Abstract
Borderline personality disorder (PD) historically is construed as an unremitting condition with poor prognosis. The present study takes a new approach to examining stability and change in borderline PD by explaining symptom expression in terms of an unchanging foundation—termed borderline proneness—on one hand, and transitory influences on the other. We monitored borderline PD symptoms annually in a large sample of high-risk adolescent girls (N = 2,450) from ages 14 to 20. Trait-state-occasion modeling revealed that just over half (52–57%) of borderline PD symptom variation was attributable to fixed borderline proneness, whereas the remainder was subject to change across yearly measurement occasions. This degree of stability was no larger than the corresponding estimate for depression, a condition known for its variable course. Our results indicate that, contrary to its reputation, borderline pathology is not set in stone, and it fluctuates in response to situational influences.
Keywords: borderline personality disorder, depression, hybrid model, trait-state-occasion model
Borderline personality disorder (PD) is associated with enduring social impairment and repeated contact with mental health services. Paradoxically, recent longitudinal research on the time course of borderline PD suggests that its symptoms are much less persistent than traditionally believed. Over the past few years, large clinical studies have shown that the majority of borderline PD patients (85–93%) remit over a 10-year follow-up interval, albeit more slowly than a comparison group diagnosed with depression but no PD (Gunderson et al., 2011; Zanarini, Frankenburg, Reich, & Fitzmaurice, 2010).
Adding a layer of complexity to these findings, a report from the Collaborative Longitudinal Personality Disorders Study (CLPS) showed that not all borderline PD symptoms were equally stable over two years (McGlashan et al., 2005). Some rarely remitted (e.g., affective instability, anger), whereas others were sporadic (e.g., self-injury, abandonment fears). This finding led a number of investigators to advance a hybrid model, a theory that posits that borderline and other PDs are a mixture of fixed features and more intermittent symptomatic behaviors (McGlashan et al., 2005; see also Clark, 2009). This model was subsequently supported in an independent sample of borderline PD patients (Zanarini et al., 2007). There is thus reason to believe that some borderline PD symptoms are highly persistent—conforming to the classical conceptualization of PD as an enduring entity—whereas others are episodically expressed and sensitive to developmental and environmental influences.
Other research in community samples has examined the trajectory of borderline PD symptom composites across development (Morey & Hopwood, 2013). A fairly flat, or rising, symptom trajectory would fit the conception of borderline PD as an unabating syndrome. Instead, developmental studies indicate that borderline PD symptoms tend to surge in mid-adolescence and then recede at the transition to adulthood and beyond (e.g., Bornovalova, Hicks, Iacono, & McGue, 2009).
Collectively, these findings suggest that borderline PD is not as stable as traditionally believed. This observation begs the question of how much of the expression of borderline PD at any given moment is due to an immutable borderline proneness, as compared to transient influences on borderline PD that cause acute fluctuations in symptom presentation. Research has yet to delineate these fixed and fluctuating contributions to borderline PD.
Trait-state-occasion (TSO) modeling offers a method for isolating fixed borderline proneness. The TSO model was formulated to parse the stable versus unstable components of psychological variables (Cole, Martin, & Steiger, 2005). TSO is a type of structural equation modeling that dissects a condition at any point in time (i.e., state) into time-invariant (i.e., trait) and time-variant (i.e., occasion) parts. Here, the trait component reflects an enduring borderline proneness, whereas the occasion component reflects transitory influences on borderline pathology. Stated differently, the occasion factor reflects the causes of acute symptoms that are not manifested across the entire period of interest. For example, deliberate self-injury might occur only in the context of a toxic romantic relationship, or reckless behavior (e.g., dangerous driving) might be confined to discrete episodes of substance misuse. The TSO framework has been applied to several psychiatric outcomes, such as anxiety, depression, and related personality traits (e.g., Olatunji & Cole, 2009; Prenoveau et al., 2011). For instance, in a high-risk adolescent sample, Prenoveau et al. (2011) found that depression was more episodic—it had a smaller time-invariant component—than personality traits such as neuroticism and extraversion.
