklist to assess the availability and adequacy of human and nonhuman resources. The second involved one-on-one interviews with key informants of ER nurses in the sampled centers.
The observational checklist was developed after reviewing the Saudi MOH quality assurance manual,[29] the Saudi essential drug list at PHC level,[31] and the Saudi Ministry of PHC manual[32] in addition to some aspects of emergency services' requirements for Central Board Accreditation of Healthcare Institutions standards for PHC centers.[7] The list finally comprised of five sections such as A, B, C, D, and E which examined workforce, emergency infrastructure, equipment, drugs, and supporting facilities, respectively.
This checklist was pretested in a pilot study conducted in two PHC centers in Dammam other than those included in the study and one PHC in Al-Qatif (10% of the total calculated study sample), 1 month before the start of data collection. The completeness and applicability of the observational checklist were checked and modifications made accordingly. The finalized observational checklist was completed by the authors after consulting the head nurse responsible for each of the units assessed in the 13 sampled health centers.
PHC ER nurses were invited to participate in one-on-one semi-structured interviews and focus group discussions from 7 out of 13 PHC centers. The interviews conducted were audio recorded with participants' permission and transcribed verbatim; field notes were taken for those who did not want to be recorded. All transcribed interviews were rechecked for accuracy by a research advisor. Translation from Arabic to English was done by the researchers and a reverse translation into Arabic was done by an external assistant.
ER nurses were invited to participate until there was data saturation. A total of 17 nurses from 7 different PHC centers were interviewed; six nurses were included in one-on-one semi-structured interviews, whereas the remaining 11 nurses participated in 3 focus groups comprising 3–5 nurses. An ER nurse was the key informant in all interviews conducted. All participants who refused to be audio recorded, were Saudi, so field notes were taken by the authors instead. Each interview lasted between 30 and 60 min.
Approval was obtained from the Research Committee of the Saudi Board of Family Medicine, the MOH, the medical directors of all participating PHC centers and participating nurses before the start of data collection. The purpose of the study was explained to all participants, who were also given the chance to ask questions on the purpose and conduct of the study and analysis of its results. Participants were also assured of the confidentiality of the collected information and informed that participation was completely voluntary. The participants were asked for their “verbal” informed consent.
All 13 checklists were screened for the completion of information before analysis. All gathered information was kept strictly confidential. Collected data were entered into a personal computer, managed, coded, and analyzed using SPSS (Released 2007, SPSS for Windows, Version 16.0. Chicago, SPSS Inc.) software package; p < 0.05 was considered statistically significant.
For the qualitative data, the authors generated a conceptual framework by which the data were labeled and sorted. This process involved identifying the recurring themes and concepts in the interview transcripts and group discussions. Subsequently, a list of main themes and subthemes was applied systematically to the whole data set.
Results
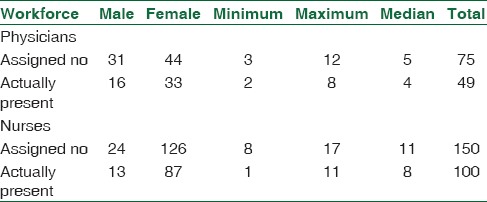
The total number of “officially” assigned physicians per PHC center ranged from 3 to 12 physicians with a median of 5, whereas the “physicians actually present” during the data collection ranged from 2 to 8 physicians per center with a median of 4, and with a female-to-male ratio of 2:1. However, the number of “officially” assigned nurses ranged from 8 to 17 nurses per PHC center with a median of 11, whereas those actually present during the study period were 4–11 with a median of 8, with a female-to-male ratio of 7:1 [Table 1].
Table 1.
