Summary
We describe a case of femtosecond laser–assisted cataract surgery (FLACS) in an eye with multiple comorbidities, including retinal detachment surgery, high myopia, posterior chamber phakic intraocular lens (PC pIOL) and residual, emulsified, silicone oil located in the anterior chamber. FLACS was affected by the optical blockage, but the incomplete capsular tear was recoverable. The case suggests that silicone oil bubbles concentrated at the dome of the posterior corneal surface, along with the PC pIOL optic edges and scars after corneal astigmatic relaxing incisions can lead to incomplete anterior capsulotomy.
Introduction
The major steps of femtosecond laser–assisted cataract surgery (FLACS) are anterior capsulotomy, nucleus fragmentation, and clear corneal incision.1 FLACS provides a precise anterior capsulotomy in uncomplicated cataract surgery.1–3 Femtosecond laser nucleus fragmentation reduces the ultrasonic energy utilized during phacoemulsification.3,4 The literature on application of FLACS in complicated cases is sparse.5 To our knowledge, only a single report documents results of femtosecond laser use for cataract surgery in postvitrectomy eyes with silicone oil located in the vitreous cavity.6 The literature is also sparse on FLACS in the presence of phakic intraocular lenses.7–9 In 2 eyes implanted with the rigid iris-claw phakic lens and in 1 eye with the implantable collamer phakic lens (ICL), all laser steps were successfully completed.8 Laser parameters were modified by increasing depth, vertical spot spacing, and anterior and posterior safety margins for the ICL case.7 It is also known that cavitation gas bubbles entrapped under the phakic intraocular lens (IOL) following femtosecond laser application may result in anterior capsulotomy tags.9
Cataract surgery in highly myopic eyes can be complicated by zonular instability, extreme deepening of the anterior chamber (known as “lens-iris diaphragm retropulsion syndrome”), higher risk of postoperative retinal detachment, difficulties in predicting correct IOL power, and lower visual potential.10–12 Theoretically, some of these challenges may be avoided by using FLACS, which helps to create a perfectly round anterior capsulotomy and softens the lens nucleus.
Case Report
A 32-year-old man was referred to S. Fyodorov Eye Microsurgery State Institution with decreased vision in the right eye. Thirteen years previously (2003) he had undergone bilateral implantation of RSK-3 collamer PC pIOLs at S. Fyodorov Eye Microsurgery, Moscow, Russia to correct high myopia. Schematic representation of the design of this lens with dimensions is presented (Figure 1A). Simultaneous bilateral arcuate keratotomy was performed to correct preexisting with-the-rule corneal astigmatism. In 2011 the patient`s right eye had a macula-off retinal detachment (RD), and he underwent vitrectomy followed by intraoperative laser photocoagulation and silicone oil tamponade (Oxane 1300, Baush&Lomb). After 2 months the retina was completely attached, and the silicone oil was removed. Right eye uncorrected distance visual acuity was 20/200 and best-corrected distance visual acuity was 20/63, with a manifest refraction of −2.50 +2.50 ×95 (Table 1). Minimal persistent subfoveal fluid accumulation was revealed by optical coherence tomography (OCT). Fundus examination and macular OCT of the left eye were unremarkable.
