Summary
Introduction
High Intensity training (HIT) is a time‐effective alternative to traditional exercise programs in adults with obesity, but the superiority in terms of improving cardiopulmonary fitness and weight loss has not been demonstrated.
Objective
to determine the effectiveness of HIT on cardiopulmonary fitness and body composition in adults with obesity compared to traditional (high volume continuous) exercise.
Methods
A systematic search of the main health science databases was conducted for randomized controlled trials comparing HIT with traditional forms of exercise in people with obesity. Eighteen studies were included in the meta‐analysis. The (unstandardized) mean difference of each outcome parameters was calculated and pooled with the random effects model.
Results
HIT resulted in greater improvement of cardiopulmonary fitness (VO2max) (MD 1.83, 95% CI 0.70, 2.96, p<0.005; I2=31%) and a greater reduction of %body fat (MD ‐1.69, 95% CI ‐3.10, ‐0.27, p=0.02, I2=30%) compared to traditional exercise. Overall effect for BMI was not different between HIT and traditional exercise.
Conclusion
Training at high intensity is superior to improve cardiopulmonary fitness and to reduce %body fat in adults with obesity compared to traditional exercise. Future studies are needed to design specific HIT programs for the obese with regard to optimal effect and long‐term adherence.
Keywords: Obesity, High intensity training, Exercise
Introduction
Physical inactivity is one of the major factors associated with obesity, and a low physical fitness is an independent risk factor for mortality. Exercise is an effective strategy to reduce weight and to improve health 1. The World Health Organization recommends at least 150 minutes of moderate intensity, or at least 75 minutes of vigorous‐intensity physical activity for healthy adults in a week 2. However, the majority of the adults with obesity are not able to achieve this target due to different barriers, such as lack of motivation, lack of time and physical limitations 3, 4, 5, 6. In addition, psychological factors like depression, anxiety and body image dissatisfaction are important limitations in people with obesity to perform exercise in public 7. High intensity training (HIT) is a time‐effective alternative to traditional exercise programs which mostly involves a low to moderate intensity training of long duration. HIT is defined as exercise performed at an intensity of > 65% of maximal capacity 8. In general, HIT is often performed with intensities above 80% of maximal capacity and therefore an interval training is often used in order to maintain the exercise performance 8. High Intensity Interval Training (HIIT), a specific form of HIT, is characterized by brief repetitions of high intensity exercise (30s‐min) alternated with periods of rest or low‐intensity exercise (1‐5 min) 9, 10. Recent studies showed that HIIT is effective to increase cardiopulmonary fitness 11, 12 and to improve insulin sensitivity 12. Also, several studies have shown similar or better results with regard to weight reduction after a HIIT intervention compared to high volume, continuous training 13, 14, 15. Traditionally for weight loss, a medium intensity, high volume training is advised to increase fat oxidation. HIIT can effectuate weight reduction by promoting fat oxidation in a shorter time period, but also mechanisms like increased post exercise fat oxidation and a decreased post exercise appetite could play a role 15. Besides, some studies showed that HIIT is perceived to be more enjoyable than moderate intensity continuous exercise, also in the obese 16, 17. This may improve the adherence to exercise and promote health benefit over a longer period. Up until now, the superiority of HIT in terms of improving cardiopulmonary fitness or weight reduction compared to moderate intensity continuous training has not been shown yet in persons with obesity. Most of the studies demonstrating weight reduction with HIT are not performed in an obese study population and there is a lot of variation in exercise protocols used in these studies. Therefore, it is currently not possible to make recommendations on the optimal type of exercise in adults with obesity. The aim of this review and meta‐analysis was to determine the effectiveness of HIT on cardiopulmonary fitness and body composition in adults with obesity compared to traditional forms of exercise (lower intensity, high volume continuous). Secondly, we were interested in the effect of HIIT compared to traditional forms of exercise on these outcomes.
Methods
This review is based on PRISMA Statement for reporting systematic reviews and meta‐analysis of studies that evaluate health care interventions 18.
Search strategy
A systematic search of the main health science databases (i.e. PubMed, Embase, Medline, Cochrane and Pedro) was conducted on 30 November 2015 and on 31 January 2017. The following search terms and matching synonyms were used: obesity, obese, high intensity, interval, exercise training and clinical trial. The full search strategy in each database can be found in the supplemental file (S1).
