Abstract
Objective
The purpose of this study was to undertake a systematic review of the literature to determine and compare, for patient sub-groups, the spinal level of the iliac crests as commonly measured through manual palpation and radiographic imaging procedures.
Methods
Relevant citations were retrieved by searching the PubMed, ICL, CINAHL, AMED, Osteopathic Research Web, OstMed, and MANTIS biomedical databases, and included articles were rated for quality. Search terms included Tuffier*, intercristal line, intercrestal line, Jacoby’s line, lumbar spine, lumbar landmark, pelvic landmark, palpation, and TL (Tuffier’s Line). Meta-analyses were performed on the full datasets as well as subsets based on various patient demographics.
Results
Original search strategies retrieved 1301 citations; 47 articles were used for qualitative synthesis and 31 for meta-analyses. Across these studies imaged crests were found to be most consistent with and closest to the L4–5 interspace in females and L4 spinous process in males. In comparison, the spinal level for the palpated crests was nearest to the L3–4 interspace in males and females. The palpated crest line was 0.7 levels cephalad to the imaged crest line in males, and 1.0 levels cephalad to the imaged line in females.
Discussion and Conclusions
During manual palpation, the examiner’s fingers contact soft tissue overlying the iliac crests, thereby usually identifying the L3–4 spinal level rather than the assumed L4–5 level. Palpating iliac crests to guide anesthetic injections or manual therapy without appreciating these findings can be hazardous or lead to suboptimal patient care.
Keywords: chiropractic, palpation, ilium, radiography, anatomic landmarks, lumbar vertebrae
Abstract
Objectif
Cette étude visait à entreprendre un examen systématique de la littérature dans le but de déterminer et de comparer, pour les sous-groupes de patients, le niveau rachidien des crêtes iliaques comme on le mesure souvent par palpation manuelle et imagerie radiographique.
Méthodologie
On a tiré des citations pertinentes par le biais d’une recherche dans les bases de données médicales PubMed, ICL, CINAHL, AMED, Osteopathic Research Web, OstMed, et MANTIS, et les articles compris étaient cotés aux fins de qualité. Les termes de recherche comprenaient Tuffier*, ligne intercrête, ligne de Jacoby, colonne lombaire, repère lombaire, repère pelvien, palpation et LT (ligne de Tuffier). On a effectué des méta-analyses des ensembles de données complètes, ainsi que des sous-ensembles, fondées sur les diverses données démographiques sur les patients.
Résultats
Les premières stratégies de recherche ont permis de tirer 1 301 citations; on a utilisé 47 articles aux fins de synthèse qualitative et 31 pour des méta-analyses. À l’échelle de ces études, les crêtes imagées étaient les plus conformes et proches de l’espace intercostal L4–5 des femmes et de l’apophyse épineuse L4 des hommes. Comparativement, le niveau rachidien des crêtes palpées était plus près de l’espace intercostal L3–4 des hommes et des femmes. La ligne de crête palpée était de niveau 0,7 vers la tête par rapport à la ligne de crête imagée des hommes et de niveau 1,0 vers la tête par rapport à la ligne imagée des femmes.
Discussion et conclusions
Lors de la palpation manuelle, les doigts de l’examinateur touchent aux tissus mous qui recouvrent les crêtes iliaques, ce qui, en général, détermine de ce fait le niveau rachidien L3–4 plutôt que le niveau L4–5 présumé. La palpation des crêtes iliaques visant à guider les injections anesthésiques ou la thérapie manuelle sans souscrire à ces constatations peut s’avérer dangereuse ou mener à des soins sous-optimaux aux patients.
MOTS CLÉS: chiropratique, palpation, ilion, radiographie, repères anatomiques, vertèbre lombaire
Introduction
Practitioners in the health care professions use anatomical landmarks to identify spinal levels, both to enhance diagnostic accuracy and specifically target the site of interventions. Anesthetists require precise placement of epidural catheters to optimize postoperative analgesia and minimize adverse effects. Anatomic landmarks have been used to locate acupuncture points1, and surgeons may in part base the location to begin incision on the location of anatomical landmarks2, p.18. Manual therapists palpate spinal and pelvic structures to determine boney symmetry and movement capacities. These procedures may involve using anatomical landmarks to numerate spinal levels. To identify lumbar levels, clinicians generally use the iliac crests as a landmark, which are generally thought based on imaging studies, to lie at L4 or L4–5. The line drawn across the superior aspect of the crests is usually called Tuffier’s line (TL)3, but has also been called the intercrestal line4–6, intercristal line7–10 or Jacoby’s line11. Other lumbar and thoracic levels are generally identified by counting up or down from the putative location of L4 or L4–5. Although Render12 and others convincingly demonstrated the accuracy of this landmark rule based on the imaged TL, the accuracy and reliability of identifying the L4 level by manually palpating the crests remains in question.
For instance, several studies have evaluated the accuracy of static palpation, which generally uses the palpated iliac crests to identify the L4–5 interspace; these studies have consistently reported errors such that the identified spinal level is almost always cephalad to the intended spinal level7, 13–18. In such studies a radio-opaque marker is applied to the skin at the presumed vertebral level, the location of which is then compared to the actual level as established by an imaging procedure19. Chakraverty’s7 research convincingly illustrated the basis for this systematic bias: that is, that the spinal level of the palpated crests is more cephalad than the spinal level of TL as seen on imaging studies. Chakraverty et al.7 found that although imaging associated TL with either the L4 or L4–5 spinal levels in 86.7% (mostly female) patients, the spinal level identified using the palpatory crest method was either the L3 or L3–4 spinal levels in 77.3% of cases, most commonly in females and in patients with higher body mass indices (BMIs). Findings by Kim20 also underscore the difference between spinal levels identified through imaging and palpatory methods (Figure 2). Several authors7,21–25 have pointed out that when an examiner’s fingers are placed on the “iliac crests”, in reality the palpator is compressing soft tissue (in some cases quite a lot of soft tissue) between the fingertips and the crest; this may help to explain the bias toward cephalad measurement errors.
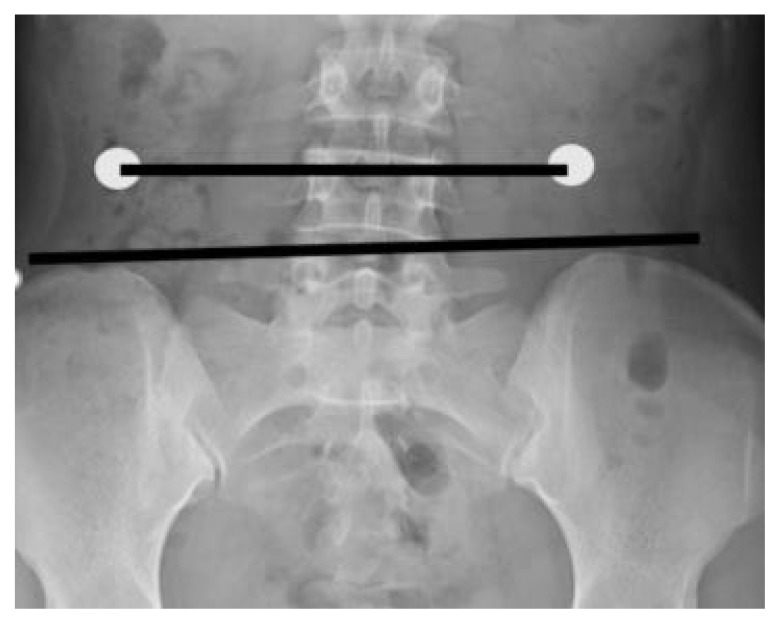
Figure 2.
