Abstract
Objective
To evaluate a model of care to improve arthritis detection and treatment in an urban Aboriginal population.
Design
Cohort study.
Setting
The Elbow River Healing Lodge in Calgary, Alta.
Participants
A total of 26 participants with noninflammatory arthritis and 12 with inflammatory arthritis.
Intervention
A monthly rheumatology clinic was embedded in the primary health care service and received referrals from primary care providers and allied health care professionals, or self-referrals. All participants had a standardized assessment to determine their diagnosis. Those with noninflammatory musculoskeletal conditions were returned to primary care management and those with inflammatory arthritis conditions were followed by the rheumatologist.
Main outcome measures
Accessibility, acceptability, effectiveness, and cultural safety were evaluated as measures of quality for the model of care.
Results
Nearly all participants (87%) thought the services were very easy or easy to obtain, and overall satisfaction with the model of care was high (89% were very satisfied or satisfied). For inflammatory arthritis patients, the swollen and tender joint counts improved over time (both P < .01) and patient safety was assured. A high degree of cultural safety was provided, with 95% of participants responding that they did not perceive discrimination on the basis of race.
Conclusion
This model of care facilitated access for diagnosis and return to care of inflammatory arthritis conditions, and was acceptable to participants. This model of care removes the complexities of access to non–family physician specialty care while providing health care in a setting valued by Aboriginal patients.
Résumé
Objectif
Évaluer l’efficacité d’un modèle de soins visant à améliorer le diagnostic et le traitement de l’arthrite chez un groupe d’Autochtones d’un milieu urbain.
Type d’étude
Une étude de cohorte.
Contexte
Elbow River Healing Lodge, à Calgary.
Participants
Un total de 26 cas d’arthrite non inflammatoire et de 12 autres cas d’arthrite inflammatoire.
Intervention
On a instauré une clinique mensuelle de rhumatologie dans le service de soins de première ligne; les demandes de consultation provenaient des soignants de première ligne, de professionnels de la santé associés ou des patients eux-mêmes. Les participants subissaient tous une évaluation standard pour établir le diagnostic. Ceux qui souffraient d’arthrite musculosquelettique non inflammatoire étaient redirigés vers les soignants de première ligne, tandis que ceux qui souffraient d’arthrite inflammatoire étaient pris en charge par le rhumatologue.
Principaux paramètres à l’étude
L’accessibilité, l’acceptabilité, l’efficacité et le respect des valeurs culturelles ont été évalués afin de déterminer la qualité de ce type d’intervention.
Résultats
Presque tous les participants (87 %) estimaient qu’il était facile ou très facile d’accéder à ce service, et 89 % étaient satisfaits ou très satisfaits de cette innovation. Chez ceux souffrant d’arthrite inflammatoire, les douleurs et les gonflements articulaires ont régressé progressivement (P < .01), assurant ainsi plus de sécurité au patient. L’intervention procurait un très bon niveau de respect des valeurs culturelles, 95 % des participants déclarant qu’ils n’avaient constaté aucune discrimination en rapport avec leur race.
Conclusion
Ce type d’intervention a permis aux patients souffrant d’arthrite inflammatoire d’obtenir plus facilement un diagnostic et un traitement de leur condition, et il était acceptable pour ces patients. Grâce à un tel modèle de soins, les Autochones pouvaient enfin avoir accès à des spécialistes autres que des médecins de famille, et ce, dans un contexte qui leur convenait.
