Abstract
Background:
The extraction of third molars is associated with some clinical outcomes and periodontal problems. It is imperative to note that the type of incision used in the surgery for the removal of the impacted third molar is critical. The design of the flap influences the healing of the surgically created defect and damage to the distal periodontal area of the adjacent second molar. However, till date, there have been conflicting reports on the influence of different flap designs used for the surgical removal of impacted third molars.
Aim:
The present study aimed to comparatively evaluate the clinical outcomes and periodontal status of the adjacent second molar, when two different flap designs, namely, the envelope and the modified triangular flap designs were used.
Materials and Methods:
Sixty female patients with bilateral impacted third molars completed the study with envelope flap on one side and modified triangular flap design on the other side of the mandible for third molar removal. Clinical parameters including pain, dehiscence and swelling were assessed postoperatively and periodontal probing depth (PPD) on the distal aspect of adjacent second molar were assessed both pre- and post-operatively.
Results:
The results were assessed on 1, 3 and 8 days for pain using visual analog scale. The subjective perception of swelling was evaluated on 3, 7 and 15 days postoperatively in a similar manner. The results of the periodontal parameters were evaluated both preoperatively and 3 months postoperatively, with cautious exploration using a University of North Carolina (UNC)-15 periodontal probe. The statistically significant results for swelling and PPD were noted for the two flap groups using the Chi-square test (P < 0.05).
Conclusion:
The study revealed that the modified triangular flap had lesser postoperative PPDs and dehiscence. The envelope flap was better when swelling was analyzed. The pain scores, though slightly higher for the modified triangular flap group, were not statistically significant.
Keywords: Envelope flap, flap design, impacted teeth, modified triangular flap, periodontal healing, third molar surgery
INTRODUCTION
Impaction of third molars is a common condition, often related with different degrees of difficulty in their surgical extractions. It is well known that impacted third molars have been associated with pericoronitis, dental caries on the distal surface of second molar or the third molar, dental crowding and different types of cysts or odontogenic tumors.[1]
Surgical extraction of impacted third molar is usually associated with postoperative complications. It is well understood that this involves the manipulation of hard and soft tissues for mucoperiosteal flap reflection and subsequent bone removal during the surgery. The postoperative complications that may ensue following the removal of the impacted third molar include pain, swelling, reduced masticatory ability and trismus. It is noteworthy that these complications are more common in the mandible than in the maxilla.[2] However, the severity of such complications may differ in different patients and may not necessarily be presented by all patients. A sound understanding of the surgical principles for the removal of the impacted third molars is therefore imperative for the effective patient management.
From the existing literature, it is obvious that the type of incision is an important consideration in the surgical removal of the impacted teeth.[3] Further, it is vital to note that the design of the flap is a critical parameter in the surgery of the third molars. The design of the flap influences the visibility and accessibility to the impacted tooth and also has an impact on the subsequent healing process of the surgical defect created following the surgery. As it is in proximity to the second molar, the untoward damage to the distal aspect of the same with resultant loss of periodontal attachment and increased probing depth following the healing of the surgical wound can be an annoying factor.[4] Over a period of years, various standards have been established and employed, particularly considering the flap design, instrumentation, amount of bone removal, sectioning methods and suturing.[5]
Various flap designs have been advocated since many years and practiced for the removal of the impacted third molar.[6,7,8] The envelope flap with the distal relieving incision and the triangular flap with the vestibular extension are widely used efficiently for the removal of impacted third molars.[9] However, the documented evidence on the influence of flap designs on postoperative complications and the conclusive absolute preference of the type of flap to be used are limited.[10] Further, from the existing literature, regarding the technique employed, it is evident that there are conflicting data on the effect of surgical removal of the impacted third molar with varying outcomes on the periodontal health of the adjacent second molar.
Therefore, the present prospective study aimed to assess the effect of two different flap designs, namely, the envelope flap technique and the modified triangular flap technique on clinical outcomes including pain, swelling and periodontal probing pocket depth at the distal aspect of the second molar, following the removal of impacted inferior third molars.