Inclusion and exclusion criteria
For this review, randomized controlled trials published after the year 2000 were included. Studies were included if the mean Body Mass Index (BMI) of the study population was above 30 kg/m2 and if the participants were adults between 18 and 60 years. At least one of the intervention groups in the studies must have performed high intensity (interval) training (HIT or HIIT), while the control group must have performed medium or low intensity (continuous) training or normal level of physical activity. At least one of the following outcome parameters must have been reported: maximal oxygen uptake (VO2max) or any of the following body composition parameters: BMI, fat mass (%), waist circumference, fat free mass, fat free mass index. Trials must have been written in English or Dutch. Studies were excluded if the details of the exercise intervention were lacking; the participations of the studies had any significant cardiovascular of neurological comorbidity; there was any significant co‐intervention (psychological, drugs or nutritional) and if the duration of the intervention was shorter than 2 weeks.
Outcome measures
The primary outcome parameter was the maximal Oxygen Uptake (VO2max) in ml/kg/min. Secondary outcome parameters were body weight (kg), Body Mass Index (BMI) (kg/m2), waist circumference (cm) and fat mass (%).
Selection of Studies
Two authors (YT, WT) screened the articles for inclusion by using the title and abstracts. Abstracts were excluded based on the study design, age and BMI of the study population. Next, the full text of the selected articles was screened by those two researchers for inclusion based on study design, patient characteristics, intervention and outcomes. If there was a disagreement between these two authors, the third researcher (MK) made the definitive decision. The reference list of all relevant articles was screened for eligible studies for this review.
Risk management
Risk of bias for each article was assessed by two reviewers (YT and WT) independently. The recommendations in the Cochrane handbook of systematic reviews of interventions were used. Authors used the risk of bias tool in Review Manager 5 (version RevMan 5.3; https://tech.cochrane.org/revman) software and evaluated the risk as “low risk”, “unclear risk” or “high risk” for each domain (selection bias, performance bias, detection bias, attrition bias and reporting bias). Disagreements were resolved by consensus between the reviewers.
Data extraction and management
Following data were extracted from the included studies: publication year, journal, study site, study design, objectives, methods of analysis, size of study population, gender, age, type of intervention, intensity and volume of exercise training, duration of the intervention and study, VO2max (before‐after), BMI (before‐after), body weight (before‐after), waist circumference (before‐after) and percentage body fat (before‐after). RevMan 5.3 was used for data management. Only 4 articles reported the change from baseline with the corresponding standard deviations of the change for different outcomes. Calculation of standard deviations of the change in other articles was not possible because of missing standard error, t‐ and p‐values. Because of the heterogeneity in time points (baseline‐final value measurement), imputation of standard deviations of the change was not recommended (Cochrane Handbook for Systematic Reviews of Interventions). Therefore, a comparison of the final measurements was used, which in randomized controlled trials estimates the same effect as the comparison of changes from baseline 19. Data were extracted from the articles. The (unstandardized) mean difference of each outcome parameters was calculated and pooled with the random effects model 19.
Heterogeneity
Heterogeneity was expected in the size and characteristics of the study populations (age and gender) and in the characteristics of the interventions, such as the type of exercise, the intensity, frequency and the total intervention period. To determine the heterogeneity across the studies, the Chi2 and I2 tests of RevMan 5.3 were used 20. Heterogeneity was interpreted as not important when I2 was between 0% to 40%, moderate when I2 was 30% to 60%, substantial when I2 was 50%‐90% and considerable when I2 was 75% to 100%. For the Chi2 test, a p‐value of 0.10 was used to determine statistical significance in heterogeneity 19.
Subgroup analysis
Subgroup analyses were performed for HIIT (interval only) for each outcome parameter if there was sufficient data available. Additionally, subgroup analysis was performed for HIT compared to medium‐ or low intensity exercise training and compared to normal level of physical activity.
Sensitivity analysis
A sensitivity analysis was conducted by excluding studies with an intervention period shorter than 4 weeks. In addition, sensitivity analysis was performed by excluding studies with less than 20 participants from the analysis.
Meta‐regression
If there were significant results, meta‐regression analysis was performed to determine the impact of study characteristics (duration of the intervention period, intensity, intervals, repetitions, baseline BMI, age, gender and publication year) on the difference in VO2max and body composition (%body fat) between the HIT and traditional interventions. Meta‐regression analyses were performed in Stata v14.2 using the ‘metareg’ procedure taking the individual study as unit as unit of analysis. For VO2max, adjusted effect sizes are reported. For % body fat, univariable (‘crude’) effect sizes are displayed.
Meta‐regression analysis to evaluate the impact of study characteristics on the before/after changes of VO2max and % body fat within the HIT/HIIT groups could not be performed because the estimated standard error of the mean before/after change in these variables was usually not reported.
Results
Results of the search
There were 4251 records identified from the initial search of electronic databases. Two additional articles were identified through other sources. After removing the duplicates, 1865 titles were left for screening. From this list, the full text of 81 relevant articles were reviewed in detail. Finally, 18 articles were included in the meta‐analysis (Figure 1).
