Abstract
Objectives
The purpose of this study was to develop a comprehensive back school program that included elements of CBT (Cognitive Behavioral Therapy), implement this through multidisciplinary collaboration, and ascertain its effectiveness as a pilot study.
Design
This school was implemented in the form of five 90-minute group sessions held every other week.
Methods
Participants comprised 7 chronic low back pain patients with poor improvement in the usual treatment. Practitioners were orthopaedic surgeon, physical therapist, and a clinical psychologist. This school contents were patient education, self-monitoring, back exercise, relaxation, stress management, cognitive restructuring, activity pacing, and exposure.
Results
From the Wilcoxon signed-rank test, each score of four scales or items (sense of control, PCS (pain catastrophizing), PASS-20 (escape/avoidance), FFD (finger-floor distance)) after this program significantly improved. Results of calculating the effect size, sense of control (d=0.55) is ‘moderate’, the PCS (d=1.12) and the PASS-20 (d=1.64) were ‘large’.
Conclusions
This back school may be useful for physical function and psychological variables which much related to pain management and daily disabilities in patients with poor respond to standard orthopaedic treatment.
Keywords: chronic pain, back school, multidisplinary collaboration, cognitive behavioral therapy (CBT), activities of daily living (ADLs)
Introduction
International studies have found that the prevalence of chronic pain is extremely high, at 17.1%1). This has a massive effect not only on patients themselves, but on their families, schools or workplaces, and society at large, and chronic pain is a physical condition that is a major issue in clinical settings. The prevalence in Japan is also high: Matsudaira et al.2) and Yabuki et al.3) reported a rate of approximately 22.9% and 22.5% respectively, meaning that one in approximately five Japanese is suffering from chronic pain. In Japan, back pain has a high lifetime incidence of 83.4%4). Kawakami5), who carried out a questionnaire survey of chronic back pain patients approximately 6 months after their initial examinations, found that almost all had discontinued treatment without an accurate outcome having been recorded, and that after 6 months, no patient responded that their pain had improved, 22.2% responded that it had improved temporarily but sometimes recurred, and 77.8% responded that they still had pain. A therapeutic approach that results in adequate improvement for chronic back pain patients has thus yet to be established within the current treatment system in Japan, and urgent measures are needed.
Back school, a group intervention program for chronic back pain patients, is a recommended form of therapy6) that has been shown in meta-analyses to be effective in improving pain symptoms and physical function7). The method and content of existing back school, however, vary in different medical institutions, and there is an issue that their mechanism of improvement is unclear. While supporting the beneficial effect of back school on symptoms and limitations on activities of daily living (ADLs), some studies have also pointed out that their actual effect is unclear8).
In around 85% of cases, the cause of chronic back pain is unknown, and in a large proportion of cases, psychosocial factors are responsible for pain symptom maintenance9), so it is said that biopsychosocial therapy is essential in addition to physiotherapy and drug therapy. Cognitive behavioral therapy (CBT) is one form of biopsychosocial therapy that has been shown to be effective in treating a range of problems associated with chronic pain, including pain symptoms and limitations on activities of daily living (ADLs)10,11). According to a review of interdisciplinary treatment for chronic pain, all studies included elements of CBT12), and CBT plays a central role in the treatment of chronic pain. The purpose of treatment for chronic pain patients is not to eliminate their pain completely, but rather to reduce limitations on ADLs, in other words, to improve their quality of life (QOL), and it is thought that alleviating limitations on ADLs can prevent pain from becoming chronic13). In particular, important factors for symptom maintenance in chronic pain are catastrophic thinking, which is the negative cognition of pain, and escape/avoidance behavior, which is an inappropriate way of dealing with pain, and improvement of both factors is the objective of CBT. Programs that aim to improve catastrophic thinking about pain and escape/avoidance behavior are actually being implemented overseas, and some studies have reported that they are effective14-17). However, there has yet to be a study of the efficacy of a comprehensive program incorporating the elements of CBT described above into the existing back school.
In addition, multidisciplinary collaboration in biopsychosocial therapy for chronic pain is regarded as desirable18), and, since CBT has been shown to be a form of psychotherapy that is effective for chronic pain, as described above, its use in back pain classes is essential from the psychological perspective. The back school that has been the subject of previous studies, however, consisted almost entirely of interventions by orthopaedic surgeons or physiotherapists, and none involved a professional with a psychological perspective or provided CBT content.