MATERIALS AND METHODS
The present clinical trial was conducted at the College of Dentistry, King Khalid University, Abha, Kingdom of Saudi Arabia. A total of female seventy patients, aged between 18 and 40 years, who presented with bilateral third molar impacted teeth were enrolled in the study. However, only sixty patients who completed the follow-up were included in the study. For the purpose of diagnosis and effective treatment planning, routine records were obtained from all the patients including panoramic and intraoral periapical radiographs.
The inclusion criteria were (1) patients with bilateral impacted inferior third molars that were of comparable clinical presentation and technical difficulty (Pell and Gregory), positioning and angulations as seen on periapical and panoramic radiographs, (2) patients who did not have any significant medical contributory history, with no pathologic findings or systemic conditions which might have an effect bone growth or on periodontal healing, (3) patients who were not on any medication that would influence the surgical procedure or postoperative course of healing, (4) nonsmokers and patients with healthy dental status. The exclusion criteria were (1) pregnancy during the extraction, (2) periodontal surgery at the time interval between the extraction and the examination, (3) patients with chronic periodontal disease.
Based on the inclusion criteria, seventy female patients aged between 18 and 40 years were enrolled in the study, of which sixty patients complied till a follow-up period of 3 months. The demographic data were recorded, a thorough history was taken and informed written consent was obtained from the patients. The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethical Committee, King Khalid University, KSA. The patients were assessed clinically and radiographic analysis was performed for all the patients to determine the difficult index. To be specific, patients with mesioangular impacted inferior third molar categorized as C1 class were selected.[11] Patients did not undergo any scaling procedure before the surgery. Periodontal health of adjacent second molar was evaluated before and after the surgery using the UNC-15 periodontal probe.
In patients with bilaterally impacted third molars, random selection of the quadrant for performing envelope technique on one side of the jaw and triangular flap on the other side was done. After the surgery was completed, no subgingival scaling or root planing on the second molar was performed. In a single appointment, one flap technique was performed and after about a month, another technique was performed on the contralateral side. The surgery was performed under local anesthesia using lignocaine in a 4% solution with 1:100,000 epinephrine.
Both the techniques were performed by the same surgeon in all the patients. In patients presenting with bilaterally impacted inferior third molars, the envelope flap was randomly allotted to one side of the arch and the modified triangular flap to the other contralateral side.
Surgical flap techniques
Envelope flap
An incision was made beginning medial to the external oblique ridge and was extended up to the middle of the distal line angle of the second molar.[12] Further, a sulcular incision was made from the distofacial line angle of the second molar to the mesiofacial line angle of the first molar [Figure 1].
Figure 1.
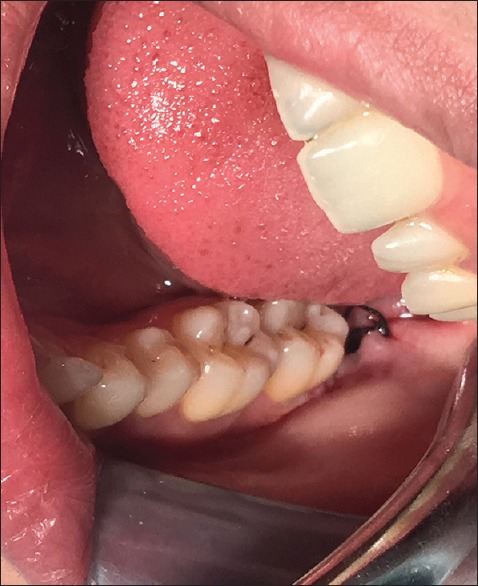
Envelope flap technique
Modified triangular flap
This flap design as described by Szmyd is similar in the first part of the incision to the envelope flap design. However, it differs from the original incision design as described by Szmyd[13] in that, a vertical incision was continued from the distofacial line angle of the second molar apically, extending to the mucogingival line about 2–3 mm. Therefore, the second molar is involved only up to the distofacial edge, thereby restricting more involvement of the periodontal tissues [Figure 2].
Figure 2.