In the present study, we determined the extent to which borderline PD symptoms reflect an unchanging borderline proneness. We applied TSO modeling to a large sample of high-risk girls assessed annually from ages 14 to 20. Our primary objective was to determine the proportion of variability in borderline PD that is perfectly stable over adolescence. We also tested predictions of the hybrid model (e.g., McGlashan et al., 2005), which asserts that some borderline PD symptoms are trait-like, whereas others are more state-like and resolve relatively quickly. Further, we compared the size of the time-invariant component of borderline PD to that of depression. We chose depression as a contrast because of its known variable course. For instance, over the CLPS 10-year follow-up, 67% of depressed patients experienced a recurrence. In community samples, recurrence rates reach 40% over adolescence and young adulthood (see Rohde, Lewinsohn, Klein, Seeley, & Gau, 2013). Although little research has examined the year-to-year stability of borderline PD, the predominant view of borderline PD is one of temporal stability. Thus, we expected the TSO to reveal that the lion’s share of variation in borderline PD is explained by fixed borderline proneness, whereas we predicted that individual differences in depression would be due predominantly to state-like processes.
Methods
Sample
The Pittsburgh Girls Study (PGS) recruited an urban community sample of girls (N = 2,450) ages 5 to 8 at the first assessment occasion. Girls and their caretakers were subsequently followed up annually through childhood and adolescence. Low-income neighborhoods in Pittsburgh were oversampled such that neighborhoods in which at least 25% of families were living at or below the poverty level were fully enumerated. A random selection of 50% of the households in all other neighborhoods was visited. The racial/ethnic sample composition was 53.0% African American, 41.2% White, and 5.8% multiracial or other race. The majority of parents (57%) were cohabiting with a spouse or domestic partner, and half had completed more than 12 years of education (see Hipwell et al., 2002, for full recruitment details).
Procedure
Trained interviewers administered the questionnaires in girls’ homes. Study questionnaires were completed annually from ages 14 through 20 (i.e., PGS assessment waves 7 through 13). All study procedures received Institutional Review Board approval by the Human Research Protection Office at the University of Pittsburgh.
Measures
Borderline PD Symptoms
Girls reported on borderline PD symptoms yearly from age 14 to 20 using the screening questionnaire of the International Personality Disorders Examination (IPDE-BOR; Loranger et al., 1994). The IPDE-BOR features 10 true/false items, at least one covering each of the borderline PD diagnostic criteria in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 2000). Example items include “I get into very intense relationships that don’t last,” “I have tantrums or angry outbursts,” and “When I’m under stress things around me don’t seem real.” Responses to the IPDE-BOR demonstrate favorable convergent validity with interview and self-report measures of borderline PD in samples of adolescents and adults (e.g., Chanen et al., 2008; Lenzenweger et al., 2007). Moreover, its pattern of intercorrelations with measures of other disorder constructs (e.g., depression), support its discriminant validity vis-à-vis other PDs and clinical disorders (e.g., Schroeder, Andresen, Naber, & Huber, 2010). Additionally, prior investigations have provided evidence of criterion validity, showing concurrent and prospective correlations of the IPDE-BOR with mental health treatment use, psychosocial functioning, aggression, criminal activity, and suicide (e.g., Lenzenweger et al., 2007; Wright, Zalewski, Hallquist, Hipwell, & Stepp, 2016). After omitting one item with an especially low item-total correlation (see below), the internal consistency (i.e., Cronbach’s alpha) for BPD symptoms ranged from .71 to .73 across waves.
Depression
Girls reported on symptoms of depression using the Adolescent Symptom Inventory-Fourth Edition (ASI-4; Gadow & Sprafkin, 1998), transitioning to the Adult Self-Report Inventory (ASRI-4; Gadow, Sprafkin, & Weiss, 2000) at age 18. This set of measures includes the 9 symptoms of DSM-IV MDD rated on a 4-point scale (0 = never, 3 = very often). Adequate concurrent validity, sensitivity, and specificity for the depression scale, relative to interview-based diagnoses, have been reported for these measures (e.g., Gadow & Sprafkin, 1998). Internal consistency estimates for the depression composite ranged from .79 to .86 across waves in the present study.
