Abstract
Background:
Epidermoid cysts, one of the common benign intradermal or subcutaneous tumors commonly result from the trauma to the pilosebaceous unit in the hair bearing area. In areas without hair, these cysts are considered implantation and proliferation of squamous epithelium into the dermis due to injury.
Aims:
The aim is to evaluate the clinicopathological details with emphasis on unusual findings related to epidermoid cysts.
Study Design:
This is a retrospective cross-sectional study carried out over 2 years.
Materials and Methods:
A total of 103 cases of epidermoid cysts were included in the study. The clinical details such as age, gender, sites, and dimensions were noted. The histopathological findings were evaluated and correlated with the clinical findings.
Results:
The highest incidence was observed in the age group of 21–30 years (23.3%, 24/103) and the most common affected region was the head and neck region (32%, 33/103). The size of cysts ranged from 0.3 to 9 cm in diameter with a mean of 2.1 cm. The unusual sites observed in this study were four at the left sole, two at right sole, two at prepuce, and one each at the right finger, left palm, and oral cavity. Histopathological findings included rupture of epidermoid cysts with giant cell reaction, melanin pigmentation, and association with other pathologies such as keloid and lipoma.
Conclusion:
Epidermoid cysts are common benign intradermal or subcutaneous tumors, but they can have unusual presentations and histopathological findings. Epidermoid cysts need early diagnosis and treatment as they can cause cosmetic and functional impairment.
Keywords: Epidermal inclusion cyst, implantation, pilosebaceous unit, squamous epithelium
INTRODUCTION
Epidermoid cysts (epidermal cysts or epidermal inclusion cysts), one of the common benign intradermal or subcutaneous tumors commonly presenting on the scalp, face, neck, trunk, and extremities.[1,2,3,4,5,6] Few cases over male and female external genitalia, palm, sole, fingers, and breast are also reported.[1,2,3,4,5,6] These cysts result from the trauma to the pilosebaceous unit in the hair bearing area.[1,3] In areas without hair such as palm and sole, these cysts are considered to be epidermal inclusion secondary to trauma such as by a sewing needle, crush injuries, or human papillomavirus (HPV) infection, which results in implantation and proliferation of squamous epithelium into the dermis.[1,2,3,4,5,6] These cysts are smooth, dome-shaped, spherical, unilocular swellings varying in size from few millimeters to a few centimeters and usually presents with a punctum.[1] Microscopically, these cysts are lined by an epidermis like epithelium including a granular cell layer containing laminated keratin.[1,2,3,4,5,6]
MATERIALS AND METHODS
This study was a cross-sectional retrospective study done on samples routinely submitted in the Department of Pathology, Informed consent was taken from all the patients before surgery. The present study includes the 103 cases reported by histopathology section of the Department of Pathology from January 1, 2015 to December 15, 2016. The clinicopathological details were taken from the record office for the given period and evaluated with emphasis on unusual finding related to epidermoid cysts. The histopathological examination in these 103 cases was done on formalin-fixed, paraffin-embedded blocks sections stained by Hematoxylin and Eosin stain. Special stains such as periodic acid-Schiff and Ziehl–Neelsen stain were performed wherever required.
RESULTS
In the present study, 103 cases of epidermoid cysts were included. The age of the patients ranged from 2 years to 75 years with the mean age of 33.42 years and the median age of 30.5 years. The highest incidence was observed in the age group of 21–30 years (23.3%, 24/103) followed by age groups of 41–50 (20.4%, 21/103) and 31–40 (16.5%, 17/103) years, respectively [Figure 1]. The head and neck region (32%, 33/103) was the most common affected region followed by lower limb (26.2%, 27/103), back (19.4%, 20/103), and upper limb (9.7%, 10/103), respectively [Figure 2]. In head and neck region 30.3% (10/33) cases were located on the face followed by scalp (21.21%, 7/33). However, in the lower limb, 40.74% (11/27) cases were seen over left afoot followed by right foot (29.63%, 8/27) [Table 1]. The males were more affected than females with an overall male:female ratio of 2:1. The unusual sites observed in this study were breast, prepuce, oral cavity, palm, plantar aspect of foot, and finger [Figure 3]. The size of cysts ranged from 0.3 to 9 cm in diameter with a mean of 2.1 cm. In 11 cases, epidermoid cyst located at the sites, which were considered to be the result of implantation and proliferation of squamous epithelium into the dermis. All 11 cases were male and manual laborers, however, none of them gave a history of any antecedent trauma. The sites of these 11 cases were four at the left sole, two at right sole, two at prepuce, and one each at the right finger, left palm, and oral cavity. Histological examination revealed cysts lined by stratified squamous epithelium with granular layer and filled with laminated keratin materials. Ten cases showed one or more breaches in the cyst wall; considered as a ruptured epidermoid cyst. The site of rupture showed dense chronic inflammatory cells with giant cell reaction. Three cases showed the presence of a dense collection of brown-black melanin pigment both extra and intracellularly in the histiocytes [Figure 4a–e]. One case over the pinna was associated with keloid [Figure 4f] and one case was associated with lipoma.