White markers indicate the spinal level of the palpated
Since palpation and imaging studies have typically reported their data in terms of the frequencies with which the iliac crests intersect the L4–5 or other spinal level, rather than in terms of the mean spinal levels and their 95% confidence intervals, it has been difficult to ascertain the precise association and variability of spinal levels as measured with palpatory or imaged methods. The purpose of this study was to undertake a systematic review of the literature and perform meta-analyses on data for patient sub-groups for the spinal level associated with TL as established by both imaging and palpatory methods, and to report the data in a clinically meaningful way as mean locations and 95% confidence intervals.
Ultimately, this study intended to determine if a common strategy could be suggested for clinicians, especially manual therapists and anesthetists, to improve their ability to accurately locate lumbar and perhaps thoracic vertebral levels, by using TL or possibly an alternative anatomical structure as a landmark.
Methods
The primary inclusion criterion for an article to be included in this review was that it concerned the location of the spinal level of TL as established through either comparison with an imaging reference standard or through manual palpation. An included article, either an imaging or palpation study, did not have to explicitly aim at establishing the spinal location of Tuffier’s Line, so long as this information could be extracted from the reported results. Exclusion criteria included: reporting results in a manner that precluded calculation of mean location of TL and its standard deviation26–28; cadaveric studies29–31; studies on the accuracy of identifying L4 or L4–5 but not in relation to TL14,32; studies with a very small sample size18; studies utilizing a non-imaging reference standard33; and review/commentary articles. Databases consulted included PubMed, ICL, CINAHL, AMED, Osteopathic Research Web, OstMed, and MANTIS.
After searching these biomedical databases, the investigators supplemented the search using the global Google search engine. Searches were conducted using the following terms and/or combinations of them: Tuffier*, intercristal line, intercrestal line, Jacoby’s line, lumbar spine, lumbar landmark, pelvic landmark, palpation, and TL. It was not necessary to construct complicated Boolean phrases to limit the number of returned citations, because even very inclusive search terms returned relatively few citations; e.g., “Tuffier’s line” (likely to capture many of the relevant citations) returned only 28 citations. The “related citations” function was deployed when articles were retrieved which fit the inclusion criteria, and additional citations were harvested from included articles. Each of the included palpation articles was rated for quality using a modified version of the QUADAS instrument34, which usually includes 14 assessment criteria. We excluded one item having to do with the time period between the index and reference standards, which did not appear relevant to studies concerned with a spinal landmark association rather than diagnostic accuracy. The highest attainable score in the modified QUADAS instrument was thus 13. We used a modified version of the Arrivé instrument for the methodological quality of the included imaging studies35, which usually has 15 criteria. In the Arrivé instrument four of the 15 assessment criteria involve a reference standard related to the imaging procedure. Since this meta-analysis concerns a spinal landmark association rather than diagnostic accuracy, these four criteria were deemed irrelevant and were dropped. Thus, the lowest attainable score for an article was 11 and the highest was 33, where the lower the score, the higher the quality. The included articles were rated for quality by two reviewers; disagreements between reviewers were resolved by coming to consensus following email exchanges.
For the purpose of meta-analysis (conducted using Open Meta-Analyst, (http://www.cebm.brown.edu/openmeta/), the investigators abstracted the following data from each included article: sample size, mean location of either the iliac crests (palpation articles) or of TL (imaging articles), and standard deviation. When an included article reported data separately for subsets of the data (e.g., males and females, or obese and non-obese patients), these data were regarded as separate studies for the purpose of meta-analysis, provided different study populations were used for each. However, when different imaging procedures were conducted on the same study population, only the study using the most characteristic protocol (e.g., a flexed rather than extended patient positioning procedure) was entered into a meta-analysis, to avoid overweighting that population. On the other hand, the investigators scrutinized these other parameters for the purpose of qualitative analysis. In addition to performing meta-analysis on the full datasets for both the palpation and imaging studies, we conducted other analyses on subsets stratified by patient gender, age, and pregnancy/post-partum status. There were too few studies available of each type to conduct meta-analysis based on type of imaging (MRI, CT scan, ultrasound, fluoroscopy, x-ray), type of patient positioning (standing, supine, prone, or lateral decubitus), or body mass index (BMI). Since the authors of two palpation studies17,36 stated that their results might have been biased since the palpators were aware of prior studies that consistently showed the spinal site of the palpated TL cephalad to the imaged TL, we attempted meta-analysis with and without these studies included. However, since the results were very similar, we elected to include these studies in the meta-analyses. Very few of the studies reported the spinal level associated with TL using the spinous process as a reference point; most used the intervertebral interspace, which is more relevant in the practice of anesthesiology. When data were presented as to whether TL intersected the upper, middle, or lower portion of a vertebral body37,38, we collapsed the data to make it compatible with the great majority of the studies, which reported the intersection as occurring either within a vertebral body or at an intervertebral interspace.
Results
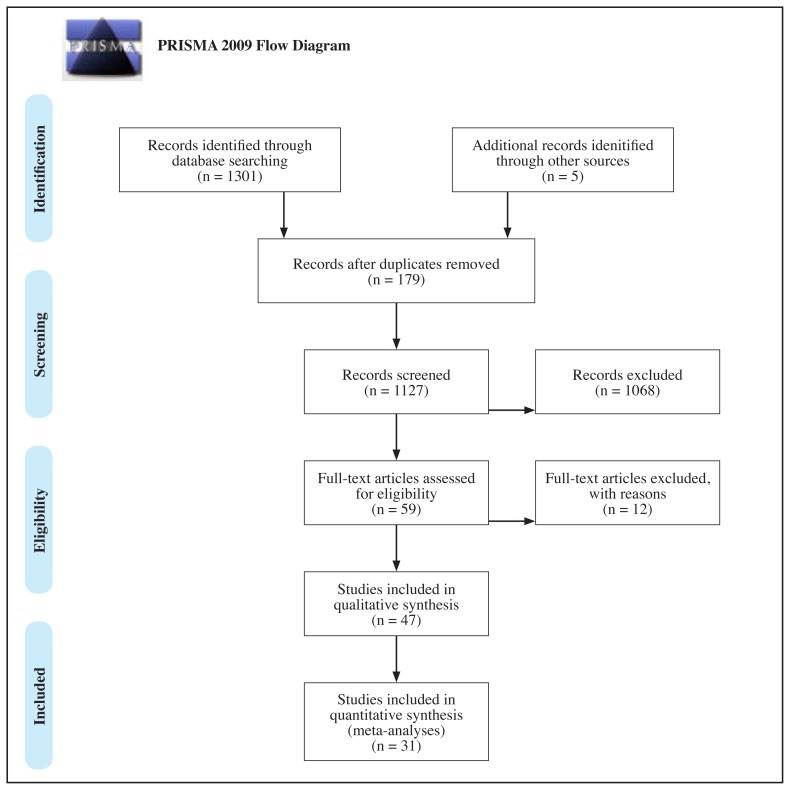
The retrieval process is summarized using the PRISMA flow diagram (Figure 1). The original search retrieved 1301 citations. After excluding 179 duplicates, 1122 unique citations remained. After inspecting their titles, 1067 were excluded from further consideration, leaving 55 abstracts to be read for consideration of possible inclusion. This resulted in the retrieval of 47 full text articles; five additional full text articles (bringing the total to 52) were retrieved either based on a secondary search of the included full text articles, searching with the Google database, or because the first author was personally familiar with them having earlier conducted a literature search on a related subject. Ultimately, 12 palpation articles and 21 imaging articles fit the inclusion criteria and were stratified into various meta-analyses. Six of the included articles7,20,21,25,36,39 contained both radiological and palpation arms. Thus 27 unique articles were included and entered into the study and included in Table 2, which summarizes these articles and includes quality ratings.