Statistical Analysis
The raw data were analyzed in Mplus (version 7.11; Muthén & Muthén, 1998–2014) using the WLSMV estimator. Model goodness of fit was evaluated by the comparative fit index (CFI), the Tucker-Lewis index (TLI), the root mean square error of approximation (RMSEA), and the weighted root mean square residual (WRMR). Guidelines offered by Hu and Bentler (1999) were used to define acceptable model fit: RMSEA values close to 0.06 or below, CFI and TLI values close to .95 or above, and SRMR values close to .08 or below. Missing data due to attrition were accommodated in all analyses using direct maximum likelihood. The retention rates for PGS assessment waves 8–13 were 89.2%, 88.1%, 86.1%, 85.6%, 85.4% and 86.1%, respectively. Retention was not related to baseline psychopathology, except for attritors at wave 12 endorsing slightly lower levels of baseline (i.e., wave 7) borderline PD symptoms, t(2,147) = 2.99, p < .01.
Results
Longitudinal Measurement Models
We tested for measurement invariance, a prerequisite of TSO modeling (e.g., Horn & McArdle, 1992), by specifying longitudinal confirmatory factor analyses (CFAs) of borderline PD symptoms at the two most distant assessment waves (i.e., PGS wave 7 and wave 13). We first estimated a baseline model with no constraints, then a model in which each indicator’s factor loading was constrained to the same value across waves (i.e., weak invariance). Cross-wave error covariances for the same indicator were freely estimated.
The longitudinal confirmatory factor model offered a good fit to the data, χ2(2,699) = 4,492.39, p < .001; CFI = .96; TLI = .95; RMSEA = 0.02; WRMR = 1.32. All items were strongly related to the borderline PD factors, except the one reflecting affective lability (“I show my feelings for everyone to see”). The standardized loadings for this item across waves ranged from −.05 to .14. This item was dropped from subsequent analyses.1
The revised unconstrained longitudinal CFA provided an even better fit, χ2(2,139) = 3,409.44, p < .001; CFI = .97; TLI = .97; RMSEA = 0.02; WRMR = 1.23, and all standardized factor loadings were moderate-to-large (range: .36–.90) and significant at a .001 alpha level. Table S1 in the online Supplemental Material presents the correlations among borderline PD factors across study waves. Constraining factor loadings to equality across time points did not significantly diminish model fit, χ2diff(8) = 3.86, p = .87. Thus, weak measurement invariance was satisfied, and we could safely estimate the TSO model (see Cole et al., 2005). Acceptable model fit and weak measurement invariance were also demonstrated for the depression longitudinal CFA (full results available upon request).
Trait-State-Occasion (TSO) Model of Borderline PD
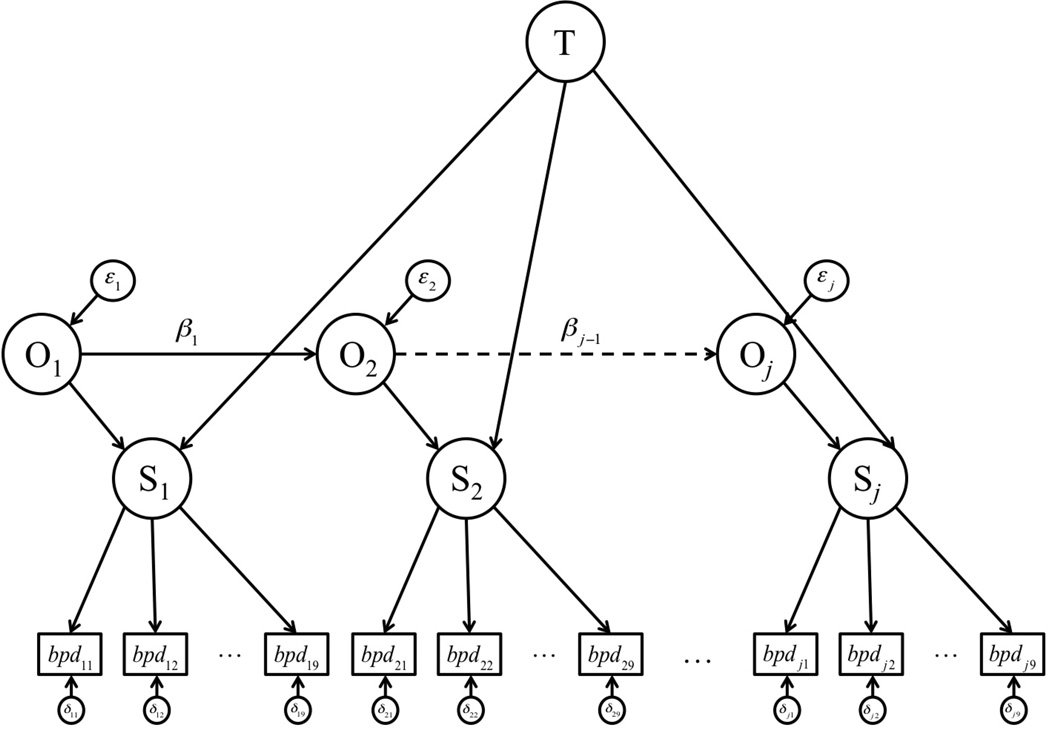