Figure 1.
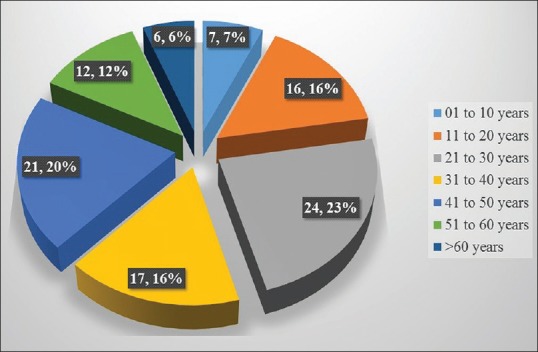
Age wise distribution of epidermoid cyst
Figure 2.
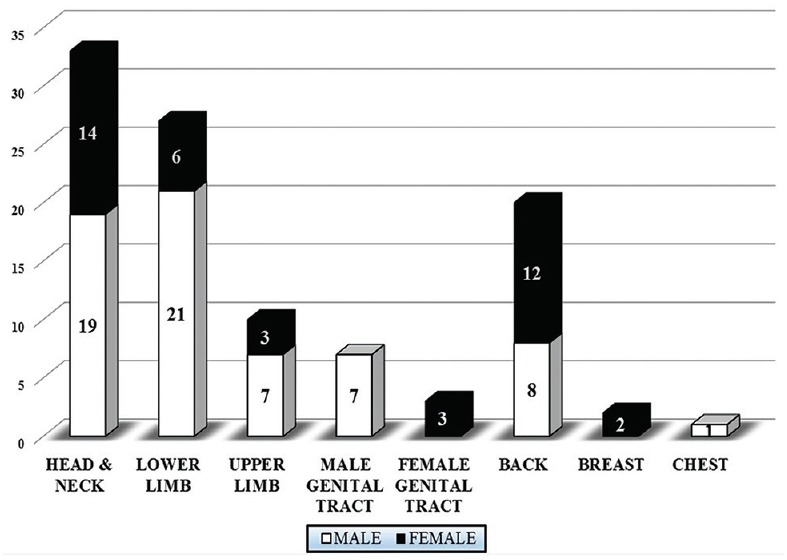
Region wise distribution of epidermoid cyst with male and female numbers
Table 1.
Region- and site-wise distribution of epidermoid cysts
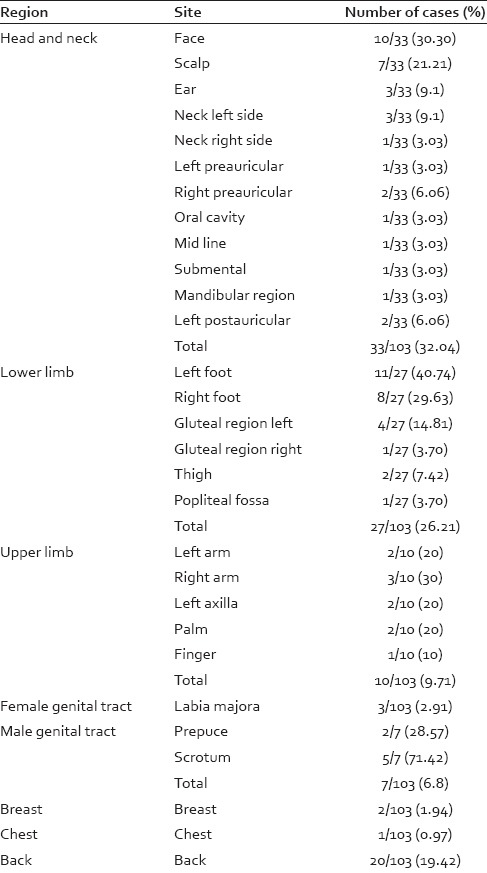
Figure 3.