Epidemiology and clinical research studies confirm an increased prevalence of osteoarthritis1,2 and inflammatory arthritis conditions1,3,4 in the Aboriginal populations of Canada (First Nations, Metis, and Inuit) compared with the general population. These conditions are characterized as being more severe in phenotype among Aboriginal patients4,5 and have higher mortality in this group.6 Timely access to diagnosis and initiation of disease-modifying therapy minimizes function loss,7 and reaching remission or low-disease-activity treatment targets helps to maintain work productivity and to avoid developing comorbidities.8 Access to rheumatology specialist services is critical for outcomes, yet Aboriginal patients face multiple system barriers to acquiring and sustaining acceptable services for arthritis management.9 These barriers include racism encountered in the health care setting, professional expectations of patients, and constraints imposed by complex health care systems that are not fully integrated at the municipal, provincial, and federal levels.9
An increasing proportion of Aboriginal people reside in urban locations. They experience disparities in health determinants, such as housing, income, and access to services, compared with the on-reserve population.10,11 A report by the Health Council of Canada highlights that mainstream health care services are alienating and intimidating owing to racism and stereotyping, leading to mistrust.12 Specialists might place emphasis on technological and biomedical solutions and neglect management of complex social situations.13
Multidisciplinary urban Aboriginal health care centres play an essential role in assisting patients with navigating complex networks of health and social services, with service delivery based on Indigenous approaches to health and healing.14 These centres provide culturally safe care, which is integral to high-quality services that address the social and cultural needs of Aboriginal patients. In designing a model of care that facilitates access to early arthritis detection and effective management of resources for the urban Aboriginal population, embedding rheumatology specialist services in the primary health care setting was tested in the domains of accessibility, acceptability, effectiveness, and cultural safety.
METHODS
Study design, sample, and intervention
Between January and July 2014, patients of the Elbow River Healing Lodge in Calgary, Alta, who were attending urban Aboriginal organizations (Calgary Urban Project Society, Metis Calgary Family Services Society, Native Network Parent Link Centre, or the Aboriginal mental health program of Alberta Health Services) were invited to participate in a model-of-care study for arthritis diagnosis and management. Primary care physicians, nurses, dietitians, and other medical professionals at the Elbow River Healing Lodge identified patients attending appointments with primary health service providers who might also benefit from focused musculoskeletal disease assessment. Participants could also self-refer, and were invited to arrange prespecified appointments or to drop in during the weekly screening clinics at their preference. Participants were followed up to July 2015.
Clinical assessments and management
A rheumatologist (C.B.) funded under an alternative relationship plan obtained musculoskeletal and medical histories for each participant, performed a physical examination, and reviewed any previous investigations pertinent to the presenting symptoms. Additional investigations were requested as necessary to confirm a diagnosis, and patients were classified using validated criteria. Participants found to have noninflammatory conditions were returned to primary care management after a discussion about self-management strategies and additional strategies to pursue if symptoms did not improve with the proposed strategies. Standardized data collection for participants with noninflammatory musculoskeletal conditions included basic demographic information (age, sex, height, weight), Health Assessment Questionnaire (HAQ) score,15 and visual analogue scale scores for patient global evaluation, fatigue, pain, and sleep. Participants with inflammatory arthritis conditions were initiated on appropriate disease-modifying therapy and were followed at intervals for measures of disease activity and medication requirements. In addition to the standardized measures recorded for patients with non-inflammatory conditions, the patients with inflammatory arthritis also had physical examination findings (tender and swollen joint counts, extra-articular manifestations), serology and inflammatory markers, treatment recommendations, and pharmacotherapy use recorded.
Questionnaires
Before the initial clinical assessment, participants completed a questionnaire about strategies for symptom management they had used at any time before the clinic visit and the perceived effectiveness of each strategy. Effectiveness was scored on a 5-point ordinal scale (−1 = worse, 0 = no effect, 1 = minimal effect, 2 = moderate effect, and 3 = good effect). After the clinical assessment, accessibility and acceptability of the model of care were measured with questions adapted from 3 sources: the Health Quality Council of Alberta Satisfaction and Experience with Healthcare Services Survey,16,17 the Measuring Patient Experiences in Primary Health Care Survey,18 and the Interpersonal Processes of Care Survey.19 For accessibility evaluation, questions exploring patients’ past experiences with non–family physician specialist care were used to contextualize patient experiences at the clinic, with specific questions about perceived and experienced accessibility for the study model of care asked and scored on a 5-point scale ranging from very easy to very difficult. General satisfaction with the care provided at the clinic was used to explore acceptability. Other domains for acceptability were drawn from the Measuring Patient Experiences in Primary Health Care Survey18 and Interpersonal Processes of Care Survey,19 including interpersonal communications (general communication and clarity, respectfulness, elicitation of concerns and responding to concerns, explaining results and medications, shared decision making, interpersonal style) and perceptions of health professional coordination to explore the effect of embedding the clinic within a primary health services setting. Effectiveness was evaluated by changes in clinical disease activity measures and patient-reported outcomes over 1 year of follow-up and patient-reported effects of care (patient safety) from the Measuring Patient Experiences in Primary Health Care Survey.18 Cultural safety assessment was done using questions from the Interpersonal Processes of Care Survey,19 which evaluates cultural sensitivity and perceived discrimination.