Figure 1.
PRISMA Flow Diagram
Table 2.
Data summary
| Study | Exam method(s) | Subjects | Imaging/palpatory technique | Findings and comments | Methodological quality* |
|---|---|---|---|---|---|
| Amin (2014) | P | N=100, mean 39yrs, 72.6kg, M 94%, 6 surg. | FL, X | Radiological and US assessments agreed; palpatory TL about ½ level cephalad. Apparent mislabeling of data columns. | 12 (Q) |
| FL | N=100, mean 39yrs, 72.6kg, M 94%, 6 surg. | Patient supine | 16 (A) | ||
| X 1 | N=100, mean 39yrs, 72.6kg, M 94%, 6 surg. | ? | |||
| US | N=100, mean 37yrs, 71.2Kg, M 100% | Patient seated | |||
| X 2 | N=100, mean 37yrs, 71.2Kg, M 100% | ? | |||
| Baxter (2016) | P | N=30, neonates, gender | US, Left lateral decubitus | Palpatory crest cephalad to radiological prior reports. | 11 (Q) |
| Broadbent (2000) | P | N=100, excluded boney tenderness, spinal deformity; in which 7 cases were palpated for the spinal level of TL; age <16 yrs, mean BMI 6, mean 73kg, gender not reported. | MRI, patients received seated and flexed palpatory assessment | Accuracy unaffected by patient position (sitting or lateral), Markers placed far from crest more likely to be misidentified. Obesity impaired accuracy. | 11 (Q) |
| Chakraverty (2007) | P | N=49 females | Prone | Mean 45 years, mean 73.3kg, Palpated crest cephalad to TL, and more cephalad spinal levels likely identified with increasing patient BMI. The PSIS line identified the S2 spinous process in 51% of cases. | 13 (Q) |
| P | N=26 male | Prone | |||
| F | N=49 females | Prone | 20 (A) | ||
| F | N=26 male | Prone | |||
| Chin (2005) | X | N=48 surgical patients, 62% female, mena 58yrs | Standing lateral, higher crest used as landmark | Slight trend for the L4/L4–L5 level to shift cephalad relative to the iliac crest in flexed/prone position. | 19 (A) |
| Farshad (2015) | MRI | N=62, 55% female, 5 with lumbosacral transitional segments | Coronal evaluation | Crest more implementable and accurate than other anatomical landmarks for correct lumbar numbering with lumbosacral transitional anomalies. | 16 (A) |
| Furness (2002 | P | N=49, 62% female, mean yrs 45, mean BMI 26 | Lateral decubitus, knees flexed | Anaesthetists were aware of prior findings and may have been biased; higher rate of caudal errors than most other studies. US also compared with x-ray, data not herein provided. One x-ray could not be marked. | 12 (Q) |
| Horsanali (2015) | X | N=317 females, 20–99 yrs, 8 brackets similar numbers per bracket | AP radiographs, supine positioning | Age did not impact imaged crest, unlike Rahmani 2011 and Kim 2007. | 19 (A) |
| X | N=273 males, 20–99 yrs, 8 brackets similar numbers per bracket | AP radiographs, supine positioning | |||
| Jung (2004) Age unrelated to spinal level of imaged TL. | X | N=100 volunteers, 50% female | Supine, lateral decubitus | With lumbar flexion, the imaged crest moved caudally. | 22 (A) |
| X | Same | Lateral fully flexed x-rays | |||
| Kim (2003) | MRI | N=690, 49.7% female, age>20, mean 63kg | MRI. Patients supine, legs elevated. | The positions of the conus medullaris and Tuffier’s line were lower in women than in men and higher with sacralization. Although transitional vertebra effect position of the conus medullaris and Tuffier’s line, the safety margin is unchanged. With increased age the conus was lower and TF line was higher. | 21 (A) |
| Kim (2007) | P | N=72, 73.6% females, males mean yrs 25.4 and mean BMI 21.9, female mean yrs 36.2 and BMI 20.9 | Prone | Interexaminer reliability of palpation was significantly greater for PSIS level than for the iliac crest. | 11 (Q) |
| X | Same as P group. | PA x-rays | 20 (A) | ||
| Kim (2014) | US | N=40 females, pregnant | Lateral decubitus | Compared palpated crest with vertebral levels established by US. Vertebral levels were more cephalad in the pregnant women compared to the non-parturient women. | 20 (A) |
| US | N=40 females, non-pregnant | Lateral decubitus | |||
| Kuhns (1978) | X | N=50, patients undergoing excretory urography. Mean BMI 25.8, mean weight 68.2kg | Supine, knees flexed | Data reported for 52 patients, although method states N=50. | 26 (A) |
| Lee (2011) | P | N=51 pregnant patients | Seated | BMI did not correlate with a greater disparity between the clinical estimates and ultrasound-determined levels. US more accurate than palpation to identifying the lumbar interspaces. | |
| US | Same as P group. | Seated | |||
| Lin (2015) | P | N=52 volunteers, 67.3% females. Males mean yrs 46.9, BMI 23.4; females mean yrs 48, BMI 23.4 | Left lateral decubitus, flexed. | Patients with smaller abdominal circumference, lower BMI, and younger patients had actual intervertebral levels lower than the palpated level. Radiographic TL in relation to spine did not change from lateral to hyperflexion positions. | 16 (A) |
| X | Same as P group | Left lateral decubitus, flexed | |||
| X | Same as P group. | AP, patient supine | |||
| McGaugh (2007) | CT | N=50 females, mean 47.2 yrs | CT, supine, no flexion | Age unrelated to spinal level of imaged TL. PSIS more consistent spinal reference landmark for iliac crest. | 19 (A) |
| CT | N=50 males, mean 47.5 yrs | CT, no flexion | |||
| Pysyk (2010) | P | N=64 females. Mean 45.8 yrs, BMI 25.8 | US, seated, flexed | Compared palpated crest with vertebral levels established by US. Greater proportion males-to-females with a more cephalad palpated compared to imaged TL. Males and taller individuals had palpated TL as high as ZL2–3, similar to reports of Kim, 2003 and Snider 2008. | 11 (Q) |
| P | N=50 males. Mean 45.3 yrs, BMI 27.0 | US, seated, flexed | |||
| Render (1996) | X | N=163 | PA supine, hips flexed | TL was <L4 in 17.8% and at L3–4 in 3.7% of patients. | 27 (A) |
| Sahin (2014) | P | N=50 lean pregnant. Mean yrs 31, BMI 26.4 | US | Compared palpated crest with vertebral levels established by US. The palpatory crest level of the spine was more cephalad in larger BMI patients. | 13 (Q) |
