Abstract
Background
Intensive physical exercise (IPE) increases strength, lean body mass, aerobic capacity, and range of motion in children with extensive burns. However, whether IPE decreases the frequency of burn scar contracture-releasing procedures in children with extensive burns is unknown.
Materials and Methods
Prospectively collected surgical records of 184 children who had undergone axilla, elbow, and/or wrist contracture-releasing procedures were reviewed. All children were 7 years or older and had sustained burns of at least 40% of the total body surface area. Eighty-two children completed an IPE program, and 102 children did not. For both groups, the axilla, elbow, and wrist were examined for tightness and restricted movement. Children with contractural difficulty were prescribed a releasing procedure. Logistic regression was used to model the relationship between multiple release surgeries and group.
Results
Patients in both groups had comparable injury severity. A total of 120 releases were carried out in the 82 IPE patients. In contrast, 211 releases were needed in the 102 non-IPE patients. An approximate 60% decrease in the frequency of re-release operations was noted in IPE patients (12.5% for the IPE group and 31.9% for non-IPE group; p<0.05).
Conclusions
When used as an adjunct therapy in post-burn rehabilitation, IPE may be useful for reducing the need for contracture release. The mechanisms underlying the beneficial effects of exercise remain undefined and should be investigated.
Keywords: exercise, burns, joint contractures, contractural-releasing procedures
INTRODUCTION
In severely burned children, physical exercise improves muscle strength, lean body mass, aerobic capacity, and range of motion in joints.1–3 Similar findings have been reported in the adult population by Paratz et al.4 and de Lateur et al.5
In 2003, Celis et al.3 followed a small number of patients participating in 12 weeks of a supervised, in-hospital exercise program in combination with physical therapy and occupational therapy (PT/OT). They found that these patients needed fewer surgical interventions than their non-exercising counterparts who received only PT/OT at home. In particular, the number of patients requiring burn scar contracture release was significantly lower in the exercise group than in the standard of care (no exercise) group. However, in this small preliminary study, it is not clear if the numbers of surgeries were the total number of surgeries (cross-sectional) or if they were the total number of surgeries required for each patient (longitudinal). In addition, the surgical techniques were not described.
Despite the fact that these findings are generally supportive of incorporation of physical exercise into burn care, the efficacy of exercise programs in improving clinical outcomes related to scar contractures has not been established. This study was undertaken to clarify whether severely burned children who participate in an exercise program require less contracture-releasing procedures in upper body joints than those not participating in an exercise program.
METHODS
Patients
A total of 184 children participated in this study. All were 7 years or older and sustained burns greater than or equal to 40% of their total body surface area (TBSA). They had burn scar contractures that involved the axilla, elbow, and/or wrist. Of these 184 children, 82 participated in a 12-week intensive physical exercise (IPE) program, as approved by the site Institutional Review Board. The remaining children had injuries of similar severity but did not undergo the exercise treatment program (non-IPE, N=102). The co-authors were blinded to the patients’ IPE program participation. Children requiring contracture-releasing procedures later because of functional tightness were examined by the senior author, who also had no knowledge of patients’ prior exercise treatment regimen. Clinical manifestations of joint contracture (i.e., subjective and objective complaints of joint tightness) were the sole indication for the releasing procedure.
A randomization scheme was implemented a priori such that upon hospital admission, the patient’s group allocation was already established (non-IPE or IPE). Prior to enrollment, legal guardians provided consent by signing a written informed consent approved by the Institutional Review Board. Assent was obtained from children ≥ 7 years. At hospital discharge, the children were enrolled in the exercise program and housed in hospital-owned apartments or an apartment complex near the hospital for a period of 12 weeks. Children were seen daily Monday through Friday in the clinic by the nursing and physiotherapy staff for care (e.g., wound care, medications, hand splinting) when and if necessary. While physio-occupational treatments are a standard regimen for all patients (IPE and non-IPE), the patients in the IPE group were seen for an additional 1 hour every day for exercise training.
IPE program
The IPE program consisted of progressive, resistive, and aerobic exercise lasting 12 weeks. IPE involved a cardiovascular workout program that adhered to guidelines of the American College of Sports Medicine.6–9 The protocol for aerobic exercise consisted of an initial warm-up phase that lasted for 5 minutes and involved performing an activity that was light enough to yield a rated perceived exertion (RPE) of a “mild-to-light” aerobic effort.10–12 This activity was then followed with exercise activities such as walking/jogging on a treadmill, exercising on an elliptical, rowing, or cycling for at least 20 minutes. The aerobic intensity was set to elicit 60% to 85% of the patient’s peak heart rate obtained during the peak exercise treadmill test and an RPE reflective of a “moderately hard-to-hard” effort on Borg’s Scale (scale of 1–10). Finally, the intensity of exercise was decreased to an RPE of “mild” for 5 minutes of recovery. The aerobic training was performed 5 days every week.
