Abstract
Male-pattern hair loss (MPHL) is a condition that affects the majority of men during adulthood. This condition is not life threatening but needs constant treatment and monitoring, especially in recent years where male appearance is gaining significant importance in society. An ideal classification with high amount of detail, practicality, and reproducibility is required to accurately diagnose and monitor this condition regularly and to assess the outcome of treatment. Numerous classifications have been invented, but many variants with different levels of detail, practicality, and reproducibility may cause confusion among clinicians. One clinician may not accurately able to convey accurate clinical description if different classifications are used. To avoid confusion, a new classification that can balance detail, practicality, and reproducibility is required. We hope that this will translate to better treatment and monitoring for patients. This review article aims to review different existing MPHL classifications and how it compares to each other in terms of detail, practicality, and reproducibility.
Keywords: Androgenic alopecia, classification, male-pattern hair loss, patterned hair loss
INTRODUCTION
Male-pattern hair loss (MPHL) is an exceedingly common problem to the majority of males that may occur as early as puberty and increases with age.[1,2,3,4,5,6] MPHL has a significant psychosocial effect and has been perceived as older and less attractive.[7] To better treat and monitor this condition, an accurate and practical classification with high degree of reproducibility is necessary. Various Classifications for Male Pattern Hair Loss has been proposed with various complexity. However, despite the numerous available classifications, none are perfect with its own limitations. In this article, we will review various classification systems for MPHL focusing on its detail, practicality, and reproducibility.
MALE-PATTERN HAIR LOSS CLASSIFICATION
Hamilton
Hamilton studied more than 700 individuals of various sex, ethnicities, and ages to create the first MPHL classification. In his publication, individuals involved includes fetuses to the elderly. This was done to ensure that all scalp types are thoroughly studied, and accurate classification can be determined from unaffected scalp to severely affected scalp. The Hamilton classification is divided into two major categories: scalp which are “not bald” and “bald.” The less severe “not bald” includes type I–III whereas the “bald” includes type IV–VIII. All types are described in Figure 1.[1]
Figure 1.
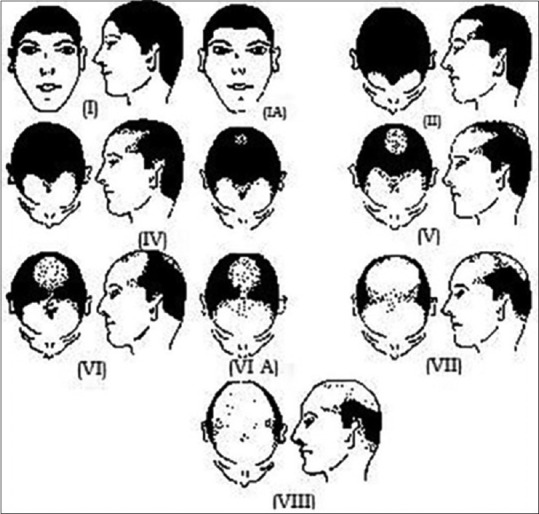
Hamilton classification of male-pattern hair loss. Type III has not been included in this figure due to its rarity and inclusion of hair loss that are difficult to classify
Type I: No bilateral recessions along the anterior border of the hairline in the frontoparietal region. For those whose entire anterior hairline lies high on forehead, they are included in the variant form of this type known as type IA
Type II: This type of Hamilton classification includes triangular areas of recession on the frontoparietal region but does not extend further than the point 3 cm anterior to a line drawn in a coronal plane between the external auditory meatuses (midcoronal line). The hair on the mid-frontal border of the scalp may have some loss but much less affected than in the frontoparietal regions
Type III: This type represents borderline cases and hair loss that are difficult to classify due to scars, asymmetry, unusual types of sparseness and thinning of the hair and other factors. This type is rare and thus not shown in the image [Figure 1]
Type IV: This type represents the minimum amount of hair loss considered sufficient to represent baldness. There are deep triangular frontotemporal recessions that extend further posteriorly than the point which lies 3 cm anterior to the midcoronal line. Moreover, just like type II, most patients will experience hair loss on the mid-frontal part of the scalp. If hair loss occurs as a broad band along the entire anterior border of the hairline, it is classified as type IVA. In older individuals, additional hair loss can also occur on the crown. This type is called type IV old
Type V: This type involves worse of frontoparietal recessions compared to type IV with hair loss also occurring on the crown area
Type VI: In type VI, the recession on frontoparietal region resembles a horseshoe when seen from above with a small island of hair on the mid-frontal area. There is also hair loss on the crown similar to type V, but this area remains separated from the frontoparietal recession. In the variant type, type VIA, the island of hair on the mid-frontal area is sparse or lost
Type VII and VIII: Both of these types represent the worst types of hair loss according to Hamilton. In these types, the recession on the frontoparietal region also resembles a horseshoe but there is no separation with the hair loss on the crown area. The difference between type VII and VIII lies on the presence of hair clump of at least 100 coarse terminal hairs in the horseshoe-shaped scalp area. There is also larger bare area on the scalp compared to the previous types.