Primary health-care center workforce
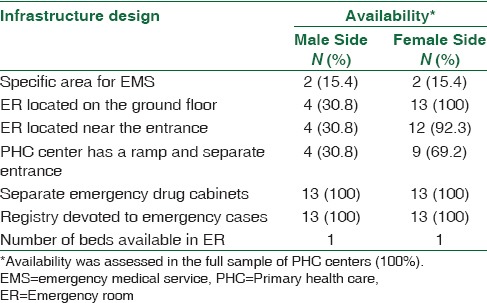
Only 2 out of 13 (15.4%) centers had a place reserved for EMS in every male and female section. Only four (30.8%) PHC centers had a male ER located on the ground floor with a separate ramp, near the entrance. All PHC centers handled emergency cases as a priority in a timely manner. All PHC centers had only one bed in the ER with separate drug cabinets for emergency services [Table 2].
Table 2.
Emergency medical services infrastructure at the studied primary health-care centers (n=13)
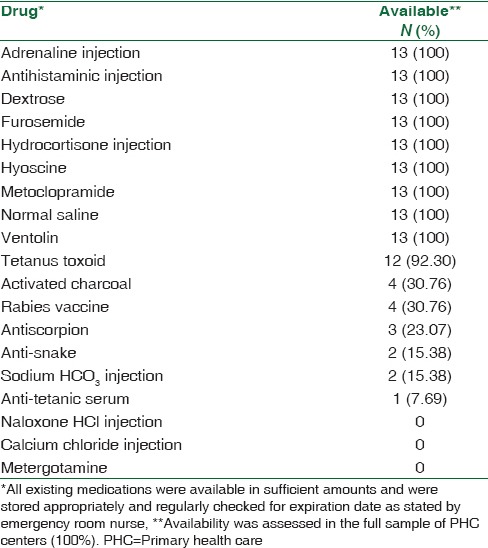
Some emergency drugs (metrogemine, calcium chloride, and naloxone) were not available in any of the PHC centers studied. The medications least available were anti-tetanus serum which was available only in one (7.69%) PHC center, sodium HCO3 and anti-snake in two (15.38%) centers, antiscorpion in three (23.07%) centers, and activated charcoal and rabies vaccine in four (30.76%) centers. In contrast, the following medications were available in all centers: adrenaline injection, antihistamine injection, dextrose, furosemide, hydrocortisone injection, hyoscine, metoclopramide, normal saline, and Ventolin. All existing medications were available in sufficient amounts and as stated by the ER nurse, were stored appropriately and regularly checked for expiration dates [Table 3].
Table 3.
Emergency drugs available at the studied primary health-care centers (n=13)
With regard to emergency equipment, none of the centers had cervical collars, mouth gags, and tracheostomy sets. The emergency equipment least available was the splint, which was found in only one (7.69%) center, urinary catheter in four (30.76%) centers, and nasogastric tubes and oral airways in eight (61.53%) centers. However, the following equipment were available in all centers: ambu bags, cannulas, forceps, intravascular (IV) stand, nebulizer, needle holders, oxygen (O2) cylinders, O2 masks, scissors, suction apparatus, and suture materials [Table 4].
Table 4.
Emergency equipment available at the studied primary health-care centers (n=13)

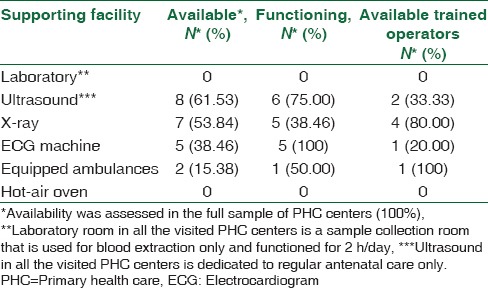
Only two (15.38%) centers had well-equipped ambulances and only one of them was functioning. Five (38.46%) centers had electrocardiogram (ECG) machines; however, only one center had a trained operator. Seven (53.84%) PHC centers had X-ray machines, five (71.42%) of which were functioning and there were four trained operators. Eight (61.53%) centers had functioning ultrasound machines, which were used only for regular follow-up of antenatal care cases. There were no laboratory facilities in any of the centers. Instead, there was a blood collection unit in all centers, operational for only 2 h/day for blood sample collection [Table 5].
Table 5.