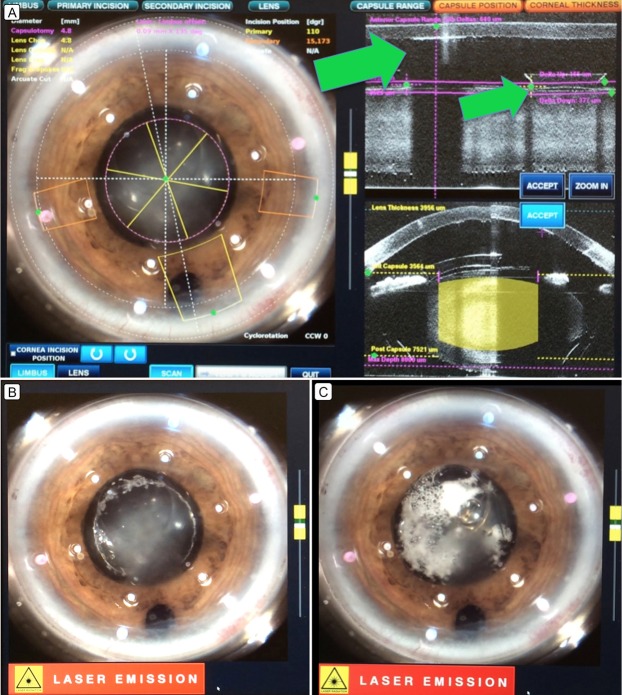
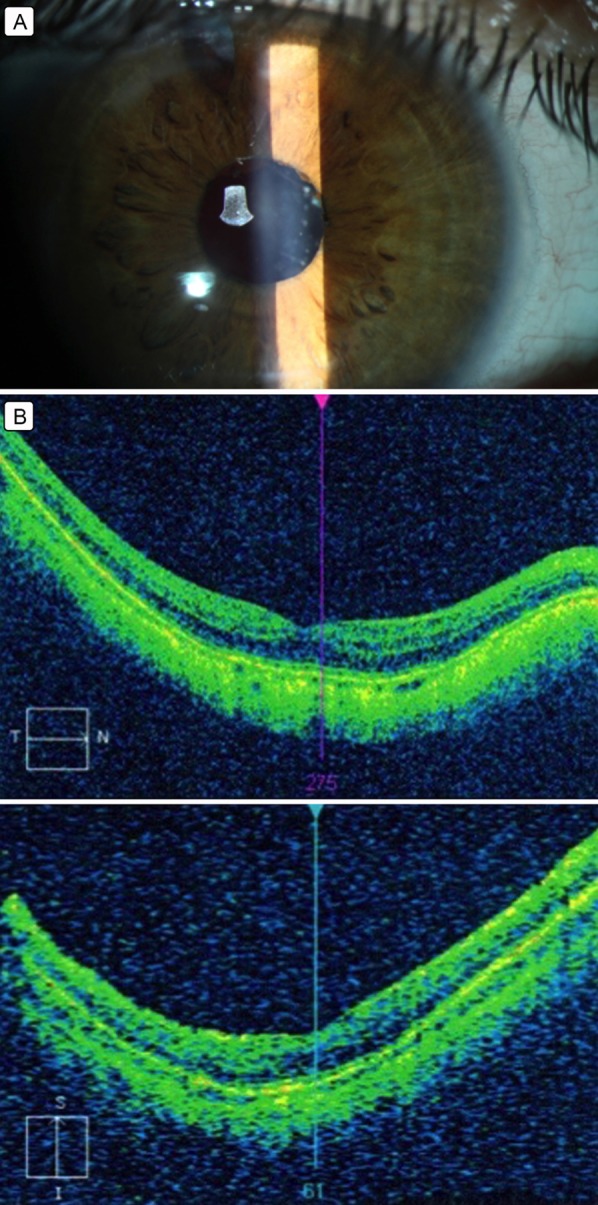
Figure 1.
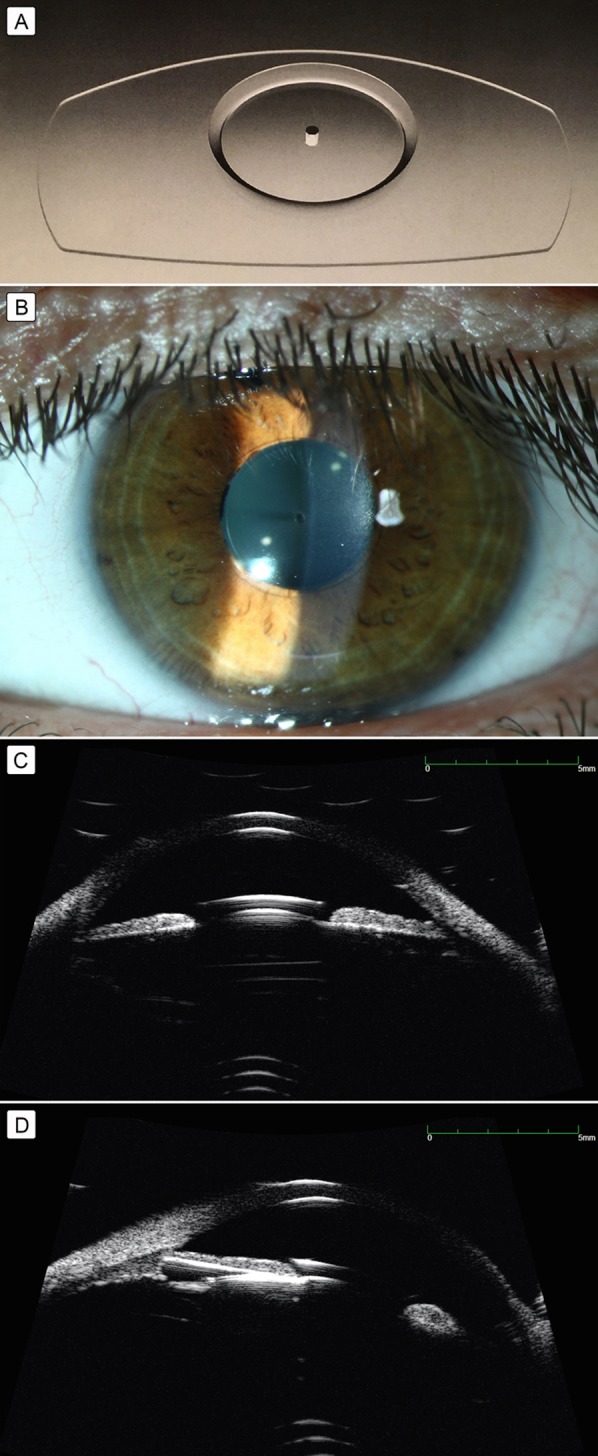
A, Posterior chamber collamer phakic intraocular lens RSK-3 (S. Fyodorov Eye Microsurgery, Moscow, Russia). B, Slit-lamp view of the anterior segment. C–D, Anterior segment ultrasound biomicroscopy of the right eye showing collar-button-type collamer posterior chamber lens (C) and visualization of lens haptics (D).
Table 1.
Preoperative diagnostic data
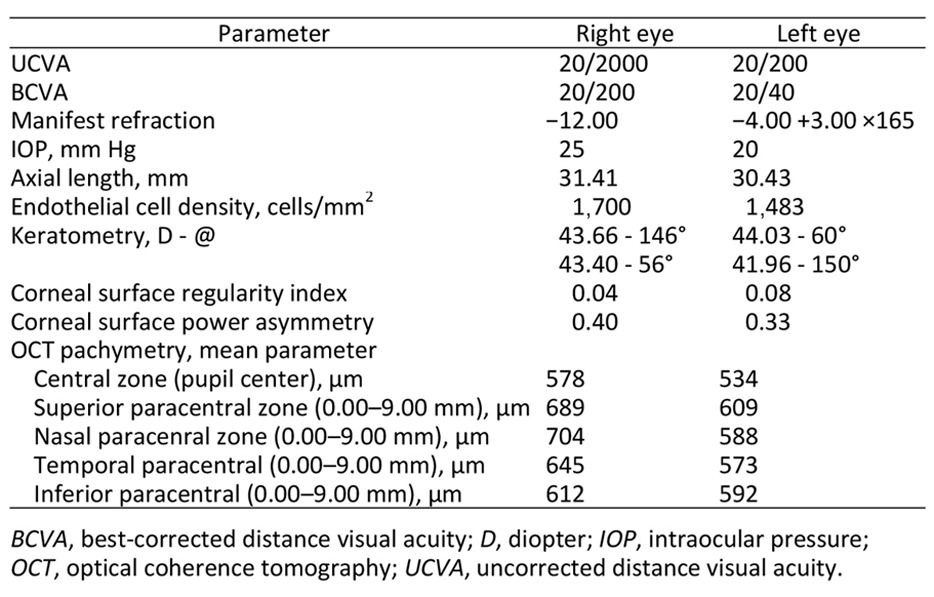
On admission, the right eye was quiet. Slit-lamp examination revealed fine dispersed droplets of emulsified silicone oil located on the upper region of the posterior corneal surface and anterior iris surface. The PC pIOL was in the correct central position, with a small peripheral iridectomy located at 12 o’clock. Opacification of the anterior subcapsular portion and nucleus of the natural lens was observed (Figure 1B). Emulsified silicone oil in the right eye was also detectable by gonioscopy, with droplets located in the superior anterior chamber angle. The patient’s right eye uncorrected visual acuity was 20/2000; best-corrected visual acuity had decreased to 20/200 with a manifest refraction of −12.00 sph. Right eye axial length (AL) was 31.41 mm as measured by IOL Master 700 (Carl Zeiss Meditec, Jena, Germany). The PC pIOL in the other eye was well centered with minimal cataractous change (Figure 1C,D).