Analysis
Descriptive statistics were used to summarize the frequency of use of different symptom management strategies, with the most common response (mode) for effectiveness reported. Means and SDs of disease activity measures and patient-reported outcomes were calculated for noninflammatory and inflammatory arthritis condition groups. Longitudinal changes in measures of disease activity over 12 months of follow-up for inflammatory arthritis patients were assessed using repeated-measures ANOVA (analysis of variance), with between-subject and within-subject effects, to take into account the lack of compound symmetry and computing conservative P values for F tests. All statistics were computed using Stata 11.2.
Ethics and community engagement
In keeping with the Tri-Council Policy Statement on Research Involving the First Nations, Inuit and Métis Peoples of Canada, representatives from the Elbow River Healing Lodge and the Indigenous Health Program (Alberta Health Services) were involved in all aspects of funding applications, study design, conduct, and interpretation of results. A formal research agreement with the Elbow River Healing Lodge defined the roles and responsibilities of the researchers and clinical partners in this project. In addition, an opening ceremony and project blessing was given by 7 Elders from the Treaty 7 Region. Participants provided prior and informed individual consent. The University of Calgary Conjoint Health Research Ethics Board approved the research project.
RESULTS
Study population
During the 7-month recruitment period, 38 patients (84% of 45 individuals seen) provided informed consent to participate in the longitudinal study, of whom 79% were female with a mean age of 49 years. Eight patients volunteered for the study after reading recruitment posters, 18 were made aware of the study by friends or family members, and 12 were referred by an Elbow River Healing Lodge staff member.
Symptom management before clinic visit
Common methods of symptom management before the rheumatologist visit and perceived effectiveness are summarized in Table 1. Symptom management strategies included primary care consultation (79%), discussion with family members or friends (71%), or acetaminophen (63%). More than half of the participants had also tried lifestyle changes (55%), nonsteroidal anti-inflammatory drugs (NSAIDs) (53%), or non-NSAID topical therapies (53%). Most strategies were rated as having a good effect, although notably use of walk-in clinics, emergency departments, urgent care services, and non-NSAID topical therapy were consistently reported to have minimal effect.
Table 1.
Frequency of use and effectiveness score of symptom management strategies: Only strategies used by > 5% of participants are reported.
| STRATEGIES | FREQUENCY OF USE, % | MODE FOR EFFECTIVENESS SCORE* |
|---|---|---|
| Physicians | ||
| • Primary care | 79 | 3 |
| • Walk-in clinic | 26 | 1 |
| • Non–family physician specialist | 29 | 3 |
| • Emergency department | 18 | 1 |
| • Urgent care | 8 | 1 |
| Allied health practitioners | ||
| • Pharmacist | 40 | 2 |
| • Nurse | 24 | 0, 2 |
| • Physiotherapist | 21 | 3 |
| • Chiropractor | 16 | 3 |
| • Acupuncturist | 16 | 3 |
| • Massage therapist | 13 | 3 |
| Support network | ||
| • Family or friend | 71 | 3 |
| • Healer | 11 | 3 |
| • Church or clergy | 8 | 1 |
| Pharmacotherapy | ||
| • Acetaminophen | 63 | 1, 3 |
| • NSAIDs | 53 | 1, 3 |
| • Acetaminophen-codeine | 45 | 3 |
| • Herbal therapy | 34 | 0 |
| • Traditional medicine | 21 | 3 |
| • Joint or soft tissue injection | 18 | 3 |
| • Narcotics | 16 | 3 |
| • Corticosteroids | 8 | 3 |
| Topical therapy | ||
| • Non-NSAID | 53 | 1 |
| • NSAID | 29 | 1, 3 |
| Conservative therapy | ||
| • Lifestyle changes | 55 | 2 |
| • Bracing | 24 | 2, 3 |
| • Walking aids | 21 | 1, 2 |
NSAID—nonsteroidal anti-inflammatory drug.
Effectiveness was scored on a 5-point ordinal scale (−1 = worse, 0 = no effect, 1 = minimal effect, 2 = moderate effect, and 3 = good effect).