Primary health-care center supporting facilities (n=13)
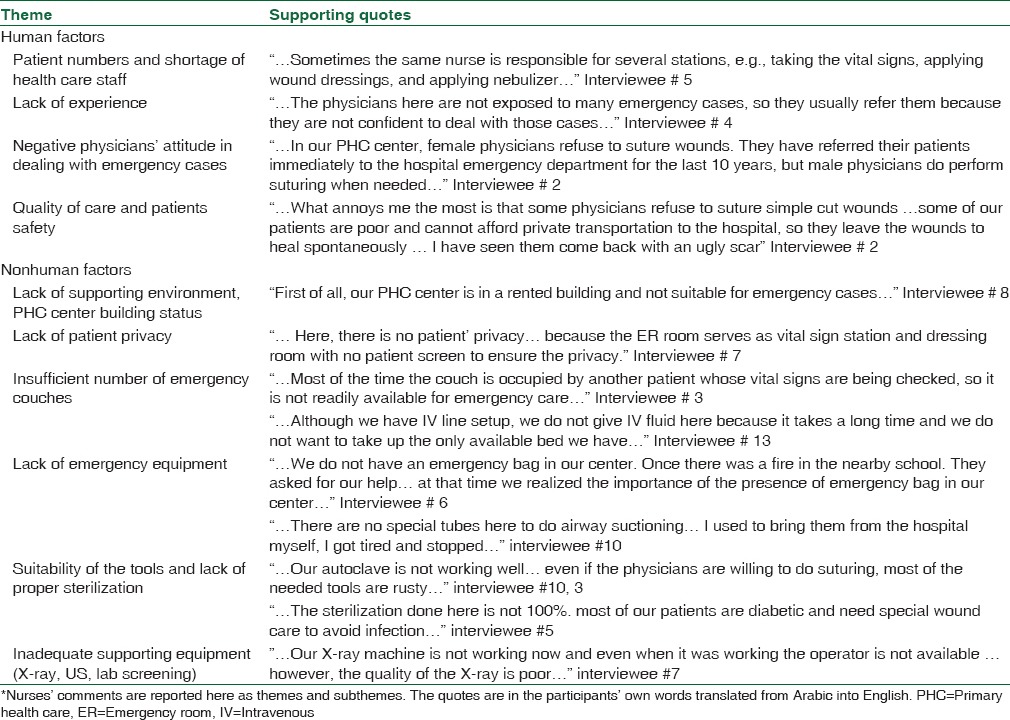
There was no specially assigned nurse to cover the ER. Nurses rotated between different clinics such as vaccination clinic, maternity clinic, acute care clinic, and chronic care clinic. When participants were asked about the emergency services in their PHC centers, some explained the role of emergency services in PHC center thus “…here physicians apply suture material for cut wound patients, use a nebulizer, and order intravenous (IV) fluid for those who need it…” Interviewee # 15. Other interviewees said that they would deal with emergency cases since they believed they were important. “…Emergency service is essential and is required almost every day…” Interviewee # 1. Most participants believed that PHC emergency services were not running well and attributed this to both structural (nonhuman) factors and workforce (human factors) [Table 6].
Table 6.
Opinion of emergency room nurses regarding the status of and factors affecting primary health-care emergency services*
Discussion
The current study revealed that emergency services at PHC centers in Dammam city were not adequately prepared to deal with emergencies.
Our results show that the total number of physicians per PHC center who were actually present during data collection ranged from 2 to 8 physicians with a median of 4, and the number of nurses was 4–11 with a median of 8. Shortage of staff was one of the main issues raised by the interviewees. The large number of patients and the shortage of health-care staff negatively affect the physicians' attitude and the quality of care provided to the patients “…the physicians here see an average of 50–70 patients daily…and cannot spend 30 min to apply sutures to one patient while many patients wait…” Interviewee # 9. This in turn affects the level of patients' satisfaction for the quality of care provided.