The TSO model decomposed borderline PD variability into a time-invariant (i.e., trait) latent variable and 7 time-varying (i.e., occasion) latent variables (see Figure 1 for a schematic). The time-invariant factor captured borderline proneness that was perfectly stable across waves, whereas the time-varying factors captured contributions to borderline pathology that fluctuated from wave to wave. Additionally, autoregressive parameters linking contiguous occasion factors were specified to allow for continuity in time-specific fluctuations in borderline symptoms (e.g., anger outbursts secondary to a tumultuous relationship that lasts for 2 years). State factor error variances were fixed to nil such that borderline PD variance was completely partitioned into the trait and occasion factors. In accordance with established guidelines (Cole et al., 2005), we (i) constrained factor loadings of borderline PD indicators to equality over time, (ii) constrained the residual terms of the latter 6 occasion factors to equality, (iii) fixed the 6 autoregressive parameters to equality, and (iv) allowed residual correlations among the same borderline PD item across waves. This last restriction ensures a conservative estimate of borderline PD stability by removing shared method variance that might otherwise inflate our estimate of the time-invariant factor variance (Cole, 2006).
Figure 1.
Trait-state-occasion model for borderline personality disorder. T = trait, O = occasion, and S = state for j waves. β= autoregressive parameter; ε = occasion factor disturbance; δ = manifest variable residual. The manifest variable subscripts represent wave (first subscript) and item (second subscript) numbers. For clarity of presentation, error covariances are not shown.
Table 1 displays the model fit and parameter estimates for the borderline PD TSO model. The model fit the data well, χ2(1,640) = 2,405.81, p < .001; CFI = .98; TLI = .98; RMSEA = 0.01; WRMR = 1.25, and factor loadings were all highly significant. The trait factor variance represented 52–57% of the total borderline PD variance from ages 14 to 20. This percentage was not constant across waves because the total variance in borderline pathology changed over time (e.g., individual differences in borderline PD state factor were more pronounced at age 20 than age 14). Thus, trait variance represented the highest proportion of total variance at age 14 because total variance (i.e., borderline PD state factor variance) was smallest then. The trait factor variance and all 7 occasion factor variances were greater than 0 (all ps < .001). Additionally, the continuity among occasion factors was moderate and statistically significant (b = 0.50, SE = 0.04, p < .001).
Table 1.
Trait-State-Occasion Model Estimates for Borderline Personality Disorder
| Borderline Personality Disorder |
|||||||
|---|---|---|---|---|---|---|---|
| Measure | Age 14 | Age 15 | Age 16 | Age 17 | Age 18 | Age 19 | Age 20 |
| Total variance (unstandardized) | .20 | .22 | .22 | .22 | .22 | .22 | .22 |
| Time-invariant variance (unstandardized) | .11 | .11 | .11 | .11 | .11 | .11 | .11 |
| Time-variant variance (unstandardized) | .09 | .11 | .11 | .11 | .11 | .11 | .11 |
| Proportion of variance due to time-invariant component | .57 | .53 | .52 | .52 | .52 | .52 | .52 |
| Proportion of variance due to time-variant component | .43 | .47 | .48 | .48 | .48 | .48 | .48 |
| Stability coefficient (unstandardized/standardized) | — | .50/.46 | .50/.49 | .50/.50 | .50/.50 | .50/.50 | .50/.50 |
Note. Model fit: χ2(1,640) = 2,405.81, p < .001; CFI = .98; TLI = .98; RMSEA = 0.01; WRMR = 1.25. All parameter estimates are statistically significant at the .001 level.