Figure 1.
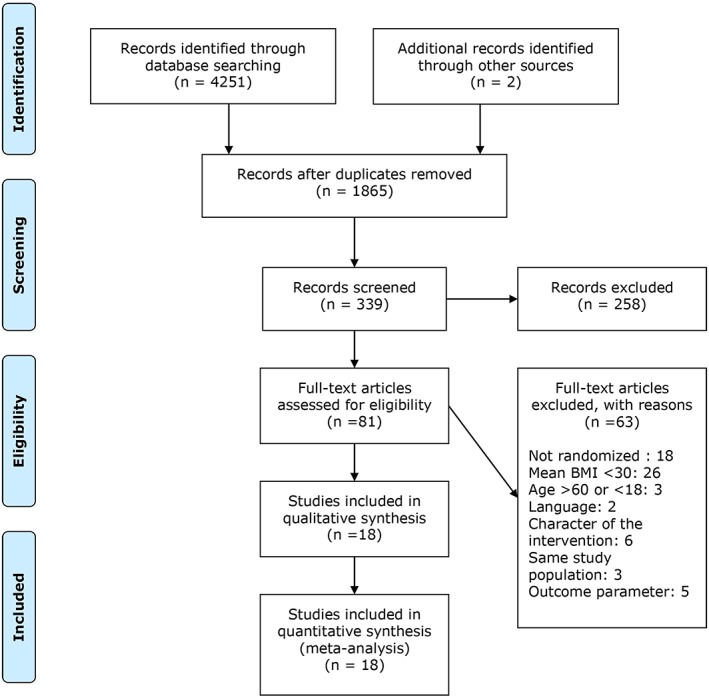
Flow diagram of screening and selection of articles for review.
Risk of bias in included studies
The overall quality of the included studies was low (Figure 2). Details about the randomization process and allocation concealment were lacking in almost all studies, so the risk of bias was unclear. Only 3 studies reported a blinded assessment of the outcomes 21, 22, 23. Also in 4 studies, the number of participants was low, ranging from 12‐18, with the risk of overestimation or underestimation of the effect on outcome parameters 21, 24, 25, 26. In most studies, there was not enough information to determine reporting bias (Figure 2 and 3, S2).
Figure 2.
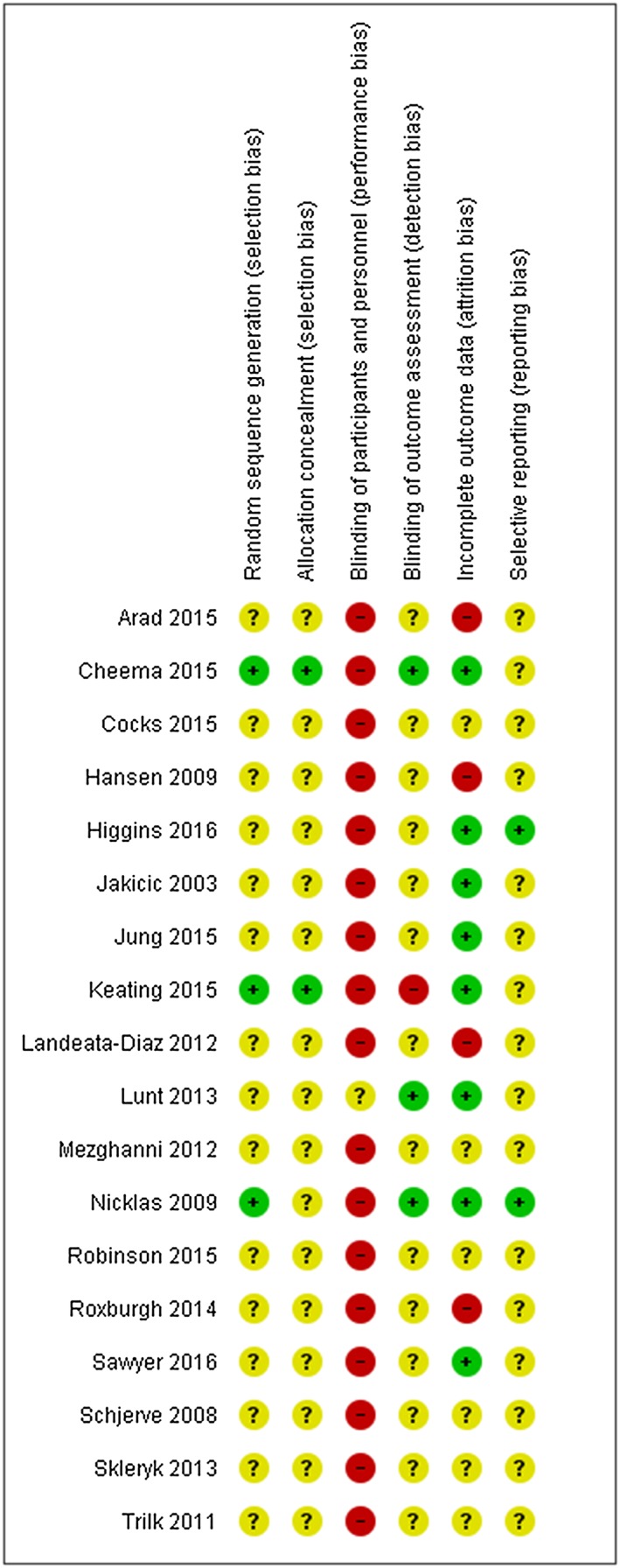
Risk of bias summary: review authors’ judgements about each risk of bias item for each included study.