Although these workforce figures were less than the actual physician/nurse numbers allocated per PHC center by the Saudi MOH, they are still better than what was found in the Asir study on thirty PHC centers in 2003, which reported much lower physician numbers (ranging from 1 to 6) as well as the number of nurses (ranging from 1 to 10).[14]
WHO studies have shown that countries with fewer than 23 physicians, nurses, and midwives per 10,000 population generally fail to achieve adequate coverage rates for selected PHC interventions.[33] However, worldwide average number of physician is 13.9 per 10,000 population with a range of 0.1 in Tanzania to 60 in Niue island.[34]
Although MOH, KSA published on its electronic webpage in 2011 that 24.4 physicians and 47 nurses were available for every 10,000 population,[35] the numbers revealed in the current study are much lower [Table 1]. Data from health statistics annual book (2012) showed that the ratio of health workforce in MOH centers per 10,000 population was 2.4–3.8 physicians and 4–7 nurses. Moreover, there are 1.9 nurses for every physician employed at PHC centers of the MOH in the KSA, in comparison to 1.3 nurses for every physician in the Eastern Mediterranean region and 1.8 nurses for every physician globally.[36]
With regard to the infrastructure of the sampled PHC centers, this study found that all PHC centers had one couch in the ER and drug cabinets for emergency services. Only 2 out of 13 PHC centers had a place reserved for emergency services for male and female sections. Several interviewees confirmed that their PHC infrastructure was not adequate for emergency care. These findings can be explained by the fact that only four PHC centers were in purpose-built buildings whereas the rest were in rented accommodation with the male sections on the upper floor with no elevators and far from the entrance. There were deficiencies here also as compared locally to the facility reported by study in Abha district (city of Asir) where 28 out of 30 centers were in specially designed buildings and a registry system for emergency services. In addition, EMS was located on the ground floor, close to the entrance, with a ramp. They had separate drug cabinets in 90%, 43.3%, 23.3%, and 76.7% of the centers, respectively.[14]
The findings of the qualitative study further reflect the effect of the building type and the infrastructure on the quality of care provided. The small number of clinics jeopardize patients' privacy as stated by a number of interviewees: “…The ER is not specially designated for emergency cases… we take vital signs for the rest of PHC patients in the same room…” Interviewee # 12.
Formalized in 1948, the Universal Declaration of Human Rights recognizes “the inherent dignity” as part of the human rights, and in accordance with that, the WHO stated that patient privacy and confidentiality of their medical information is a fundamental component of the rights of the patient. The patient is human, and his dignity has to be respected both in sickness and in health. This is even more important in emergencies where it may be crucial to expose patients' bodies to make a proper assessment of their condition.[37]
Regarding emergency drugs, almost all essential drugs were available in all PHC centers. Notably, however, calcium chloride was not available in any of the studied PHC centers. Calcium chloride is used to treat arrhythmias secondary to hypocalcemia, hyperkalemia, or hypermagnesemia, but since there were neither crash carts (ECG machines) nor laboratory facilities to diagnose or follow such cases, its use here was limited. The medications that were least available were anti-tetanus serum, sodium bicarbonate, anti-snake vaccine, antiscorpion vaccine, activated charcoal, and rabies vaccine. The unavailability of these serums and vaccines are due to the present national policy of referring cases requiring the use of these medications to specialized PHC centers. These findings were at variance with the Asir study findings where antiscorpion vaccine and tetanus toxoid were available in all centers for the simple reason that study covered rural parts of Abha district where cases requiring the use of these medications were frequently encountered.[14]
None of the surveyed centers had any of the following emergency equipment: cervical collars, mouth gags, and tracheostomy sets. The least available were splints, urinary catheters, nasogastric tubes, and oral airways. However, most centers had other emergency equipment.
The deficiencies encountered here were in agreement with similar deficiencies reported by other studies. On a national level, a study done by Muneera H. Al-Osimy to assess the extent to which the resources in PHC centers in Riyadh corresponded with specified standards in terms of availability and quality showed that, in two out of three PHC centers, emergency service was one of the clinical areas most underequipped.[38] Other international studies done in south east Queensland, Australia,[22] the USA,[24] and Ottawa, Canada[26] support the previous findings.
