Abstract
Oral focal mucinosis (OFM) is a rare connective tissue disorder characterized by myxoid degeneration of submucosal connective tissue. It usually presents as gingival or mucosal overgrowth. Due to its uncommon occurrence and lack of pathognomonic clinical or radiological features, diagnosis mainly relies on histopathological evaluation. The paper reports a rare case of large OFM in a 58-year-old female patient involving the posterior maxilla and hard palate. Diagnosis of the lesion was established based on histopathological and immunohistochemical analysis. The lesion was excised surgically and showed no recurrence at 1 year follow-up. The cases presented intend to bring OFM to the attention of oral pathologists and clinicians while considering the differential diagnosis of myxoid lesions of oral cavity.
Keywords: Connective tissue disorder, gingival growth, mucosal lesion, myxoid degeneration
INTRODUCTION
Oral focal mucinosis (OFM) is a rare pathology, believed to be an oral counterpart of cutaneous focal mucinosis.[1] Pathogenesis of OFM is due to overproduction of hyaluronic acid by fibroblasts underlying the oral mucosa resulting in myxoid degeneration of the connective tissue. Hyaluronic acid is a glycosaminoglycan distributed widely throughout connective, epithelial and neural tissues. It is an important component of articular cartilage and plays role of lubricant in muscular connective tissue. It is also a major component of skin and plays role in cell proliferation and wound repair. Increase in its level is correlated well with certain malignancy and is often used as a tumor marker for prostate and breast cancer.
OFM primarily affects the mucosa overlying the jaw bone and usually presents as asymptomatic small pedunculated or sessile gingival overgrowth. Due to its rarity, it may be misdiagnosed as other common mucosal growths such as gingival hyperplasia, epulis or fibroma. Lack of any pathognomonic clinical feature means, histopathological evaluation is paramount in final diagnosis of these lesions.
A review of English literature reveals 57 cases of OFM reported since the first case described by Tomich in 1974.[2] Although these lesions commonly involve gingival or palatal mucosa, large lesion involving the posterior maxilla and hard palate has been rarely reported. This paper presents a rare case of large OFM of maxilla in an old female patient.
CASE REPORT
A 58-year-old female patient reported to the department of oral and maxillofacial surgery with a chief complaint of painless swelling over roof of mouth. The patient first noticed the swelling 6 months back and had gradually increased to its present size. Past medical and dental history was noncontributory. The patient was otherwise systemically healthy and gave no previous history of trauma or long-term drug therapy. On examination, swelling localized over left posterior maxilla was noticed. The mucosal swelling occupied space distal to the second premolar to third molar, measuring about 4.5 cm. The lesion extended medially presenting as submucosal swelling over the left side of palate [Figure 1]. The overlying mucosa appeared normal with small areas of inflammation at few places. The molar teeth were displaced, mobile and appeared partially submerged in the mucosa. Left maxillary second molar was grossly decayed. The swelling was nontender and firm on palpation. A digital orthopantomogram was advised which showed resorption of the left posterior maxillary alveolus with floating maxillary molars [Figure 2]. Based on the presentation, differential diagnosis included peripheral giant cell lesion, peripheral ossifying fibroma, pyogenic granuloma, traumatic fibroma and focal gingival hyperplasia. Incision biopsy of the lesion was carried under local anesthesia, and the specimen was submitted for histopathological evaluation. Hematoxylin and eosin stain (H and E) sections of the specimen showed hyperplastic stratified squamous epithelium with underlying dermis composed of stellate cells in abundant myxoid stroma. Nuclear atypia, mitosis or necrosis was not seen [Figure 3]. The above features were suggestive of benign myxoid lesion, like OFM. Alcian blue staining of myxoid stroma showed strong staining suggestive of of hyaluronic acid [Figure 4]. Based on these histological findings, a definitive diagnosis of OFM was made.
Figure 1.

Clinical presentation of the lesion
Figure 2.
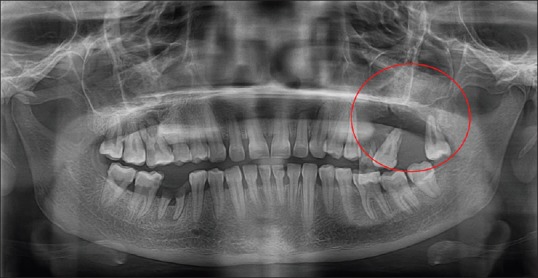
Orthopantomogram showing floating appearance of left maxillary molars and resorbtion of crestal bone. No intraosseous lesion is noted
Figure 3.