Therefore, the objective of this study was to develop a comprehensive program of back pain classes that included elements of CBT, implement this through multidisciplinary collaboration, and ascertain its effectiveness.
Methods
The analysis set comprised 7 adult chronic back pain patients who were attending outpatient clinics in the Department of Orthopaedic Surgery of a university hospital near an urban area and who provided complete responses to the survey materials. Specifically, they comprised chronic pain patients who had suffered from persistent back pain for ≥6 months that was not adequately explained by organic findings and that responded poorly to standard orthopaedic surgical treatment and conservative treatment.
The program was implemented in the form of five 90-minute group sessions held every other week. Written materials including that week’s content were prepared for and used in each session. Session 1 was educational session. We gave participants the information about explanation of factors associated with back pain and the mechanism of symptom maintenance. Session 2 was back pain exercise and general physical movement to prevent participants to hurt their low back and maintain their muscle to work. Session 3 and 4 were the parts of learning methods of dealing with back pain including self-monitoring, relaxation, cognitive restructuring, exposure, and activity pacing. Self-monitoring, what is called “back pain diary”, was to write the changes of pain severity, frequency and pain related disability per day participants had. It was so important for them to recognize their objective symptoms and daily burden. And the progressive relaxation technique, which often used for pain management, was taught as a measure to cope with back pain. Cognitive restructuring was the content to modify the participants’ catastrophic thoughts about pain. In clinical situations, we identified the situations, the moods and the thoughts of the moment when patients’ feel pain and examined their validity. Finally, we aimed that patients could achieve adaptive and flexible perceptions about pain. The content of exposure was for participants to act escape/avoidance behaviors, which they couldn’t practice because they fear of pain. And, activity pacing was the approach that participants kept amount or time of activity constant to prevent them from becoming physical load. Session 5, at the end of this program, was summary which we reviewed past four sessions and make sure of further points to keep in mind in the future.
All sessions were led by a clinical psychologist, with an orthopaedic surgeon also leading Sessions 1 and 5 and a physiotherapist leading Session 2. Also, all patients received orthopaedic treatment as usual (TAU) in addition to this program. It was the conservative treatment including pharmacological therapy and nerve block.
Survey Materials are Data from Interview Sheet/Medical Records, Pain Disability Assessment Scale (PDAS), Japanese version19), Pain Catastrophizing Scale (PCS), Japanese version20), Pain Anxiety Symptoms Scale (PASS-20), Japanese version21), and Physical function. Data from Interview Sheet/Medical Records are Disease duration, frequency of pain (days per month), severity of pain (mean severity assessed on an 11-point scale, from 0=no pain at all to 10=greatest possible pain), and sense of pain control (subjective sense of control assessed on an 11-point scale, from 0=no control at all to 10=extremely well controlled). The PDAS is a 20-item, 4-point scale that measures limitations imposed by chronic pain on ADLs (minimum score 20 points, maximum score 80 points) and provides a simple scale for measuring the degree of limitations on ADLs related to actual physical movement and mobility in the everyday living situations of chronic pain patients. The mean PDAS score for chronic pain patients is 17.3±13.6 points19). The PCS is a 13-item, 5-point scale that measures catastrophic thinking about pain (minimum score 0 points, maximum score 52 points). It has three subscales, comprising rumination, helplessness, and magnification, which respectively reflect the degree to which respondents think repeatedly about pain, feel overwhelmed by it, and are threatened by the perception of pain. The mean score for chronic pain patients is 24.29±13.20 points22). The PASS-20 is a 20-item, 6-point scale that measures fear of pain. It has four subscales which are cognitive anxiety, fear, physiological anxiety, and escape/avoidance. In this study, only the five items in the “escape/avoidance behavior” subscale were used in the analysis (minimum score 0 points, maximum score 25 points). The “escape/avoidance behavior” subscale of the PASS-20 is considered to reflect the concept of escape and avoidance behaviors that explain the transformation of pain into chronic pain. Indeed, several previous studies related to pain chronicity or aggravation are also use only this scale to analyze the consistency of the pain model or the effect of the treatment23,24). The mean score for chronic pain patients is 12.84 points25). As physical function, we assessed Grip strength (dominant hand) and finger-floor distance (FFD) which were used as objective measures of muscle strength and trunk function.