The American Academy of Family physicians published an article in 2007 regarding the Medical Emergency Preparedness in Office Practice. It recommended that the choice of emergency medications and equipment should reflect the spectrum of anticipated emergencies in a practice's patient population, the skills of the practitioners, and the distance to the nearest emergency department.[23]
Furthermore, the present study showed substantial deficiencies in PHC support facilities namely, X-ray machines, ECG machines, and well-equipped functioning ambulances which were available in only 53.84%, 38.4%, and 15.3% of our sampled centers, respectively. Although all visited centers had laboratory facilities (sample collection room), they were operational for only 2 h/day. However, there was no laboratory for sample analysis in any of the centers, so the specimens had to be sent to the districts' central laboratory for analysis. This took 3–21 days, depending on the type of the analysis required, for return to the appropriate health centers. These findings were consistent with those of the Asir study, which showed a major deficiency in support facilities. There only 26.6% of the PHC centers had X-ray machines, 53.3% had laboratory facilities, and 23.3% had equipped ambulances.[14] Our key informants also confirmed these findings “…we do not have ECG machines here…” Interviewee # 11
Several national[14,38] and international studies[27,28] on the preparedness of PHC centers in terms of the availability of emergency drugs, equipment, and supporting facilities have reported that PHC centers were ill-prepared to deal with emergencies. One extensive review done through MEDLINE search on American family medicine, pediatric, dental, and dermatological articles published between January 1980 and December 2001, found that family medicine clinics were frequently poorly equipped and inadequately prepared to deal with medical emergencies.[25]
Evaluation of preparedness for medical emergencies has been done in a variety of clinics all over the world. In 2014, 250 dental graduates in India were asked about preparedness of their clinics in terms of emergency drugs and equipment available The responses revealed an alarming inability of dental clinics to deal with such situations.[39] Similar results were found in other studies, in which it was recommended that certain basic emergency medications and equipment should be present in any clinical practice.[39,40,41]
One of the limitations in our study is that the catchment population was used in the sampling technique instead of the number of patient visits per PHC center. However, since the difference between these two figures was not substantial, the ordering of the PHC center would not have significantly changed. The other limitation is that we developed our own (de novo) checklist because we believed that some vital points were not present in the published data.[14] However, we ensured that the checklist fulfilled all requirements of the PHC manual.[32] Future studies should focus on how and when these drugs and equipment can be used and demonstrate the skills and competencies required by team members who deal with emergencies.
Conclusion
It was found that for EMS at Dammam PHC centers, deficiencies were noted mainly in infrastructure and support facilities. There was no equipment specifically for ER that met the national accreditation standards, no emergency medical bags with all essential medications and crash carts, and well-equipped functioning ambulances with trained personnel to accompany patients. Therefore, it is recommended that the ERs should be well equipped and should be able to meet the requirements of accreditation standards. There should be emergency medical bags with all essential medications and crash carts which are checked regularly in all PHC centers.[7]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to express our great thanks to Mr. Ibrahim AlHassan from King Fahad Specialist Hospital and Research Center for the initial sample size calculation and Dr. Moataza Mahmoud Abdel Wahab from the Department of Family and Community Medicine, University of Dammam, for statistical advice during the study.
References
- 1.Mahler H. The meaning of “Health for All by the Year 2000”. World Health Forum. 1981;2:5–22. [Google Scholar]
- 2.Al-Ahmadi H, Roland M. Quality of primary health care in Saudi Arabia: A comprehensive review. Int J Qual Health Care. 2005;17:331–46. doi: 10.1093/intqhc/mzi046. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Country Cooperation Strategy for WHO and Saudi Arabia 2012–2016. Contract No: WHO-EM/PME/003/E. World Health Organization, Regional Office for the Eastern Mediterranean. 2013 [Google Scholar]
- 4.Almalki M, Fitzgerald G, Clark M. Health care system in Saudi Arabia: An overview. East Mediterr Health J. 2011;17:784–93. doi: 10.26719/2011.17.10.784. [DOI] [PubMed] [Google Scholar]
- 5.Simpson J. Oxford Dictionary of English. 3rd ed. United Kingdom: Oxford University Press; 2010. [Last accessed on 2015 Jul 04]. Available from: http://www.dictionary.oed.com/ [Google Scholar]
- 6.Hirshon JM, Risko N, Calvello EJ, Stewart de Ramirez S, Narayan M, Theodosis C, et al. Health systems and services: The role of acute care. Bull World Health Organ. 2013;91:386–8. doi: 10.2471/BLT.12.112664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Institutions CBAH. Primary Healthcare Standards Ministry of Health. 2011 [Google Scholar]
- 8.Indian Public Health Standards (IPHS) For Primary Health Centres: Directorate General of Health Services Ministry of Health & Family Welfare Government of India. Revised 2012. [Last accessed date 2017 Aug 05]. Available from: http://nhm.gov.in/images/pdf/guidelines/iphs/iphsrevised-guidlines-2012/primay-health-centres.pdf .
