Abstract
Patient: Female, 44
Final Diagnosis: Agranulocytosis
Symptoms: Fever • pharyngalgia
Medication: Sinomenine
Clinical Procedure: Stop taking medicine and treat it
Specialty: Rheumatology
Objective:
Unknown ethiology
Background:
Sinomenine hydrochloride is an alkaloid that is extracted from the Chinese herbal plant Sinomenium acutum, and is used as a herbal medicine in the treatment or rheumatic disease. This report is the first to describe a case of sinomenine hydrochloride-induced agranulocytosis.
Case Report:
A 44-year-old woman with systemic lupus erythematosus (SLE) and systemic sclerosis (SSc) was treated with sinomenine hydrochloride and developed agranulocytosis with a neutrophil count of 0.01×109/L. She subsequently developed an opportunistic bacterial infection. Bone marrow aspiration showed a severe reduction in the proportion of mature granulocytes. The patient discontinued sinomenine hydrochloride therapy and was treated with granulocyte colony-stimulating factor (G-CSF) and antibiotics. The patient showed a return to normal granulocyte levels within ten days of discontinuing treatment with sinomenine hydrochloride.
Conclusion:
The findings of this case report show that monitoring of bone marrow function and granulocyte levels should be performed during treatment with sinomenine hydrochloride.
MeSH Keywords: Agranulocytosis, Opportunistic Infections, Sinomenium
Background
Agranulocytosis is characterized by a severe decrease in or lack of circulating granulocytes and is defined as a neutrophil count of <0.5×109/L [1,2]. Patients with agranulocytosis are more likely to experience opportunistic infections, which can be life-threatening. Most, but not all, cases of agranulocytosis result from exposure to drugs or are a consequence of exposure to a drug metabolite as the causative agent, including chemotherapy, and idiosyncratic or unpredictable drug-induced responses to a wide range of drugs [3]. These drugs include ticlopidine, clozapine, sulfasalazine, dipyrone, angiotensin-converting enzyme inhibitors and anti-thyroid drugs [3,4]. Over the last 20 years in the USA, the incidence of idiosyncratic drug-induced agranulocytosis has remained stable at between 2.4–15.4 cases per million, and the associated mortality rate has been estimated at 5% [3].
The alkaloid, sinomenine hydrochloride (7,8-didehydro-4-hydroxy-3,7-dimethoxy-17- methylmorphinane-6-one, C19H23NO4), CAS number 6080-33-7, is extracted from the Chinese herbal medicinal plant, Sinomenium acutum, and has been widely used for centuries in China to treat patients with rheumatic diseases. Clinical side effects typically associated with sinomenine hydrochloride therapy include gastrointestinal symptoms, allergic responses, increased serum alanine transaminase (ALT), dizziness, and leukopenia [5,6]. This report is the first to describe a case of sinomenine hydrochloride-induced agranulocytosis.
Case Report
In April 2016, a 44-year-old woman was referred for hospital admission from our rheumatology department after presenting with a three-day history of fever and pharyngeal pain. Nine years prior to admission, she had been diagnosed with systemic lupus erythematosus (SLE) and systemic sclerosis (SSc), which were associated with skin sclerosis of the extremities and widespread arthralgia. The patient reported long-term use of methylprednisolone 8 mg/day and hydroxychloroquine 400 mg/day. The patient denied a history of smoking and did not drink alcohol. Also in April 2016, she was prescribed sinomenine hydrochloride at a dose of 180 mg/day in the outpatient department of our hospital. On April 23rd 2016, the patient described symptoms of pharyngeal pain, discomfort and was found to have a fever that reached a maximum of 38.3°C.
On admission to hospital, physical examination showed a temperature of 36.5°C. There was fibrosis of the skin of the forearms and legs in the absence of any palpable erythema of her face. Laboratory investigations showed a hemoglobin level of 116 g/L, leukocyte count of 0.81×109/L, neutrophil count of 0.01×109/L, lymphocyte count of 0.70×109/L, platelet count of 110×109/L, an erythrocyte sedimentation rate (ESR) of 11 mm/h, and C-reactive protein (CRP) level of 2 mg/dL. Liver and renal function, complement C3 and C4 levels, and urinalysis were all normal, and there was no proteinuria. Anti-nuclear antibody (ANCA) was positive at a titer of 1/320. Anti-double stranded DNA (dsDNA) and anti-neutrophil cytoplasmic antibodies (ANCA) were negative. The Naranjo algorithm, or adverse drug reaction probability score, was 5. Chest computed tomography (CT) and electrocardiogram (ECG) were both normal. Quantification of 24-hour urinary protein was within normal limits, at a level of 56 mg.