Children also underwent 12 weeks of progressive resistance training 3 times a week. The activities consisted of the following 7 exercises: bench press, biceps curls, triceps curls, lateral pull down, knee extension exercises, hamstring curls, and abdominal curls. Each load was lifted 12 to 15 times, with 3 sets being performed. Each set was separated by a 1-minute rest period. The abdominal curls were done to maximal tolerance.
Non-IPE group
Children in the non-IPE group underwent a standard rehabilitative therapy consisting of PT/OT in a similar manner as the IPE group. In addition, they were housed in a similar manner as the IPE group, being accommodated in a facility readily accessible to the hospital. They participated in daily physio-occupational activities 5 days a week.3, 13 Once finished with PT/OT at the hospital, the non-IPE group returned to their permanent home with instructions to continue physiotherapy either at home under the supervision of their parents or guardians or in a private physiotherapy office/clinic if available.
Physical assessment and indications for surgical intervention
Children in both groups were examined by the senior author to ascertain the magnitude of scarring and contractural problems in the axilla, elbow, and wrist. Limitation in joint movement grossly attributable to scarring as well as subjective complaint of tightness and limitation in joint movement served as an indication for surgical intervention. Patients from both groups received additional PT/OT following the surgical treatment.
Surgical technique
A transpositional random fasciocutaneous flap technique (i.e., ¾ random fasciocutaneous Z-plasty) with or without supplementary use of partial-thickness skin graft was the primary method used to reconstruct the deformities.
Statistical methods
Between-group differences in age and TBSA burned were assessed by Mann-Whitney tests. Gender differences were assessed by chi-square test. A multiple logistic regression model was used to assess the effects upon whether a subject required single or multiple release surgeries due to the exercise participation group (IPE versus non-IPE), while adjusting for effects due to the demographic covariates gender, age, and TBSA burned. Statistical analysis was performed using R statistical software (R Core Team, 2013, version 3.0.1). A 95% level of confidence was assumed.
RESULTS
Patients in both groups were followed beginning at the year of surgery, with follow-up ranging from 0.5 to 10 years. The mean length of follow-up was 4.6 years for IPE children and 4.2 years for non-IPE children. As shown in the Table 1, the magnitude of burns was similar between the two groups. A significant difference was noted in age (p=0.026), though mean age differed by around only a year (10.9 years in non-IPE versus 12.2 years in IPE). Sex also differed between the non-IPE (60% male) and IPE groups (78% males, p=0.010). As expected, due to the children in the non-IPE group being relatively younger than the children in the IPE group, height, weight and body mass index were significantly lower in the non-IPE group. The initial BMI followed a similar pattern as the age. That is, patients in the IPE group tended to be older than those patients in the non-IPE group (mean age of 12.1years versus 10.9 years respectively; p < 0.026); taller (1.4 meters versus 1.1 meters respectively; p < 0.0001); heavier (40.8 kg versus 21.9 kg respectively; p < 0.0001); and with a higher BMI (19.1 kg/m2 versus 16.4 kg/m2 respectively; p < 0.0001).
Table 1.
| Characteristic | Non-IPE | IPE | P value |
|---|---|---|---|
| N | 102 | 82 | |
| Sex (M/F) | 81/54 | 64/18 | |
|
| |||
| Age (years) | 10.9 ± 3.5 | 12.1 ± 3.7 | P = 0.026 |
|
| |||
| TBSA Burned (%) | 61 ± 16 | 62 ± 16 | NS |
|
| |||
| Height (m) | 1.1 ±0.2 | 1.4 ± 0.2 | < 0.0001 |
|
| |||
| Weight (kg) | 21.9 ±11.2 | 40.8 ± 12.9 | < 0.0001 |
|
| |||
| BMI (kg/m2) | 16.4 ± 2.4 | 19.1 ± 5.2 | < 0.0001 |
|
| |||
TBSA, total body surface area. Values are means ± SD. NS = not significantly different between Non-IPE vs. IPE. BMI, body surface area
A total of 331 releasing procedures were performed to reconstruct contractural deformities involving the axilla, elbow, or wrist. Of these, 120 releases were carried out in the 82 IPE children, and 211 releases were needed in the 102 non-IPE children. The transpositional random fasciocutaneous flap technique produced satisfactory surgical outcomes at all sites.