| P | N=50 obese pregnant. Mean yrs 32.4, BMI 34.1 | US | |||
| Sargin (2015) | X | N=204 female children <16 yrs | Standing AP X-rays | TL was related to age, more caudal in younger children. No differences based on gender. Unlike Tame, 2003, reported spinal level of TL in range L4 to L5-S1. | 19 (A) |
| X | N=315 male children <16 yrs | Standing AP X-rays | |||
| Shiraishi (2006) | X | N=48 females | Standing, neutral | Mean age both genders combined 48.3 yrs. Could not determine if AP, PA, or lateral radiography. No difference between males and females between extension or flexion, whereas in flexion the spinal level of TL became more caudal in males. Spinal level of TL more cephalad in older patient due to spinal degeneration. | 20 (A) |
| X | N=48 females | Standing, flexed | |||
| X | N=48 females | Standing, extended | |||
| X | N=52 males | Standing, neutral | |||
| X | N=52 males | Standing, flexed | |||
| X | N=52 males | Standing, extended | |||
| Shlotterbeck (2008) | P | N=99 pregnant females, in which 20 cases were palpated for the spinal level of TL at L4–5 | US assessment performed in same position as one in which block performed. | US used to determine spinal level of needle insertion during neuraxial anesthesia. Six punctures were actually carried out at the L1/L2 intervertebral space. | 11 (Q) |
| Snider (2008) | X | N=33 female | PA prone | Age not recorded, but range 2–45 yrs. No clinical data available, for x-ray arm. Mean BMI 25.9 palpatory arm. BMI did not impact spinal location of TL. No difference in standing and prone results. | 19 (A) |
| X | N=27 male | PA prone | |||
| X | N=100 females | PA standing | |||
| X | N=100 males | PA standing | |||
| Tame (2003) | MRI | N=49 children, both genders, <10 yrs | Supine | No clinical information provided. No age effect. | 21 (A) |
| Tanaka (2013) | P | N=967 C-section cases, in which 20 cases were palpated for the spinal level of TL | X-ray, right lateral decubitus | Abdominal x-ray confirmed level of insertion of epidural catheters. Palpation not reliable for spinal level of TL. | 13 (Q) |
| Walsh (2011) | X | N=450, 20–90 yrs, | AP and lateral x-ray | Spinal level of TL increased with age. | 19 (A) |
| Wattanaruangkowit (2010) | X | N=270, 6 age brackets 2–80 yrs. | AP and lateral x-ray | No clinical information provided other than age. Spinal level of TL increased with age. | 22 (A) |
| Whittey (2008) | P | N=121 post-partum, in which 22 cases were palpated for the spinal level of TL | US, seated | The backs of subjects were examined to identify the puncture site of the spinal or epidural needle. No other clinical information provided. | 13 (Q) |
(A )= Arrivé for imaging studies, n/33, lower scores, higher quality. QUADAS for palpation studies, n/13, higher numbers, higher quality
Abbreviations: P=palpation study; X=x-ray, MRI=magnetic resonance image; CT= computed tomography; F=fluoroscopy; US=ultrasound
Among the imaging studies that included an arm addressing the ability of a palpator to numerate the lumbar spinal level associated with TL, one of them10 did not provide sufficient detailed information to be included among the palpation articles. Some of the included palpation studies8,13,15–18,40 reported on the spinal level that was associated with the crests, but did not address the actual spinal level of TL.
Several of the included studies considered the impact of various demographic variables on the location of either the crests or the imaged TL. Although some authors found age insignificant10,15,41 in adult patient cohorts, and one study found the same in a pediatric cohort42, other authors found that the imaged TL was more cephalad in an elderly population6,23,25,38 and among older pediatric patients37. Several studies determined the palpated crests or imaged TL to be more caudal in females 7–9,23,26,27,41,43,44, although gender was insignificant in a pediatric population37. Sagittal plane posture (extension, flexion, or neutral) had a modest impact in which TL became more caudal in flexion4,,22,36; Lin25 on the other hand did not find flexion in patient positioning to have this effect. Even though Shiraishi38 reported that flexion lowered TL compared with extension in males, the findings as reported in percentage terms are at best heuristic; in our secondary analysis, we found the change clinically insignificant, with the mean spinal level of TL in males in flexion dropping only minutely from L4.21 to L4.26. In agreement with our analysis, Snider 9 did not report a flexion effect. Pregnancy shifted TL cephalad24,45. Obesity or elevated BMI tended to diminish accuracy in palpation according to Broadbent13 and raised the spinal level of TL 7,25,37. Although weight and height had an equivocal impact on the location of the spinal level of the palpated crests, a variety of overlapping factors – increased body mass index7, obesity10,13,36, and abdominal circumference25 – resulted in the palpatory TL level being at a more cephalad spinal level.
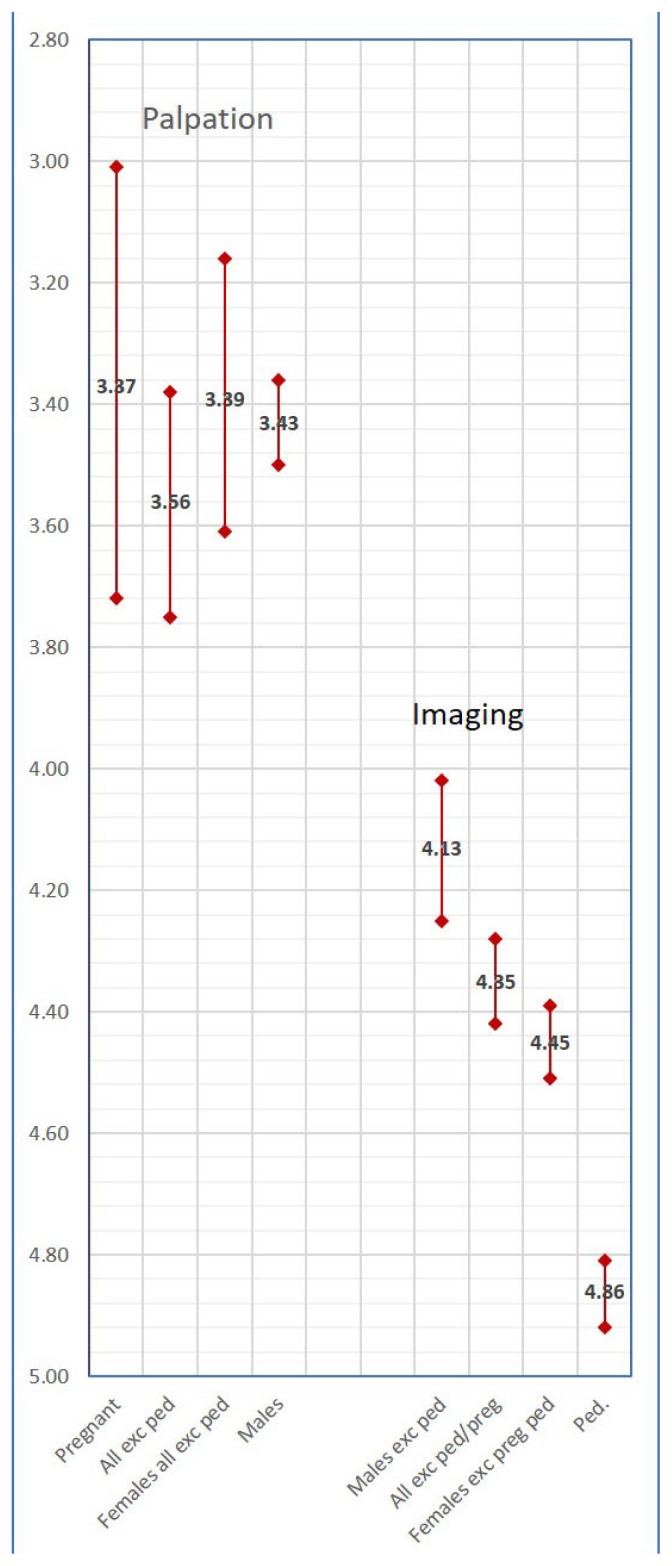
Table 1 summarizes the results of a number of representative meta-analyses performed on various subsets of the data. The spinal levels corresponding to either the iliac crests in palpation studies or TL in imaging studies are reported as “L” followed by a number with 2 decimal places. For example, “L3.45” indicates that the spinal level was a little cephalad to the L3–4 interspace. Although the status of being pregnant or post-partum impacted imaging results for females, the lack of an effect while identifying the spinal level associated with crest palpation allowed us to include these cohorts in the meta-analytic results for the female palpation articles. Table 1 includes several rows that compare representative means of the imaged and palpatory crests. Figure 6 provides the means and 95% confidence intervals for the imaged vs. palpatory spinal levels corresponding to Tuffier’s Line for representative studies.
