Abstract
Thoracic outlet syndrome (TOS) was first introduced in literature by Peet et al. in 1956. Since then is has been studied extensively and subcategorized into at least four closely related syndrome. Neurogenic TOS due to the compression of brachial plexus, arterial TOS in cases of compression of the subclavian artery, venous TOS in cases of compression of the subclavian vein, and non-specific type of TOS. Neurogenic TOS is by far the most common consisting of 95% of the cases, followed by venous and lastly arterial. Arterial TOS comprises ~1% of all TOS cases, they are caused largely by presence of cervical rib and/or anomalies of first rib. Here we describe arterial TOS caused by hypertrophy of the anterior scalene muscle in a 65-year-old male. Patient underwent successful open surgical repair with Dacron interposition graft. Postoperative course was unremarkable. Patient was discharged home on POD 2.
INTRODUCTION
Clinical presentation of arterial thoracic outlet syndrome (TOS) can be variable ranging from pain on the affected arm, numbness or tingling or limb threatening distal embolization. A thorough physical exam is crucial. Typically a CT angiography is diagnostic in 99% of the cases. Many surgical approaches to the thoracic outlet have been described: transaxillary, supraclavicular, infraclavicular and posterior. Historically standard procedure for TOS has been first rib resection with more than 90% success rate. Recently comparable results have been reported without routine first rib resection [1]. In our patient, subclavian aneurysm degeneration was secondary to hypertrophy to the anterior scalene muscle as noted intraopertively. We encountered classic poststenotic aneurysmal changes of the subclavian aneurysm inferiorly to the anterior scalene muscle. The aneurysm itself was sitting superiorly to the first rib. Such favorable anatomic location facilitated aneurysm resection without the need of first rib resection.
CASE REPORT
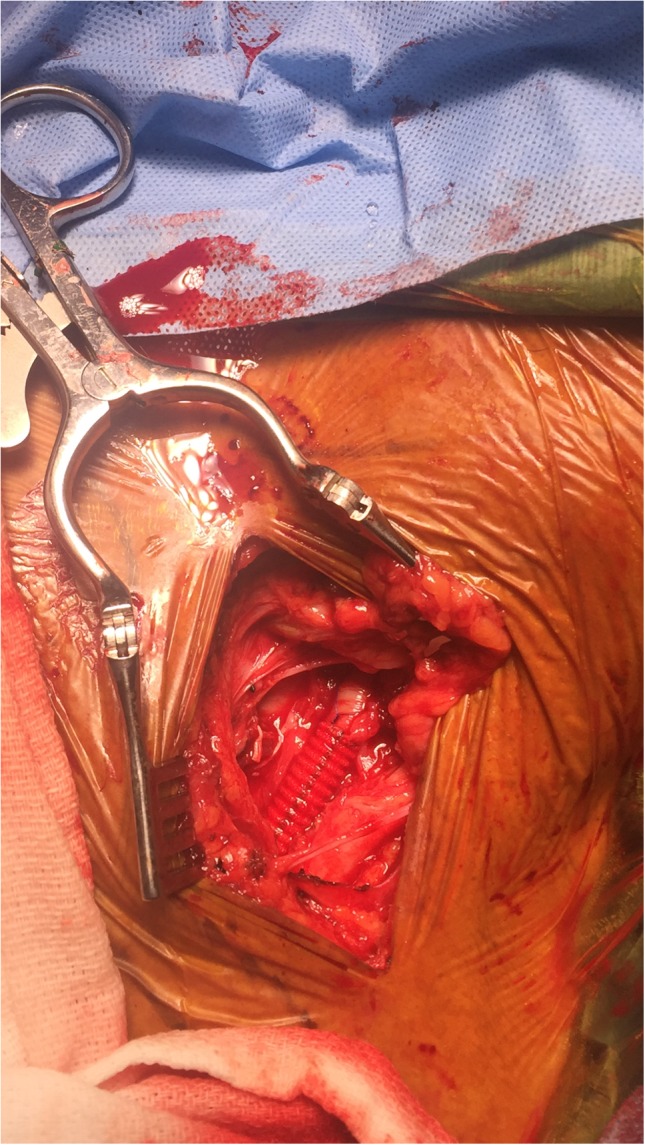
Patient is a 65-year-old male with a past medical history of hypertension who was seen by his primary care physician for left hand pain, especially after repetitive arm movements. He works as a flight attendant where often times has to perform frequent over the head hand movements. He is right hand dominant. Further work up was centered towards investigating an arterial problem as the cause of patient symptoms. CT angiography confirmed the diagnosis where a 2 × 3 cm2 aneurysm of the left subclavian artery was identified (Fig. 1). On physical exam patient had a palpable pulse in the left supraclavicular fossa, which was not present on the right side. He has palpable +2 brachial, radial and ulnar artery on the left. Adson test was positive on the left. There was no muscle atrophy noted and no neurosensory symptoms elicited. Physical exam on the right arm was unremarkable. He underwent aneurysm resection via a left supraclavicular approach. It was noted intraoperatively that anterior scalene was compressing on the subclavian artery against the superior aspect of the first rib. Poststenotic dilation was evident at this point of the dissection (Fig. 2). Once the anterior scalene was divided the full extent of the aneurysm came into view. After adequate proximal and distal control of the subclavian artery it was resected. Aneurysm measured 2 × 3 cm2. It was then open and inspected; there was no thrombus within the aneurysm (Fig. 3). A polyester (Dacron) graft was used to complete our end-to-end anastomosis (Fig. 4). Post operatively patient had a +2 radial and ulnar pulse with full range of motion of the left hand. Patient postoperative course was unremarkable. He was discharged home on POD 2.