With eight different stages and subtypes of various severity, the author considers that this classification is able to provide accurate diagnosis of MPHL and assessment of its severity. This classification is also practical, as demonstrated by Hamilton in his studies when 4 untrained individuals are able to make diagnosis and classify MPHL with only 2% variance compared to Hamilton himself. Hamilton also demonstrated its reproducibility by himself producing the same result in 199 out of 200 patients 3 months apart between examinations.
However, Hamilton classification is not without its drawback. One of the Hamilton's types of MPHL, type III was described as borderline cases or cases which are difficult to assess. This type basically serves as a basket criteria for other type of scalp that did not fit the other types. This classification is thus unable to accurately observe stages of hair loss.
Norwood-Hamilton
In 1975, Dr. Norwood after studying 1000 Caucasian Male male individuals used Hamilton classification as a guide then modified the classification to create the Norwood-Hamilton classification that conform better to the observed stage of hair loss. Currently, Norwood-Hamilton classification is the most widely used hair loss classification.[8,9]
The Norwood-Hamilton classification simplified Hamilton classification by reducing the amount of types from eight to seven with five subdivisions. Type I is similar to Hamilton's classification with none or minimal recession along the anterior border of the frontotemporal region. Type II–V differs from Hamilton's classification by each having “type A” variants for presentation variability. He also removed the basket criteria of type III that may cause confusion to clinicians while added considerable detail in the pictures.
The types II–V of the Norwood-Hamilton classification are described as such [Figure 2][10]:
Figure 2.
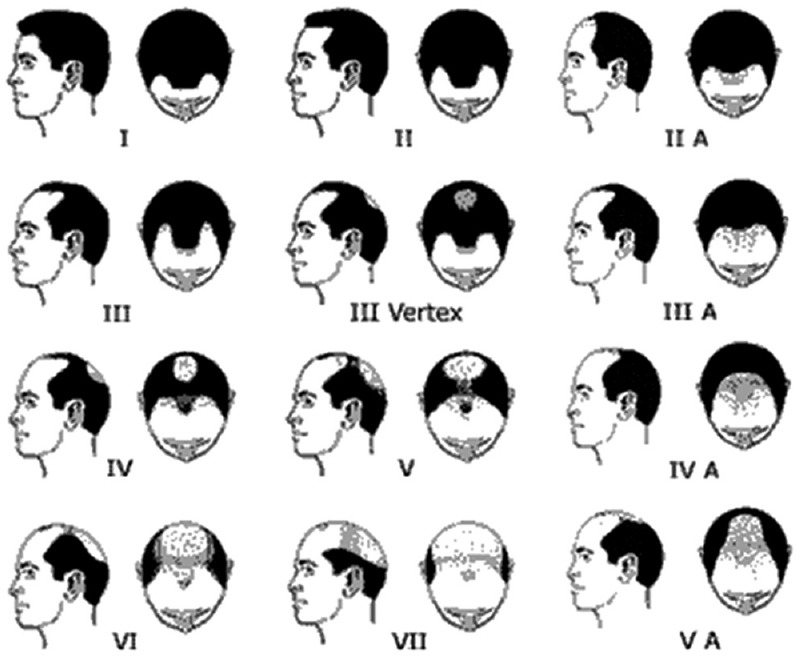
Norwood-Hamilton classification
Type II: The frontotemporal recession of hairline does not extend further than 2 cm anterior to the midcoronal line
Type III: The frontotemporal recession of hairline extends further than type II and may reach the midcoronal line
Type IV: The frontotemporal recession of hairline has receded beyond the midcoronal line
Type V: The area of denudation includes the vertex. Hair loss more severe than type VA cannot be distinguished from types VI or VII.[10]
The function of “type A” variants are to compliment type II–V previously described due to presentation variability attributed to these types. According to Norwood, the type A variant constituted approximately 3% of all individual studies. The type A variant must have 2 major features, with 2 other minor features being optional. The major features are: (1) the frontotemporal recession of the hairline progresses to the rear without leaving an island of hair in the mid-frontal region and (2) frontotemporal recession of the hair line is not accompanied by simultaneous development of a bald area on the vertex but instead the frontal hairline recession keeps progressing to the rear of the scalp. The minor features are: (1) persistent sparse hair scattering in the area of hair loss and (2) the horseshoe-shaped hair that remains on the side and back of the scalp tends to be wider and reaches higher on the head.