Table 1.
Meta-analyses and most representative differences (higher numbers more caudal spinal level*).
| n | Subjects | Spinal level | Lower | Upper | I^2 % | |
|---|---|---|---|---|---|---|
| Row | Palpation studies | |||||
| 1 | 15 | All, exclude pediatric | 3.56 | 3.01 | 3.72 | 93.5 |
| 2 | 8 | Females, all exclude pediatric | 3.39 | 3.16 | 3.61 | 92.6 |
| 3 | 3 | Males, all, exclude pediatric | 3.43 | 3.36 | 3.50 | 5.3 |
| Imaging studies | ||||||
| 4 | 23 | All, excluding pediatric, pregnancy | 4.35 | 4.28 | 4.42 | 96.1 |
| 5 | 6 | Females, PP, pregnant, pediatric excluded | 4.44 | 4.39 | 4.51 | 91.3 |
| 6 | 7 | Males, pediatric excluded | 4.13 | 4.02 | 4.25 | 93.1 |
| 7 | 3 | Pediatric studies only | 4.86 | 4.81 | 4.92 | 69.1 |
| *Explanation regarding spinal numeration: “4.5” = L4–5 interspace, so that 4.75 would be more caudal | ||||||
| Most representative differences | Delta | Interpretation | ||||
| 8 | Imaged vs. palpatory crest, genders combined (mean 5–6 minus mean 2–3) | 0.88 | Palp crest almost 1 level cephalad, average for both genders | |||
| 9 | Imaged vs palpatory crest, males (3–6) 0.70 Palp crest cephalad | 0.7 | levels more cephalad to crests in males | |||
| 10 | Imaged vs. palpatory crest females (2–5) | 1.05 | Palp crest almost one level cephalad to crests in females. | |||
| 11 | Imaged crest males vs. females (5–6) | 0.31 | TL nearest L4 in males, nearest 4.5 females | |||
| 12 | Palpatory crest males vs. females (2–3) | 0.04 | Male/female palpatory crests near L3.5, slightly higher in males. | |||
Abbreviations: n= number studies included; PP=post-partum; ped=pediatric
Figure 6.
Imaged vs. palpatory spinal levels corresponding to Tuffier’s Line.
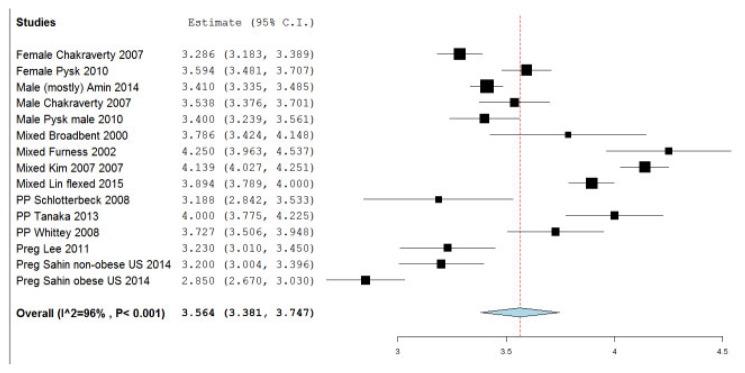
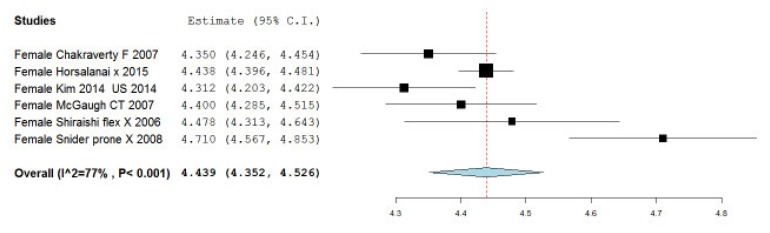
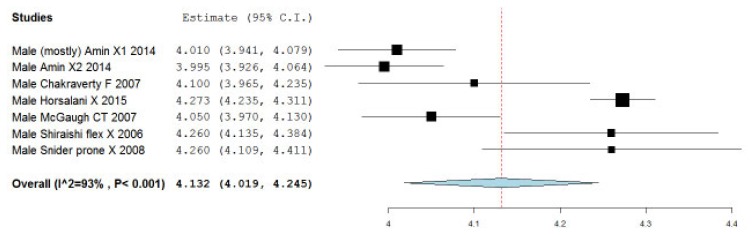
The most representative of the meta-analyses performed are provided in Figures 3–5, which includes forest plots summarizing the data. Figure 3 includes all non-pediatric palpation articles. Figure 4 includes imaged crest studies for females, exclusive of pediatric and pregnancy/post-partum patient cohorts. Figure 5 includes the imaged crest studies for males, exclusive of pediatric studies.
Figure 3.
Palpatory crests (pediatric excluded)
Figure 4.
Imaged crest, females (excluding pediatric, pregnant/post-partum)
Figure 5.
Imaged crest (males, excluding pediatric)
The forest plots in Figures 3–5 include a vertical line that represents the central tendency of the combined data, the Grand Mean. The horizontal lines then illustrate the individual study means for the spinal level of the imaged or palpated iliac crests, and their 95% confidence intervals. The diamond represents the point estimate and confidence interval for the combined studies.
Discussion
Meta-analytic methods usually calculate the odds ratios for alternative treatments, assigned to experimental and control groups. In that scenario, the forest plot includes a vertical line intersecting the X axis at an odds ratio of one. The individual studies are then mapped to show their mean effects and confidence intervals, which makes it easy to see whether their odds ratio is above or below 1.0, and thus whether the control or experimental treatment is favored. Since we were not looking at alternative treatments, but rather mean spinal levels and 95% CIs, the forest plots in our study include a vertical line that represents the central tendency of the combined data, the Grand Mean. The horizontal lines then illustrate the individual study means and their CIs. Most authors would suggest that overlapping lines suggest studies that show statistical agreement. We pooled data from several smaller studies to establish the relationship of the spinal level identified by iliac crest palpation and that of the imaged TL, including sub-analyses based on demographic and other characteristics. To select the most representative population for determining the difference between the spinal level of the imaged and palpated iliac crests (row 8, Table 1), we excluded studies featuring post-partum and pregnant females; as well as pediatric patients. In addition to reporting the data by gender, we also reported means for combined male and female cohorts. The imaged TL was closest to the L4–5 interspace while the palpated TL was closest to the L3–4 interspace, corresponding to about a one-level difference. The female imaged crest line is at L4.44 (row 5) whereas the imaged male crest line is slightly higher at L4.13 (row 11). The female and male palpatory crests are both very similar, very close to the L3–4 interspace (rows 2 and 3, respectively).