Swept-source Fourier-domain OCT (Casia SS-1000, Tomey Corp) showed unusual peripheral corneal steepening of the right cornea of unclear etiology, given that pachymetry values were within physiologic limits. We cannot completely rule out early keratoconus or pellucid marginal degeneration, but circular cuts performed in the midperiphery of the cornea to correct preexisting astigmatism may explain this finding (Table 1).
Though controversial, in our study, the Barrett Universal II formula was selected for IOL power calculation (http://www.apacrs.org/barrett_universal2/) and the manufacturer’s A-constant was used. IOL power of 3.0 D for the Bi-flex 1.8 677AB lens (Medicontour, Geneva, Switzerland) was chosen. Because of patient preference for intermediate vision, target refraction of −1.77 D was selected. One month after surgery the uncorrected visual acuity was 20/50 and the manifest refraction was −1.5 D −0.5 ×10 with best-corrected visual acuity of 20/40. Target refraction was successfully achieved in the right eye. Right eye uncorrected and best-corrected visual acuity was significantly improved compared to preoperative visual acuity thus the history of the retinal surgery.13
The patient was informed of the risks and benefits associated with the surgical procedure, signed an informed consent, and underwent FLACS with the LenSx (Alcon, Fort Worth, TX) laser system (2.30 software) in the right eye.
Surgical Technique
The main stages in the procedure are recorded in Video 1. The first step was performed with the femtosecond laser installed in the operating room. Conventional femtosecond laser settings were used: anterior capsulotomy diameter 4.8 mm (incision depth 640 µm, pulse energy 5 µJ, tangential spot separation 4 µm, layer separation 4 µm), and lens fragmentation diameter 4.8 mm (incision depth 3956 µm, pulse energy 10 µJ, tangential spot separation 7 µm, layer separation 7 µm). Three radial cuts were adjusted for lens fragmentation. Three-plane primary corneal tunnel incision (pulse energy 5 µJ, spot separation 4 µm, layer separation 4 µm, incision position 110°, incision width 2.4 mm, desired tunnel length 1700 µm) and two additional incisions were programmed (incisions width 1.5 mm, incisions position 15° and 173°, resp.). After docking, integrated three dimensional (3-D) spectral domain optical coherence tomography (SD-OCT) was activated to visualize the anterior segment of the eye in the usual manner. An interrupted image of the capsular-lens complex was seen (Figure 2A). Using manual adjustments, the marker for anterior capsulotomy was centered according to the limbus on the laser system screen. Capsulotomy and lens fragmentation were performed (Figure 2B) followed by creation of the main and two additional clear corneal incisions (CCIs). Trapped cavitation gas was observed under the PC pIOL (Figure 2C).
Video 1.
Femtosecond laser–assisted cataract surgery in the vitrectomized eye of a 32-year-old man with a posterior chamber phakic intraocular lens
Figure 2.
Intraoperative femtosecond laser–assisted step view. A, Intraoperative view and optical coherence tomography (OCT) images of the anterior segment of the right eye showing blockage due to accumulation of emulsified silicone oil posterior to the corneal endothelium and PC pIOL optics margin. B, Intraoperative view of incomplete capsulotomy during the femtosecond laser step. C, Intraoperative view of trapped cavitation bubbles under the posterior chamber phakic intraocular lens.