(a) Vague swelling over the sole of left foot. (b) X-ray showing well-defined oval radiopaque lesion in heel pad region below calcaneum. (c) Vague swelling on the left leg. (d) Cystic swelling over right palm
Figure 4.
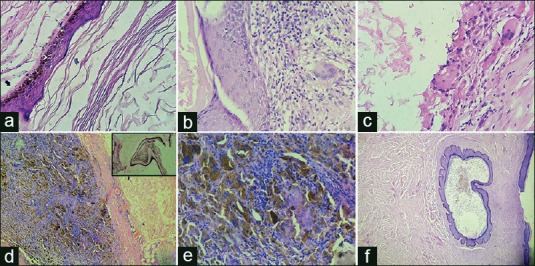
(a) Epidermoid cyst lined by stratified squamous lining having granular layer with laminated keratin material (H and E, ×400). (b) Epidermoid cyst showing giant cell (H and E, ×400). (c) Rupture epidermoid cyst with giant cell reaction (H and E, ×400). (d) Epidermoid cyst with dense melanin pigment containing macrophages (H and E, ×100, inset: Masson–Fontana, ×100). (e) Epidermoid cyst with dense melanin pigment containing macrophages (H and E, ×400). (f) Epidermoid cyst with keloid (H and E, ×100)
DISCUSSION
An epidermoid cyst is a common benign mid/lower dermis or subcutaneous cystic lesion of skin commonly occurring on the scalp, face, neck, trunk, extremities and rarely on male and female external genitalia, palm, sole, fingers, and breast.[1,2,3,4,5,6] In the present study, the head and neck region (32%, 33/103) was the most common affected region followed by lower limb (26.2%, 27/103), back (19.4%, 20/103), and upper limb (9.7%, 10/103), respectively. Usually, epidermoid cysts are solitary, but rarely presence of multiple epidermoid cysts may be the manifestation of Gardner's syndrome, the basal cell nevus syndrome or complication of cyclosporine therapy and imiquimod therapy.[1,7] These cysts are slowly growing, smooth, dome-shaped, firm to the cystic lesion, varying in size from few millimeters to a few centimeters.[1,2] The lesions were single in all the cases of this study except in three cases of scrotal cysts which were multiple and cysts varying in size from 0.3 cm to 9 cm.
These cysts had equal sex predilection and most commonly affect the young and middle-aged adults.[1] In the present study, most common age group affected was of 21–30 years (23.3%, 24/103) followed by age groups of 41–50 (20.4%, 21/103). However, in the present study, males were more affected than females with a male:female of 2:1, which may reflect the reluctance of society to the women to seek medical help in Andaman and Nicobar Islands.
Approximately 7% of all dermoid and epidermoid cysts occur in the head and neck.[7] The cheek is the most common site followed by the neck.[7,8] In the present study, the face was the most common site followed by scalp in the head and neck region. One case showed ruptured cyst with giant cell reaction. Intraoral dermoid and epidermoid cysts are rare, and majority arise in the floor of the mouth which account for <0.01% of all the cysts in the oral cavity. These cysts become symptomatic when they interfere with mastication and speech, or if get secondarily infected otherwise they remain asymptomatic for years.[9] In the present study, one case was observed in the oral cavity of 4.5 years male. One case was observed over pinna in the female which was associated with keloid. No such case has been reported in the literature.
The uncommon sites in the upper and lower limb were palm, finger, and sole as these sites are devoid of hair.[1,4] We had one case each in palm and finger and six cases in the sole. These cysts are considered to be epidermal inclusion secondary to trauma or HPV infection.[4] The characteristic histopathological findings of vacuolated cells and keratohyalin granules are seen in cases with HPV infection.[4] The epidermoid metaplasia of eccrine glands occurs due to HPV infection leading to the development of epidermoid cyst is also suggested by few recent studies.[4] In this study, histological examination did not confirm vacuolated cells, keratohyalin granules, or eccrine glands and therefore tests for HPV virus were not done.