Even though the imaged TL is 0.31 levels more caudal in females than in males (4.44 females, 4.13 males), as seen in row 11, the palpated crest line is virtually the same at the L3–4 interspace for both genders (3.39 females, 3.43 males), as seen in row 12. Chakraverty7 explains why the discrepancy between the imaged TL and palpated TL is greater in women: “Adult females who have more percentage body fat for equivalent BMIs, different fat distribution and who develop progressively greater waist to hip ratios with age than adult males were found to have proportionately more higher levels identified on palpation.” The palpator’s fingers overlay soft tissue situated above the iliac crests, especially in obese patients or those with relatively abundant subcutaneous fat tissue relative to their body mass index.7,21–25
Gallagher et al. 46 found that for an equivalent body mass index, women have significantly greater amounts of total body fat than men. The palpated crests in females at L3.39 is slightly more than 1 level higher than the imaged TL at 4.35 (row 10); while the palpated TL in males at L3.43 is 0.73 levels higher than the imaged TL at L4.13. To get a sense of the relationship between the imaged and palpated TLs for a mixed population of males and females, row 8 compares the means of males and females combined. Irrespective of gender, the spinal level of the palpated crests is almost 1 level more cephalad than that of the imaged TL.
These results suggest that using the palpated crests to determine the site for anesthetic injections can be a very hazardous practice. The safety and success of epidural blocks and cerebrospinal fluid taps depends on accurate palpation of spinal levels23,26,42. The greatest risk lies in puncturing the conus medullaris47, which on average extends to the lower portion of L1 but may reach the upper portion of L3 48. This is very close to the level of the palpated crests in our secondary analyses. Although this is not of pressing concern for the manual therapist, the success of diagnostic and therapeutic interventions in manual therapy may depend to some extent on accurate spinal palpation. The process of identifying spinal targets of intervention in the upright position, and then attempting to locate those same spinal levels in the prone position, can be quite challenging49.
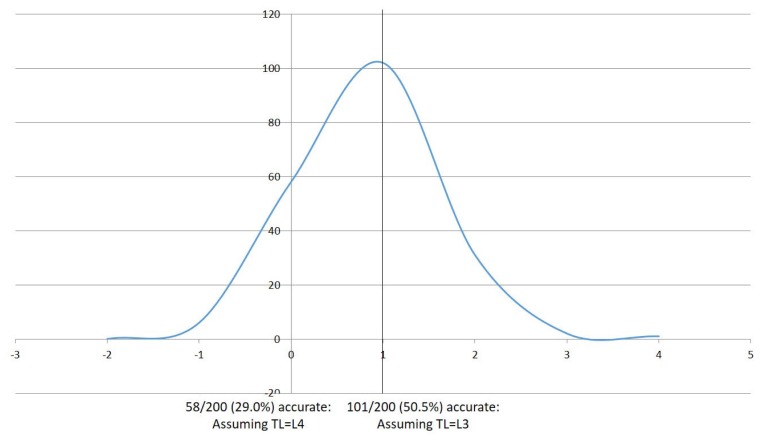
Previous studies have shown low accuracy for palpators in numerating lumbar levels and the mistakes tended to be cephalad7,13–17. This is clearly due to confounding the imaged and palpatory crest levels in relation to the lumbar spine. It would be instructive to reinterpret the accuracy achieved in these studies after having adjusted for the erroneous landmark rule wherein the palpated crest was assumed equivalent to the imaged TL; the accuracy would then be seen to have been higher than had been previously reported. As an example, Broadbent et al.13 reported that among 200 attempts by anesthetists’ to accurately identify a lumbar spinal level, only 29% were accurate. Although this may appear to indict the anesthetists’ palpatory skill per se, their error was in part explained by the erroneous landmark rule. Had they understood that the palpatory crest line was closer to the L3–4 level, their accuracy rate would have been reported to be 50.5%. Figure 7 shows the actual error rate as reported, as compared with what would have been reported based on better understanding of the spinal location of the palpatory crests.
Figure 7.
Broadbent accuracy data, reinterpreted.
A similar confusion has confounded the literature on the accuracy of thoracic spine palpation. Cooperstein has demonstrated that using the scapula to localize thoracic landmarks is very error prone, especially given the inadequacy of spinal landmark rules that are based on conventional wisdom rather than clinical research50–53. For instance, the inferior scapular tip lies closer to the T8 rather than T7 spinous process, as is commonly thought.
It is very likely that health professionals, both manual therapists and others, have been diagnosing and treating patients in part by associating spinal levels with scapular and iliac crest landmark rules that are now known to be inaccurate. In manual therapy, an intended site of spine care is often principally determined by history and physical examination, including assessment of positional asymmetry, pain/tenderness, and joint movement capacity. In such cases, it may not be crucial for an individual provider to know the exact level being treated. However, in a clinical setting with multiple providers, charting errors in numerating diagnosed and treated spinal levels could lead to improper care due to addressing non-intended levels. In addition, when physical examinations are obtained in the seated or standing position, or are in part based on imaging or specific neurological findings, it may be challenging to locate the intended spinal level in the prone position.49 These errors could lead to sub-optimal clinical outcomes, depending on the degree to which specificity in identifying sites of spine and sacroiliac care is clinically important. While correct utilization of landmark associations for the determination of a particular spinal level is plausibly important to the manual therapist, they are crucial to the anesthetist trying to identify safe and accurate locations for epidurals and other injection procedures.
This present study had several limitations. Some of the I^2 % values indicated a high degree of heterogeneity among the included studies; no doubt due to differences in the imaging technology used, the patient positioning in the imaging and palpation studies, the way the palpatory procedures were performed, and differences in the selected patient populations. The need to convert data reported for segments of a vertebra (upper, middle, lower) in some studies, rather than for discrete vertebral or intervertebral levels, may have also increased heterogeneity. In addition to explaining the variability in the data, more importantly this could compromise accuracy in clinical practice, which is something anesthesiologists and manual therapists should take into consideration. Since the QUADAS quality scores for the palpation articles were uniformly high (mean=11.8/13, s=0.94), it would have been fruitless to attempt interpreting results based on study quality. Likewise, the Arrivé scores were quite uniform (mean=20.4/33, s=2.84). Since we used the included articles only to determine spinal levels corresponding to the imaged or palpated iliac crests, and were not concerned with diagnostic accuracy, various criteria in the QUADAS and Arrivé instruments were irrelevant in our study and thus excluded. As a result, the quality scores in our study cannot be compared to possible ratings by other reviewers, who may have used all the assessment criteria. The Render study12 stood out as of lower quality than the others, with a quality score of 27/30. That stated, the reported value of L4.34 for TL was in line with the estimate of L4.45 reported by other imaging studies including both genders. As is often the case in meta-analysis, some of the articles, for both the imaging and palpation studies, showed statistically different study outcomes. That did not obscure our central finding, which is the tendency in most patient populations for the spinal level of the palpated TL to lie cephalad to the spinal level of the imaged TL. In no subject population does the 95% confidence interval for the spinal level associated with the iliac crests overlap that of the imaged TL (Figure 6)., confirming statistically different mean spinal levels.
One way of increasing accuracy in numerating lumbar vertebral levels would be for practitioners to deploy a revised landmark association whereby the spinal level, as identified using the palpatory iliac crest method, will usually be the L3 spinous process or the L3–4 interspace. However, the variability noted in these meta-analyses suggests that there may be an even better strategy: since the 2nd sacral tubercle is very dependably situated between the posterior superior iliac spines7,20,44, numerating lumbar levels based on this landmark association might be most accurate. Finding S2 in this manner, a palpator would then identify the most immediately cephalad sacral tubercle as S1, and then an equal distance cephalad to this would be the soft depression corresponding to the hypoplastic L5 spinous process, followed by the L4 spinous process (which will likely be caudal to the palpated iliac crests), followed by the L3 spinous process, and so on.