- 9.David Carson HC, Stern R. Primary Care and Emergency Departments. United kingdom: Primary Care Foundation; 2010. [Google Scholar]
- 10.Klig JE, O'Malley PJ. Pediatric office emergencies. Curr Opin Pediatr. 2007;19:591–6. doi: 10.1097/MOP.0b013e3282efd4cc. [DOI] [PubMed] [Google Scholar]
- 11.Razzak JA, Kellermann AL. Emergency medical care in developing countries: Is it worthwhile? Bull World Health Organ. 2002;80:900–5. [PMC free article] [PubMed] [Google Scholar]
- 12.Rehmani R, Norain A. Trends in emergency department utilization in a hospital in the Eastern region of Saudi Arabia. Saudi Med J. 2007;28:236–40. [PubMed] [Google Scholar]
- 13.Siddiqui S, Ogbeide DO. Utilization of emergency services in a community hospital. Saudi Med J. 2002;23:69–72. [PubMed] [Google Scholar]
- 14.Mahfouz AA, Abdelmoneim I, Khan MY, Daffalla AA, Diab MM, El-Gamal MN, et al. Primary health care emergency services in Abha district of Southwestern Saudi Arabia. East Mediterr Health J. 2007;13:103–12. [PubMed] [Google Scholar]
- 15.Selasawati HG, Naing L, Wan Aasim WA, Winn T, Rusli BN. Inappropriate utilization of emergency department services in Universiti Sains Malaysia hospital. Med J Malaysia. 2004;59:26–33. [PubMed] [Google Scholar]
- 16.Lowy A, Kohler B, Nicholl J. Attendance at accident and emergency departments: Unnecessary or inappropriate? J Public Health Med. 1994;16:134–40. doi: 10.1093/oxfordjournals.pubmed.a042947. [DOI] [PubMed] [Google Scholar]
- 17.Khangura JK, Flodgren G, Perera R, Rowe BH, Shepperd S. Primary care professionals providing non-urgent care in hospital emergency departments. Cochrane Database Syst Rev. 2012;11:CD002097. doi: 10.1002/14651858.CD002097.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Furber AS. Referral to hospital in Nepal: 4 years' experience in one rural district. Trop Doct. 2002;32:75–8. doi: 10.1177/004947550203200205. [DOI] [PubMed] [Google Scholar]
- 19.Carret ML, Fassa AC, Domingues MR. Inappropriate use of emergency services: A systematic review of prevalence and associated factors. Cad Saude Publica. 2009;25:7–28. doi: 10.1590/s0102-311x2009000100002. [DOI] [PubMed] [Google Scholar]
- 20.Bosch X, Escoda O, Nicolás D, Coloma E, Fernández S, Coca A, et al. Primary care referrals of patients with potentially serious diseases to the emergency department or a quick diagnosis unit: A cross-sectional retrospective study. BMC Fam Pract. 2014;15:75. doi: 10.1186/1471-2296-15-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shah NM, Shah MA, Behbehani J. Predictors of non-urgent utilization of hospital emergency services in Kuwait. Soc Sci Med. 1996;42:1313–23. doi: 10.1016/0277-9536(95)00233-2. [DOI] [PubMed] [Google Scholar]
- 22.Johnston CL, Coulthard MG, Schluter PJ, Dick ML. Medical emergencies in general practice in South-East Queensland: Prevalence and practice preparedness. Med J Aust. 2001;175:99–103. doi: 10.5694/j.1326-5377.2001.tb143540.x. [DOI] [PubMed] [Google Scholar]
- 23.Toback SL. Medical emergency preparedness in office practice. Am Fam Physician. 2007;75:1679–84. [PubMed] [Google Scholar]