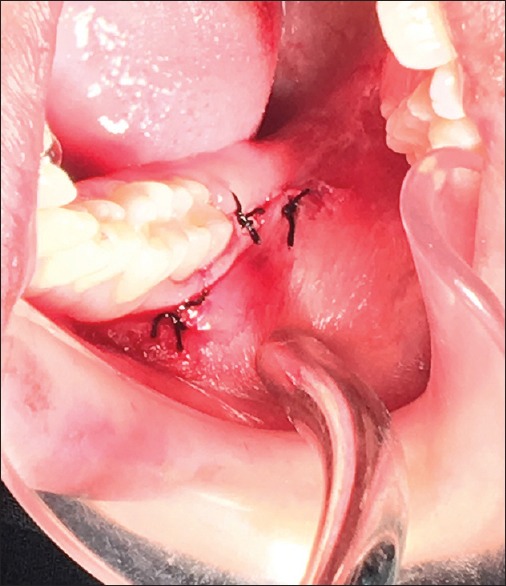
Modified triangular flap technique
Following the placement of incisions in both the techniques, the mucoperiosteal flap was reflected and the impacted molar was exposed. Further, ostectomy was performed and if required, odontosection was done aiding in the removal of the impacted molar. After the extraction and cavity treatment with saline solution, atraumatic sutures were used for suturing, facilitating primary wound healing (Ethicon silk 4-0; Johnson and Johnson, Sao Paulo, Brazil). Two or three single-button sutures were used to approximate the envelope flap distal to the second molar, followed by interdental sutures between the first and second molars. For the triangular flap, the suturing distally was similar to that of the envelope flap, with a coronally placed suture on the perpendicular incision. Following the surgery, all the patients were placed on similar antibiotic and analgesic regime and recalled after 7 days for suture removal.
Postoperative follow-up
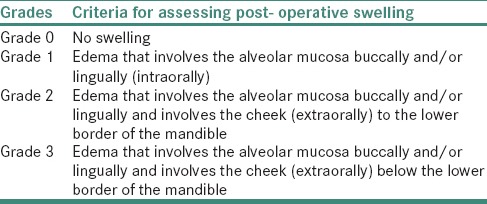
The patients were followed up on 1, 3 and 8 days for pain using visual analog scale [Table 1].[14] Similarly, the swelling scores were evaluated on 3, 7 and 15 days postoperatively subjectively [Table 2].[15] The periodontal probing pocket depths were evaluated both preoperatively and 3 months postoperatively, using a UNC-15 periodontal probe. Every gaping along the line of incision was considered to define dehiscence.
Table 1.
Visual analog scale for assessment of pain
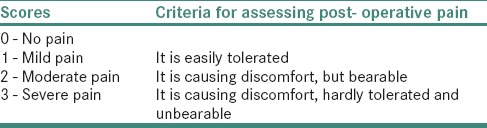
Table 2.
Assessment of swelling
RESULTS
The statistical analysis was performed using the Chi-square test, in which it was considered as statistically significant if P < 0.05.
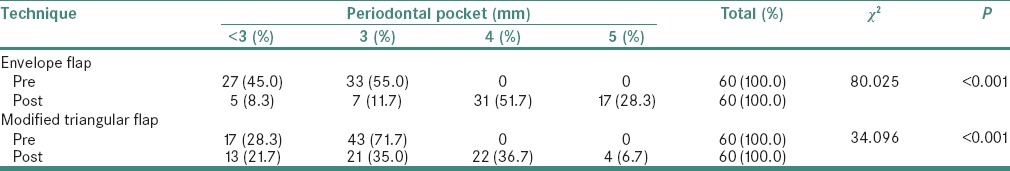
In the modified triangular flap group, when swelling scores were analyzed on the 3rd day postoperatively, 6.7% patients (4 patients) showed Grade 3 scores, while 48.3% showed Grade 1 involvement (29 patients) and 45% (27 patients) showed Grade 2 involvement. From statistical point of view, this was considered statistically significant with a P = 0.011 when compared with the envelope flap group, where no patients showed Grade 3 involvement, 71.7% (43 patients) showed Grade 1 and 28.3% (17 patients) showed Grade 2 involvement [Table 3 and Graph 1].
Table 3.
Comparison of post- operative swelling scores between the envelope and modified triangular flap
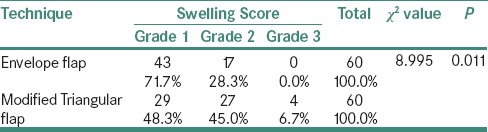
Graph 1.