Postoperative complications such as infection, flap necrosis, and bleeding were encountered in 5% to 8% of children (7.5% for IPE and 5.6% for non-IPE); however, these complications were seen only in children who had undergone axillary-releasing procedures (Table 2). The overall incidence of reoperation (2 or more operations) was reduced by approximately 60% in the IPE group (12.5%) compared to the non-IPE group (31.9%) (Table 3). The axilla was the site that most commonly required reoperation (Table 4).
Table 2.
Number of complications in each region
| Group | N | Region | ||
|---|---|---|---|---|
|
| ||||
| Axilla | Elbow | Wrist | ||
| IPE | 82 | 5/67 | 0/27 | 0/26 |
| Non-IPE | 102 | 6/108 | 0/45 | 0/58 |
Table 3.
Number of operations
| Group | N | Total number of releasing operations | Patients requiring ≥ 2 operations in one site (ie, recontractures) |
|---|---|---|---|
| IPE | 82 | 120 | 15 (12.5%) |
| Non-IPE | 102 | 211 | 67 (31.9%) |
Table 4.
Number of re-release operations by site
| Group | N | Re-Release Site* | ||
|---|---|---|---|---|
|
| ||||
| Axilla | Elbow | Wrist | ||
| IPE | 82 | 11 | 1 | 3 |
| Non-IPE | 102 | 48 | 7 | 12 |
Re-release defined as ≥ 2 operations.
Children who participated in the IPE exercise program had 3.6 times the odds of requiring only a single release surgery compared to non-IPE children (p=0.0003). Moreover, IPE patients had 1/3.6 or about one-third the odds of requiring multiple release surgeries compared to non-IPE patients. Male children had half the odds of requiring only a single surgery as compared to females (p=0.045). Neither age (p=0.62) nor TBSA burned (p=0.08) showed significant evidence of a relationship with the number of surgeries required.
DISCUSSION
Fully understanding the ramifications of physical problems arising from devastating injuries, namely the loss of body parts and scarring, is often difficult if not impossible. The task is especially difficult in those who have sustained severe burns; the magnitude of scarring and scar contractures can be so extensive that an accurate assessment of their future impact may not be possible. Although range of motion measured in an affected joint is the objective parameter most commonly used to assess the functional status of joints such as the axilla and knee, subjective complaints of scar tightness and scar thickness noted by the patients are seldom taken into account when assessing the difficulty.
Patients often complain of tightness felt in and around a joint such as the axilla, elbow, and wrist, especially in instances in which scar tissue has formed across a joint surface. This feeling of tightness is real even though the interference with joint movement may be minimal. This feeling of tightness is of key importance to the patient (i.e. patient-centered surgical need assessment) and caretaker and needs to be considered by the surgeon. The sensation of scar tightness may or may not appear immediately; it can appear in later years after the injury. Although the exact reason for the delay in manifestation is not entirely clear, return of bone growth, which is known to be delayed or underdeveloped during the period immediately following the injury, could account for the delayed onset of tightness. In this study, the need for re-release of a contracted axilla, for instance, was often delayed for 3 to 4 years; the average age at re-release was 10 years and the average time interval to the re-release was 4 years. Future studies could add more objective measures for the need for surgical intervention, however, the subjective feeling of tightness must not be underestimated.
We believe that description of technical details of the various surgical modalities used to manage scar contractures is beyond the scope of this paper. However, we note that in this study the skin flap technique was most effective as it follows the reconstructive principles of restoring a defective bodily structure with like tissues.
Physical exercise is defined as bodily activities designed to enhance health and general wellness.14 It is well established that a regimen of exercise can be used for ill individuals to increase muscle mass, thus improving muscular strength as well as cardiopulmonary capacities.15–21 In recent years, a short-term but intensive physical exercise regimen has been found to be similarly effective for individuals experiencing loss of lean body mass and cardiopulmonary dysfunction as a consequence of burn injuries.1, 22 Although the exact effect that IPE exerts upon scarring and scar contracture has not been elucidated, this study clearly shows that the need for surgery is lessened in children who have completed a regimen of IPE that involves the axilla, elbow, and/or wrist.