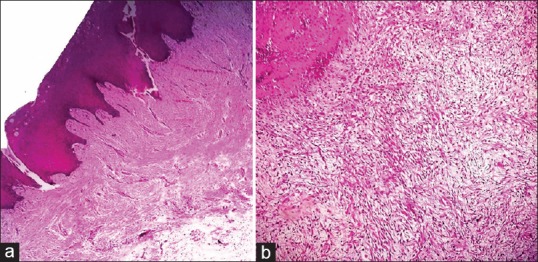
(a) area of myxiod degeneration underlying stratified squamous epithelium (H&E, ×4), (b) underlying connective tissue showing multiple fusiform plump fibroblasts (H&E, ×10)
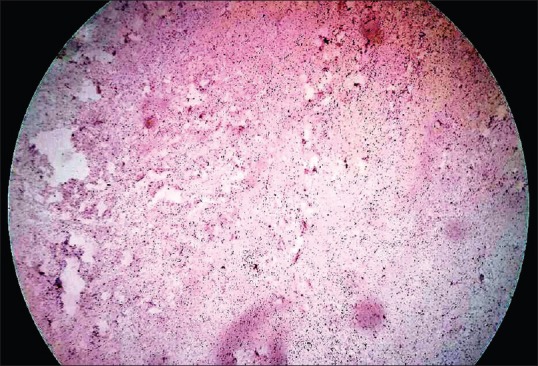
Figure 4.
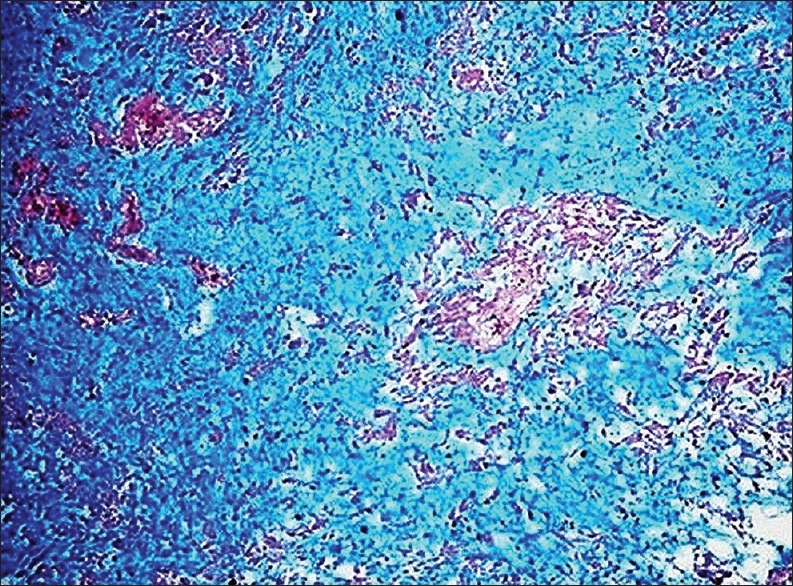
Alcian blue staining of the mxyoid background
Excision of the pathology was planned and executed under local anesthesia. After complete removal of the lesion, buccal mucoperiosteal flap was advanced palatally and primary closure was attained [Figure 5]. The excised specimen was subjected to histological examination. H and E stained slide from the lesion showed loose and myxomatous connective tissue stroma with scarce inflammatory cells underlying the epithelial lining. Deeper stroma showed multiple fusiform and stellate-shaped fibroblasts interspersed between thin collagen fiber bundles distributed in the myxomatous background [Figure 6]. The microscopic finding was consistent with OFM. There was no evidence of granulomatous pathology, dysplasia or malignancy is the examined specimen. Immunohistochemical (IHC) analysis was advised to rule out the possibility of myxoid neuroma. IHC analysis for S-100 protein showed that the lesion was negative for this marker in the mucinous area ruling out other myxomatous lesions of neural origin [Figure 7].
Figure 5.
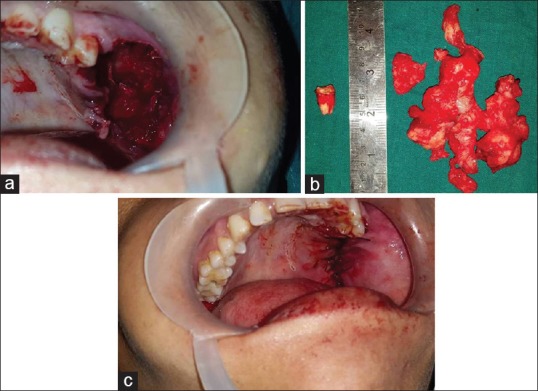
Surgical removal of the lesion; site after surgical excision, (a) excised specimen, (b) primary closure (c)
Figure 6.
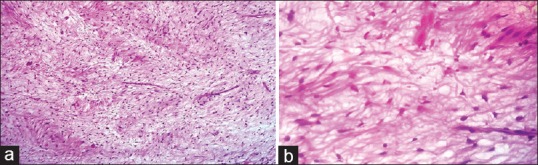
(a) underlying connective tissue stroma was composed of loose fibromyxoid stroma with stellate-shaped fibroblasts (H&E, ×10), (b) multiple fusiform plump and stellate shaped fibroblasts interspersed between thin collagen fiber bundles distributed in the myxomatous background (H&E, ×40)
Figure 7.
Immunohistochemistry for S100 showing negativity in the myxoid area
The postoperative healing was uneventful. At 1 year follow-up, there was no recurrence and healing of the surgical site was satisfactory. A removable partial denture was fabricated for prosthetic rehabilitation of the missing teeth [Figure 8].
Figure 8.

