Abstract
Objective
To suggest a functional definition for identification of “high-frequency” emergency department (ED) users in rural areas.
Design
Retrospective analysis of secondary data.
Setting
Sioux Lookout Meno Ya Win Health Centre in northwestern Ontario.
Participants
All ED visitors (N = 7121) in 2014 (N = 17 911 visits) in one rural hospital.
Main outcome measures
The number of patients and visits identified using different definitions of high-frequency use.
Results
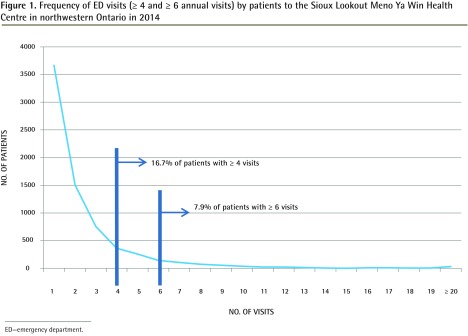
By using the most common definition of high-frequency use (≥ 4 annual visits) for our hospital data, we identified 16.7% of ED patients. Using 6 or more annual visits as the definition, we identified 7.9% of ED patients; these patients accounted for 31.3% of the ED visit workload. Using the definition of 6 or more identifies less than 10% of the patients, which is a similar result to using the lower visit standard (≥ 4) in urban centres.
Conclusion
We suggest that the definition for high-frequency visitors to a rural ED should be 6 or more annual visits. Other useful subsets might include very high-frequency users (12 to 19 annual visits) and super users (≥ 20 annual visits).
Résumé
Objectif
Proposer une définition fonctionnelle pour identifier les utilisateurs à « fréquence élevée » des services d’urgence dans les régions rurales.
Conception
Une analyse rétrospective de données secondaires.
Contexte
Le Centre de santé Sioux Lookout Meno Ya Win, dans le nord-ouest de l’Ontario.
Participants
Tous les visiteurs à l’urgence (N = 7121) en 2014 (N = 17 911 visites totales) dans un hôpital rural.
Principaux paramètres à l’étude
Le nombre de patients et de visites déterminé à l’aide de différentes définitions d’utilisation à fréquence élevée.
Résultats
En appliquant la définition la plus courante de l’expression utilisation à fréquence élevée (≥ 4 visites annuelles) aux données de notre hôpital, nous avons identifié 16,7 % des patients à l’urgence. En nous servant de 6 visites annuelles ou plus comme définition, nous avons identifié 7,9 % des patients à l’urgence; ces patients représentaient 31,3 % de la charge de travail. En utilisant la définition de 6 visites ou plus, nous avons cerné moins de 10 % des patients, ce qui est un résultat semblable à celui obtenu avec un seuil inférieur (≥ 4 visites) dans les centres urbains.
Conclusion
Nous proposons que la définition des visiteurs à fréquence élevée dans une urgence rurale se situe à 6 visites annuelles ou plus. D’autres sous-groupes utiles à cerner pourraient inclure les utilisateurs à très grande fréquence (12 à 19 visites annuelles) et les super utilisateurs (≥ 20 visites annuelles).
Analyses of emergency department (ED) use have always acknowledged patients who use the service more often than the norm.1–3 Certainly, front-line ED physicians and nurses are very familiar with these patients. Despite the regularity of discussing high-frequency ED users, there is no consistent definition.4 Agreeing on a broadly applicable definition of high-frequency use is important. In this study, we will examine common definitions in the literature, see how they might apply in one rural ED in northwestern Ontario, and suggest a rural standard.
Rural service environments are unique
In 1997 in Ontario, the number of ED visits per capita was 33 per 100 population.5 Ten years later, it had increased to 42 per 100 population.6 Rural figures differ: in an emergency-use analysis of 5 rural Huron County EDs in 2000, the rate of use was 89 per 100 population.7 Although these figures do not account for the influx of summer-only populations to this area, it does highlight a heavier reliance on rural EDs.
Rural ED environments differ from urban centres in both context and complement. In a rural setting the same group of general practitioners who provide primary care during office hours also attend the ED after hours. They might, for convenience, have some patients “schedule” a visit when they are on shift in the ED. Similarly, patients know who is on shift and might choose an elective visit to the ED to see their family doctors.
The context also differs in a rural setting. There is typically no discrete set of emergency service providers, nor alternate treatment services available, and after-hours primary or urgent care is limited, by default, to the local ED. Patients with simple sprains and lacerations must seek ED treatment, where urban environments have alternative services for after-hours and weekend care for such concerns. The rural ED is an after-hours extension of primary care services. Such context and complement differences affect use and seem to increase it.