Conclusion
This study confirms reports by previous authors that the spinal level of the palpated crests is cephalad to the imaged TL, and this difference was quantified as being just about 1 spinal level. The difference is greater in females than males. Past studies on the accuracy of lumbar static palpation should be re-interpreted considering these findings, since reported accuracy rates in those studies assumed that TL corresponded to the L4 spinous process or the L4–5 interspace. A more accurate method is recommended to locate the TL spinal level, especially for higher risk procedures including the epidural blocks and cerebrospinal fluid punctures practiced by anesthesiologists. Clinicians would be well-served practicing according to an updated landmark association wherein the palpated crests will usually correspond to the L3–4 interspace; or clinicians may attempt to locate L4 or L4–5 by counting up from the 2nd sacral tubercle 7,20,44; or by using the 10th rib 22 as a landmark. Using a combination of those methods would most likely be good clinical practice compared with abject reliance on any one method.
Footnotes
Disclaimer: Neither of the investigators have any commercial or other conflict of interest associated with this project.
References
- 1.Omi S, editor. WHO standard acupuncture point locations in the Western Pacific Region. Manila, Phillippines: World Health Organization; 2008. 2008. [Google Scholar]
- 2.Little GL, Merrill WH, editors. Complications in Cardiothoracic Surgery: Avoidance and Treatment. 2 ed. Hoboken: Wiley-Blackwell; 2011. [Google Scholar]
- 3.Tuffier T. The treatment of chronic empyema. Ann Surg. 1920;72(3):266–287. doi: 10.1097/00000658-192009000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim JT, Jung CW, Lee JR, Min SW, Bahk JH. Influence of lumbar flexion on the position of the intercrestal line. Reg Anesth Pain Med. 2003;28(6):509–511. doi: 10.1016/j.rapm.2003.08.027. [DOI] [PubMed] [Google Scholar]
- 5.Mullin L. Radiographic variability of the intercrestal line. J Chiropr Educ. 2006;20(1):37. [Google Scholar]
- 6.Wattanaruangkowit P, Lakchayapakorn K. The position of the lumbar vertebrae in relation to the intercrestal line. J Med Assoc Thai. 2010;93(11):1294–1300. [PubMed] [Google Scholar]
- 7.Chakraverty R, Pynsent P, Isaacs K. Which spinal levels are identified by palpation of the iliac crests and the posterior superior iliac spines? J Anat. 2007;210(2):232–236. doi: 10.1111/j.1469-7580.2006.00686.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pysyk CL, Persaud D, Bryson GL, Lui A. Ultrasound assessment of the vertebral level of the palpated intercristal (Tuffier’s) line. Can J Anaesth. 2010;57(1):46–49. doi: 10.1007/s12630-009-9208-5. [DOI] [PubMed] [Google Scholar]
- 9.Snider KT, Kribs JW, Snider EJ, Degenhardt BF, Bukowski A, Johnson JC. Reliability of Tuffier’s line as an anatomic landmark. Spine. 2008;33(6):E161–165. doi: 10.1097/BRS.0b013e318166f58c. [DOI] [PubMed] [Google Scholar]
- 10.Sahin T, Balaban O, Sahin L, Solak M, Toker K. A randomized controlled trial of preinsertion ultrasound guidance for spinal anaesthesia in pregnancy: outcomes among obese and lean parturients: ultrasound for spinal anesthesia in pregnancy. J Anesth. 2014;28(3):413–419. doi: 10.1007/s00540-013-1726-1. [DOI] [PubMed] [Google Scholar]
- 11.Shiraishi N, Matsumura G. What is the true location of Jacoby’s line? Okajimas Folia Anat Jpn. 2006;82(4):111–115. doi: 10.2535/ofaj.82.111. [DOI] [PubMed] [Google Scholar]
- 12.Render CA. The reproducibility of the iliac crest as a marker of lumbar spine level. Anaesthesia. 1996;51(11):1070–1071. doi: 10.1111/j.1365-2044.1996.tb15009.x. [DOI] [PubMed] [Google Scholar]
- 13.Broadbent CR, Maxwell WB, Ferrie R, Wilson DJ, Gawne-Cain M, Russell R. Ability of anaesthetists to identify a marked lumbar interspace. Anaesthesia. 2000;55(11):1122–1126. doi: 10.1046/j.1365-2044.2000.01547-4.x. [DOI] [PubMed] [Google Scholar]
- 14.Snider KT, Snider EJ, Degenhardt BF, Johnson JC, Kribs JW. Palpatory accuracy of lumbar spinous processes using multiple bony landmarks. J Manipulative Physiol Ther. 2011;34(5):306–313. doi: 10.1016/j.jmpt.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 15.Tanaka K, Irikoma S, Kokubo S. Identification of the lumbar interspinous spaces by palpation and verified by X-rays. Revista brasileira de anestesiologia. 2013;63(3):245–248. doi: 10.1016/S0034-7094(13)70224-1. [DOI] [PubMed] [Google Scholar]
- 16.Whitty R, Moore M, Macarthur A. Identification of the lumbar interspinous spaces: palpation versus ultrasound. Anesth Analg. 2008;106(2):538–540. doi: 10.1213/ane.0b013e31816069d9. [DOI] [PubMed] [Google Scholar]
- 17.Schlotterbeck H, Schaeffer R, Dow WA, Touret Y, Bailey S, Diemunsch P. Ultrasonographic control of the puncture level for lumbar neuraxial block in obstetric anaesthesia. Br J Anaesth. 2008;100(2):230–234. doi: 10.1093/bja/aem371. [DOI] [PubMed] [Google Scholar]
- 18.Parate LH, Manjunath B, Tejesh CA, Pujari V. Inaccurate level of intervertebral space estimated by palpation: The ultrasonic revelation. Saudi J Anaesth. 2016;10(3):270–275. doi: 10.4103/1658-354X.170104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cooperstein R, Young M, Haneline M. Criterion validity of static palpation compared with a reference standard. J Chiro Educ. 2015;29(1):74. [Google Scholar]
- 20.Kim HW, Ko YJ, Rhee WI, Lee JS, Lim JE, Lee SJ, et al. Interexaminer reliability and accuracy of posterior superior iliac spine and iliac crest palpation for spinal level estimations. J Manipulative Physiol Ther. 2007;30(5):386–389. doi: 10.1016/j.jmpt.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 21.Amin WA, Abou Seada MO, Bedair E, Elkersh MM, Karunakaran E. Comparative study between ultrasound determination and clinical assessment of the lumbar interspinous level for spinal anesthesia. Middle East J Anaesthesiol. 2014;22(4):407–412. [PubMed] [Google Scholar]
- 22.Jung CW, Bahk JH, Lee JH, Lim YJ. The tenth rib line as a new landmark of the lumbar vertebral level during spinal block. Anaesthesia. 2004;59(4):359–363. doi: 10.1111/j.1365-2044.2004.03657.x. [DOI] [PubMed] [Google Scholar]
- 23.Kim JT, Bahk JH, Sung J. Influence of age and sex on the position of the conus medullaris and Tuffier’s line in adults. Anesthesiology. 2003;99(6):1359–1363. doi: 10.1097/00000542-200312000-00018. [DOI] [PubMed] [Google Scholar]
- 24.Lee AJ, Ranasinghe JS, Chehade JM, Arheart K, Saltzman BS, Penning DH, et al. Ultrasound assessment of the vertebral level of the intercristal line in pregnancy. Anesth Analg. 2011;113(3):559–564. doi: 10.1213/ANE.0b013e318222abe4. [DOI] [PubMed] [Google Scholar]