Postoperative photographs; (a) showing the surgical site, (b) dental prosthesis to replace the lost teeth and (c) orthopantomogram at 1 year follow-up
DISCUSSION
OFM is a rare clinicopathological entity which is considered to be the oral counterpart of cutaneous focal mucinosis.[2] Histologically these lesions are characterized by the presence of myxomatous degeneration of connective tissue stroma, mostly of keratinized mucosa overlying the alveolar bone. The myxomatous degeneration is believed to be due to overproduction of hyaluronic acid by the fibroblasts in the connective tissue, at the cost of collagen production.
A review of the English literature by Vipin in 2012 revealed 57 cases of OFM, reported since the first case described by Tomich in 1974. Only three of them were reported in Indian literature.[3] OFM has predilection for involvement of mucosa overlying jaw bone, with 80% of the case seen on gingival. Rest of the lesions has been reported over palate, alveolar mucosa, buccal mucosa and lip in order of decreasing preference.[4] OFM manifest as localized sessile or pedunculated mucosal overgrowth, usually varying in few millimeters to 2 cm in size. They clinically mimic pyogenic granuloma, peripheral giant cell granuloma, peripheral ossifying fibroma, traumatic fibroma or focal gingival hyperplasia. In the present case, the lesion was particularly large, involving almost entire left posterior maxilla and hard palate. Resorption of alveolar bone with displacement of molars was also seen, which made an accurate clinical diagnosis difficult.
Due to its rare occurrence, lack of pathognomonic clinical feature and resemblance to any localized gingival or mucosal overgrowth, OFM is often difficult to diagnose clinically. Histopathological examination plays a key role in accurate identification of the lesion. Microscopic features of OFM described in the literature include area of myxoid tissue in the connective tissue stroma underlying the stratified squamous epithelium of oral mucosa. The myxoid tissue consist of an area of loose connective tissue formed by an accumulation of hyaluronic acid and widely spaced collagen fibers interspersed with stellate-shaped fibroblasts, with or without inflammation.[5] As similar features may be appreciated in odontogenic myxoma (OM) and nerve sheath myxoma, these lesions should be included in histological differential diagnosis of OFM.[6] OM is a true neoplasm of mesenchymal origin. It mainly consists of spindle-shaped cells and scattered collagen fibers distributed through a loose, mucoid material. Unlike OFM which presents as localized gingival enlargement, OM invariably presents as intraosseous expansile lesion causing slow growing enlargement of jaw bone. OFM specimens are Alcian blue-positive, showing strong and diffuse positivity, which confirms the abundant mucin dispersed throughout the connective tissue. The lesion is negative for Periodic acid–Schiff staining. OFM should also be differentiated from myxoid neural lesions. Immunohistochemical analysis using S-100 marker is important in establishing the diagnosis, which stains positive for myxoid neuroma. In the present case, negativity for S-100 was observed in the mucinous area, which confirmed diagnosis of OFM.
Management of OFM includes surgical excision. Recurrence is rare. Simple surgical removal with the primary closer of defect by buccal advancement flap was done. The healing was satisfactory with no recurrence at 1 year follow-up.
CONCLUSION
OFM is a rare pathology which is often difficult to diagnose clinically due to its common presentation as localized mucosal enlargement, usually over gingival. Histopathological evaluation plays a critical role to arrive at definitive diagnosis. This paper reports a case of OFM which was relatively large, involving entire left posterior maxilla. The lesion also caused tooth displacement and resorption of alveolar bone which is unusual for the lesion. Although cases of OFM of this size are rare, it should be considered in the differential diagnosis of localized growth of oral mucosa, especially when located in the gingiva. Detailed Microscopic study is always the basis of final diagnosis is such situations.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Buchner A, Merrell PW, Leider AS, Hansen LS. Oral focal mucinosis. Int J Oral Maxillofac Surg. 1990;19:337–40. doi: 10.1016/s0901-5027(05)80076-1. [DOI] [PubMed] [Google Scholar]
- 2.Tomich CE. Oral focal mucinosis. A clinicopathologic and histochemical study of eight cases. Oral Surg Oral Med Oral Pathol. 1974;38:714–24. doi: 10.1016/0030-4220(74)90392-2. [DOI] [PubMed] [Google Scholar]
- 3.Saito I, Ide F, Enomoto T, Kudo I. Oral focal mucinosis. J Oral Maxillofac Surg. 1985;43:372–4. doi: 10.1016/0278-2391(85)90259-9. [DOI] [PubMed] [Google Scholar]
- 4.Bharti V, Singh J. Oral focal mucinosis of palatal mucosa: A rare case report. Contemp Clin Dent. 2012;3(Suppl 2):S214–8. doi: 10.4103/0976-237X.101098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Silva K, Monteiro B, Norões T, Godoy G, Miguel M. Large oral focal mucinosis: A case report. J Bras Patol Med Laboratorial. 2014;50:54–6. [Google Scholar]
- 6.Etges A. Oral focal mucinosis: Clinical, histopathological and histochemical study. Rev Pos Graduacao. 2007;7:140–4. [Google Scholar]