- 24.Fuchs S, Jaffe DM, Christoffel KK. Pediatric emergencies in office practices: Prevalence and office preparedness. Pediatrics. 1989;83:931–9. [PubMed] [Google Scholar]
- 25.Sempowski IP, Brison RJ. Dealing with office emergencies. Stepwise approach for family physicians. Can Fam Physician. 2002;48:1464–72. [PMC free article] [PubMed] [Google Scholar]
- 26.Liddy C, Dreise H, Gaboury I. Frequency of in-office emergencies in primary care. Can Fam Physician. 2009;55:1004–5.e1. [PMC free article] [PubMed] [Google Scholar]
- 27.Heath BW, Coffey JS, Malone P, Courtney J. Pediatric office emergencies and emergency preparedness in a small rural state. Pediatrics. 2000;106:1391–6. doi: 10.1542/peds.106.6.1391. [DOI] [PubMed] [Google Scholar]
- 28.Paula J, Schweich DC, Anne D. Preparedness of practicing pediatricians to manage emergencies. Am Acad Pediatr. 1991;88:223–9. [PubMed] [Google Scholar]
- 29.Al-Mazrou Y, Farag M. Manual of Quality Assurance in Primary Health Care. 1st ed. Riyadh: General Directorate of Health Centres, Ministry of Health; 1993. [Google Scholar]
- 30.The Annual Report of the Indicators of Patients Services for Primary Health Care Sectors in Eastern Region. Saudi Arabia. 1434 [Google Scholar]
- 31.MOH. Saudi Essential Drug List at Primary Health Care Level. Riyadh: Ministry of Health, Saudi Arabia; 1995. [Google Scholar]
- 32.Al-Mazrou Y, Salem A. Manual of Primary Health Care. Riyadh: General Directorate of Health Centres, Ministry of Health, Saudi Arabia; 2003. [Google Scholar]
- 33.World Health Organization. Human Resources For Health. 2009 May [Google Scholar]
- 34.Physicians (Per 10,000 Population) [Last accessed on 2015 Jul 21]. Available from: http://www.kff.org/global-indicator/physicians/
- 35.Ministry Of Health Portal, KSA. Health Indicators for the Year of 1432 H. 2011. [Last accessed on 2015 Jul 21]. Available from: http://www.moh.gov.sa/en/Ministry/Statistics/Indicator/Pages/Indicator-2013-06-19-001.aspx .
- 36.WHO. WHO World Health Statistics 2013. 2016. [Last accessed on 2016 Dec 07]. Available from: http://www.who.int/gho/publications/world_health_statistics/2013/en/
- 37.Anon. 2016. [Last accessed on 2016 Dec 07]. Available from: http://www.who.int/genomics/public/patientrights/en/
- 38.Ai-Osimy MH. Evaluation of primary health care in Riyadh, Saudi Arabia. J Family Community Med. 1994;1:45–54. [PMC free article] [PubMed] [Google Scholar]
- 39.Kumarswami S, Tiwari A, Parmar M, Shukla M, Bhatt A, Patel M, et al. Evaluation of preparedness for medical emergencies at dental offices: A survey. J Int Soc Prev Community Dent. 2015;5:47–51. doi: 10.4103/2231-0762.151977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dym H. Preparing the dental office for medical emergencies. Dent Clin North Am. 2008;52:605–8, x. doi: 10.1016/j.cden.2008.02.010. [DOI] [PubMed] [Google Scholar]
- 41.Wilson MH, McArdle NS, Fitzpatrick JJ, Stassen LF. Medical emergencies in dental practice. J Ir Dent Assoc. 2009;55:134–43. [PubMed] [Google Scholar]