Figure 3.
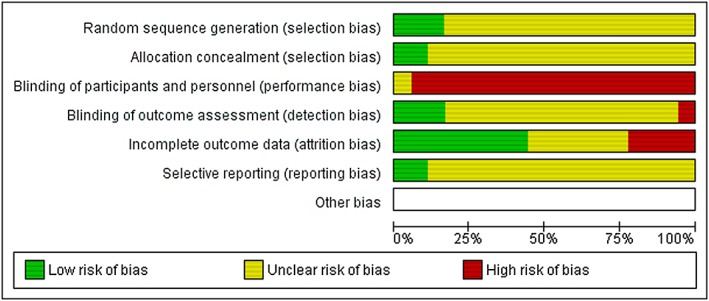
Risk of bias graph. Review authors’ judgement about each risk of bias item presented as percentages across all included studies.
Characteristics of the included studies
The characteristics of the 18 included studies are summarized in Table 1 and S2. A total of 854 participants were randomized in these studies. The sample size differed between 12 and 201 participants. All studies were published between 2003 and 2016. The mean age of the included patients was between 24 and 59 year and the mean BMI range was between 30‐38 kg/m2. In all included studies, obesity was defined as a BMI equal or greater to 30 kg/m2. Twelve studies excluded participants with diabetes (I and II) 21, 24, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, and 13 studies excluded patients with hypertension and cardiac comorbidity 21, 23, 24, 26, 28, 29, 30, 32, 33, 34, 35, 36, 37 . One study did not provide information about the presence of comorbidities 25.
Table 1.
Overview of the characteristics of included studies. Data are presented in means ±SD. Abbreviations: HIIT (High intensity interval training), CON (control), SIT (sprint interval training), MICT (medium intensity continuous training), HI (high intensity), LI (low intensity), MeD (Mediterranean diet), MeDE (Mediterranean diet with exercise), AIT (aerobic interval training), MVIT (maximal volitional intensity training), WALK (walking exercise), CR (caloric restriction), CR+MI (caloric restriction + medium intensity exercise), CR+HI (caloric restriction +high intensity exercise), CMIET (continuous medium intensity exercise training), TER (traditional exercise recommendations)
| Study | N | Age (y) | BMI (kg/m 2 ) | Training | Intensity | Duration | Control | Outcome VO2max (ml.min.kg) | Outcome BMI (kg/m 2 ) |
|---|---|---|---|---|---|---|---|---|---|
| Arad et al. 2015 27 | 28 female |
HIIT: 29 ± 4 CON: 30 ±7 |
HIIT: 32.5 ±3.6 CON: 32.1 ±3.2 |
HIIT (cycling; 24 min) (3/week) |
6 min warm‐up 50%HRR 4x30‐60s 75‐90% HRR 5 min cool‐down | 14 weeks | Normal level of physical activity |
HIIT: from 23.1 ±4.9 to 24.9±5.5 CON: from 19.7 ±6.3 to 20.9 ±4.6 |
HIIT: from 32.5±3.6 to 32.7 ±3.8 CON: from 32.1±3.2 to 31.6 ±3.6 |
| Cheema et al. 2015 21 |
12 7: female 5: male |
39 ±17 |
HIIT: 32.0±5.9 CON: 30.8±2.6 |
HIIT (Boxing; 50 min) (4/week) |
5 min warm up HIIT 2:1 >75% HRR vs rest/pacing |
12 weeks |
50 min brisk walking (4/week) |
HIIT: from 27.9 ±2.4 to 32.5 ±5.0 CON: from 29.0 ±6.4 to 28.8 ±8.0 |
HIIT: from 32.0 ±5.9 to 30.5 ±4.0 CON: from 30.8 ±2.6 to 30.7 ±3.0 |
| Cocks et al. 2015 24 | 16 male |
SIT: 24 ±5.7 MICT:26±5.7 |
SIT: 35.8 ±4.2 MICT: 33.7±4.2 |
SIT (cycling) (5/week) |
2 min warm up (50W) 30s 200% Wmax /120s 30W 4 to 7 intervals |
12 sessions |
40‐60 min continuous cycling ‐65% VO2peak (5/week) |
SIT: from 33.9 ±3.4 to 36.3 ±4.5 MICT: 35.1 ±4.2 to 39.8 ±7.6 |
SIT: from 35.8 ±4.2 to 35.7 ±4.2 MICT: 33.7±4.2 to 33.1±4.5 |
| Hansen et al. 2009 38 | 50 male | 59 ±8 |
HIT: 32.1±4.5 LIT: 32.7±3.9 |
HIT (walking, cycling, cross‐country ski‐type exercise) (3/week) |