The epidermoid inclusion cysts of the hands are usually slowly enlarging, asymptomatic, superficial localized, painless swellings over the palm, occasionally arising from deeper structures such as tendon and phalangeal bones.[10] In finger, epidermoid cyst commonly arises in the terminal phalanx and present with variable degrees of pain, swelling, and nail deformity.[10] In the present study, both the cases of palm and finger were males. The distal phalanx was affected in the finger. Swellings were small, painless and did not cause any deformity.
The lateral border of the sole is the most common site of the plantar epidermoid cyst.[11] These cysts are thought to occur following traumatic implantation of epidermal cells into the dermis as sole bears mechanical pressure during standing, walking, and running.[11] In the present study, all cases of plantar epidermoid cysts were found in male and ball of the heel was the most common site followed by a lateral border of the sole. No virus-induced changes were seen in the epidermis. Two cases showed rupture with giant cell reaction.
Epidermoid cyst of the breast is a rare benign lesion, which clinically and radiologically mimics benign/malignant breast tumors.[6,12] Less than fifty cases have been reported in the English literature and can occur in both skin layer and breast parenchyma.[6,12,13] Damage to the epidermis, which gets implanted deep within the breast tissue, cystic ectasia of the infundibulum of hair follicles, ectatic duct in fibroadenoma, fibrocystic change or phyllodes tumor undergoes squamous metaplasia of normal columnar cells, or congenital inclusions along the lines of embryonic closure are the possible pathogenic mechanisms of formation of epidermoid cyst in breast parenchyma.[12] The present study had two cases of small epidermoid cysts in the subareolar skin layer of the left breast, and one of them was ruptured with giant cell reaction. No other breast lesion was found clinically.
Epidermoid cyst also occurs over external genitalia of both male and female.[1,2,3,5] Vulvar epidermoid cysts are frequently localized on the clitoral region, labia majora, and very rarely labia minora, and are frequently multicystic, slowly growing and may reach a size of 5 cm in diameter when their growth process stops.[3] These cysts are also thought to be as a result of implantation of superficial epidermal tissue into the dermis or subcutaneous tissue following trauma, episiotomy or as a secondary effect of female circumcision.[3] In the present study, two cases of vulvar epidermoid cyst were reported, one case had undergone for an episiotomy during normal labor, and other case had no history of trauma or any surgical intervention.
The penile epidermoid cysts are very rare, however, epidermoid cyst is still most common among all penile cysts, and are usually found on the penile shaft.[5,14] Congenital penile epidermoid cysts occur due to the abnormal embryologic closure of the median raphe.[5] In adults, as the penis is a nonhair bearing area, implantation mechanism following trauma or surgery is thought to be the cause of epidermoid cysts development.[5] In the present study, two cases of epidermoid cyst were reported on prepucial skin. Epidermoid cysts are common in the scrotum, and are single or multiple.[14] The present study had three cases of multiple scrotal epidermoid cysts.
One case reported in the popliteal fossa, an uncommon site for epidermoid cyst was also reported in this study.
The infected and ruptured epidermoid cyst results in heavy inflammatory cell infiltrate in the adjacent dermis. However, when an uninfected epidermal cyst ruptures, the cyst's content are released into the dermis causing foreign body reaction with numerous multinucleated giant cells forming keratin granuloma.[15] In the present study, ten cases showed ulceration, rupture, and foreign body giant cell reaction with typical keratin granuloma in the deep dermis. Sometimes, the ruptured cyst leads to accumulation of the extensive large amount of melanin pigment with the proliferation of melanophages.[15] We had three cases which showed an unusual finding of a dense collection of melanin pigment in the macrophages and giant cells.