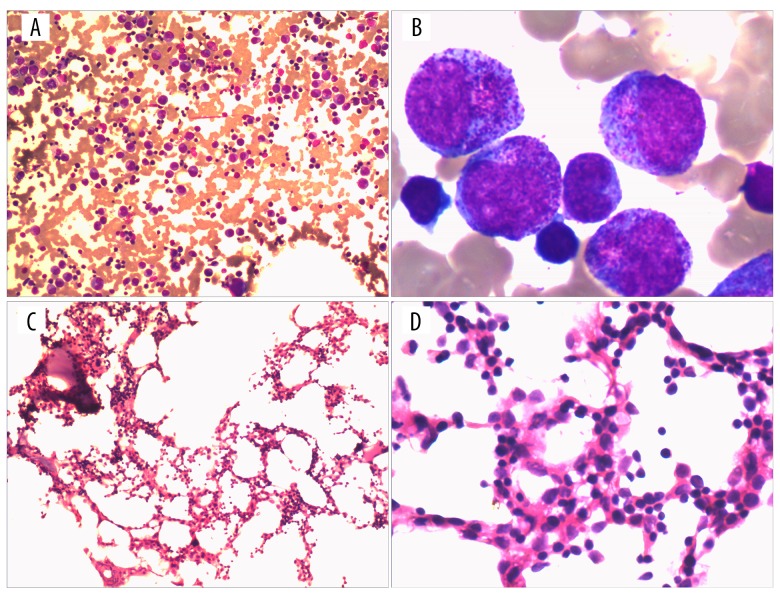
The patient was diagnosed with SLE, SSc, agranulocytosis, and the presence of a possible bacterial infection. Infection control measures were implemented, and the patient was monitored through routine blood testing. The initial diagnostic bone marrow aspirate showed reduced numbers of granulocytes that showed an increased cell volume and enlarged cytoplasmic granules (Figure 1A, 1B). Histology of the bone marrow biopsy showed an absence of the mature stages of granulocyte development (Figure 1C, 1D).
Figure 1.
Photomicrographs of the bone marrow aspirate and bone marrow biopsy. (A) Bone marrow aspirate; ×100. (B) Bone marrow aspirate; ×1,000. (C) Bone marrow biopsy; ×100. (D) Bone marrow biopsy; ×1000.
The patient ceased treatment with sinomenine hydrochloride and was subsequently treated with recombinant granulocyte colony-stimulating factor (G-CSF) subcutaneously at a dose of 150 µg twice daily. Intravenous imipenem and cilastatin sodium were given to treat the presumed bacterial infection. The patient had a systemic lupus erythematosus disease activity index (SLEDAI) score that was very low, suggesting her SLE was stable. There was no microbial growth in blood and urine cultures; fungi D-glucan was absent from the blood, supporting a lack of fungal infection. On the third day of treatment, the leukocyte and neutrophil count increased to 1.11×109/L and 0.07×109/L, respectively, and her fever resolved. After ten days of treatment, the leukocyte and neutrophil counts had increased to 29.99×109/L and 2.45×109/L, respectively, in keeping with resolution of the agranulocytosis. Routine monitoring of leukocyte and neutrophil counts revealed normal levels at final follow-up, one month following initial hospital admission (Figure 2).
Figure 2.
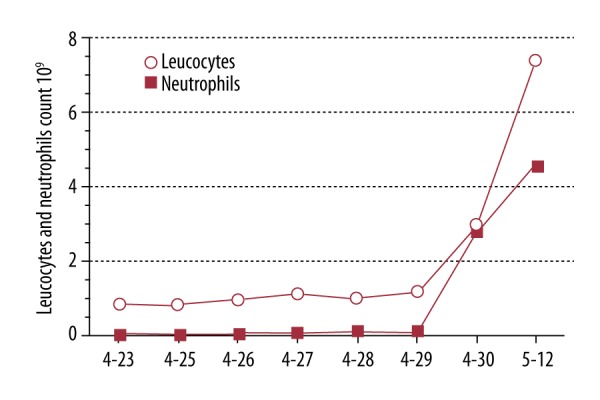
Leukocyte and neutrophil counts during treatment.
Discussion
Recent reports of adverse events associated with Chinese herbal medicines have increased [7]. For example, the use of herbal remedies containing aristolochic acid has recently been banned in China due to the association with renal toxicity and carcinogenicity [8]. This case has shown that agranulocytosis followed an 18-day treatment course of sinomenine hydrochloride use in a patient who presented with stable systemic lupus erythematosus (SLE).
According to a 30-year retrospective study of antithyroid drug-induced agranulocytosis, bone marrow changes usually develop within 90 days following the start of therapy and typically demonstrates a female predominance [9]. The patient described in this case report had a normal granulocyte count before treatment with sinomenine hydrochloride. The Naranjo algorithm, or adverse drug reaction probability score, was 5, which indicated a probable treatment-associated adverse effect from sinomenine hydrochloride therapy. Also, other causes of agranulocytosis were excluded. Sinomenine-induced agranulocytosis was diagnosed in this case, which is the first report of this finding.