In conducting the study, written, informed consent was obtained from the study participants on the basis of an oral and written explanation of the content of the study to the participants. In addition to the study objective, the consent form specifically stated that participants were free to withdraw from the study, that data would be used for medical purposes, and that personal information would be protected. This study was screened and approved by the Ethics Committee of the institution where it was performed.
IBM SPSS 19.0 was used for statistical analysis. The effect size was calculated from the values for each indicator before and after the program. According to Cohen26), an effect size of 0.20 is considered to be “small,” 0.50 “moderate,” and 0.80 “large.”
Results
(1) Subject Basic Attributes, Pain Symptoms, sense of control, and Limitations on ADLs
Table 1 shows the basic attributes of the 7 subjects (3 men, 4 women, mean age 65.29±3.54 years). The orthopaedic diagnosis (including multiple diagnoses) was lumbar spinal stenosis in 4 cases, lumbar disc herniation in 2 cases, lumbar spondylosis in 2 cases, and lumbar intervertebral arthropathy in 1 case. Two subjects had concomitant psychiatric conditions. The mean disease duration was 9.71±1.41 years.
Table 1.
Characteristcs of subjects
| case | sex | age | orthopaedic diagnosis | psychiatric comorbidity | duration (year) |
| 1 | F | 70 | lumbar spinal stenosis | none | 5 |
| 2 | F | 75 | lumbar spondylosis
lumbar facet disorder |
insomnia
anxiety neurosis |
4 |
| 3 | M | 70 | lumbar disc hernia | bipolar affective disorder
hypochondriasis |
34 |
| 4 | F | 56 | lumbar spinal stenosis | none | 4 |
| 5 | F | 58 | lumbar spinal stenosis | none | 9 |
| 6 | M | 63 | lunbar spondylosis | none | 9 |
| 7 | M | 65 | lumbar spinal stenosis
lumbar disc hernia |
none | 3 |
Table 2 shows changes in the frequency and severity of pain. The frequency decreased in 1 subject and was unchanged in 6 after the program compared with before the program. The severity decreased in 5 subjects, unchanged in 1, and increased in 1. The changes of pain frequency and severity between before and after the program were not significant with Wilcoxon signed-rank test. Changes in sense of control are shown in Table 2. Among the 7 subjects, it increased in 5, unchanged in 1, and decreased in 1, and sense of control increased significantly (Z=-1.81, p<.10). The effect size was d=0.55.
Table 2.
Changes in pain symptoms (frequency and severity) and sense of pain control
| case | frequency | severity | sense of pain control | |||
| pre | post | pre | post | pre | post | |
| 1 | 30 | 30 | 7 | 6 | 5 | 6 |
| 2 | 30 | 30 | 7 | 5 | 6 | 5 |
| 3 | 25 | 30 | 2 | 7 | 4 | 5 |
| 4 | 20 | 20 | 5 | 3 | 2 | 5 |
| 5 | 30 | 30 | 7 | 4 | 7 | 7 |
| 6 | 30 | 30 | 6 | 2 | 1 | 3 |
| 7 | 30 | 30 | 6 | 6 | 4 | 6 |
Note. frequency:frequency of pain (days per month) severity:severity of pain (mean severity assessed on an 11-point scale, from 0=no pain at all to 10=greatest possible pain) sense of control:sense of pain control (subjective sense of control assessed on an 11-point scale, from 0=no control at all to 10=extremely well controlled)
Figure 1 shows changes of PDAS scores. The PDAS score decreased in 6 subjects and increased in 1 after the program compared with before the program. Before the program, 6 subjects had scored above the mean score for chronic pain patients (17.3±13.6), but after the program this number had decreased to 3. However, the PDAS score showed no significant difference.
Fig. 1.