The presence of 12 different categories including its “type A” variants added more detail and refinement to the Hamilton classification. This level of detail in the classification, especially with replacement of basket type III by Hamilton, will clear up the confusion that may arise among clinicians.
However, the Norwood-Hamilton criteria also have its drawbacks. The level of detail may be hard to remember due to the amount of details involved. Its reproducibility has also proved unsatisfactory in trials such as the ones conducted by Hong et al. and Guarrera et al.[9,11] Both these trials studied intergroup agreement among clinicians and found that all results were deemed unsatisfactory. To improve its reproducibility, Guarrera suggested that the number of the types should be drastically cut from 12 to 4, but this will severely reduce the amount of details presented.
Adapted Norwood-Hamilton
The adapted Norwood-Hamilton is a further improvement of the most widely used Norwood-Hamilton classification. As mentioned before, the Norwood-Hamilton classification is abundant in details and it is widely used but lacking reproducibility. Khumalo and Gumedze attempted to improve the reproducibility of the Norwood-Hamilton classification without sacrificing detail that has been an important part of this classification.
Compared to the original Norwood-Hamilton, Khumalo and Gumedze stages hair loss into type I–VII. To make this classification more practical, additional designations to the classifications were replaced by either anterior (A) or vertex (V) on stages III–V to indicate the main site of hair loss. The type IIA that was present in the original Norwood-Hamilton was removed for simplification. Types VI and VII also do not have additional classification designation as the hair loss on these types involves both anterior (A) and vertex (V) [Figure 3][8].
Figure 3.
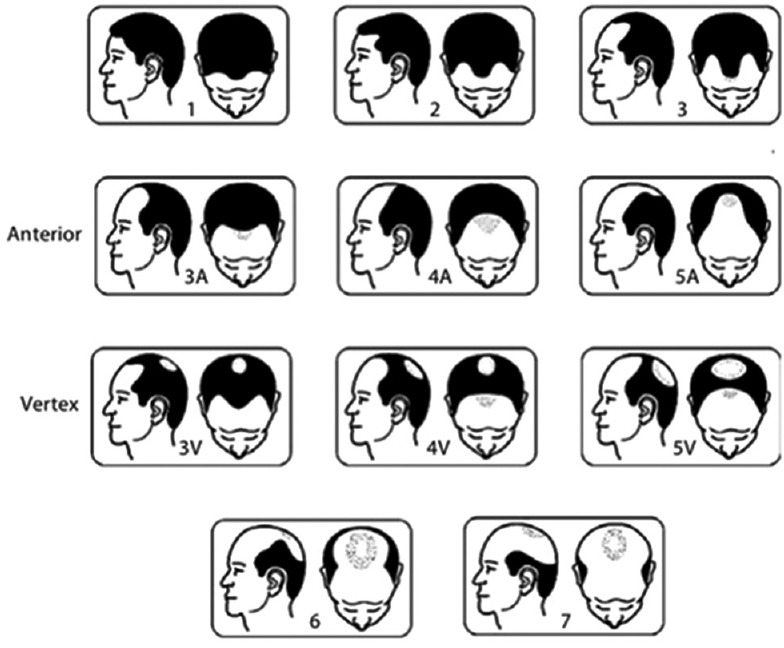
Adapted Norwood-Hamilton classification
With these modifications, Khumalo and Gumedze hoped to improve practicality and reproducibility of the original Norwood-Hamilton. To measure the improvement, they did a small study involving 12 observers (both clinicians and nonclinicians) evaluating 16 men with MPHL using the original Norwood-Hamilton, followed by the adapted Norwood-Hamilton. The result showed statistically significant improvement in interobserver agreement compared to the original Norwood Hamilton.