Diagnoses, severity, and management
Noninflammatory musculoskeletal conditions (n = 26) and inflammatory arthritis conditions (n = 12) diagnosed and classified in the study participants are summarized in Table 2. The participants with inflammatory arthritis conditions included those with established diagnoses returning to active care (n = 5) and those with a new diagnosis (n = 7). Mean scores for disease activity measures, HAQ scores, and patient-reported outcomes by type of condition are summarized in Table 3. Treatment recommendations for participants with noninflammatory musculoskeletal conditions included exercise (62%), physical adaptations (46%), and weight loss (12%), with 27% referred to a physiotherapist, 15% referred to a physical medicine and rehabilitation or orthopedic specialist, and 8% referred to an allied health specialist. Additional investigations were requested for 31% of participants, 54% received prescriptions for topical or oral analgesia, and 31% had a joint or soft tissue injection. For participants with inflammatory arthritis, during the course of follow-up, therapy use included methotrexate (22%), hydroxychloroquine (38%), sulfasalazine (22%), azathioprine (5%), and leflunomide (5%), and 27% of patients treated with disease-modifying antirheumatic drugs received some of these as combination therapy. Biologics and continuous oral prednisone were each used by 14% of participants.
Table 2.
Diagnoses in study participants
| DIAGNOSES | NO. OF PARTICIPANTS WITH DIAGNOSIS (N = 38) * |
|---|---|
| Noninflammatory conditions | 26* |
| • Osteoarthritis | 14 |
| • Rotator cuff tendinopathy or subacromial bursitis | 10 |
| • Patellofemoral pain syndrome | 7 |
| • Mechanical or degenerative back pain | 6 |
| • Joint injury | 4 |
| • Arthralgias | 1 |
| • Myalgias, myofascial pain, or fibromyalgia | 5 |
| Inflammatory arthritis conditions | 12 |
| • Rheumatoid arthritis | 8 |
| • Psoriatic arthritis | 2 |
| • Systemic autoimmune rheumatic disease† | 2 |
Some participants had multiple diagnoses.
Includes systemic lupus erythematosus, Sjögren syndrome, and scleroderma.
Table 3.
Disease activity measures and patient-reported outcomes: All reported as mean (SD). Pain, fatigue, sleep, and patient global evaluation were scored on a 0- to 10-cm visual analogue scale.
| MEASURES AND OUTCOMES | NONINFLAMMATORY MUSCULOSKELETAL DIAGNOSIS (N = 26) | NEW INFLAMMATORY ARTHRITIS DIAGNOSIS (N = 7) | ESTABLISHED INFLAMMATORY ARTHRITIS DIAGNOSIS (N = 5) |
|---|---|---|---|
| Health Assessment Questionnaire* | 1.18 (0.64) | 1.45 (0.85) | 1.22 (0.66) |
| Pain | 7.5 (2.4) | 7.1 (2.0) | 6.0 (1.7) |
| Fatigue | 7.5 (2.2) | 6.3 (2.9) | 6.6 (1.5) |
| Sleep | 8.2 (1.9) | 7.9 (2.2) | 7.0 (1.2) |
| Patient global evaluation | 9.2 (8.8) | 6.3 (3.0) | 7.0 (1.6) |
| Disease Activity Score 28† | NA | 5.09 (1.76) | 4.35 (1.34) |
| Erythrocyte sedimentation rate, mm/h | NA | 23.2 (11.7) | 21.8 (10.2) |
| Stiffness, min | NA | 52 (39) | 88 (97) |
NA—not applicable.
The Health Assessment Questionnaire overall score can range from 0 (no disability) to 3 (completely disabled).
A Disease Activity Score of greater than 5.1 implies active disease, less than 3.2 low disease activity, and less than 2.6 remission.
Evaluation of the model of care
Accessibility.