The patient was moved under the surgical microscope while still in the supine position and the anterior chamber was filled with dispersive ophthalmic viscosurgical device (OVD); a mixture of 4.0% chondroitin sulfate and 3.0% sodium hyaluronate (Viscoat; Alcon Inc, Fort Worth, TX). The PC pIOL was repositioned into the anterior chamber, placed on the anterior surface of the iris and bisected with scissors. Each half of the lens was removed through the main corneal incision with toothed forceps. Inspection of the laser capsulotomy showed an uncut area. To complete the anterior capsulotomy, the capsular flap was grasped by microforceps and torn in a circular manner similar to manual continuous curvilinear capsulorhexis. Gentle hydrodissection with subsequent release of the gas bubbles located in the posterior portion of the lens was performed. During phacoemulsification it was possible to divide the nucleus along the lasered cleavage planes. After cortical clean-up, a +3.0 D hydrophilic acrylic IOL (Bi-flex 1.8 677AB Medicontour, Geneva, Switzerland) was implanted into the capsular bag.
At the first postoperative examination the eye was quiet, with minimal signs of intraocular inflammation. Postoperative medication regimen included nonsteroidal anti-inflammatory drops daily (bromfenac 0.09%) and antibiotic/steroid drops four times daily (levofloxacin 0.5%, dexamethasone 0.1%). Right eye uncorrected visual acuity significantly improved to 20/50, and the intraocular pressure was 17 mm Hg. After 1 month uncorrected visual acuity further improved to 20/40 (Figure 3A), with no improvement with refraction or pinhole. Three month postoperatively fundus examination revealed a fully attached retina, with unchanged peripheral laser photocoagulation scars and sectoral thinning of retinal nerve fiber layers in the superior paracentral, inferior paracentral and peripheral macular zones by OCT (Figure 3B).
Figure 3.
Postoperative diagnostic data. A, Slit-lamp view of the anterior segment on postoperative day 1. B, Optical coherence tomography of the macular area; retinal layers attached. There is sectoral thinning of the superior paracentral, inferior paracentral and peripheral retinal nerve fiber layers in the macular area.
Discussion
To our knowledge this is the first report of FLACS in an eye with a collamer posterior chamber phakic intraocular lens (PC pIOL) and a history of pars plana vitrectomy and silicone oil tamponade for retinal detachment. A history of previous vitreoretinal surgery can present a challenge for the cataract surgeon. Various factors including posterior synechiae, zonular dehiscence, fibrinoid reactions, glaucoma and other concurrent pathologies may impact functional outcomes.14,15 Absence of the vitreous body may lead to increased mobility of the lens capsule diaphragm and altered intraocular fluid dynamics.16
Use of the femtosecond laser is feasible in cataract surgery due to its ultrafast pulses and low energy required for tissue disruption mitigating collateral damage.5 Efficient and reproducible, laser corneal incisions, anterior capsulotomy and lens fragmentation theoretically provide advantages for vitrectomized eyes. Especially those with high axial length often associated with zonular deficiency and capsular bag instability both intra- and postoperatively.
Residual silicone oil bubbles in the anterior chamber will interfere with laser beam delivery, diverting it from its target anterior lens capsule and nucleus. If diagnosed preoperatively with gonioscopy or anterior segment OCT, it is a relative contraindication to FLACS because of the likelihood of resultant capsular tags and/or incomplete capsulotomy. Small particles of emulsified silicone oil in the anterior chamber also partially block capsule visualization by the native laser system OCT.17 In our case, oil remnants were most probably the cause of the incomplete capsulotomy from 1 to 10 clock (Figure 3A). “Light” silicone oil (in our case, Oxane 1300 cSt) has a tendency to migrate to the superior anterior chamber, locating under the endothelial layer of the cornea with the patient in a supine position. When the number of particles is minimal, the concentration of oil at the very center of the posterior corneal dome near the optical axis will mitigate the risk of laser beam interruption. Theoretically by changing the patient’s head position it is possible to move the silicone oil location in the anterior chamber. Unfortunately no laser systems allow for significant head position deviation. Another pitfall of silicone oil is its propensity to accumulate between the posterior surface of the phakic IOL and the anterior surface of the natural lens. This can be assessed preoperatively by slit-lamp examination. Should the surgeon wish to continue with FLACS, any silicone oil droplets could be moved from the path of the laser beam by pre-placing a paracenthesis and injecting OVD into the anterior chamber, forcing the droplets to the periphery and thus providing a homogeneous media for laser beam delivery and a complete capsulotomy. This technique has not been reported in the literature.