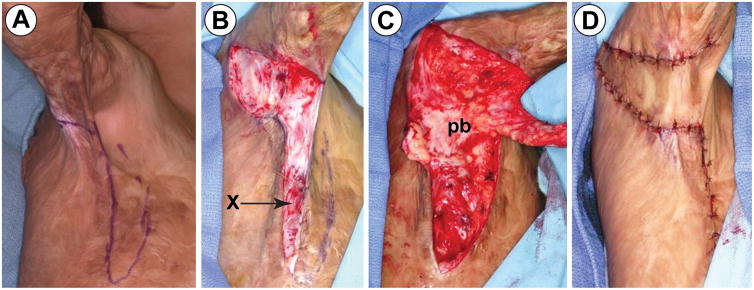
Figure 1.
Transpositional random fasciocutaneous flap technique: (A) Right triangle of skin showing the cathetus adjacent, which is perpendicular to the line of release. (B) An incision is made along the cathetus adjacent following the release of contracted area. The incision is continued down to the fascial layer and the fascia is anchored to the skin edge. (“x” mark). Identification of the vascular pedicle is not necessary. (C) A random fasciocutaneous flap is fabricated. Blunt dissection is used to mobilize the pedicle to minimize damage to the vascular pedicle. (D) The random fasciocutaneous flap is rotated 90° for flap inset. All wound edges are closed primarily.
Acknowledgments
Source of Funding: This research was supported by National Institute for Disabilities, Independent Living, and Rehabilitation Research (90DP0043-01-00); National Institutes of Health (P50 GM060388 and R01 HD049471) and Shriners of North America (71006, 71008, 71009, and 84080). This clinical trial is registered at Clincaltrials.gov (NCT00675714).
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest.
Ted T. Huang, MD Memorial
Dr. Ted T. Huang passed away on August 26th, 2016; too early for his countless pediatric patients. Some of whom had been his patients for many years. Dr. Huang came to Shriners Hospitals for Children-Galveston as a burn reconstructive surgeon in 1991. While there he developed the field of burn reconstruction for massively-burned children. His understanding and technical mastery of the entire scope of burn reconstruction were unquestioned, yet his “signature” operation was simple and the results most beneficial to the burned children.
Although he maintained utmost professionalism in his interactions with his patients, Dr. Huang considered and treated his patients as an extension of his family. When his international patients would return to see him, he looked over their photographic medical records as “Oggi” (Japanese grandfather). An appointment with him had a familiar basic routine: “Photos” (pointing to the wall next to the exam room door). Photos from previous encounters recalled for him what was special about the patient’s injury and scars. Often speaking with Spanish patients via an interpreter, he would say “Would you ask him to point to what bothers him the most, numbers 1 through 4.” Using about ten words, he and his patients could arrive at a clear mutual understanding of the problem and its surgical treatment. He instinctively knew what troubled his patients.
He had an uncanny comprehension of his patients’ perspective, and he recommended treatments that were implicitly acceptable to them. “I hate pain,” he would say, reflecting his expression of simple compassion. This also led Dr. Huang to drastically simplify procedures and post-operative care. To him a physician’s duty required right understanding of what was acceptable, mentally and physiologically, to each individual patient.
Dr. Huang loved scientific inquiry, and applied it often, first in microbiology and surgical physiology, and later in the review of his case logs, practice, and outcomes. In his written work, like his work with patients, the self-evident results spoke for themselves. Dr. Huang was fascinated with life and healing. The world of burn reconstruction has lost a most dedicated and altruistic surgeon, but his work will live on through the myriad of patients that he cared for and that he benefited.