Basic and specific
Basic and Specific (BASP) classification is the newest classification developed by Lee et al. in 2007. This classification was developed to create a balance between detail, practicality, and reproducibility. This classification is divided into 2, “basic” and “specific.”
The basic types define the shape of anterior hairline using the letters L, M, C, and U that correspond to how the hairline looks when viewed from above, except for the letter L that stands for linear. Clinical history is of great importance in the basic type as it is determined by patient's subjective recognition of their own original anterior hairline. The breakdown of basic types and its subtypes is shown in Figure 4.[5]
Figure 4.
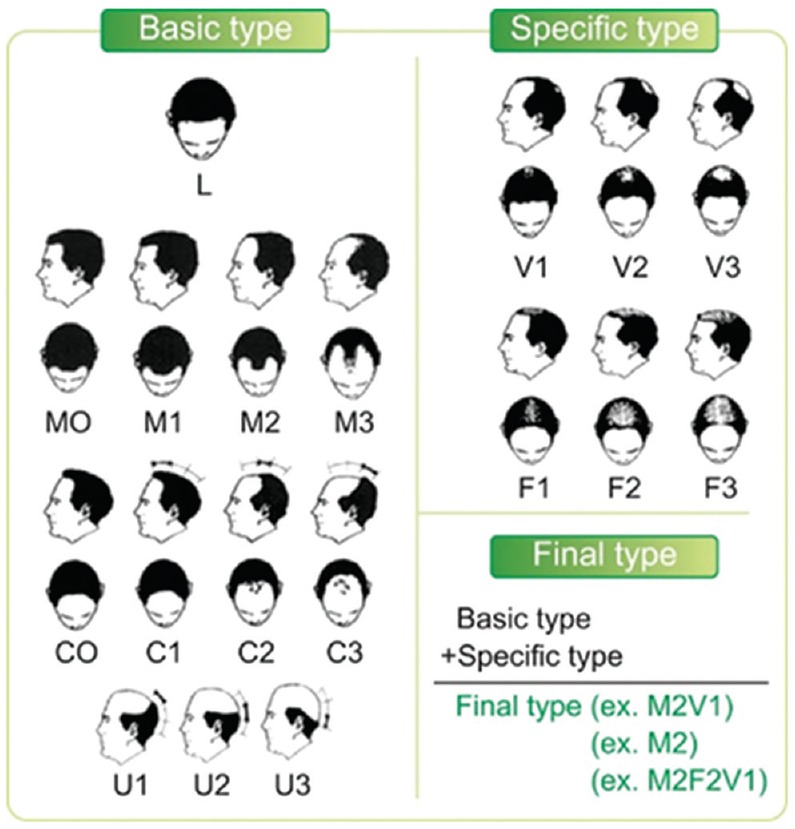
Basic and specific classification
Type L: No recession observed along the anterior border in the frontotemporal region. The hairline appears linear, and there is usually no hair loss
Type M: Recession present on the anterior hairline resembling the letter M. This type is further divided into four subtypes depending on the severity
Type M0: The original hairline resembles the letter M, and no hair loss is visible
Type M1: The anterior hairline has receded posteriorly but does not exceed beyond the anterior third of a virtual line connecting the original hairline and the top of the vertex
Type M2: The anterior hairline has receded posteriorly but does not exceed beyond the middle third of a virtual line connecting the original hairline and the top of the vertex
Type M3: The anterior hairline has receded posteriorly beyond the middle third section reaching posterior third of a virtual line connecting the original hairline and the top of the vertex
Type C: Recession is present on the anterior hairline resembling the letter C. The entire anterior hairline recession is in the shape of half-circle, resembling the letter C. It is further divided into four subtypes depending on the severity
Type C0: The original hairline resembles the letter C, and no hair loss is visible
Type C1: The anterior hairline has receded to the anterior one-third of the virtual line connecting the original hairline and the top of the vertex
Type C2: The anterior hairline has receded to the middle one-third of the virtual line connecting the original hairline and the top of the vertex
Type C3: The anterior hairline has receded into the posterior one-third of the virtual line original hairline and the top of the vertex
Type U: This type represents anterior hairline that has receded posterior of the vertex forming a horseshoe shape resembling the letter U. This type represents the most severe type of hair loss. It is further divided into three subtypes depending on the severity of baldness. There is no U0 in this type as no original hairline without hair loss recedes posterior of the vertex
Type U1: Anterior hairline has receded into the superior one-third of the virtual line connecting vertex and the posterior occipital protuberance
Type U2: Anterior hairline has receded into the middle one-third of the virtual line connecting the vertex and the posterior occipital protuberance
Type U3: Anterior hairline has receded into the inferior one-third of the virtual line connecting the vertex and the posterior occipital protuberance.