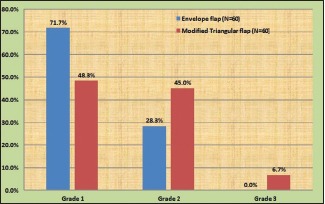
Distribution of swelling score between two treatment groups
When dehiscence was evaluated, it was observed that, in patients treated with envelope flap, 30% (18 patients) and 10% (6 patients) in the modified triangular flap group, showed the presence of dehiscence, with a P = 0.006, which was statistically significant [Table 4 and Graph 2].
Table 4.
Comparison of occurence of post- operative dehiscence between the envelope and modified triangular flap
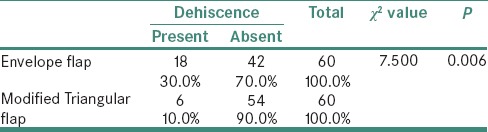
Graph 2.
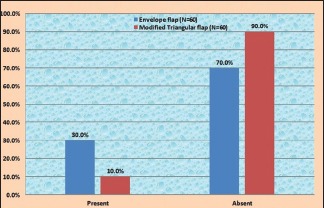
Distribution of dehiscence between two treatment groups
In the evaluation of pain, it was noted that on the 1st day postoperatively, in the patients treated with the modified triangular flap, 8.3% (5 patients) exhibited severe pain while no patients showed on 3rd day and no patients treated with the envelope flap exhibited severe pain. The P values for envelope flap were 0.3 and 0.06 for the modified triangular flap group patients which was not statistically significant as evaluated on the 1st and 3rd day postoperatively [Table 5 and Graph 3].
Table 5.
Comparison of post operative pain scores between the envelope and modified triangular flaps
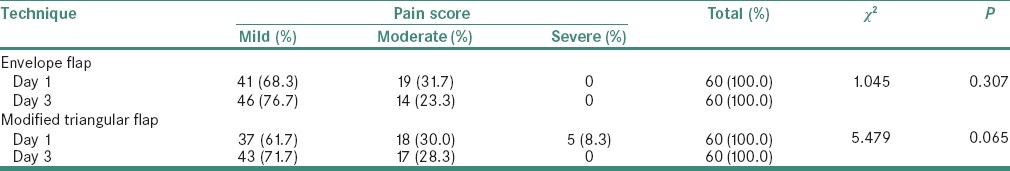
Graph 3.
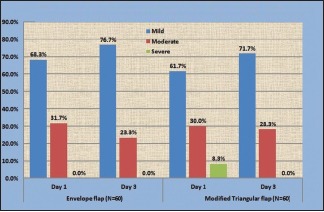
Distribution of periodontal pocket (in mm) between two treatment groups
When the periodontal probing depths (PPDs) were evaluated 3 months postoperatively, it was observed that, in the envelope flap treated group, 28.3% (17 patients) had a PPD of 5 mm, 51.7% (31 patients) had 4 mm probing depths, 11.7% (7 patients) had 3 mm probing depths and 8.3% (5 patients) still had <3 mm probing depths. When compared to the preoperative values, it was considered statistically significant (P < 0.001).
In the modified triangular flap group, at the 3-month follow-up, though only 6.7% (4 patients) had PPD of 5 mm and 36.7% (22 patients) had 4 mm PPD, it was statistically significant (P < 0.001) when compared to the preoperative PPD [Table 6 and Graph 4].
Table 6.
Comparison of assessment of periodontal status between the envelope and modified triangular flaps after the third molar removal
Graph 4.