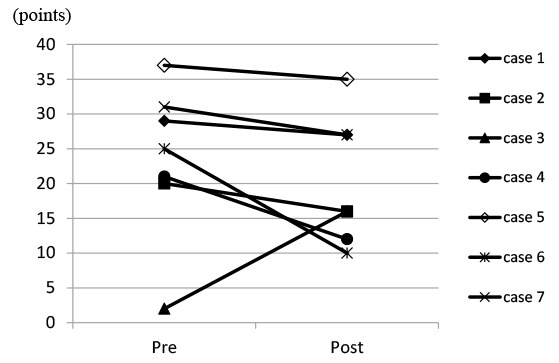
Changes of the PDAS (Pain Disability Assessment Scale) score in each patient.
PDAS score decreased in 6 subjects and increased in 1 after the program compared with before the program.
(2) Pain Cognition and Behavior and Physical Function
Figures 2 and 3 show changes of the PCS and PASS-20 “escape/avoidance behavior” scores. Both scores decreased in 6 subjects after the program. Before the program, 6 subjects had scored above the mean PCS score of chronic pain patients, but after the program this number had decreased to 2. On the other hand, with respect to the PASS-20 “escape/avoidance behavior” score, all 7 subjects had scored above the mean score of chronic pain patients before the program, but after the program all their scores had decreased or stayed unchanged, but 3 were still above the mean score. The scores of the PCS and escape/avoidance decreased significantly through this program (PCS: Z=1.87, p<.10; escape/avoidance: Z=2.21, p<.05). The effect size was d=1.12 for PCS and d=1.64 for PASS-20 “escape/avoidance behavior,” both “large” effects.
Fig. 2.
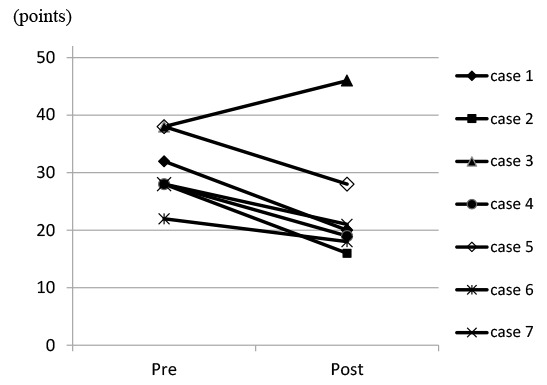
Changes of the PCS (Pain Catastrophizing Scale) score in each patient.
PCS score decreased in 6 subjects and increased in 1 after the program compared with before the program.
Fig. 3.
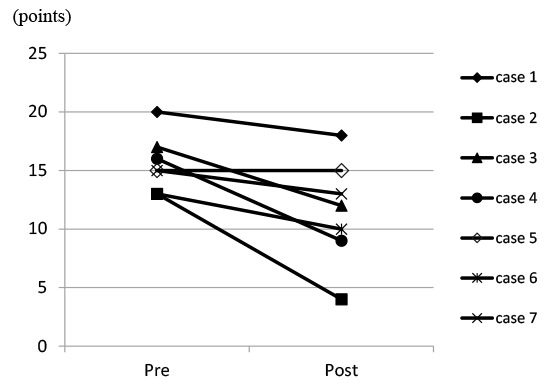
Changes of the escape/avoidance score in each patient.
Escape/avoidance score decreased in 6 subjects and stayed unchanged in 1 after the program compared with before the program.
Table 3 shows changes of FFD and grip strength. After the program, 6 subjects had improved FFD and 3 had improved function in terms of grip strength. Only FFD improved significantly (Z=-2.20, p<.05) and the effect size were d=0.31.
Table 3.