Before the clinical evaluation, 29% of participants (11 of 38) had been to see a non–family physician specialist for arthritis or another joint condition (50% of those with an inflammatory diagnosis and 19% with a noninflammatory diagnosis). Difficulties with accessing a non–family physician specialist were reported by 42% (16 of 38), with some participants having more than 1 listed issue, including difficulty getting the primary care physician to make a referral (n = 9), difficulty getting an appointment with the non–family physician specialist once referred (n = 4), having a lack of non–family physician specialists in the geographic area (n = 5), having to wait too long to see the non–family physician specialist from the time of referral (n = 6), and appointments being canceled or deferred by the physician’s office (n = 2). Once a non–family physician specialist appointment was secured, participants reported having to wait too long in the specialist’s office on the day of the consultation (n = 2), transportation problems (n = 4), or language problems (n = 1); 1 participant decided not to attend owing to fear of diagnosis and procedures at the visit. With regard to the Elbow River Healing Lodge clinic specifically, only 55% (21 of 38) believed it would be easy or very easy to access arthritis specialist services at the clinic, but that percentage increased to 87% (33 of 38) after their experience with the model of care.
Acceptability.
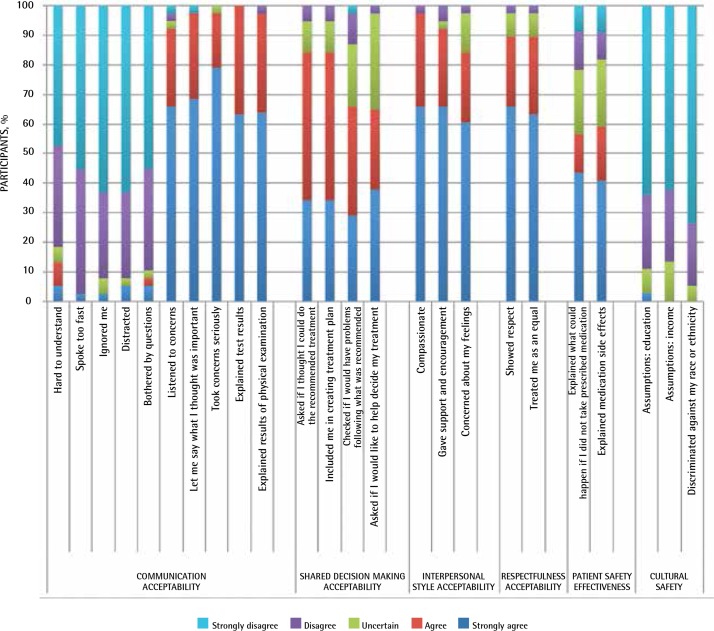
Participants were asked about their overall satisfaction with the arthritis model of care, and 89% (34 of 38) reported they were satisfied (11%) or very satisfied (79%). Coordination of services by health care professionals in the clinic was highly rated (63% excellent and 26% very good). Measures of communication acceptability included patients believing that their health concerns were taken very seriously (79% strongly agreed and 18% agreed) and results of the examination and investigations being explained to all participants. Most participants perceived being supported and encouraged by the physician (66% strongly agreed and 26% agreed). A shared decision-making approach was perceived by most, with 84% (32 of 38) reporting that a treatment plan was worked out in collaboration with the physician. Most also reported perceiving respect (66% strongly agreed and 24% agreed) and being treated as an equal (63% strongly agreed and 26% agreed). Responses to additional domains of acceptability surveyed are reported in Figure 1.
Figure 1.
Patient satisfaction and cultural safety evaluation
Effectiveness.
Patients with inflammatory arthritis had significant reductions in tender joint count (68 joints, repeated-measures ANOVA, F26,39 = 2.51, P = .0045) and swollen joint count (66 joints, repeated-measures ANOVA, F26,39 = 2.84, P = .0016) during the year after diagnosis. However, improvements in the HAQ score, patient global evaluation score, and pain levels were not significant. For measures of patient safety, of 23 participants with whom treatments were discussed, 13 (57%) either strongly agreed or agreed that they were informed of what could happen if medications were not taken and 13 of 22 (59%) were told of the side effects they might experience from the medication (Figure 1).
Cultural safety.
Nearly all participants (95%) disagreed (21%) or strongly disagreed (74%) that they felt discriminated against because of race or ethnicity (Figure 1). They also did not perceive that assumptions were made about their level of education or income, or that less attention was paid to them based on race or ethnicity (24% disagreed and 68% strongly disagreed).