The specific types represent general thinning of the scalp. These types are divided based on location, whether it is frontal (F) or vertex (V) and further divided into three subtypes each, with similar levels of severity. The following is the breakdown of the specific types and its subtypes.
Type F/V1: The general decrease of hair density is only perceptible
Type F/V2: The general decrease of hair density is more pronounced
Type F/V3: The general decrease of hair density is severe; there is only very sparse or even absence of hair.
The final type is decided by a combination of the basic and specific type and its subtypes. For example, basic type (C1) + specific type (V1) denotes final type C1V1. By using combination of letters that resembles the shape of anterior hairline and location of reduced hair density, a clinician can easily imagine the clinical picture better than the previous classifications. This classification is also not exclusive to MPHL but can also be used in female-pattern hair loss. Moreover, this system is easy to learn, memorize, practice and has better reproducibility than the previous classifications in routine clinical practice.[5,8,9,12]
However, BASP has several disadvantages. The first one is severe specific F types, for example, F2 and F3 may cause confusion with the more severe V types as the area represented overlaps each other, causing accurate reading difficult. The second disadvantage of BASP classification is the stark change compared to the current most commonly used classification Norwood-Hamilton. This makes adaptation of this classification slow in clinical practices.
DISCUSSION
Throughout the years, many studies have attempted to create an ideal MPHL classification. There are three important variables in an MPHL classification. The three important variables are detail, practicality, and reproducibility. In our search for the most ideal MPHL classification, the ideal classification must have a high level of detail yet easy to use, memorize, and reproducible at different times by different clinicians.
Detail is the first important variable in our assessment of the available classifications. A detailed classification must be able to determine the correct diagnosis, pattern, and severity of MPHL which will then best represent the actual condition of the patient. This will be determined by the number of evolutionary patterns in a classification, the more the better. In our assessment of the different classifications, BASP is the most detailed classification, due to the presence of 12 categories encompassing different patterns of PHL and 6 density parameters. This, in turn, will translate to the more appropriate treatment whether it is topical, oral, or surgical [Table 1].
Table 1.
Comparison of different classifications according to detail, practicality, and reproducibility
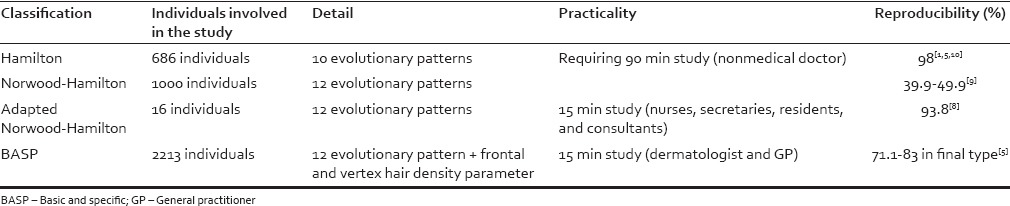
Practicality is the second important variable. An ideally practical classification should be easy to learn, use, and remember even by nonexperienced clinicians. We seek to review this by looking at the amount of time needed to learn, use, and remember the classification or if the classification can be learnt by nonmedical personnel. In this case, we find that the most practical classification is the Norwood-Hamilton classification due to its familiarity with most studies worldwide.[9] Although the levels of detail are high and may be hard to remember, the familiarity of this classification makes up for its practicality.
The third important variable is reproducibility. This is defined by how the classifications are able to reproduce consistent result despite being done at different times by different clinicians. The scores are compared, and higher percentage of identical results indicate better reproducibility. The Hamilton classification has showed the highest reproducibility, achieving identical result in 199 out of 200 individuals in his study.[1] BASP and adapted Norwood-Hamilton also showed great promise in reproducibility rates, achieving 83% and 93.8%, respectively.[5,8,13] Unfortunately, despite being the most commonly used classification, Norwood-Hamilton classification does not have nearly as high reproducibility.[8,9]
Unfortunately, no MPHL classification is able to fulfill all these criteria perfectly. Each classification has its own strengths and weakness. Hamilton, the first classification for MPHL, is highly reproducible, but unfortunately, the presence of basket criteria hurts its ability to present high level of actual clinical details of patients. Norwood-Hamilton, which was developed to improve Hamilton's details, suffers in reproducibility. Adapted Norwood-Hamilton aims to improve reproducibility, but unfortunately, the number of individuals in the study is too small with only 16 individuals and need to be replicated. To date, this is the only study that can be found in PubMed. BASP has a fairly high level of detail and reproducibility but its completely new concept is unfamiliar and adaptation has been slow. As of 2017, there are only few studies regarding hair loss that used BASP classification as its benchmark. The search for an ideal MPHL classification is still ongoing.