40 min continuous at 75% VO2peak | 6 months | 55 min continuous at 50% VO2peak |
HIT: from 20.8 ±5.5 to 24.7 ±6 LIT: from 20.9 ±5 to 23.5 ±5.5 |
HIT: from 32.1±4.5 to 31.4 ±4.5 LIT: from 32.7 ± 4 to 32.3 ±4.5 |
|
Higgins et al 2016 20 |
60 female | 20.4 ±1.5 | 30.3 ±4.5 |
SIT (cycle ergometer) (3/week) |
4 min warm‐up 30 s ‘all out” sprints, 4 min active recovery. 5 repetitions in week 1‐2, 6 repetitions in week 3‐4 and 7 repetitions in week 5‐6 |
6 weeks | 20‐30 min cycling at 60‐70% Heart rate reserve |
SIT: from 29.1 ±4.8 to 33.2 ± 4.4 MICT: from 26.9 ±4.5 to 28.8 ± 4.3 |
|
| Jakicic et al. 2003 29 | 201 female |
HI/HI: 38.3 ±5.4 MI/HI: 36.8±5.3 |
HI: 32.8 ±3.9 MI: 32.2 ±3.9 |
High intensity/high duration (treadmill) (5/week) |
12 months |
Moderate intensity/high duration (5/week) |
HI: from 20.2±2.9 to 24.5±4.8 MI: from 19.4±3.2 to 22.1±4.0 |
HI: from 32.9 ±3.9 to 29.5 ±4.8 MI: from 32.3 ±3.9 to 29.2 ±4.8 |
|
| Jung et al. 2015 30 |
32 27:female 5:male |
51 ±10 | 32.9 ±6.3 |
HIIT (25 min) (walking,elliptical machine, treadmill or cycling) (3/week) |
3 min warm up 10x1 min 90% HRpeak 2 min cool‐down |
10 days + 4 weeks | 20‐50 min continuous 65% HRpeak |
HIIT: from 20.7 ±3.3 to 22.6 ±4.1 MICT: from 20.8 ±5.2 to 22.0 ±4.6 |
HIIT: from 29.8 ±5.5 to 29.9 ±5.1 MICT: from 32.1 ±4.1 to 31.9 ±3.7 |
|
Keating et al. 2015 31 |
48 | 43.6 ±3.0 | 33.4 ±1.3 |
HI (cycling) (3/week) |
30‐45 min 60‐70% VO2peak | 8 weeks |
Low to moderate intensity, high volume (Brisk walking) 45‐60 min 50% VO2peak |
HI: from 21.9 ±4.8 to 24.9 ±5.5 LO: from 24.9 ±3.5 to 27.2 ±2.8 |
HI: from 36.3 ±5.9 to 35.8± 5.9 LO: from 33.9 ±3.1 to 33.4 ±3.1 |
| Landaeta‐Diaz et al. 2012 32 |
45 30: female 15: male |
MeD: 57.2 ±4.4 MeDE: 59.05 ±5.5 |
MeD: 38.44 ±6.5 MeDE: 37.05 ±3.22 |
MeDE (diet +exercise) (ergometer) (3/week) |
30 min 80% HRmax | 12 weeks | Diet only‐ calori restriction (500kcal/day) |
MeDE: from 18.87 ±5.59 to 27.31 ±4.70 MeD: from 19.99 ±5.72 to 22.38 ± 6.98 |
MeDE: from 37.05±3.22 to 33.79±3.21 MeD: from 38.44 ±6.5 to 36.35 ±6.12 |
|
Lunt et al. 2013 22 |
49 36:female 13:male |
WALK: 46.3 ±5.4 AIT: 48.2 ±5.6 MVIT: 50.3 ±8.0 |
WALK: 32.7 ±4.3 AIT: 32.1 ±3.1 MVIT: 32.4 ±2.9 |
AIT: aerobic interval training (walking) MVIT: maximal volitional intensity training (3/week) |
AIT: 4min HIIT (85‐95% HRmax)/3 min walking 4 repetitions (40 min) MVIT: 30 s volitional intensity/4 min walking 3‐6 repititions (25‐40 min) 10 min warming up 5 min cool‐down |
12 weeks |
WALK: 10 min warming up 5 min cool down 33 min walk (65‐75% HRpeak) |
AIT: from 24.2 ±4.8 to 25.6 ±4.8 MVIT: from 25.0 ±2.8 to 25.2 ±3.4 WALK: from 26.5 ±5.3 to 25.2 ±3.6 |
AIT: from 32.1 ±3.1 to 32.1 ±3.0 MVIT: from 32.4 ±2.9 to 32.3 ±2.9 WALK: from 32.4 ±2.9 to 32.3 ±2.9 |
| Mezghanni et al. 2012 33 | 31 female | 25.2 ±4.8 |
G75: 32.9 ±1.8 G50: 34.1 ±3.6 CON: 33.2 ±1.8 |
High intensity aerobic training (walking and jogging) |
G75: 20‐55 min 75% HRR | 12 weeks |
Moderate intensity aerobic training G50: 20‐55min 50% HRR OR Control |
G75: from 32.9 ±1.8 to 30.5 ±2.4 G50: from 34.1 ±3.6 to 32.9 ±3.8 CON: from 33.2 ±1.8 to 33.3 ±1.7 |
|
|
Nicklas et al. 2009 23 |
112 female |