Defining high-frequency ED use
Published studies use a range of definitions and acknowledge that a standard has not been established.1 The most common standard used to define high-frequency ED users is 4 or more annual individual patient visits, and definitions that have been used range from 3 or more to 12 or more annual visits.1,8 These definitions generally identify 3% to 10% of the patients who have visited an urban hospital ED.9
No rural definition of high-frequency ED use has been developed.10,11 The higher per capita visit rate indicates that rural patients have a lower threshold for visiting their EDs. Given these differences in overall use profile and service context, we sought to develop a functional definition of high-frequency ED use in rural EDs.
METHODS
We used anonymized annual ED visit information from 2014 for the Sioux Lookout Meno Ya Win Health Centre, a rural 60-bed facility in northwestern Ontario. Data were accessed from regional and national data sets (from the National Ambulatory Care Reporting System) through Northwest Health Alliance, regional health analysts. The data were analyzed to identify high-frequency use using SPSS, version 21. Descriptive statistics, frequencies, and means were obtained to define and characterize high-frequency, very high-frequency, and super users. Ethics approval was granted by the Meno Ya Win Health Centre Research Review and Ethics Committee.
RESULTS
In 2014, 7121 patients made a total of 17 911 visits to the ED at the Sioux Lookout Meno Ya Win Health Centre. The total catchment population is 30 000, for a visit per capita rate of 59.7 per 100 population. The region served encompasses 300 000 km2, and half of those in the 30 000 catchment population require air transportation to access the ED for emergencies and further triaged care.12
Applying the common high-frequency definition of 4 or more annual visits to 2014 ED visitors, 1188 (16.7%) ED patients were identified as high-frequency users (Figure 1).
Figure 1.
Frequency of ED visits (≥ 4 and ≥ 6 annual visits) by patients to the Sioux Lookout Meno Ya Win Health Centre in northwestern Ontario in 2014
ED—emergency department.
Using a standard of 6 or more ED visits a year identified a smaller number of patients (n = 566 [7.9%]) as the high-frequency subset and “normalized” ED use for the remaining 92.1% of patients (Table 1).
Table 1.
Number of visits and admissions for average and high-frequency ED users in 2014
| NO. OF ANNUAL VISITS | PATIENTS, N (%) | VISITS, N (%) | ADMISSIONS, N (%) |
|---|---|---|---|
| 0–5 | 6554 (92.1) | 11 702 (65.3) | 855 (72.8) |
| ≥ 6 | 566 (7.9) | 5607 (31.3) | 284 (24.1) |
| Other | 1 (0.01)* | 602 (3.4) | 36 (3.1) |
ED—emergency department.
Non-insured visits were removed from our analysis. In Ontario Health Insurance Plan data, they are all identified with the same patient identifier number and the number of visits by a specific patient is not available.
We analyzed further subsets of visit pattern categories of very high-frequency use (12 to 19 visits annually) and super users (≥ 20 visits annually). This identified sequentially smaller numbers of patients responsible for disproportionate ED workloads (Table 2).
Table 2.
Subanalysis of ED user frequency by number of visits with admission data
| NO. OF ANNUAL VISITS | PATIENTS, N (%) | VISITS, N (%) | ADMISSIONS, N (%) |
|---|---|---|---|
| Average user (0–5) | 6554 (92.1) | 11702 (65.3) | 855 (72.8) |
| High-frequency user (6–11) | 446 (6.3) | 3381 (18.9) | 205 (17.4) |
| Very high-frequency user (12–19) | 85 (1.2) | 1235 (6.9) | 48 (4.1) |
| Super user (≥ 20) | 35 (0.5) | 991 (5.5) | 31 (2.6) |
| Other | 1 (0.01)* | 602 (3.4) | 36 (3.1) |
ED—emergency department.
Non-insured visits were removed from our analysis. In Ontario Health Insurance Plan data, they are all identified with the same patient identifier number and the number of visits by a specific patient is not available.
DISCUSSION
The context of the ED in a rural setting is important. In an urban context, patients have access to after-hours primary care and urgent-care centres. Applying a high-frequency definition that works well in urban centres is a poor fit for a rural hospital ED when analyzing visit and service patterns.
A definition of high-frequency ED use (≥ 4 visits) that identifies 16.7% of the population as high-frequency users is intuitively overinclusive. A more manageable standard would identify the top 10% or less of ED patients who visit most frequently. Urban studies using the definition of 4 or more visits consistently characterize the high-frequency ED population as less than 10% (typically 3% to 6%) of their total ED visitor populations. It is important to identify such patients, as they account for up to 30% of the ED’s visit workload.3,4 Rather than reuse this definition, we propose a rural standard of 6 or more annual visits to capture a similar proportion of the rural ED visitor population. Applying that benchmark in our ED, we document that 7.9% of patients (with ≥ 6 annual ED visits) are high-frequency and account for 31.3% of visit workload and 24.1% of admissions. Using this high-frequency definition in our setting, we identify a proportion of the population similar to that described by applying the standard of 4 or more in larger urban settings.