The Hybrid Model for Borderline PD
We performed separate TSOs of acute versus temperamental borderline PD criteria to test the hybrid model for borderline PD (McGlashan et al., 2005; Zanarini et al., 2000). As stated earlier, the theory stipulates that some symptoms are intermittent and resolve quickly, whereas others are more stable. Under the hybrid model, acute symptoms comprised self-harm, stress-linked paranoia, abandonment concerns, and identity disturbance. We first fit a TSO model wherein these four symptoms served as indicators of a borderline PD factor at each measurement occasion. This model provided an excellent fit to the data, χ2(245) = 252.96, p = .35; CFI = 0.99; TLI = 0.99; RMSEA = 0.00; WRMR = 0.81. The ratio of trait variance to total variance was 52–53% across waves. The autoregressive parameter estimate among occasion factors was moderate and statistically significant (b = 0.38, SE = 0.06, p < .001).
We carried out the same analysis for the temperamental borderline PD symptoms. The theoretically more enduring, temperamental criteria were impulsivity, unstable relationships, chronic emptiness, and intense anger. The TSO model also fit these data well, χ2(482) = 778.55, p < .001; CFI = 0.99; TLI = 0.99; RMSEA = 0.02; WRMR = 1.16. The proportion of trait variance (relative to total variance) ranged from 51–57% across waves. Thus, contrary to hybrid model predictions, the influence of time-invariant factors was no more prominent for the putatively temperamental symptoms than it was for the putatively acute symptoms. The autoregressive parameter estimate for the temperamental symptoms TSO model was moderate in size (b = 0.57, SE = 0.04, p < .001).2
TSO Model of Depression
A TSO model of depressive symptoms was fit according to the same specifications. As was the case for borderline PD, TSO model fit was good for depression, χ2(2,623) = 5,754.10, p < .001; CFI = 0.97; TLI = 0.97; RMSEA = 0.02; WRMR = 1.77. The trait factor accounted for 46–53% of the total variation in depression across time points (see Table S2 for full results).
After demonstrating good fit for the depression TSO model, we simultaneously estimated the borderline PD and depression TSO models to examine (i) the similarity of trait factor variances and (ii) the correlation among trait factors for these two outcomes. In this combined model, we allowed cross-construct correlations among the trait factors and all occasion factors (the latter were constrained to equality across follow up waves). This model fit the data well, χ2(8,829) = 13.614.14, p < .001; CFI = 0.97; TLI = 0.97; RMSEA = 0.01; WRMR = 1.58. The correlation between trait factors was large and statistically significant (r = .82, SE = .02, p < .001). Finally, using the model test command in Mplus, we found that the ratio of trait variance to total variance in borderline PD did not differ significantly from the corresponding ratio for depression, χ2(1) = 0.01, p = .97.
Discussion
Modern classification systems, not to mention most mental health professionals, cast borderline PD as an immutable condition. Our data, gathered from a large sample of girls assessed seven times across adolescence, seem to tell a different story. Approximately half of the variation in borderline PD symptoms at any moment was attributable to time-specific factors; in other words, nearly half of symptom expression was subject to change across measurement occasions. Further, borderline pathology proved to be no more stable than depression—a quintessentially episodic disorder—across the seven-year interval.
We applied a novel conceptual and analytic framework to study the temporal course of borderline PD features. That is, we directly quantified the amount of variation in borderline pathology that reflects an unchanging “borderline proneness” versus more transient influences on symptom development. Borderline proneness—the TSO trait factor—represents genetic, static biological, and unremitting psychological and environmental conditions that predispose to borderline pathology (e.g., Distel et al., 2008). In contrast, the TSO occasion factors reflect psychological, social, and even biological characteristics that change over time and influence borderline PD vulnerability. Indeed, some of these state-like influences (e.g., exiting an abusive relationship, shifting to a new medication regimen) were cited as possible determinants of sudden remissions of borderline PD diagnoses in the CLPS (Gunderson et al., 2003).