References
- 1.Suman OE, Spies RJ, Celis MM, et al. Effects of a 12-wk resistance exercise program on skeletal muscle strength in children with burn injuries. J Appl Physiol (1985) 2001;91:1168–1175. doi: 10.1152/jappl.2001.91.3.1168. [DOI] [PubMed] [Google Scholar]
- 2.Cucuzzo NA, Ferrando A, Herndon DN. The effects of exercise programming vs traditional outpatient therapy in the rehabilitation of severely burned children. J Burn Care Rehabil. 2001;22:214–220. doi: 10.1097/00004630-200105000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Celis MM, Suman OE, Huang TT, et al. Effect of a supervised exercise and physiotherapy program on surgical interventions in children with thermal injury. J Burn Care Rehabil. 2003;24:57–61. doi: 10.1097/00004630-200301000-00014. discussion 56. [DOI] [PubMed] [Google Scholar]
- 4.Paratz JD, Stockton K, Plaza A, et al. Intensive exercise after thermal injury improves physical, functional, and psychological outcomes. J Trauma Acute Care Surg. 2012;73:186–194. doi: 10.1097/TA.0b013e31824baa52. [DOI] [PubMed] [Google Scholar]
- 5.de Lateur BJ, Magyar-Russell G, Bresnick MG, et al. Augmented exercise in the treatment of deconditioning from major burn injury. Arch Phys Med Rehabil. 2007;88:S18–23. doi: 10.1016/j.apmr.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Pescatello LS, editor. ACSM’s Guidelines for Exercise Testing and Prescription. Philadelphia: Lippincott Williams & Wilkins; 2013. General principles of exercise prescription; pp. 162–191. No authors. [Google Scholar]
- 7.Przkora R, Herndon DN, Suman OE. The effects of oxandrolone and exercise on muscle mass and function in children with severe burns. Pediatrics. 2007;119:e109–116. doi: 10.1542/peds.2006-1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Suman OE, Mlcak RP, Herndon DN. Effect of exercise training on pulmonary function in children with thermal injury. J Burn Care Rehabil. 2002;23:288–293. doi: 10.1097/00004630-200207000-00013. discussion 287. [DOI] [PubMed] [Google Scholar]
- 9.Suman OE, Thomas SJ, Wilkins JP, et al. Effect of exogenous growth hormone and exercise on lean mass and muscle function in children with burns. J Appl Physiol (1985) 2003;94:2273–2281. doi: 10.1152/japplphysiol.00849.2002. [DOI] [PubMed] [Google Scholar]
- 10.Borg G. Ratings of perceived exertion and heart rates during short-term cycle exercise and their use in a new cycling strength test. Int J Sports Med. 1982;3:153–158. doi: 10.1055/s-2008-1026080. [DOI] [PubMed] [Google Scholar]
- 11.Borg G. Borg’s Perceived Exertion and Pain Scales. Champaign: Human Kinetics; 1998. [Google Scholar]
- 12.Borg G, Hassmen P, Lagerstrom M. Perceived exertion related to heart rate and blood lactate during arm and leg exercise. Eur J Appl Physiol Occup Physiol. 1987;56:679–685. doi: 10.1007/BF00424810. [DOI] [PubMed] [Google Scholar]
- 13.Porro LJ, Al-Mousawi AM, Williams F, et al. Effects of propranolol and exercise training in children with severe burns. J Pediatr. 2013;162:799–803. e791. doi: 10.1016/j.jpeds.2012.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American College of Sports Medicine Position Stand. The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30:975–991. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]
- 15.Feigenbaum MS, Pollock ML. Prescription of resistance training for health and disease. Med Sci Sports Exerc. 1999;31:38–45. doi: 10.1097/00005768-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Faigenbaum AD, Zaichkowsky LD, Westcott WL, et al. The effects of a twice-a-week strength training program on children. Pediatr Exerc Sci. 1993;5:339–346. [Google Scholar]
- 17.Falk B, Tenenbaum G. The effectiveness of resistance training in children. A meta-analysis. Sports Med. 1996;22:176–186. doi: 10.2165/00007256-199622030-00004. [DOI] [PubMed] [Google Scholar]
- 18.Hass CJ, Feigenbaum MS, Franklin BA. Prescription of resistance training for healthy populations. Sports Med. 2001;31:953–964. doi: 10.2165/00007256-200131140-00001. [DOI] [PubMed] [Google Scholar]
- 19.Scheuer J, Tipton CM. Cardiovascular adaptations to physical training. Annu Rev Physiol. 1977;39:221–251. doi: 10.1146/annurev.ph.39.030177.001253. [DOI] [PubMed] [Google Scholar]
- 20.Rogers MA, Yamamoto C, Hagberg JM, et al. Effect of 6 d of exercise training on responses to maximal and sub-maximal exercise in middle-aged men. Med Sci Sports Exerc. 1988;20:260–264. doi: 10.1249/00005768-198806000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Hagberg JM, Ehsani AA, Holloszy JO. Effect of 12 months of intense exercise training on stroke volume in patients with coronary artery disease. Circulation. 1983;67:1194–1199. doi: 10.1161/01.cir.67.6.1194. [DOI] [PubMed] [Google Scholar]
- 22.Hardee JP, Porter C, Sidossis LS, et al. Early rehabilitative exercise training in the recovery from pediatric burn. Med Sci Sports Exerc. 2014;46:1710–1716. doi: 10.1249/MSS.0000000000000296. [DOI] [PMC free article] [PubMed] [Google Scholar]