The exact mechanisms responsible for agranulocytosis in this case, and other drug-associated cases, are not well understood. The proposed mechanisms for agranulocytosis have been classified as either toxic or autoimmune [10]. In autoimmune agranulocytosis, autoantibodies against the neutrophil are generated because of a loss in self-tolerance, a phenomenon that has been reported in levamisole-induced agranulocytosis [11]. It is also possible that patient characteristics, including host genetics, appear to be key factors in future prediction and prevention of drug-induced agranulocytosis [10].
In this case report, the bone marrow biopsy showed that the number of granulocytes were both reduced and showed a maturation disorder, which may indicate that sinomenine hydrochloride causes bone marrow suppression through an as yet unknown mechanism. Even though sinomenine hydrochlo-ride-induced agranulocytosis appears to be rare, the potentially severe effects of agranulocytosis warrant a warning to patients who are treated with sinomenine hydrochloride, which should be discontinued if fever and a sore throat occur. We also advise monitoring of peripheral blood granulocytes during treatment with sinomenine hydrochloride.
Conclusions
For many centuries, traditional Chinese herbal medicines have played an important role in the prevention and treatment of the symptoms of disease in China. However, risk factors that are associated with the use of these drugs remain poorly understood. Based on this case study, we suggest frequent monitoring of granulocyte numbers during clinical use of sinomenine hydrochloride.
Acknowledgments
Professor Cong-qiu Chu of Oregon Health and Science University provided helpful opinion
Footnotes
Conflict of Interests
None.
References:
- 1.Andrès E, Zimmer J, Affenberger S, et al. Idiosyncratic drug-induced agranulocytosis: Update of an old disorder. Eur J Intern Med. 2006;17:529–35. doi: 10.1016/j.ejim.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 2.Andersohn F, Konzen C, Garbe E. Nonchemotherapy drug-induced agranulocytosis: A systematic review of case reports. Ann Intern Med. 2007;146:657–65. doi: 10.7326/0003-4819-146-9-200705010-00009. [DOI] [PubMed] [Google Scholar]
- 3.Andrès E, Maloisel F. Idiosyncratic drug-induced agranulocytosis or acute neutropenia. Curr Opin Hematol. 2008;15(1):15–21. doi: 10.1097/MOH.0b013e3282f15fb9. [DOI] [PubMed] [Google Scholar]
- 4.Hashmi HR, Jabbour R, Schreiber Z, Khaja M. Benazepril-induced agranulocytosis: A case report and review of the literature. Am J Case Rep. 2016;17:425–28. doi: 10.12659/AJCR.898028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Y, Fang YF, Huang W, et al. Effect of sinomenine on cytokine expression of macrophages and synoviocytes in adjuvant arthritis rats. J Ethnopharmacol. 2005;98(1–2):37–43. doi: 10.1016/j.jep.2004.12.022. [DOI] [PubMed] [Google Scholar]
- 6.Chen XM, Huang RY, Huang QC, et al. Systemic review and meta-analysis of the clinical efficacy and adverse effects of Zhengqing Fengtongning combined with methotrexate in rheumatoid arthritis. Evid Based Complement Alternat Med. 2015;2015:910376. doi: 10.1155/2015/910376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zheng QH, Li XL, Mei ZG, et al. Efficacy and safety of puerarin injection in curing acute ischemic stroke: A meta-analysis of randomized controlled trials. Medicine (Baltimore) 2017;96(1):e5803. doi: 10.1097/MD.0000000000005803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shi M, Ma L, Zhou L, et al. Renal protective effects of 17β-estradiol on mice with acute aristolochic acid nephropathy. Molecules. 2016;21(10) doi: 10.3390/molecules21101391. pii: E1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakamura H, Miyauchi A, Miyawaki N, Imagawa J. Analysis of 754 cases of antithyroid drug-induced agranulocytosis over 30 years in Japan. J Clin Endocrinol Metab. 2013;98(12):4776–83. doi: 10.1210/jc.2013-2569. [DOI] [PubMed] [Google Scholar]
- 10.Tesfa D, Keisu M, Palmblad J. Idiosyncratic drug-induced agranulocytosis: Possible mechanisms and management. Am J Hematol. 2009;84(7):428–34. doi: 10.1002/ajh.21433. [DOI] [PubMed] [Google Scholar]
- 11.Thompson JS, Herbick JM, Klassen LW, et al. Studies on levamisole – induced agranulocytosis. Blood. 1980;56:388–96. [PubMed] [Google Scholar]