The hybrid model is a popular theoretical account of borderline PD instability. It posits that borderline PD can appear to be intermittently present because some borderline features are acute symptomatic reactions to situational stressors, whereas other features are more slowly evolving and trait-like (McGlashan et al., 2005). Our analyses did not support the hybrid model: the temperamental symptoms were empirically no more stable than acute symptoms in this sample. This conclusion contrasts with findings from the 10-year McLean Study of Adult Development, in which some borderline PD symptoms and associated features showed appreciable improvement over follow up whereas others persisted (Zanarini et al., 2007). On the other hand, the 10-year follow up of the CLPS found that all DSM-IV criteria for borderline PD exhibited the same trajectory of improvement over time (Gunderson et al., 2011). Results from these three samples are not directly comparable, given the varying analytic approaches to studying stability. Nonetheless, our data align with those from CLPS in challenging the hybrid account of borderline PD instability.
Depressive symptom stability served as a benchmark for borderline PD symptom continuity. We hypothesized that borderline PD stability would surpass that of depression, which typically follows a variable pattern of relapse and remission. Instead, similar to borderline PD symptoms, nearly 50% of depression variation was completely stable across time. A significance test confirmed that this proportion (of stable variance to total variance) was not smaller than the corresponding estimate for borderline PD. This comparison reinforces the conclusion that, at least for adolescent girls, borderline pathology is far more fluid over time than most researchers and clinicians believe.
If corroborated in future work, these results could have implications for the borderline PD diagnosis. First, in DSM-5 borderline PD is described as “stable and of long duration” (APA, 2013, p. 647) and “lifelong” (p. 665). That language is tempered in DSM-5 Section III (Alternative DSM-5 Model for Personality Disorders), where the general definition of PD indicates that “impairments in personality functioning and the individual’s personality trait expression are relatively stable across time” (emphasis added, p. 761). Our data are more consistent with the latter view. Second, given the instability observed here, nosologists must establish a minimum duration criterion for borderline PD symptoms. Only then will diagnosticians be able to distinguish first onsets and possible recurrences of borderline PD from closely related clinical conditions and from normality. Third, in this same vein, we believe our results underscore the importance of careful probing into the time course of borderline pathology when considering a borderline PD diagnosis. A “snapshot” of a clinical profile may reveal a symptom presentation that appears consistent with borderline PD but is in fact a transient flare-up of painful emotions and disinhibited behavior.
As a secondary objective, we examined the covariation between the time-invariant factors for depression and borderline PD symptoms. They were very strongly correlated (r = .82), indicating that the stable substrates underlying these two conditions are largely overlapping. This result accords with structural models of psychopathology that show borderline PD loads on an internalizing spectrum undergirding anxiety and depression (e.g., Eaton et al., 2011) and, more generally, the decision to collapse across Axes I and II in DSM-5 (see Krueger, 2005). We recommend continued research into the discriminant validity of borderline PD—especially as it relates to depression—in ways that inform the differential diagnosis process.
Additionally, an intriguing implication for etiological research is that the search for causes of borderline PD—a condition that has earned comparatively little research attention and funding—could be allied with that of depression. That is, given the overlap observed here among the foundations of these two conditions, it could be inferred that many of the stable causes (e.g., genetics, neurobiology, early life experiences) of depression also set the stage for borderline pathology. In this scenario, researchers hunting the early origins of borderline PD might look to etiological findings for depression for guidance. By the same token, the risk factors that are distinctive to the static core of depression or borderline pathology might account for why people develop one syndrome versus the other (i.e., divergent trajectories). For example, there is good reason to believe that disinhibition is a key component of borderline proneness, but it unlikely to be a diathesis for depression (e.g., Trull, 2001).