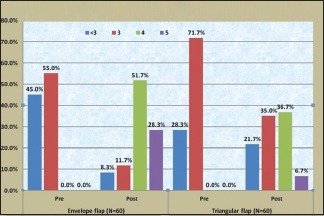
Distribution of pain score between two treatment groups at day 1 and 3 examination
DISCUSSION
Impacted third molars are commonly seen in the adult population.[16] The envelope flap with sulcular incision from the first to the second molar followed by a distal relieving incision to the ramus of the mandible has been more commonly employed for the removal of the impacted third molars.[17,18] However, from the existing literature, it is evident that there are definite benefits and negative impacts of using the envelope flap. The envelope flap provides better visibility as a larger area is uncovered, facilitating better removal of the third molar. Furthermore, this type of flap with a broad base ensures increased vascularity to the flap, extending up to the wound margins. However, there are definite disadvantages of the use of envelope flap. The most common complications reported in literature include pain, swelling, trismus and periodontal damage of the adjacent second molar following the surgery.[19]
It has been reported that smaller incisions, employing minimal reflection of the mucoperiosteum, are associated with less postoperative pain and swelling.[20] Findings of the present study revealed that the results regarding swelling were statistically significant between the envelope and the modified triangular flap. It was comparatively higher in the modified triangular flap group than the envelope flap group (P < 0.05). This is consistent with the reports of Baqain et al. and Kirk et al. who observed that the triangular flap design resulted in greater postoperative facial swelling in comparison to the envelope flap.[21,22] The probable explanation to the increased swelling noticed in the triangular flap design could be attributed to the anterior releasing incision which induces a greater inflammatory response and the resultant edema in the buccal tissues. However, in a study conducted by Dolanmaz, it was noted that there was no significant difference between the envelope and modified triangular flaps regarding postoperative swelling after impacted third molar surgery.[23]
In the present study, though pain scores were not statistically significant, the modified triangular flap group exhibited greater pain scores compared to the envelope flap group on the 1st and the 3rd days postoperatively. From the existing literature, it is evident that there is no significant correlation between the flap design and ensuing postoperative pain. Kirk et al. have observed no statistically significant results concerning pain between the envelope and the triangular flap designs which is similar to the findings of our study.[22] However, higher pain scores were observed with the envelope flap design in a study conducted by Sandhu et al.[24] and Aliasghari Abandansari S and Foroughi R et al.[25] which is contradictory to the findings of our study.
In the present study, it was observed that the envelope flap design revealed higher evidence of the presence of dehiscence (30%) in relation to the second molar. Six patients treated with the modified triangular flap (10%) had evidence of dehiscence postoperatively, but it was significantly higher with the envelope flap design. However, in a study conducted by Rahpeyma et al.,[26] it was observed that the dehiscence was higher following both techniques but more significant with the envelope flap design, 43% and 19% in the envelope and triangular transposition flap groups, respectively. It is evident from previous literature that the envelope flaps are commonly associated with occurrence of dehiscences at the distofacial aspect of the second molars.[14] Such gapings maybe usually seen at the distobuccal gingival rim of the adjacent second molar, at the position where the distal relieving incision leads into the sulcular incision. The occurrence of dehiscence can be explained by the fact that the envelope flap is fixed anteriorly with intersulcular sutures and the resulting postoperative hematoma causes soft tissue tension, leading to the rupture of the wound margins. In accordance with this, previous studies have shown higher occurrence of dehiscence following envelope flap technique for the third molar removal,[14,26] which is consistent with the findings of our study.
Proper assessment of the impacted third molars is crucial for improving the third molar conditions, particularly the periodontal health of the adjacent second molar. This is because surgical extraction of the third molars has been attributed to cause periodontal problems.[27]