DISCUSSION
Optimal treatment of arthritis is associated with access to rheumatology specialty care.20 It is not surprising to see evidence that facilitating access to an integrated arthritis model of care in Aboriginal communities yields positive outcomes. Service was perceived to be accessible by nearly all participants and resulted in confirming diagnoses and initiating appropriate care plans. Overall acceptability and individual measures of acceptability in domains of communication, shared decision making, interpersonal style, and respectfulness were rated highly. Coordination of care by team members was similarly well rated, as was evaluation of patient safety measures and the cultural safety of the clinic environment. The tested model of care resides within a biomedical health model, which is not always a good fit in an Aboriginal context; however, this model appeared to positively resonate with the Aboriginal patients participating in the study. This might in part be owing to the uncomplicated pathways to diagnosis and care in an environment that respects patients’ experiences, as was proposed as a solution to the traditional care paradigms that create barriers to care for Aboriginal patients.9
A systematic review on outreach interventions in primary care and rural hospital settings found that non– family physician specialist outreach models improve access, outcomes, and service use.21 From a simplistic viewpoint, our model of care had positive outcomes similar to those of surgical specialty outreach services to remote Aboriginal populations compared with a hospital-based consultation model.22 Our study’s urban-based Aboriginal population, while not a remote population, nonetheless experiences rheumatology access barriers9 that strongly influence arthritis outcomes. The distinguishing features of this study’s intervention model include more direct access to the rheumatology provider (facilitated access) and the integration of the service within an Aboriginal-focused primary health care centre. Although health care team perceptions of the model of care and evaluation of the effect of the interdisciplinary team were not outcomes measured in this pilot study, theoretically, coordinating care plans between non–family physician specialists and primary care providers would improve integration of care plans to benefit system efficiency and clinical outcomes.
One might argue that many of the reported outcomes are linked to the provider’s approach, rather than the nature of the facilitated access model. Individuals who favour that perspective would opine that the Aboriginal patient outcomes of the provider’s service approach should be consistent in an urban Aboriginal primary health service and in a tertiary heath service location. Admittedly, our results are influenced by the nature of existing validated tools and we recognize the need for further research to untangle the effect of the service context including location, provider relationships, resources, and the organization. We are also pursuing more formal assessment around communication of medication risks and benefits to enhance shared decision making. Nonetheless, patient care experience and perception of quality of care are linked to the service environment.23
This research conducted at the Elbow River Healing Lodge is a successful case study in how a decolonizing space that recognizes, respects, and nurtures the unique identities of Aboriginal Canadians in its daily practice can benefit health outcomes. These elements nurture cultural safety and bring focus to the specific needs of the population. The embedded specialist model of care is effective in this environment; however, more research is needed to explore the environmental effect and determine its applicability in other primary care settings and in other chronic diseases. Sustainability in models of care is also an important aspect to consider, especially in rheumatology, where a mismatch between supply and demand for service and the longstanding relationship between providers and patients with chronic disease eventually reduces capacity for seeing new patients within a practice or service area. However, bringing this type of advanced, specialized arthritis care into a setting that practises medicine with cultural safety inherent in the model is an excellent strategy for overcoming structural barriers to care for a population with such a high burden of disease.
Limitations
These findings are preliminary and only reveal the short-term effect of the intervention in a voluntary cohort of participants. Evaluation of the model has been from a biomedical perspective and could be improved by incorporating patient-valued domains and outcomes, and considering other aspects of quality such as efficiency and appropriateness.
Conclusion
We present a proposal for how to meet arthritis care needs in an urban Aboriginal population, and an opportunity to build on this model to ensure the health care system meets the needs of a population that continues to face inequities in health. The model of care facilitated access for diagnosis and return to care of patients with inflammatory arthritis conditions, and was acceptable to participants. This model of care removes the complexities of access to specialty care while providing health care in a setting valued by Aboriginal patients.
Acknowledgments
This research was funded by a Models of Care Catalyst Grant from The Arthritis Society.
EDITOR’S KEY POINTS
The Elbow River Healing Lodge in Calgary, Alta, is a primary care health service designed to provide comprehensive and culturally safe care to urban Aboriginal populations. The model of care in this study embedded a rheumatologist to facilitate access for diagnosis and return to care of patients with inflammatory arthritis conditions.