Figure 1:
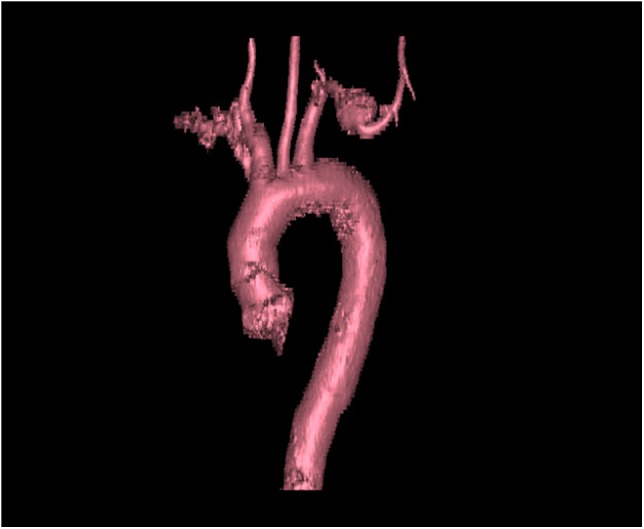
3D CT reconstruction of the big vessels. Note aneurysm location at the midportion of the subclavian artery.
Figure 2:
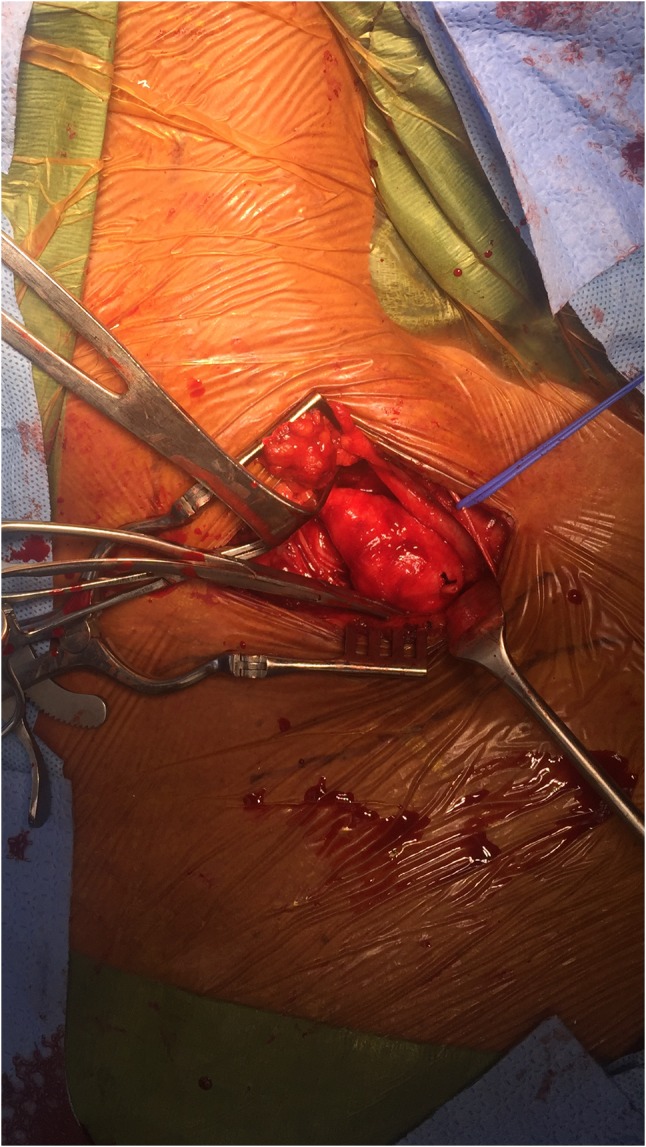
Anterior scalenectomy with poststenotic aneurysmal changes of the subclavian artery.
Figure 3:

Resected portion of aneurysm inspected for mural thrombus.
Figure 4:
Reconstruction of subclavian artery with Dacron graft.