Literature suggests that about 43.3% of the cases result in probing depths of 7 mm or greater 2 years after the removal of the third molar.[28] However, there is evidence also suggesting that the removal of mandibular third molars is known to significantly improve the periodontal status on the distal root of second molars, positively influencing the overall periodontal health.[29] Furthermore, the influence of the type of flap used for lower third molar surgery on the periodontal status of the second molar is unclear.[3]
In a study conducted by Desai et al.,[30] statistically significant difference was observed in postoperative hematoma, wound gaping and distal pocket in adjacent tooth, which was significant in triangular incision group in comparison to envelope incision group. The results of this study are contradictory to the findings of our study. Periodontal pockets were more conspicuous with the envelope flap design compared to the triangular flap design in our study. However, previous studies have revealed no significant differences in the type of flap used and the outcome of increased periodontal pocket depths.[17,18] The increased postoperative pocket depths in the envelope flap designs may be explained by the fact that the sulcular incision interferes with the periodontal ligament and may lead to compromised periodontal status.[14]
One of the limitations of the study is the use of subjective scale for the assessment of swelling because the postoperative facial swelling has to be measured in three planes and thus maybe subject to error in the reproducibility. However, there is evidence from literature that the scale used for assessing swelling can be used reliably.[31]
CONCLUSION
Within the limitations of the study, it can be concluded that, when pain and swelling were considered, the envelope flap design was better compared to the modified triangular flap. The triangular flap was more efficacious when we consider the postoperative periodontal status of the adjacent second molar and the dehiscence following the wound healing in comparison to the envelope flap. Although the present study provides an insight that the modified triangular flap may be employed effectively for minimizing the compromise in the periodontal status, it is imperative that the findings of the present study must be validated in the future by a larger sample size of patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chaparro-Avendaño AV, Pérez-García S, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Morbidity of third molar extraction in patients between 12 and 18 years of age. Med Oral Patol Oral Cir Bucal. 2005;10:422–31. [PubMed] [Google Scholar]
- 2.Motamedi MH. Concepts to consider during surgery to remove impacted third molars. Dent Today. 2007;26:136, 138–41. [PubMed] [Google Scholar]
- 3.Karaca I, Simşek S, Uğar D, Bozkaya S. Review of flap design influence on the health of the periodontium after mandibular third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:18–23. doi: 10.1016/j.tripleo.2006.11.049. [DOI] [PubMed] [Google Scholar]
- 4.Monaco G, Daprile G, Tavernese L, Corinaldesi G, Marchetti C. Mandibular third molar removal in young patients: An evaluation of 2 different flap designs. J Oral Maxillofac Surg. 2009;67:15–21. doi: 10.1016/j.joms.2007.05.032. [DOI] [PubMed] [Google Scholar]
- 5.Koerner KR. The removal of impacted third molars. principles and procedures. Dent Clin North Am. 1994;38:255–78. [PubMed] [Google Scholar]
- 6.Koyuncu BÖ, Cetingül E. Short-term clinical outcomes of two different flap techniques in impacted mandibular third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:e179–84. doi: 10.1016/j.oooo.2011.12.023. [DOI] [PubMed] [Google Scholar]
- 7.Roode GJ, Bütow K. An alternative surgical flap design for impacted third molars: A comparison of two different surgical techniques. SADJ. 2010;65:246, 248–51. [PubMed] [Google Scholar]
- 8.Silva JL, Jardim EC, dos Santos PL, Pereira FP, Garcia Junior IR, Poi WR, et al. Comparative analysis of 2-flap designs for extraction of mandibular third molar. J Craniofac Surg. 2011;22:1003–7. doi: 10.1097/SCS.0b013e3182101551. [DOI] [PubMed] [Google Scholar]
- 9.Suarez-Cunqueiro MM, Gutwald R, Reichman J, Otero-Cepeda XL, Schmelzeisen R. Marginal flap versus paramarginal flap in impacted third molar surgery: A prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:403–8. doi: 10.1067/moe.2003.84. [DOI] [PubMed] [Google Scholar]
- 10.Briguglio F, Zenobio EG, Isola G, Briguglio R, Briguglio E, Farronato D, et al. Complications in surgical removal of impacted mandibular third molars in relation to flap design: Clinical and statistical evaluations. Quintessence Int. 2011;42:445–53. [PubMed] [Google Scholar]
- 11.Pell GJ, Gregory GT. Impacted mandibular third molars: Classification and modified technique for removal. Dent Dig. 1933;39:330. [Google Scholar]