CR: 58.4 ±6.0 CR+MI: 57.7 ±5.5 CR+HI: 59.0 ±5.0 |
CR: 33.9 ±4.0 CR+MI: 33.7 ±3.5 CR+HI: 32.9 ±3.7 |
Caloric restriction + high intensity exercise (treadmill) (3/week) |
3‐5 min warm up CR+HI: 70‐75%HRR |
20 weeks |
CR+MI: 45‐50%HRR OR CR only |
CR+HI: +4.1 ± 3.7 CR+MI: +2.5 ±2.6 CR only: +2.0 ±2.6 |
|
| Robinson et al. 2015 34 | 39 | 52±10 |
HIIT: 32.9± 6.6 MICT: 31.4 ± 4.1 |
HIIT (cycle, treadmill, elliptical) |
HIIT: 3 min warm up 4x 1:1 85‐90% Wpeak/20% Wpeak to 10x 1:185‐90% Wpeak / 20% Wpeak Cooldown (32.5% Wpeak) |
2 weeks | 20‐50 min of continuous activity at 32.5% Wpeak |
HIIT: from 20.4 ±3.4 to 21.9 ±4.0 MICT: from 20.6 ±4.9 to 22.1 ±4.7 |
HIIT: from 32.9 ±6.6 to 32.6 ±6.7 MICT: from 31.4 ±4.1 to 31.3 ±4.0 |
|
Roxburgh et al. 2014 36 |
29 19: female 10: male |
36.3 ± 6.9 |
CMIET+HIIT: 30.7± 6.3 CMIET: 29.6± 4.7 Control: 29.2 ±4.2 |
CMIET+ single bout of HIIT (treadmill and cycling) (5/week) |
4 sessions CMIET +1 session HIIT: 60s 100%VO2max ‐150 s recovery 8‐12 repetitions |
12 weeks |
CMIET: 15 min walking and 15 min cycling (45‐60%HRR) Control: normal activity level. No exercise |
CMIET+HIIT: from 32.7 ±9.2 to 36.0±11.5 CMIET: from 33.2±4.0 to 34.5 ±6.1 CON: from 30±4.6 to 28.3±6.5 |
CMIET+HIIT: from 30.7 ±6.3 to 30.6±6.1 CMIET: from 29.6±4.7 to 29.4±4.7 CON: from 29.2 ±4.2 to 29.5±4.4 |
|
Sawyer et al. 2016 26 |
18 9: female 9: male |
HIT: 35.6 ±8.9 MICT: 34.8 ±7.7 |
HIIT: 37.4 ±6.2 MICT: 34.5 ±3.2 |
HIIT (cycle ergometer) (3/week) |
5 min warm‐up (50‐60% HRmax) 10x 1 min intervals (90‐95% HRmax) 5 min cool‐down (50‐60% HRmax) |
8 weeks |
5 min warm‐up (50‐60% HRmax) 30 min cycling at 70‐75% of HRmax 5 min cool‐down (50‐60% HRmax |
HIIT: from 20.3 ±4.9 to 24.4 ±5.9 MICT: from 22.4 ±3.6 to 25.5 ±4.5 |
HIIT: from 37.4 ±6.2 to 37.4 ±6.1 MICT: from 34.5 ±3.2 to 34.5 ±3.2 |
|
Schjerve et al. 2008 37 |
40 32: female 8: male |
Strength: 46.2 ± 10.6 Moderate intensity: 44.4 ±7.9 High intensity: 46.9±7.9 |
Strength: 34.5±5.05 Moderate intensity: 36.7±5.05 High intensity: 36.6±4.49 |
HIIT (treadmill, walking and running) (3/week) |
10 min warm up 50‐60% HRmax 4x4 min 85‐95% + 3 min interval walking 50‐60% HRmax 5 min cool down |
12 weeks |
Moderate intensity: 47 min walking 60‐70% HRmax Strenght training: 15 min warm up 40‐50% HRmax 4x5 90% 1RM |
||
| Skleryk et al. 2013 25 | 16 male | 38.7±5.5 | 33.7±5.7 |
Sprint interval training (SIT) (ergometer) (6 sessions) |
8‐12x10 s ‘all out’ sprints | 2 weeks |
Traditional exercise recommendations (TER) 30 min 65% VO2max (10 sessions) |
SIT: from 29.7 ±3.7 to 29.3±5.3 TER: from 26.3±5.7 to 26.3±6.2 |
SIT: from 32.2±5.9 to 32.2±5.9 TER: from 35.2±5.1 to 35.2±5.1 |
| Trilk et al. 2011 35 | 28 female |
SIT: 30.1±6. CON: 31.4±5.5 |
SIT: 35.7±6. CON: 34.6±5.9 |
Sprint interval training (SIT)(ergometer) (3/week) |
SIT: 4 min warm up 30 s sprint against resistance (0.05kg/kg) 4 min active recovery (low RPM at 0% body mass) |
4 weeks | Normal level of physical activity |
SIT: from 21.6±4.12 to 24.5±4.12 CON: from 20.5±3.4 to 20.4±3.0 |
Characteristics of the interventions