Changes in physical function (FFD and grip strength)
| case | FFD (cm) | grip strength (Kg) | ||
| pre | post | pre | post | |
| 1 | 7.3 | 13.7 | 26.5 | 26.2 |
| 2 | -20.3 | -16.8 | 20.2 | 19.5 |
| 3 | -11.0 | -12.0 | 34.7 | 36.9 |
| 4 | -4.3 | -0.7 | 21.5 | 21.4 |
| 5 | -26.3 | -25.0 | 31.3 | 40.1 |
| 6 | -23.3 | -19.3 | 29.7 | 22.1 |
| 7 | -16.7 | -9.0 | 32.9 | 43.0 |
Note. FFD:finger-floor distance
Discussion
The objective of this study was to develop a comprehensive program of back school that included elements of CBT, implement this through multidisciplinary collaboration, and ascertain its effectiveness. The results suggested that back school that focus on improving catastrophic thinking about pain and escape/avoidance behavior might produce certain short-term improvement in the FFD, as well as in psychological variables (sense of control, catastrophic thinking about pain, and escape/avoidance behavior). This suggested that this program might be effective against chronic pain that responds poorly to standard orthopaedic treatment. The effect size was “large” for catastrophic thinking about pain and escape/avoidance behavior and “moderate” for sense of control, but “small” for FFD. This showed that, although this program had a major effect on negative cognition of pain and behavior during the course of the program, its effect on pain symptoms, symptom-associated limitations on ADLs, and physical function was small. The cognitive behavioral model of explaining symptom maintenance in chronic pain holds that changing the cognition of pain and behavior leads to reduced limitations on ADLs and the alleviation of pain symptoms13). In this model, it is thought that correcting thinking and behavior should improve limitations on ADLs and result in the alleviation of symptoms, but in our program, there was little change in limitations on ADLs. With respect to physical function, although back school focusing on muscle-strengthening exercises led by staff of rehabilitation departments with the aim of preventing back pain have resulted in some improvement in FFD and other measures of flexibility and muscle strength after the program, this change was not significant27). Even programs not aimed at back pain patients that are tailored to improving physical function fail to produce sufficient improvement, and the “small” effect size for physical function in the present study is therefore understandable. It is possible that it may require some time for the changes in cognition of pain and behavior that were the focus of this study to extend their effect to pain symptoms, limitations on ADLs, and physical function. Implementing this program may thus be expected to promote behavior that had formerly been restricted by pain symptoms as a result of practicing what was taught in the program in actual everyday situations, leading to changes in limitations on ADLs and physical function. Self-efficacy, the belief that things will be alright, is an important part of pain management and improvements in self efficacy also lead to increases in ADLs and physical function28). Moderate improvement in sense of control that resulted from this program may help lead to good outcomes from future treatment.
Looking at the results of the present study in terms of the changes in scores for each scale, starting with PDAS, the number of subjects who scored above the mean score of chronic pain patients was halved by this program. The 3 subjects who still scored over the mean score after the program all had PDAS scores of ≥27, 0.5 SD or more above the mean score, indicating that they still felt severely limited in their ADLs. With respect to PCS scores, 2 subjects still scored above the mean score of chronic pain patients after the program, but 4 of 7 had scores at or below the mean score of healthy individuals in Japan (20.14 points)20), indicating that the number of people whose understanding of pain had improved to around the same level as that of healthy individuals by the program had increased. PASS “escape/avoidance behavior” scores decreased after the program in all subjects, and the number of subjects who scored above the mean score decreased to 3. Of the 4 subjects who scored under the mean score, 3 had scores at or below the mean score for healthy individuals in Japan (10.82 points)21). These results suggested that implementing this program not only had a major effect on cognition of pain and behavior, but also in fact improved them to around the same level as in healthy individuals. However, some subjects still scored highly on limitations on ADLs, despite some reduction in their scores, suggesting that these sessions alone failed to result in sufficient improvement particularly for subjects with severe ADL limitations. In concrete terms, it may be important to increase the number of sessions devoted to back pain exercises, cognitive restructuring, and exposure, which in our program were only covered in Sessions 1 and 2, in order to encourage the assimilation of cognitive and behavioral changes. Although the back school in this study focused on transforming the cognition of pain and behavior, CBT for chronic pain may also incorporate sessions for improving factors that may modify subjects’ pain symptoms, such as assertiveness training, anger management, and stress management29). The use of additional sessions for subjects for whom back pain classes alone were insufficiently effective must also be considered.
An investigation of changes in individual cases found that the pattern of program-associated changes seen in Subject 3 differed from those of the other 6 subjects. Therefore, it is thought that, although the PASS “escape/avoidance behavior” score decreased after the program, frequency and severity were both exacerbated, PCS and PDAS scores both increased, and no effect was evident. Subject 3 had suffered from pain for 34 years, exceptionally longer than any of the other subjects, and was also subject to the concomitant psychiatric conditions of bipolar affective disorder and hypochondriasis, as well as being emotionally unstable, which may have made it difficult to reflect appropriately on physical symptoms. Murakami30) pointed out that chronic pain patients who also suffer from psychiatric conditions are particularly difficult to treat. The present results suggest that at least disease duration and presence or absence of concomitant psychiatric conditions must be taken into account when considering the subjects of short-term group programs such as the one used in the present study.