CONCLUSION
Epidermoid cysts are relatively the common benign intradermal or subcutaneous tumors presenting anywhere over the body including hair free sites. In this study, male predominance may be due to the reluctance of society to the women to seek medical help for this simple lesion. The head and neck, lower limb and back were the leading affected sites. The unusual site such as oral cavity, breast, palm, finger, external genitalia, and confusing clinical presentation may enhance the chance of diagnostic dilemma manifold. Considering that these cysts have a relatively high risk of recurrence, the thorough histopathological examination is required. Epidermoid cysts need early diagnosis and treatment as they can cause cosmetic and functional impairment. The variations in sites, clinical presentations and histopathological findings in the present study have added both to the diagnostic and clinical knowledge known so far.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Calonje E, Brenn T, Lazar A, McKee PH. McKee's Pathology of the Skin with Clinical Correlations. 4th ed. China: Elsevier Saunders; 2012. pp. 1571–4. [Google Scholar]
- 2.Kirkham N. Tumors and cysts of the epidermis. In: Elder DE, Elenitsas R, Johnson BL, Murphy GF, Xu X, editors. Lever's Histopathology of the Skin. 10th ed. China: Lippincott Williams and Wilkins; 2009. pp. 800–2. [Google Scholar]
- 3.Pehlivan M, Özbay PÖ, Temur M, Yilmaz Ö, Gümüs Z, Güzel A. Epidermal cyst in an unusual site: A case report. Int J Surg Case Rep. 2015;8C:114–6. doi: 10.1016/j.ijscr.2015.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gomi M, Naito K, Obayashi O. A large epidermoid cyst developing in the palm: A case report. Int J Surg Case Rep. 2013;4:773–7. doi: 10.1016/j.ijscr.2013.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumaraguru V, Prabhu R, Kannan NS. Penile epidermal cyst: A case report. J Clin Diagn Res. 2016;10:PD05–6. doi: 10.7860/JCDR/2016/18246.7794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh M, Maheshwari B, Khurana N, Jain S. Epidermal inclusion cyst in breast: Is it so rare? J Cytol. 2012;29:169–72. doi: 10.4103/0970-9371.101165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Khateeb TH, Al-Masri NM, Al-Zoubi F. Cutaneous cysts of the head and neck. J Oral Maxillofac Surg. 2009;67:52–7. doi: 10.1016/j.joms.2007.05.023. [DOI] [PubMed] [Google Scholar]
- 8.Golden BA, Zide MF. Cutaneous cysts of the head and neck. J Oral Maxillofac Surg. 2005;63:1613–9. doi: 10.1016/j.joms.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 9.Kini YK, Kharkar VR, Rudagi BM, Kalburge JV. An unusual occurrence of epidermoid cyst in the buccal mucosa: A case report with review of literature. J Maxillofac Oral Surg. 2013;12:90–3. doi: 10.1007/s12663-011-0188-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saraf S. Implantation dermoid of the palm: An unusual presentation. Indian Dermatol Online J. 2012;3:37–9. doi: 10.4103/2229-5178.93499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee KM, Park JH, Min KH, Kim EK. Epidermal cyst on the sole. Arch Plast Surg. 2013;40:475–6. doi: 10.5999/aps.2013.40.4.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chandanwale SS, Buch AC, Kumar H, Mishra N. Epidermoid cyst in the breast: A common benign lesion at a rare site. Clin Cancer Investig J. 2015;4:99–101. [Google Scholar]
- 13.Whang IY, Lee J, Kim JS, Kim KT, Shin OR. Ruptured epidermal inclusion cysts in the subareolar area: Sonographic findings in two cases. Korean J Radiol. 2007;8:356–9. doi: 10.3348/kjr.2007.8.4.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ro JY, Kim KR, Shen SS, Amin MB, Ayala AG. Tumors and tumor-like conditions of the male genital tract. Part C: Penis and scrotum. In: Fletcher CD, editor. Diagnostic Histopathology of Tumours. 4th ed. China: Saunders, an Imprint of Elsevier Inc; 2013. p. 1012. [Google Scholar]
- 15.Jayalakshmy PS, Subitha K, Priya PV, Johnson G. Pigmented epidermal cyst with dense collection of melanin: A rare entity – Report of a case with review of the literature. Indian Dermatol Online J. 2012;3:131–4. doi: 10.4103/2229-5178.96714. [DOI] [PMC free article] [PubMed] [Google Scholar]