Service was perceived to be accessible by nearly all participants and resulted in confirming diagnoses and initiating appropriate care plans. Overall acceptability and individual measures of acceptability in domains of communication, shared decision making, interpersonal style, and respectfulness were rated highly. Coordination of care by team members was similarly well rated, as was evaluation of patient safety measures and the cultural safety of the clinic environment.
The tested model of care resides within a biomedical health model, which is not always a good fit in an Aboriginal context; however, this model appeared to positively resonate with the Aboriginal patients participating in the study. This might in part be owing to the uncomplicated pathways to diagnosis and care in an environment that respects patients’ experiences.
POINTS DE REPÈRE DU RÉDACTEUR
Elbow River Healing Lodge, à Calgary, est un service de soins de première ligne qui offre à des Autochtones des soins de santé complets, respectueux de leur culture. Dans cette étude, on voulait permettre à des patients souffrant d’arthrite inflammatoire d’avoir un meilleur accès à un rhumatologue.
Presque tous les participants estimaient que ce service était accessible, et qu’il permettait d’établir le diagnostic et d’amorcer le traitement approprié. Ils attribuaient une cote élevée à son accessibilité générale et individuelle dans les domaines de la communication, de la prise de décisions partagées, des relations interpersonnelles et du respect des valeurs. On attribuait également une bonne cote à la coordination des soins dispensés par l’équipe de soignants de la clinique ainsi qu’à la sécurité et au respect de la culture.
Le modèle de soins évalué dans cette étude s’insère dans un modèle d’ordre biomédical, ce qui n’est pas toujours idéal dans un contexte autochtone; il semble toutefois avoir été bien accepté par les Autochtones qui participaient à l’étude. Cela pourrait être dû en partie au fait qu’il était facilement accessible.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
Drs Barnabe and Crowshoe designed the study and Drs Erasmus and Barnabe were responsible for data collection. Drs Lockerbie and Barnabe performed the analysis. All authors contributed to the interpretation of the results, drafting the manuscript, and approving the version for submission.
Competing interests
None declared
References
- 1.Barnabe C, Elias B, Bartlett J, Roos L, Peschken C. Arthritis in Aboriginal Manitobans: evidence for a high burden of disease. J Rheumatol. 2008;35(6):1145–50. Epub 2008 Apr 15. [PubMed] [Google Scholar]
- 2.Barnabe C, Hemmelgarn B, Jones CA, Peschken CA, Voaklander D, Joseph L, et al. Imbalance of prevalence and specialty care for osteoarthritis for First Nations people in Alberta, Canada. J Rheumatol. 2015;42(2):323–8. doi: 10.3899/jrheum.140551. Epub 2014 Nov 29. [DOI] [PubMed] [Google Scholar]
- 3.Barnabe C, Joseph L, Belisle P, Labrecque J, Edworthy S, Barr SG, et al. Prevalence of systemic lupus erythematosus and systemic sclerosis in the First Nations population of Alberta, Canada. Arthritis Care Res (Hoboken) 2012;64(1):138–43. doi: 10.1002/acr.20656. [DOI] [PubMed] [Google Scholar]
- 4.Peschken CA, Esdaile JM. Systemic lupus erythematosus in North American Indians: a population based study. J Rheumatol. 2000;27(8):1884–91. [PubMed] [Google Scholar]
- 5.Peschken CA, Hitchon CA, Robinson DB, Smolik I, Barnabe CR, Prematilake S, et al. Rheumatoid arthritis in a North American Native population: longitudinal followup and comparison with a white population. J Rheumatol. 2010;37(8):1589–95. doi: 10.3899/jrheum.091452. [DOI] [PubMed] [Google Scholar]
- 6.Peschken CA, Puar R, Hitchon CA. High mortality in North American Natives with systemic lupus erythematosus. Arthritis Res Ther. 2014;16(Suppl 1):A41. [Google Scholar]
- 7.Van der Linden MP, le Cessie S, Raza K, van der Woude D, Knevel R, Huizinga TW, et al. Long-term impact of delay in assessment of patients with early arthritis. Arthritis Rheum. 2010;62(12):3537–46. doi: 10.1002/art.27692. [DOI] [PubMed] [Google Scholar]