To gain access to the natural lens during cataract extraction, the phakic IOL should be extracted first, although this is challenging depending on the material and design. RSK - 3 (S. Fyodorov Eye Microsurgery, Moscow, Russia) is best repositioned into the anterior chamber and then bisected with scissors, with special attention to fixating the haptic and avoiding lens rotation and damage to the iris and anterior lens capsule. Although hydrophilic acrylic and collamer lenses are relatively easy to cut, silicone IOLs are known for their slippery nature, necessitating appropriate instrumentation to avoid excessive movement. Previously published literature shows both FLACS being used to successfully complete a circular anterior capsulotomy in the presence of pIOLs,7,8 and laser blockage by redundant gas accumulated beneath the PC pIOL, resulting in incomplete anterior capsulotomy.9 Low levels of laser energy avoid excessive cavitation and gas bubble formation.7
It is critically important to assure a complete capsulotomy before proceeding to phacoemulsification. Visualization, especially in intumescent or mature cataracts, may require staining, and capsular margin revision is amenable to a central dimple-down maneuver in the absense of free-floating capsular flap and suspected capsular tags.18 The central dimple-down maneuver is the downward motion that indents the capsule disk. The cannula or other blunt instrument can be centered at the capsule area and pressed gently downward to separate the capsule disk from the surrounding peripheral capsule.
In our case we witnessed the laser beam optical blockage by silicone oil and by the pIOL optic margin (Figure 3A). It was possible to continue the anterior continuous curvilinear capsulorhexis manually without violation of capsulorhexis integrity by grasping the capsular tear edge and lifting tissue following the circular contour created by the laser.19
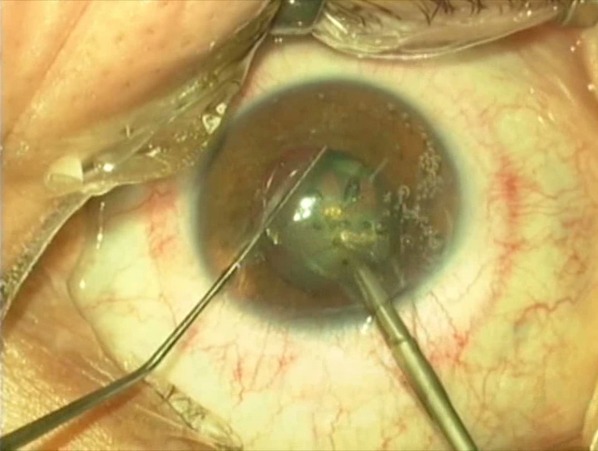
The integrated 3-D SD-OCT image shows that mydriasis may promote decentration of the collar button haptic displacing it from the optical axis thereby allowing the margin of the lens optic to deviate the beam. We believe that, when possible, the capsulotomy diameter should be adjusted to be bigger than the pIOL optic to avoid interaction of the laser beam with the margin when the laser beam would inevitably meet the optic-haptic junction laser capsulotomy, which should be avoided ( Figure 4).
Figure 4.
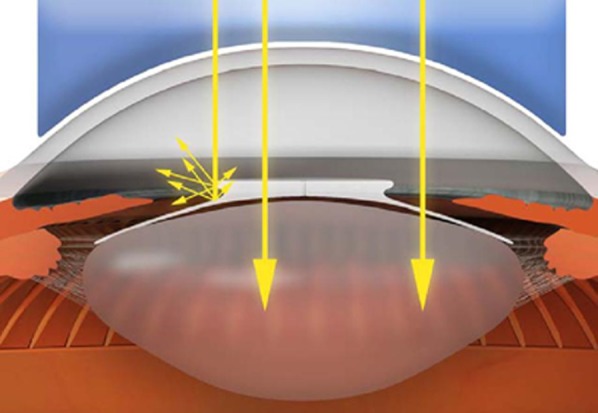
Optical blockage of the femtosecond laser beam by lens optic margin.