Limitations
This study benefitted from a large, diverse sample and an intensive follow up data structure, but several limitations must be considered alongside these strengths. First, adolescence is a period of heightened PD symptoms and symptom change (e.g., Johnson et al., 2000). Borderline pathology, like normative personality traits, may be more stable in later developmental stages. Future TSO modeling in adult samples can determine whether traitlike borderline proneness becomes a more prominent influence on borderline features later in development. Second, our sample was entirely female, so gender differences in borderline PD severity or stability could not be addressed. Third, our analyses relied exclusively on self-reported symptoms. Symptom-based assessments are often preferred to diagnosis-level data in the context of stability research because even minor changes in symptom severity around a diagnostic threshold can give the impression of major symptom change (Clark, 2009). However, self-report instruments tend to overestimate the prevalence of PD symptoms, which could affect stability estimates (Miller et al., 2012). Surveys, as compared to interviews, are also susceptible to mood state distortion, which could have artificially inflated the association between borderline pathology and depression in our study. Although interview measures limit false-positives and are less susceptible to mood state distortion, the resource costs likely would have rendered them impractical in our sample (N = 2,450). Moreover, our self-report version of the IPDE corresponds well to the IPDE interview in prior validation research (e.g., Lenzenweger et al., 2007).
We believe, therefore, that some caution is advisable when drawing conclusions from these results until replication studies involving gold-standard interview assessment of borderline PD are available. Although interview measures can also be biased by mood states or other situational reactions (cf. Gunderson et al., 2003), interviewers can more flexibly make differential diagnoses, detect the possibility of mood state distortion, and probe the temporal course of symptoms. Additionally, based on structural modeling of mental disorders that shows strong overlap among the biological and psychological dimensions underlying borderline PD and other psychopathology (e.g., Eaton et al., 2011; Lahey, Krueger, Rathouz, Waldman, & Zald, in press), we recommend that future studies incorporate assessment measures that distinguish the common versus specific elements of borderline PD.
Conclusion
Just over half (52–57%) of the variation in adolescent borderline pathology is caused by a borderline proneness that never changes. This degree of continuity in borderline PD symptoms was no larger than that of depression, a condition known for its instability. These observations lead us to conclude that, at least among adolescent girls, borderline pathology is neither set in stone nor mostly variable from year to year. We believe that this conclusion has important implications for borderline PD prognostic decisions, treatment delivery, and prevention efforts. For one, borderline PD features may be amenable to focused intervention to address acute conditions that produce symptom flare-ups. From a research standpoint, a heuristic of borderline pathology as an ever-changing condition opens up new avenues for investigating the causes of the development and progression of borderline PD symptoms. By the same token, conceptual and statistical models that recognize the fluid nature of borderline pathology can accelerate the hunt for etiological factors by isolating the signal of the stable core of borderline proneness amid transient changes in symptom expression.
Supplementary Material
Footnotes
Author Contributions
C.C.C. developed the study concept, performed data analyses, and drafted the report. A.E.H. and S.D.S. contributed to the study design and provided critical reviews of the analyses and manuscript. All authors approved the final version of the paper for submission.
The TSO model results were nearly identical in sensitivity analyses that included the affective lability item (results available upon request).
To evaluate whether borderline PD symptom stability varied by age, we simultaneously estimated TSO models using data from (i) ages 14 to 16 and (ii) ages 18 to 20. The percentages of total borderline PD variance due to the trait factor were 60–63% and 66–67%, respectively. A chi-square difference test demonstrated that those stability estimates did not differ significantly across early- and late-adolescence, χ2diff(1) = 1.18, p = .28. Thus, stable borderline proneness seems to account for similar proportions of individual differences during these two developmental stages.