DISCUSSION
Arterial TOS accounts for 1% of all reported cases of the TOS spectrum. Arterial TOS results from compression of the subclavian artery at the point where it crosses the first rib. In patients with arterial TOS, cervical rib is present in nearly half, followed by soft tissue anomalies in one-third of patients and scar tissue after clavicle fracture representing 5%, leading to impingement of the artery. Chronic compression and trauma to the subclavian artery as it arises out of the thoracic outlet may lead to intimal ulceration or stenosis with poststenotic dilatation of aneurysmal degeneration of the artery just distal to the site of compression. Mural thrombus from the site of damaged intima or within the aneurysm can embolize distally. Patient present with symptoms of pain and transient color changes in the digits that can be difficult to differentiate from Raynaud syndrome. Repeated episodes of embolization results in progressive occlusion of the upper extremity arterial tree with progressive symptoms [2].
Clinical syndrome of aTOS derives from three anatomic areas in which compression of the artery may occur: the scalene triangle, the costoclavicular space and the subcoracoid space. The scalene triangle is the region bordered by anterior scalene muscle, the middle scalene muscle and the first rib. Brachial plexus and subclavian artery pass over the first rib between the scalene muscles, and the subclavian vein also passes over the first rib but external to scalene triangle. The costoclavicular space is bordered by the clavicle and the first rib. This space contains the brachial plexus, subclavian artery and vein, and the subclavius muscle. Anomalous cervical ribs are found in <1% of the population. They may compress neurovascular structures in this region. Most common sites of compression in patients with aTOS are the scalene triangle and the subcoracoid space [3]. What makes our case unique is that aneurysmal changes were noted due to hypertrophy of the anterior scalene with no involvement of the first rib and the absence of congenital anatomical variants.
Clinical features of aTOS include, digital ischemia, upper extremity exertion fatigue, pallor, poikilotherimia, parasthesia and pain in the hand. These symptoms are result of hypoperfusion from arterial thromboemboli or subclavian artery compression during arm abduction. Unlike patients with neurogenic TOS, these patients seldom have any symptoms of shoulder or neck pain. An absent radial pulse at rest is common, as emboli often lodge near the antecubital space. There is usually no scalene muscle tenderness, commonly observed in neurogenic TOS, and neck rotation or head tilt elicits no symptoms. Varying degrees of ischemic sings are noted on physical examination, depending on chronicity and duration of arterial ischemia [4].
Physical examination is important and includes several provocative manouvers. Upper limb tension test and abducting the arms to 90° in external rotation usually brings on symptoms. Cervical plain radiography should be performed first to assess for bony abnormalities and to narrow the differential diagnosis. CTA or MR imaging performed in association with postural manouvers is helpful in analyzing dynamic compression. Color duplex (US) is good supplementary tool for assessment of vessel compression in association with postural manouvers. Arteriography is the gold standard, however, not necessary. Most would advocate for arteriography to assist with planning arterial reconstruction [5].
Effective management of the aTOS requires early recognition and prompt correction of the compressive mechanism. Interventions are indicted in most patients with ischemia as well as asymptomatic patients with arterial injury. Goals of treatment include (i) decompression of the structures compressing the artery, (ii) removal of the embolic source and (iii) restoration of distal perfusion. Thrombolytic therapy has been used effectively in acute management of arterial embolic complications prior to definite operative decompression [6].
We have presented aTOS on a 65-year-old male. Although case reports of aTOS are numerous in various databases, we believe our case is unique due to aneurysmal changes of subclavian artery caused by hypertrophy of the anterior scalene. To our knowledge there have been no reported cases of muscle hypertrophy being the culprit of aneurysmal degeneration of the subclavian artery causing aTOS.
AUTHOR'S CONTRIBUTIONS
All coauthors have seen and agree with the contents of the article. We certify that the submission is original work and has not been published previously elsewhere.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Buller LT, Jose J, Baraga M, Lesniak B. Thoracic outlet syndrome: current concepts, imaging features, and therapeutic strategies. Am J Arthop 2015;44:376–82. [PubMed] [Google Scholar]
- 2. Thompson JF, Jannsen F. Thoracic outlet syndromes. Br J Surg 1996;83:435–6. [DOI] [PubMed] [Google Scholar]
- 3. Davidovic LB, Kostic DM, Jakovljevic NS, Kuzmanovix IL, Simic TM. Vascular thoracic outlet syndrome. World J Surg 2003;27:545–50. [DOI] [PubMed] [Google Scholar]
- 4. Sanders RJ, Pearce WH. The treatment of thoracic outlet syndrome: a comparison of different operations. J Vasc Surg 1989;10:626–34. [DOI] [PubMed] [Google Scholar]
- 5. Rayan GM, Jensen C. Thoracic outlet syndrome: provocative examination maneuvers in a typical population. J Shoulder Elbow Surg 1995;4:113–7. [DOI] [PubMed] [Google Scholar]
- 6. Lindgren KA, Oksala I. Long-term outcome of surgery for thoracic outlet syndrome. Am J Surg 1995;169:358–60. [DOI] [PubMed] [Google Scholar]