If the objective of identifying high-frequency ED users is to design programs and interventions that better meet the needs of these patients, we need a more manageably sized cohort.
Such interventions typically include a form of interdisciplinary case management for identified high-frequency patients and can decrease ED visits by up to 30%.13–16
Our initial high-frequency category (≥ 6) identified 566 patients. This is a rather large number of patients for a small rural hospital to attempt a case management style of intervention.
By further breaking down our visit volume to smaller categories of high-frequency users (≥ 6 to 11 visits), very high-frequency users (12 to 19 visits), and super users (≥ 20 visits), we identify increasingly smaller numbers of patients, with increasingly higher associated per patient visit workloads. This allows for a graded series of interventions, perhaps with greater attention to the 35 super users who are responsible for almost 5.5% of annual ED visits (Table 2). Less intensive interventions can be designed for the 85 patients who are very high-frequency users (12 to 19 visits) and account for almost 7% of the ED visits (Table 2).
Limitations
The setting in northwestern Ontario is unique. The catchment population of 30 000 is spread across 31 remote communities in an area the size of France.12 Most of the remote communities served have no road access to the hospital ED. In these communities, a system of care exists in which urgent care is provided by in-community nurses and emergent care is triaged by a physician in Sioux Lookout arranging a medical evacuation by air. This geographic access barrier likely explains the lower visit per capita ED visit rate of 59.7 per 100 compared with the Huron Country rural visit rate of 89 per 100, but the rate remains higher than the largely urban provincewide rate of 42 per 100 population.5–7
These unique regional characteristics make direct comparison of our high-frequency ED users with other rural centres uncertain. Nonetheless, understanding the demographic characteristics, clinical needs, disposition, and pattern of attendance of high-frequency users can clarify hospital service needs in our setting. The data and resultant high-frequency use definition might not be generalizable to other rural institutions. We encourage other rural EDs to see what visit cutoff level nets them the top 10% of frequent users of their ED.
Conclusion
We suggest the definition of high-frequency rural ED use should be 6 or more annual visits. It makes sense to differentiate the definition from that used in large urban ED centres, both because of the different service context and the size of the subset of ED patients subsequently identified. Further identifying intense users of ED services can be achieved with subset categories of very high-frequency users (12 to 19) and super users (≥ 20). These smaller categories of users allow a graded set of interventions to be considered in a manageable number of patients.
Acknowledgments
This study was partially supported by the Northern Ontario Academic Medicine Association Clinical Innovation Fund.
EDITOR’S KEY POINTS
Patients in rural areas tend to have a higher reliance on emergency departments (EDs) than patients in urban areas do. Definitions of high-frequency use commonly used in research in urban areas might not be appropriate in rural studies.
This study aimed to identify a cutoff for high-frequency ED use that would identify a similar proportion of patients to that identified by the most common cutoff (≥ 4 annual ED visits) used in urban centres. A cutoff of 6 or more annual visits identified 7.9% of ED users in rural northwestern Ontario, similar to proportions identified in urban studies using the lower cutoff.
The 7.9% of high-frequency users accounted for 31.3% of ED workload. Super users (≥ 20 annual visits) amounted to only 35 of the 7121 patients but accounted for 5.5% of ED workload. The 85 very high-frequency users (12 to 19 visits) accounted for a further 6.9% of workload. Graded interventions aimed at these groups could target a manageable number of patients with the potential for a relatively large reduction in workload.
POINTS DE REPÈRE DU RÉDACTEUR
Les patients en milieux ruraux ont tendance à se fier davantage à l’urgence que leurs homologues urbains. Les définitions de l’utilisation à fréquence élevée communément utilisées en recherche dans les centres urbains pourraient ne pas être appropriées dans les études portant sur les milieux ruraux.
Cette étude visait à déterminer un seuil d’utilisation de l’urgence à fréquence élevée qui servirait à déterminer une proportion semblable de patients à celle établie avec les seuils les plus courants (≥ 4 visites annuelles à l’urgence) dans les centres urbains. Un seuil de 6 visites annuelles ou plus a identifié 7,9 % des utilisateurs de l’urgence dans le Nord-Ouest rural de l’Ontario, soit une proportion semblable à celles trouvées dans les études en milieux urbains à l’aide du seuil inférieur.