Details of the exercise interventions in each study are summarized in Table 1. Twelve studies compared HIIT with lower intensity exercise or normal level of physical activity 21, 22, 24, 25, 26, 27, 28, 30, 35, 36, 37. Six studies compared the effect of a continuous HIT with lower intensity exercise training 29, 31, 38 or normal level of physical activity 23, 32, 33. In two studies, there was a diet intervention included in both the intervention and control group, so the intensity of the exercise was the only difference between these groups 23, 32. In the majority of the studies, participants trained 3 to 5 times a week, and the duration of the interventions varied from 2 weeks to 6 months. Different exercise modalities were cycling 24, 25, 26, 27, 28, 30, 31, 32, 34, 35, 36, 38, walking/running 22, 23, 29, 30, 33, 34, 36, 37, 38 and boxing 21. There was considerable variation in the used HIIT protocols. The number of repetitions varied from 4 to 12 repetitions, with intervals of 10s to 4 min. The intensity of the exercise varied from 70‐100% of the maximal heart rate (HRmax) 21, 22, 26, 27, 30, 37, 90‐100% of VO2max 36 or 85‐200% of Wmax 24, 34 . Three studies performed “all out” sprints against a resistance equivalent to 0.05 kg/body mass 25, 28, 35. The intensity of continuous HIT was 60‐75% of VO2max 31, 38 or 70‐80% of HRmax 23, 29, 32, 33 . Adherence to the intervention program was above 75% in 10 of the 18 studies 21, 23, 25, 29, 30, 31, 32, 34, 36, 38. One study reported a lower adherence rate of 59% 22; one study excluded patients with an attendance of < 70% from analysis 28, and in the other 6 studies, no information was provided about adherence 24, 26, 27, 33, 35, 37. Three of the 18 studies reported adverse events related to the intensity of the exercise. In the study of Lunt et al. three participants had developed injuries in the group with maximal volitional interval training. No injuries occurred in the group with aerobic interval training or walking 22. In the study of Nicklas et al., one patient in the vigorous intensity vs. 4 patients in the moderate intensity group discontinued exercising because of time problems (2) or injuries (3) 23. In the study of Keating et al. during exercise a syncopal episode occurred in one patient in the high intensity and one patients in the low intensity group 31.
Measurements
Anthropometric parameters such as height and weight were measured in a standardized way in all studies. Cardiopulmonary fitness was measured by determining the maximal oxygen uptake (VO2max) either by an incremental cycling test 24, 25, 26, 27, 28, 30, 31, 32, 34, 35, 38 or by the use of a treadmill for maximal exercise 21, 22, 23, 29, 36, 37. Different protocols were used for exercise testing 39, 40 but mainly a load‐incremental protocol was used until volitional exhaustion and/or reaching >85% age‐predicted heart rate and/or plateau of VO2max and/or a drop of the pedaling rate < 50/rpm. Body composition was measured by a bioelectrical impedance 33 or a dual energy x‐ray absorptiometry (DXA) 23, 24, 26, 27, 28, 35, 37, 38. In one study, the % body fat was computed from six skinfold sites using validated equations 21.