The limitations of this study include the facts that it was an open study of a small analysis set, which made quantitative analysis difficult and limited the conclusions that can be reached. The effect was also evaluated solely in terms of symptoms and psychological factors. The former problem could be resolved by increasing the number of subjects to secure a number sufficient to withstand quantitative analysis and by setting up a control group in order to investigate the effect of the program more fully. The latter would require an investigation of medium- to long-term changes in objective indices, such as number of days of hospital attendance and treatment costs, in addition to symptoms and psychological factors. Evidence on this point is inconsistent, with some previous studies having found an effect31), whereas others have not8), and such a study could be expected to provide new information.
Notwithstanding these limitations, this study is thought to be highly significant because it demonstrated certain effects obtained by a multidisciplinary, systematic program of CBT-based back school that were not known previously.
Acknowledgments/ Conflict of Interest Disclosure
The present study was supported by JSPS Grant-in-Aid for Young Scientists (B) (Number 24730586) which Ryo Motoya received. Other than that, the authors declare that they have no competing interests.
Note
Part of this article have been already published as the review paper in Japanese. It was request paper and not peer reviewed one. (Pain Clinic, 37: 1269-76, 2016)
References
- 1.Ohayon MM, Schatzberg AF. Using chronic pain to predict depressive morbidity in the general population. Arch Gen Psychiatry, 60: 39-47, 2003. [DOI] [PubMed] [Google Scholar]
- 2.Matsudaira K, Takeshita K, Kusanogi J, et al. Prevalence and characteristics of chronic pain in the general Japanese population—Pain Associated Cross-sectional Epidemiological (PACE) survey 2009. JP—. (in Japanese) Pain Clinic, 32: 1345-56, 2011. [Google Scholar]
- 3.Yabuki S, Ushida T, Takeshita K, et al. : A national survey of patients with chronic pain in Japan (in Japanese). Clin Orthop (Rinsho Seikeigeka), 47: 127-134, 2012. [Google Scholar]
- 4.Fujii T, Matsudaira K. Prevalence of low back pain and factors associated with chronic disabling back pain in Japan. Eur Spine J, 22: 432-8, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kawakami T. The self-care and prevention of acute low back pain. (in Japanese) MB Orthop, 18: 10-16, 2005. [Google Scholar]
- 6.Burton AK, Balague F, Cardon, G, et al. Chapter 2 European guidelines for prevention in low back pain. Eur Spine J, 15: S136-S168, 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heymans MW, van Tulder MW, Esmail R, Bombardier C & Koes BW. Back schools for non-specific low-back pain. Cochrane database Syst Rev, 2, 2011. [DOI] [PubMed] [Google Scholar]
- 8.Brox JI, Stroheim K, Grotle M, Tveito TH, Indahl A & Eriksen HR. Systematic review of back schools, brief education, and fear-avoidance training for chronic low back pain. Spine J, 8: 948-58, 2008. [DOI] [PubMed] [Google Scholar]
- 9.Nakai Y. What is chronic pain ? (in Japanese) Jpn Med J, 3772: 7-12, 1996. [Google Scholar]
- 10.Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomized controlled trial of cognitive behavior therapy and behavior therapy for chronic pain in adults, excluding headache. Pain, 80: 1-13, 1999. [DOI] [PubMed] [Google Scholar]
- 11.Williams ACDC, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults (Review). Cochrane database Syst Rev, 11, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scascighini L, Toma V, Dober-Spielmann S, Sprott H. Multidisciplinary treatment for chronic pain: A systematic review of interventions and outcomes. Rheumatol, 47: 670-8, 2008. [DOI] [PubMed] [Google Scholar]