References
- Bornovalova MA, Hicks BM, Iacono WG, McGue M. Stability, change, and heritability of borderline personality disorder traits from adolescence to adulthood: A longitudinal twin study. Development and Psychopathology. 2009;21:1335–1353. doi: 10.1017/S0954579409990186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA. Stability and change in personality disorder. Current Directions in Psychological Science. 2009;18:27–31. [Google Scholar]
- Cole DA. Coping with longitudinal data in research on developmental psychopathology. International Journal of Behavioral Development. 2006;30:20–25. [Google Scholar]
- Cole DA, Martin NC, Steiger JH. Empirical and conceptual problems with longitudinal trait-state models: Introducing a trait-state-occasion model. Psychological Methods. 2005;10:3–20. doi: 10.1037/1082-989X.10.1.3. [DOI] [PubMed] [Google Scholar]
- Distel MA, Trull TJ, Derom CA, Thiery EW, Boomsma DI. Heritability of borderline personality disorder features is similar across three countries. Psychological Medicine. 2008;38:1219–1229. doi: 10.1017/S0033291707002024. [DOI] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Keyes KM, Skodol AE, Hasin DS. Borderline personality disorder co-morbidity: Relationship to the internalizing–externalizing structure of common mental disorders. Psychological Medicine. 2011;41:1041–1050. doi: 10.1017/S0033291710001662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadow K, Sprafkin J. Adolescent Symptom Inventory 4 norms manual. Stony Brook, NY: Checkmate Plus; 1998. [Google Scholar]
- Gadow KD, Sprafkin J, Weiss M. Adult Self-Report Inventory-4 manual. Stony Brook, NY: Checkmate Plus; 2004. [Google Scholar]
- Gunderson JG, Bender D, Sanislow C, Yen S, Skodol AE. Plausibility and possible determinants of sudden “remissions” in borderline patients. Psychiatry. 2003;66:111–119. doi: 10.1521/psyc.66.2.111.20614. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Stout RL, McGlashan TH, Shea MT, Skodol AE. Ten-year course of borderline personality disorder: Psychopathology and function from the Collaborative Longitudinal Personality Disorders study. Archives of General Psychiatry. 2011;68:827–837. doi: 10.1001/archgenpsychiatry.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hipwell AE, Loeber R, Stouthamer-Loeber M, Keenan K, White HR, Kroneman L. Characteristics of girls with early onset disruptive and antisocial behaviour. Criminal Behaviour and Mental Health. 2002;12:99–118. doi: 10.1002/cbm.489. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- McGlashan TH, Grilo CM, Sanislow CA, Ralevski E, Pagano M. Two-year prevalence and stability of individual DSM-IV criteria for schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders: Toward a hybrid model of axis II disorders. American Journal of Psychiatry. 2005;162:883–889. doi: 10.1176/appi.ajp.162.5.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morey LC, Hopwood CJ. Stability and change in personality disorders. Annual Review of Clinical Psychology. 2013;9:499–528. doi: 10.1146/annurev-clinpsy-050212-185637. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus version 7. Los Angeles, CA: Muthén & Muthén; 1998–2014. [Google Scholar]
- Olatunji BO, Cole DA. The longitudinal structure of general and specific anxiety dimensions in children: Testing a latent trait-state-occasion model. Psychological Assessment. 2009;21:412–424. doi: 10.1037/a0016206. [DOI] [PubMed] [Google Scholar]
- Prenoveau JM, Craske MG, Zinbarg RE, Mineka S, Rose RD, Griffith JW. Are anxiety and depression just as stable as personality during late adolescence? Results from a three-year longitudinal latent variable study. Journal of Abnormal Psychology. 2011;120:832–843. doi: 10.1037/a0023939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde PL, Klein PM, Seeley DN, Gau JR. Key characteristics of major depressive disorder occurring in childhood, adolescence, emerging adulthood, and adulthood. Clinical Psychological Science. 2013;1:41–53. doi: 10.1177/2167702612457599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trull TJ. Structural relations between borderline personality disorder features and putative etiological correlates. Journal of Abnormal Psychology. 2001;110:471–481. doi: 10.1037//0021-843x.110.3.471. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Time to attainment of recovery from borderline personality disorder and stability of recovery: A 10-year prospective follow-up study. American Journal of Psychiatry. 2010;167:663–667. doi: 10.1176/appi.ajp.2009.09081130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Silk KR, Hudson JI, McSweeney LB. The subsyndromal phenomenology of borderline personality disorder: A 10-year follow-up study. American Journal of Psychiatry. 2007;164:929–935. doi: 10.1176/ajp.2007.164.6.929. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.