- 25.Lin N, Li Y, Bebawy JF, Dong J, Hua L. Abdominal circumference but not the degree of lumbar flexion affects the accuracy of lumbar interspace identification by Tuffier’s line palpation method: an observational study. BMC Anesthesiol. 2015;15:9. doi: 10.1186/1471-2253-15-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rahmani M, Vaziri Bozorg SM, Ghasemi Esfe AR, Morteza A, Khalilzadeh O, Pedarzadeh E, et al. Evaluating the reliability of anatomic landmarks in safe lumbar puncture using magnetic resonance imaging: does sex matter? Int J Biomed Imaging. 2011;2011:868632. doi: 10.1155/2011/868632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Margarido CB, Arzola C, Carvalho JCA. The intercristal line determined by palpation is not a reliable anatomical landmark for neuraxial anesthesia. Can J Anaesth. 2011;58(3):262–266. doi: 10.1007/s12630-010-9432-z. [DOI] [PubMed] [Google Scholar]
- 28.Borghi B, Tognu A, White PF, Paolini S, Van Oven H, Aurini L, et al. Soft tissue depression at the iliac crest prominence: a new landmark for identifying the L4–L5 interspace. Minerva Anestesiol. 2012;78(12):1348–1356. [PubMed] [Google Scholar]
- 29.Lakchayapakorn K, Suwanlikhid N. The interlaminar and the narrowest distances at the L3/4 and L4/5 interspinous spaces and location of the intercrestal line in Thai cadavers. J Med Assoc Thai. 2014;97(Suppl 8):S1–6. [PubMed] [Google Scholar]
- 30.Windisch G, Ulz H, Feigl G. Reliability of Tuffier’s line evaluated on cadaver specimens. Surg Radiol Anat. 2009;31(8):627–630. doi: 10.1007/s00276-009-0493-z. [DOI] [PubMed] [Google Scholar]
- 31.Ievins FA. Accuracy of placement of extradural needles in the L3–4 interspace: comparison of two methods of identifying L4. Br J Anaesth. 1991;66(3):381–382. doi: 10.1093/bja/66.3.381. [DOI] [PubMed] [Google Scholar]
- 32.Cooper K, Alexander L, Hancock E, Smith FW. The use of pMRI to validate the identification of palpated bony landmarks. Man Ther. 2013;18(4):289–293. doi: 10.1016/j.math.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 33.Kettani A, Tachinante R, Tazi A. Evaluation of the iliac crest as anatomic landmark for spinal anaesthesia in pregnant women. Ann Fr Anesth Reanim. 2006;25(5):501–504. doi: 10.1016/j.annfar.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 34.Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC medical research methodology. 2003;3:25. doi: 10.1186/1471-2288-3-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arrivé L, Renard R, Carrat F, Belkacem A, Dahan H, Le Hir P, et al. A scale of methodological quality for clinical studies of radiologic examinations. Radiology. 2000;217(1):69–74. doi: 10.1148/radiology.217.1.r00oc0669. [DOI] [PubMed] [Google Scholar]
- 36.Furness G, Reilly MP, Kuchi S. An evaluation of ultrasound imaging for identification of lumbar intervertebral level. Anaesthesia. 2002;57(3):277–280. doi: 10.1046/j.1365-2044.2002.2403_4.x. [DOI] [PubMed] [Google Scholar]
- 37.Sargin M. Radiological evaluation of the Tuffier’s Line in pediatric patients. J Clin Analyt Med. 2015:1–4. [Google Scholar]
- 38.Shiraishi N, Matsumura G. Establishing intercrestal line by posture:--a radiographic evaluation. Okajimas Folia Anat Jpn. 2006;82(4):139–416. doi: 10.2535/ofaj.82.139. [DOI] [PubMed] [Google Scholar]
- 39.Hayes J, Borges B, Armstrong D, Srinivasan I. Accuracy of manual palpation vs ultrasound for identifying the L3–L4 intervertebral space level in children. Paediatr Anaesth. 2014;24(5):510–515. doi: 10.1111/pan.12355. [DOI] [PubMed] [Google Scholar]
- 40.Baxter B, Evans J, Morris R, Ghafoor U, Nana M, Weldon T, et al. Neonatal lumbar puncture: are clinical landmarks accurate? Arch Dis Child Fetal Neonatal Ed. 2016;101(5):F448–450. doi: 10.1136/archdischild-2015-308894. [DOI] [PubMed] [Google Scholar]
- 41.Horsanalı BÖ, Tekgül ZT, Özkalkanlı MY, Adıbelli ZH, Esen ÖE, Durna FY. Radiological evaluation of the line between the crista iliaca (Tuffier’s line) in elderly patients. 2015;43:149–153. doi: 10.5152/TJAR.2015.35761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tame SJ, Burstal R. Investigation of the radiological relationship between iliac crests, conus medullaris and vertebral level in children. Paediatr Anaesth. 2003;13(8):676–680. doi: 10.1046/j.1460-9592.2003.01120.x. [DOI] [PubMed] [Google Scholar]
- 43.Hubley-Kozey C, Wall J, Hogan D. Effects of a general exercise program on plantarflexor and dorsiflexor strength and power of older women. Top Geriatr Rehabil. 1995;10(3):45–60. [Google Scholar]
- 44.McGaugh JM, Brismee JM, Dedrick GS, Jones EA, Sizer PS. Comparing the anatomical consistency of the posterior superior iliac spine to the iliac crest as reference landmarks for the lumbopelvic spine: a retrospective radiological study. Clin Anat. 2007;20(7):819–825. doi: 10.1002/ca.20531. [DOI] [PubMed] [Google Scholar]
- 45.Kim SH, Kim DY, Han JI, Baik HJ, Park HS, Lee GY, et al. Vertebral level of Tuffier’s line measured by ultrasonography in parturients in the lateral decubitus position. Korean J Anesthesiol. 2014;67(3):181–185. doi: 10.4097/kjae.2014.67.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol. 1996;143(3):228–239. doi: 10.1093/oxfordjournals.aje.a008733. [DOI] [PubMed] [Google Scholar]
- 47.Ohtsuka K, Kiyono S, Takimoto M. A potential hazard of spinal cord injury by spinal and epidural anesthesia in a patient with low-placed conus medullaris (author’s transl) Masui. 1977;26(9):967–979. [PubMed] [Google Scholar]
- 48.Saifuddin A, Burnett SJ, White J. The variation of position of the conus medullaris in an adult population. A magnetic resonance imaging study. Spine. 1998;23(13):1452–1456. doi: 10.1097/00007632-199807010-00005. [DOI] [PubMed] [Google Scholar]
- 49.Cooperstein R, Young M. Mapping intended spinal site of care from the upright to prone position: an interexaminer reliability study. Chiropr Man Therap. 2014;22:20. doi: 10.1186/2045-709X-22-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cooperstein R, Haneline M. Spinous process palpation using the scapular tip as a landmark vs a radiographic criterion standard. J Chiropr Med. 2007;6(3):87–93. doi: 10.1016/j.jcme.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cooperstein R, Haneline M, Young M. The location of the inferior angle of the scapula in relation to the spine in the upright position: a systematic review of the literature and meta-analysis. Chiropr Man Therap. 2015;23:7. doi: 10.1186/s12998-014-0050-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cooperstein R, Haneline MT, Young MD. The location of the inferior angle of the scapula in relation to the spinal level of prone patients. J Can Chiropr Assoc. 2009;53(2):121–128. [PMC free article] [PubMed] [Google Scholar]
- 53.Haneline M, Cooperstein R, Young M, Ross J. Determining spinal level using the inferior angle of the scapula as a reference landmark: a retrospective analysis of 50 radiographs. J Can Chiropr Assoc. 2008;52(1):24–29. [PMC free article] [PubMed] [Google Scholar]