Our patient also presented the dilemma of abnormal corneal topography, with 16 μm thinner pachymetry readings inferiorly, presumably due to early-stage corneal pellucid marginal degeneration. The patient’s left eye presented against-the-rule corneal astigmatism, with more regular topography and pachymetry readings. If stable in the future, this eye may benefit from phacoemulsification combined with toric IOL implantation, but for the right eye, with unknown stability and early disease, we considered a one-piece aspheric IOL implanted in the capsular bag to be the best option without including intrastromal corneal ring segments and ultraviolet crosslinking. Theoretically, several other nonsurgical approaches for management of pellucid marginal degeneration, including spectacles and/or contact lenses, may be used postoperatively.20
FLACS is not always beneficial, especially in the presence of corneal comorbidity. The femtolaser is limited to cutting tunnels in clear cornea. In keratectasia it is desirable to incorporate the limbus or sclera in the cataract incision to decrease the biomechanical impact on the thinned corneal tissue. Currently there are no studies of long-term effects of femtosecond laser clear corneal incisions on thin and unstable corneas in patients with keratectasias.
As previously reported, lens fragmentation significantly lowers ultrasound time in FLACS compared to conventional phacoemulsification.21 It can be easily applied in most complicated cases. In patients with pIOL with endothelium counts decreased due to previous surgery, FLACS may have an advantage of decreasing ultrasound and irrigation trauma, especially in cases with very dense cataracts.22
Apart from technical difficulties, accurate refractive predictability of cataract surgery in highly myopic postvitrectomized eyes is challenging and often leads to unexpected postoperative hyperopia.10
Literature Search
PubMed and Google Scholar was searched in English on August 11, 2016, using the following key words: anterior capsulotomy, femtosecond laser-assisted cataract surgery, posterior chamber phakic intraocular lens, retinal detachment, postvitrectomy, and silicone oil emulsification.
Acknowledgments
The authors thank Michael Vaulin for providing original artwork in 3D graphics (Figure 4).
References
- 1.Friedman NJ, Palanker DV, Schuele G, et al. Femtosecond laser capsulotomy. J Cataract Refract Surg. 2011;37:1189–98. doi: 10.1016/j.jcrs.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 2.Popovic M, Campos-Möller X, Schlenker MB, Ahmed IIK. Efficacy and safety of femtosecond laser–assisted cataract surgery compared with manual cataract surgery: a meta-analysis of 14,567 eyes. Ophthalmology. 2016;123:2113–26. doi: 10.1016/j.ophtha.2016.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Tackman RN, Kuri JV, Nichamin LD, Edwards K. Anterior capsulotomy with an ultrashort-pulse laser. J Cataract Refract Surg. 2011;37:819–24. doi: 10.1016/j.jcrs.2010.11.030. [DOI] [PubMed] [Google Scholar]
- 4.Nagy Z, Takacs A, Filkorn T, Sarayba M. Initial clinical evaluation of an intraocular femtosecond laser in cataract surgery. J Refract Surg. 2009;25:1053–60. doi: 10.3928/1081597X-20091117-04. [DOI] [PubMed] [Google Scholar]
- 5.Grewal DS, Schultz T, Basti S, Dick HB. Femtosecond laser–assisted cataract surgery—current status and future directions. Surv Ophthalmol. 2016;61:103–31. doi: 10.1016/j.survophthal.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Grewal DS, Singh Grewal SP, Basti S. Incomplete femtosecond laser–assisted capsulotomy and lens fragmentation due to emulsified silicone oil in the anterior chamber. J Cataract Refract Surg. 2014;40:2143–7. doi: 10.1016/j.jcrs.2014.09.022. [DOI] [PubMed] [Google Scholar]