- 12.Jakse N, Bankaoglu V, Wimmer G, Eskici A, Pertl C. Primary wound healing after lower third molar surgery: Evaluation of 2 different flap designs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:7–12. doi: 10.1067/moe.2002.119519. [DOI] [PubMed] [Google Scholar]
- 13.Szmyd L. Impacted teeth. Dent Clin North Am. 1971;15:299–318. [PubMed] [Google Scholar]
- 14.Beirne OR, Camilleri GE. The effect of methyl prednisolone on pain, trismus and swelling after removal of third molars. Oral Surg Oral Med Oral Pathol. 1985;61:134–9. doi: 10.1016/0030-4220(86)90173-8. [DOI] [PubMed] [Google Scholar]
- 15.Sabur JJ. Clinical Evaluation of the Dexamethasone and Piroxicam for the Control of Swelling, Trismus and Pain Following the Removal of Impacted Third Molar. MSc thesis. College of Dentistry. University of Baghdad. 1993 [Google Scholar]
- 16.Krausz AA, Machtei EE, Peled M. Effects of lower third molar extraction on attachment level and alveolar bone height of the adjacent second molar. Int J Oral Maxillofac Surg. 2005;34:756–60. doi: 10.1016/j.ijom.2005.02.006. [DOI] [PubMed] [Google Scholar]
- 17.Stephens RJ, App GR, Foreman DW. Periodontal evaluation of two mucoperiosteal flaps used in removing impacted mandibular third molars. J Oral Maxillofac Surg. 1983;41:719–24. doi: 10.1016/0278-2391(83)90188-x. [DOI] [PubMed] [Google Scholar]
- 18.Quee TA, Gosselin D, Millar EP, Stamm JW. Surgical removal of the fully impacted mandibular third molar. the influence of flap design and alveolar bone height on the periodontal status of the second molar. J Periodontol. 1985;56:625–30. doi: 10.1902/jop.1985.56.10.625. [DOI] [PubMed] [Google Scholar]
- 19.Nageshwar Comma incision for impacted mandibular third molars. J Oral Maxillofac Surg. 2002;60:1506–9. doi: 10.1053/joms.2002.36152. [DOI] [PubMed] [Google Scholar]
- 20.Shevel E, Koepp WG, Bütow KW. A subjective assessment of pain and swelling following the surgical removal of impacted third molar teeth using different surgical techniques. SADJ. 2001;56:238–41. [PubMed] [Google Scholar]
- 21.Baqain ZH, Al-Shafii A, Hamdan AA, Sawair FA. Flap design and mandibular third molar surgery: A split mouth randomized clinical study. Int J Oral Maxillofac Surg. 2012;41:1020–4. doi: 10.1016/j.ijom.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 22.Kirk DG, Liston PN, Tong DC, Love RM. Influence of two different flap designs on incidence of pain, swelling, trismus, and alveolar osteitis in the week following third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:e1–6. doi: 10.1016/j.tripleo.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 23.Dolanmaz D, Esen A, Isik K, Candirli C. Effect of 2 flap designs on postoperative pain and swelling after impacted third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:e244–6. doi: 10.1016/j.oooo.2011.11.030. [DOI] [PubMed] [Google Scholar]
- 24.Sandhu A, Sandhu S, Kaur T. Comparison of two different flap designs in the surgical removal of bilateral impacted mandibular third molars. Int J Oral Maxillofac Surg. 2010;39:1091–6. doi: 10.1016/j.ijom.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 25.Aliasghari Abandansari S, Foroughi R. Effect of releasing incision on the post operative complications of third molar surgery. International Journal of Advanced Biotechnology and Research. 2016;7:1144–51. [Google Scholar]
- 26.Rahpeyma A, Khajehahmadi S, Ilkhani S. Wound dehiscence after wisdom tooth removal in mandibular mesioangular class IB impactions: Triangular transposition flap versus envelope flap. J Dent Res Dent Clin Dent Prospects. 2015;9:175–80. doi: 10.15171/joddd.2015.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ganss C, Hochban W, Kielbassa AM, Umstadt HE. Prognosis of third molar eruption. Oral Surg Oral Med Oral Pathol. 1993;76:688–93. doi: 10.1016/0030-4220(93)90035-3. [DOI] [PubMed] [Google Scholar]
- 28.Hassan KS, Marei HF, Alagl AS. Does grafting of third molar extraction sockets enhance periodontal measures in 30- to 35-year-old patients? J Oral Maxillofac Surg. 2012;70:757–64. doi: 10.1016/j.joms.2011.09.010. [DOI] [PubMed] [Google Scholar]
- 29.Motamedi MH. Preventing periodontal pocket formation after removal of an impacted mandibular third molar. J Am Dent Assoc. 1999;130:1482–4. doi: 10.14219/jada.archive.1999.0060. [DOI] [PubMed] [Google Scholar]
- 30.Desai A, Patel R, Desai K, Vachhani NB, Shah KA, Sureja R, et al. Comparison of two incision designs for surgical removal of impacted mandibular third molar: A randomized comparative clinical study. Contemp Clin Dent. 2014;5:170–4. doi: 10.4103/0976-237X.132308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huskisson EC. Measurement of pain. Lancet. 1974;2:1127–31. doi: 10.1016/s0140-6736(74)90884-8. [DOI] [PubMed] [Google Scholar]