- 8.Stoffer MA, Schoels MM, Smolen JS, Aletaha D, Breedveld FC, Burmester G, et al. Evidence for treating rheumatoid arthritis to target: results of a systematic literature search update. Ann Rheum Dis. 2016;75(1):16–22. doi: 10.1136/annrheumdis-2015-207526. Erratum in: Ann Rheum Dis 2016;75(5):946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thurston WE, Coupal S, Jones CA, Crowshoe LF, Marshall DA, Homik J, et al. Discordant Indigenous and provider frames explain challenges in improving access to arthritis care: a qualitative study using constructivist grounded theory. Int J Equity Health. 2014;13(1):46. doi: 10.1186/1475-9276-13-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Firestone M, Smylie J, Maracle S, Spiller M, O’Campo P. Unmasking health determinants and health outcomes for urban First Nations using respondent-driven sampling. BMJ Open. 2014;4(7):e004978. doi: 10.1136/bmjopen-2014-004978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ontario Federation of Indian Friendship Centres, Ontario Métis Aboriginal Association, Ontario Native Women’s Association . Urban Aboriginal Task Force final report. Toronto, ON: Ontario Federation of Indian Friendship Centres, Ontario Métis Aboriginal Association, Ontario Native Women’s Association; 2007. [Google Scholar]
- 12.Health Council of Canada . Empathy, dignity and respect. Creating cultural safety for Aboriginal people in urban health care. Ottawa, ON: Health Council of Canada; 2012. [Google Scholar]
- 13.McDonald HL. Arthritis, aches and pains, and arthritis services: experiences from within an urban First Nations community. Vancouver, BC: University of British Columbia; 2011. [Google Scholar]
- 14.Browne AJ, McDonald H, Elliott D. Urban First Nations health research discussion paper. A report for the First Nations Centre, National Aboriginal Health Organization. Ottawa, ON: National Aboriginal Health Organization; 2009. [Google Scholar]
- 15.Bruce B, Fries JF. The Health Assessment Questionnaire (HAQ) Clin Exp Rheumatol. 2005;23(5 Suppl 39):S14–8. [PubMed] [Google Scholar]
- 16.Health Quality Council of Alberta . Alberta Quality Matrix for Health user guide. Calgary, AB: Health Quality Council of Alberta; 2005. [Google Scholar]
- 17.Health Quality Council of Alberta . Satisfaction and experience with healthcare services: a survey of Albertans 2012. Calgary, AB: Health Quality Council of Alberta; 2013. Available from: http://hqca.ca/surveys/satisfaction-experience-with-healthcare-services/2012/. Accessed 2017 Jul 25. [Google Scholar]
- 18.Wong ST, Haggerty J. Measuring patient experiences in primary health care. A review and classification of items and scales used in publicly-available questionnaires. Vancouver, BC: University of British Columbia; 2013. [Google Scholar]
- 19.Stewart AL, Nápoles-Springer AM, Gregorich SE, Santoyo-Olsson J. Interpersonal processes of care survey: patient-reported measures for diverse groups. Health Serv Res. 2007;42(3 Pt 1):1235–56. doi: 10.1111/j.1475-6773.2006.00637.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nell-Duxneuner V, Rezende LS, Stamm TA, Duer M, Smolen JS, Machold KP. Attending and non-attending patients in a real-life setting of an early arthritis clinic: why do people leave clinics and where do they go? Clin Exp Rheumatol. 2012;30(2):184–90. Epub 2012 Apr 13. [PubMed] [Google Scholar]
- 21.Gruen RL, Weeramanthri TS, Knight SS, Bailie RS. Specialist outreach clinics in primary care and rural hospital settings. Cochrane Database Syst Rev. 2003;(4):CD003798. doi: 10.1002/14651858.CD003798.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gruen RL, Bailie RS, d’Abbs PH, O’Rourke IC, O’Brien MM, Verma N. Improving access to specialist care for remote Aboriginal communities: evaluation of a specialist outreach service. Med J Aust. 2001;174(10):507–11. doi: 10.5694/j.1326-5377.2001.tb143400.x. [DOI] [PubMed] [Google Scholar]
- 23.Mohammed K, Nolan MB, Rajjo T, Shah ND, Prokop LJ, Varkey P, et al. Creating a patient-centered health care delivery system: a systematic review of health care quality from the patient perspective. Am J Med Qual. 2016;31(1):12–21. doi: 10.1177/1062860614545124. [DOI] [PubMed] [Google Scholar]