- 13.Leeuw M, Goossens MEJB, Linton SJ, Crombez G, Boersma K & Vlaeyen JWS. The fear-avoidance model of musculoskeletal pain: Current state of scientific evidence. J Behav Med, 30: 77-94, 2007. [DOI] [PubMed] [Google Scholar]
- 14.de Jong JR, Vlaeyen JWS, Onghena P, Cuypers C, den Hollander M & Ruijgrok J. Reduction of pain-related fear in complex regional pain syndrome type I: The application of graded exposure in vivo. Pain, 116: 264-75, 2005. [DOI] [PubMed] [Google Scholar]
- 15.Nelson PJ, Tucker S. Developing an intervention to alter catastrophizing in persons with fibromyalgia. Orthop Nurs, 25: 205-14, 2006. [DOI] [PubMed] [Google Scholar]
- 16.Smeets RJEM, Vlaeyen JWS, Kester ADM, Knottnerus JA. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. J Pain, 7: 261-71, 2006. [DOI] [PubMed] [Google Scholar]
- 17.Woods MP, Asmundson GJG. Evaluating the efficacy of graded in vivo exposure for the treatment of fear in patients with chronic back pain: A ramdomized controlled clinical trial. Pain, 136: 271-80, 2008. [DOI] [PubMed] [Google Scholar]
- 18.Ushida T, Arai K. 33 Multimodality treatment system In: Ogawa S, editor. Attack on chronic pain distressed the patients. (in Japanese) Tokyo: Japan Medical Journal, 201-8, 2014. [Google Scholar]
- 19.Arimura T, Komiyama H, Hosoi M. Pain Disability Assessment Scale (PDAS) —A simplified scale for clinical use—. (in Japanese) Jap J Behav Ther, 23: 7-15, 1997. [Google Scholar]
- 20.Matsuoka H, Sakano Y. Assessment of cognitive aspect of pain: Development, reliability, and Validation of Japanese version of pain catastrophizing scale. (in Japanese) Jpn J Psychosom Med, 47: 95-102, 2007. [Google Scholar]
- 21.Matsuoka H, Sakano Y. Development and validation of Japanese version of Pain Anxiety Symptoms Scale-20. (in Japanese) Jpn J Behav Med, 14: 1-7, 2008. [Google Scholar]
- 22.Sullivan MJL, Thibault P, Andrikonyte J, Butler H, Catchlove R & Lariviere C. Psychological influences on repetition-induced summation of activity-related pain in patients with chronic low back pain. Pain, 141: 70-8, 2009. [DOI] [PubMed] [Google Scholar]
- 23.Asmundson GJG, Norton PJ, Norton GR. Beyond pain: the role of fear and avoidance in chronicity. Clin Psycho Rev, 19: 97-119, 1999. [DOI] [PubMed] [Google Scholar]
- 24.Dannecker EA, George SZ. A comparison of laboratory measures of escape and avoidance behavior. J Pain, 10: 53-59, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCracken LM, Dhingra L. A short version of the Pain Anxiety Symptoms Scale (PASS-20): Preliminary development and validity. Pain Res Manage, 7: 45-50, 2002. [DOI] [PubMed] [Google Scholar]
- 26.Cohen J. Statistical power analysis for the behavioral science. New York: Academic Press; 1977. [Google Scholar]
- 27.Sawada S, Hayashi H, Sato K, Umino J. The suggestion of the lumbago prevention exercises that can be continued in the workplace. (in Japanese) Jpn J Occup Med Traumatology, 58: 24-8, 2009. [Google Scholar]
- 28.Woby SR, Urmston M, Watson PJ. Self-efficacy mediates the relation between pain-related fear and outcome in chronic low back pain patients. Eur J Pain, 11: 711-8, 2007. [DOI] [PubMed] [Google Scholar]
- 29.Otis JD. Managing chronic pain —A cognitive-behavioral therapy approach—Therapist guide. Oxford; Oxford University Press; 2007. [Google Scholar]
- 30.Murakami S. Treatment of psychiatric co-morbidity in chronic pain (in Japanese). Jpn J Clin Psychiatr, 42: 765-9, 2013. [Google Scholar]
- 31.Shirado O, Ito T, Kikumoto T, Takeda N, Minami A & Strax TE. A novel back school using a multidisciplinary team approach featuring quantitative functional evaluation and therapeutic exercises for patients with chronic low back pain. Spine, 30: 1219-25, 2005. [DOI] [PubMed] [Google Scholar]