- 7.Diakonis VF, Yoo SH, Kontadakis GA, El Danasoury AM, Donaldson KE, Culbertson WW. Femtosecond laser-assisted cataract surgery in a patient with posterior chamber phakic intraocular lens. Am J Ophthalmol Case Rep. 2016;1:11–2. doi: 10.1016/j.ajoc.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaur M, Sahu S, Sharma N, Titiyal JS. Femtosecond laser-assisted cataract surgery in phakic intraocular lens with cataract. J Refract Surg. 2016;32:131–4. doi: 10.3928/1081597X-20160106-01. [DOI] [PubMed] [Google Scholar]
- 9.Li S, Chen X, Kang Y, Han N. Femtosecond laser-assisted cataract surgery in a cataractous eye with implantable collamer lens in situ. J Refract Surg. 2016;32:270–2. doi: 10.3928/1081597X-20160217-03. [DOI] [PubMed] [Google Scholar]
- 10.Abulafia A, Barrett GD, Rotenberg M, et al. Intraocular lens power calculation for eyes with an axial length greater than 26.0 mm: comparison of formulas and methods. J Cataract Refract Surg. 2015;41:548–56. doi: 10.1016/j.jcrs.2014.06.033. [DOI] [PubMed] [Google Scholar]
- 11.Cionni RJ, Barros MG, Osher RH. Management of lens-iris diaphragm 12 retropulsion syndrome during phacoemulsification. J Cataract Refract Surg. 2004;30:953–6. doi: 10.1016/j.jcrs.2004.01.030. [DOI] [PubMed] [Google Scholar]
- 12.Neuhann IM, Neuhann TF, Heimann H, et al. Retinal detachment after phacoemulsification in high myopia: analysis of 2356 cases. J Cataract Refract Surg. 2008;34:1644–57. doi: 10.1016/j.jcrs.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 13.Wolfensberger TJ, Gonvers M. Optical coherence tomography in the evaluation of incomplete visual acuity recovery after macula-off retinal detachments. Graefe’s Arch Clin Exp Ophthalmol. 2002;240:85–9. doi: 10.1007/s00417-001-0410-6. [DOI] [PubMed] [Google Scholar]
- 14.Senn P, Schipper I, Perren B. Combined pars plana vitrectomy, phacoemulsification, and intraocular lens implantation in the capsular bag; a comparison to vitrectomy and subsequent cataract surgery as a two-step procedure. Ophthalmic Surg Lasers. 1995;26:420–8. [PubMed] [Google Scholar]
- 15.Sebestyen JG. Fibrinoid syndrome: A severe complication of vitrectomy surgery in diabetics. Ann Ophthalmol. 1982;14:853–6. [PubMed] [Google Scholar]
- 16.Díaz Lacalle V, Orbegozo Gárate FJ, Martinez Alday N, López Garrido JA, Aramberri Agesta J. Phacoemulsification cataract surgery in vitrectomized eyes. J Cataract Refract Surg. 1998;24:806–9. doi: 10.1016/s0886-3350(98)80135-1. [DOI] [PubMed] [Google Scholar]
- 17.Grewal DS, Grewal SPS, Basti S. Incomplete femtosecond laser–assisted capsulotomy and lens fragmentation due to emulsified silicone oil in the anterior chamber. J Cataract Refract Surg. 2014;40:2143–7. doi: 10.1016/j.jcrs.2014.09.022. [DOI] [PubMed] [Google Scholar]
- 18.Arbisser LB, Schultz T, Dick HB. Central dimple-down maneuver for consistent continuous femtosecond laser capsulotomy. J Cataract Refract Surg. 2013;39:1796–7. doi: 10.1016/j.jcrs.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 19.Femto laser cataract: avoiding complications. Review of Ophthalmology. Jul 7, 2014. https://www.reviewofophthalmology.com/article/femto-laser-cataract-avoiding-complications. Accessed March 20, 2017.
- 20.Biswas S, Brahma A, Tromans C, Ridgway A. Management of pellucid marginal corneal degeneration. Eye. 2000;14:629–34. doi: 10.1038/eye.2000.155. [DOI] [PubMed] [Google Scholar]
- 21.Daya SM, Nanavaty MA, Espinosa-Lagana MM. Translenticular hydrodissection, lens fragmentation, and influence on ultrasound power in femtosecond laser-assisted cataract surgery and refractive lens exchange. J Cataract Refract Surg. 2014;40:37–43. doi: 10.1016/j.jcrs.2013.07.040. [DOI] [PubMed] [Google Scholar]
- 22.Taravella MJ, Meghpara B, Frank G, Gensheimer W, Davidson R. Femtosecond laser–assisted cataract surgery in complex cases. J Cataract Refract Surg. 2016;42:813–6. doi: 10.1016/j.jcrs.2016.02.049. [DOI] [PubMed] [Google Scholar]