Les 7,9 % d’utilisateurs à fréquence élevée représentaient 31,3 % de la charge de travail à l’urgence. Le nombre des super utilisateurs (≥ 20 visites annuelles) se situait à seulement 35 sur les 7121 patients, mais ces patients constituaient 5,5 % de la tâche de travail à l’urgence. Les 85 utilisateurs à très grande fréquence (12 à 19 visites) représentaient une proportion additionnelle de 6,9 % de la charge de travail. Des interventions ciblées à l’intention de ces groupes pourraient porter sur un nombre de patients possible à gérer, tout en ayant le potentiel de réduire une proportion relativement importante de la charge de travail.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
All authors contributed to the concept and design of the study; data gathering, analysis, and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Locker TE, Baston S, Mason SM, Nicholl J. Defining frequent use of an urban emergency department. Emerg Med J. 2007;24(6):398–401. doi: 10.1136/emj.2006.043844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mason SM. Frequent attendance at the emergency department is a symptom but not a disease. Emerg Med J. 2014;31(7):524–5. doi: 10.1136/emermed-2014-203674. Epub 2014 Mar 4. [DOI] [PubMed] [Google Scholar]
- 3.Uscher-Pines L, Pines J, Kellerman A, Gillen E, Mehrotra A. Emergency department visits for nonurgent conditions: a systematic literature review. Am J Manag Care. 2013;19(1):47–59. [PMC free article] [PubMed] [Google Scholar]
- 4.Doupe MB, Palatnick W, Day S, Chateau D, Soodeen RA, Burchill C, et al. Frequent users of emergency departments: developing standard definitions and defining prominent risk factors. Ann Emerg Med. 2012;60(1):24–32. doi: 10.1016/j.annemergmed.2011.11.036. Epub 2012 Feb 2. [DOI] [PubMed] [Google Scholar]
- 5.Ovens HJ, Chan BT. Heavy users of emergency services: a population-based review. CMAJ. 2001;165(8):1049–50. [PMC free article] [PubMed] [Google Scholar]
- 6.Hospital emergency departments . In: Annual report 2010. Auditor General of Ontario, editor. Toronto, ON: Queen’s Printer for Ontario; 2010. pp. 132–63. Available from: www.auditor.on.ca/en/content/annualreports/arreports/en10/2010ar_en.pdf. Accessed 2017 Aug 1. [Google Scholar]
- 7.Rourke JT, Kennard M. Emergency patient transfers from rural hospitals: a regional study. CJEM. 2001;3(4):296–301. doi: 10.1017/s1481803500005807. [DOI] [PubMed] [Google Scholar]
- 8.Vinton DT, Capp R, Rooks SP, Abbott JT, Ginde AA. Frequent users of US emergency departments: characteristics and opportunities for intervention. Emerg Med J. 2014;31(7):526–32. doi: 10.1136/emermed-2013-202407. Epub 2014 Jan 28. [DOI] [PubMed] [Google Scholar]
- 9.Van der Linden MC, van den Brand CL, van der Linden N, Rambach AH, Brumsen C. Rate, characteristics and factors associated with high emergency department utilization. Int J Emerg Med. 2014;7(1):9. doi: 10.1186/1865-1380-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hardie TL, Polek C, Wheeler E, McCamant K, Dixson M, Gailey R, et al. Characterizing emergency department high-frequency users in a rural hospital. Emerg Med J. 2015;32(1):21–5. doi: 10.1136/emermed-2013-202369. Epub 2013 Dec 18. [DOI] [PubMed] [Google Scholar]
- 11.Fleet R, Archambault P, Légaré F, Chauny JM, Levesque JF, Ouimet M, et al. Portrait of rural emergency departments in Quebec and utilization of the Quebec emergency department management guide: a study protocol. BMJ Open. 2013;3:e002961. doi: 10.1136/bmjopen-2013-002961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walker RN, Cromarty H, Kelly L, St Pierre-Hansen N. Achieving cultural safety in Aboriginal health services: implementation of a cross-cultural safety model in a hospital setting. Divers Health Care. 2009;6(1):11–22. [Google Scholar]
- 13.LaCalle E, Rabin E. Frequent users of emergency departments: the myths, the data and the policy implications. Ann Emerg Med. 2010;56(1):42–8. doi: 10.1016/j.annemergmed.2010.01.032. Epub 2010 Mar 26. [DOI] [PubMed] [Google Scholar]
- 14.Althaus F, Paroz S, Hugli O, Ghali WA, Daeppen JB, Peytremann-Bridevaux I, et al. Effectiveness of interventions targeting frequent users of emergency departments: a systematic review. Ann Emerg Med. 2011;58(1):41–52.e42. doi: 10.1016/j.annemergmed.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 15.Kumar GS, Klein R. Effectiveness of case management strategies in reducing emergency department visits in frequent user patient populations: a systematic review. J Emerg Med. 2013;44(3):717–29. doi: 10.1016/j.jemermed.2012.08.035. Epub 2012 Nov 29. [DOI] [PubMed] [Google Scholar]
- 16.Morgan SR, Chang AM, Alqatari M, Pines JM. Non-emergency department interventions to reduce ED utilization: a systematic review. Acad Emerg Med. 2013;20(10):969–85. doi: 10.1111/acem.12219. [DOI] [PMC free article] [PubMed] [Google Scholar]