CONCLUSION
Various MPHL classifications have been available but every single one of them suffered from critical defect, either it is the details, practicality, or reproducibility. To date, no classification is perfectly balanced on the three variables. New classification may be needed for better monitoring and treatment planning.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Hamilton JB. Patterned loss of hair in man; types and incidence. Ann N Y Acad Sci. 1951;53:708–28. doi: 10.1111/j.1749-6632.1951.tb31971.x. [DOI] [PubMed] [Google Scholar]
- 2.Koo SH, Chung HS, Yoon ES, Park SH. A new classification of male pattern baldness and a clinical study of the anterior hairline. Aesthetic Plast Surg. 2000;24:46–51. doi: 10.1007/s002669910009. [DOI] [PubMed] [Google Scholar]
- 3.Varothai S, Bergfeld WF. Androgenetic alopecia: An evidence-based treatment update. Am J Clin Dermatol. 2014;15:217–30. doi: 10.1007/s40257-014-0077-5. [DOI] [PubMed] [Google Scholar]
- 4.Tsuboi R, Itami S, Inui S, Ueki R, Katsuoka K, Kurata S, et al. Guidelines for the management of androgenetic alopecia (2010) J Dermatol. 2012;39:113–20. doi: 10.1111/j.1346-8138.2011.01361.x. [DOI] [PubMed] [Google Scholar]
- 5.Lee WS, Ro BI, Hong SP, Bak H, Sim WY, Kim DW, et al. A new classification of pattern hair loss that is universal for men and women: Basic and specific (BASP) classification. J Am Acad Dermatol. 2007;57:37–46. doi: 10.1016/j.jaad.2006.12.029. [DOI] [PubMed] [Google Scholar]
- 6.Lee WS, Lee HJ, Choi GS, Cheong WK, Chow SK, Gabriel MT, et al. Guidelines for management of androgenetic alopecia based on BASP classification – The Asian Consensus Committee guideline. J Eur Acad Dermatol Venereol. 2013;27:1026–34. doi: 10.1111/jdv.12034. [DOI] [PubMed] [Google Scholar]
- 7.Lee HJ, Ha SJ, Kim D, Kim HO, Kim JW. Perception of men with androgenetic alopecia by women and nonbalding men in Korea: How the nonbald regard the bald. Int J Dermatol. 2002;41:867–9. doi: 10.1046/j.1365-4362.2002.01446.x. [DOI] [PubMed] [Google Scholar]
- 8.Khumalo NP, Gumedze F. The adapted classification of male pattern hair loss improves reliability. Dermatology. 2012;225:110–4. doi: 10.1159/000341542. [DOI] [PubMed] [Google Scholar]
- 9.Hong H, Ji JH, Lee Y, Kang H, Choi GS, Lee WS. Reliability of the pattern hair loss classifications: A comparison of the basic and specific and norwood-hamilton classifications. J Dermatol. 2013;40:102–6. doi: 10.1111/1346-8138.12024. [DOI] [PubMed] [Google Scholar]
- 10.Norwood OT. Male pattern baldness: Classification and incidence. South Med J. 1975;68:1359–65. doi: 10.1097/00007611-197511000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Guarrera M, Cardo P, Arrigo P, Rebora A. Reliability of hamilton-norwood classification. Int J Trichology. 2009;1:120–2. doi: 10.4103/0974-7753.58554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agarwal S, Godse K, Mahajan A, Patil S, Nadkarni N. Application of the basic and specific classification on patterned hair loss in Indians. Int J Trichology. 2013;5:126–31. doi: 10.4103/0974-7753.125606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meng-Long RA, Jian-You C, Yang P, Liang-Nong GU, Shan W, Shu-Xia Y. BASP. Concordance of basic and specific (BASP) classification in Chinese androgenetic alopecia patients. J Clin Dermatol. 2014;43:67–9. [Google Scholar]