Outcome VO2 max
Fifteen studies reported VO2max as an outcome parameter. Compared to traditional exercise, HIT was significantly more effective to improve VO2max (MD 1.83, 95% CI 0.70, 2.96, p<0.005; I2=31%) (Figure 4). In addition, comparing HIIT with traditional exercise revealed a significant effect in favour of HIIT (MD=1.79, 95% CI 0.21, 3.36, p=0.03; I2=38%) (Figure 5). Continuous HIT showed a statistical significant effect for VO2max (MD 1.68, 95% CI 0.10, 3.27, p=0.04; I2=25%).
Figure 4.
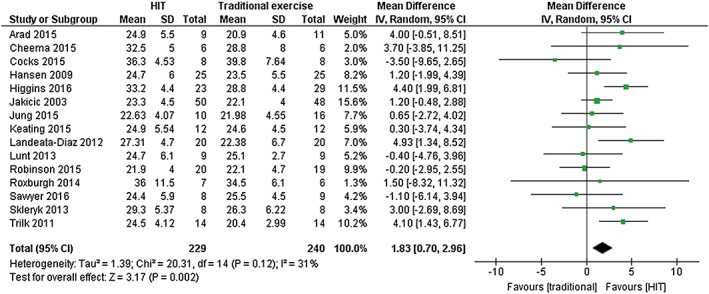
Forest plot of comparison: HIT vs. traditional exercise. Outcome: Maximal Oxygen Uptake (VO2max)
Figure 5.
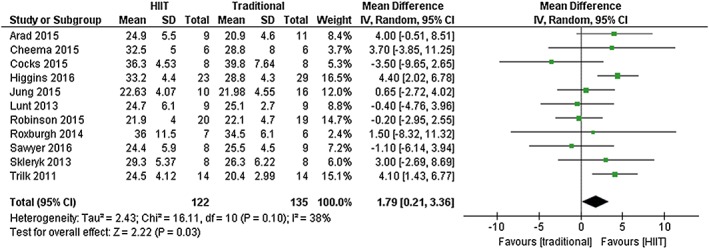
Forest plot of comparison: HIIT vs. traditional exercise. Outcome: Maximal Oxygen Uptake (VO2max)
Outcome Body composition
The overall effect for BMI, body weight, waist circumference was not different between HIT and traditional exercise (Table 2a). However, HIT resulted in a significant reduction in the percentage of body fat compared to traditional exercise (MD ‐1.69, 95% CI ‐3.10, ‐0.27, p=0.02, I2=30%) (Figure 6). In addition, comparing HIIT with traditional exercise revealed a significant effect for the percentage of body fat in favour of HIIT (MD ‐2.01, 95% CI ‐3.75, ‐0.30, p=0.02, I2=0%) (Table 2b).
Table 2.
a) Effect of HIT vs. lower intensity exercise on cardiopulmonary fitness (VO2max) and body composition. b) Effect of HIIT vs. lower intensity exercise on cardiopulmonary fitness (VO2max) and body composition
| a | study (n) | participants (n) | MD (IV, Random, 95% CI) | p‐value | I2 |
|---|---|---|---|---|---|
| VO2max (ml/kg/min) | 15 | 469 | 1.83 [0.70, 2.96] | <0.05 | 31% |
| BMI (kg/m2) | 15 | 437 | 0.20 [‐1.10, 1.50] | 0.76 | 91% |
| Body weight (kg) | 12 | 386 | ‐1.18 [‐4.16, 1.80] | 0.44 | 0% |
| Body fat (%) | 10 | 296 | ‐1.69 [‐3.10, ‐0.27] | 0.02 | 30% |
| Waist circumference (cm) | 8 | 253 | ‐1.04 [‐4.54, 2.45] | 0.56 | 27% |
| b | |||||
|---|---|---|---|---|---|
| VO2max (ml/kg/min) | 11 | 257 | 1.79 [0.21, 3.36] | 0.03 | 38% |
| BMI (kg/m2) | 9 | 177 | 0.37 [‐1.44, 2.18] | 0.69 | 70% |
| Body weight (kg) | 7 | 153 | ‐0.42 [‐5.30, 4.47] | 0.87 | 7% |
| Body fat (%) | 7 | 157 | ‐2.01 [‐3.73, ‐0.30] | 0.02 | 0% |
| Waist circumference (cm) | 5 | 111 | ‐1.63 [‐6.37, 3.10] | 0.87 | 7% |
Figure 6.
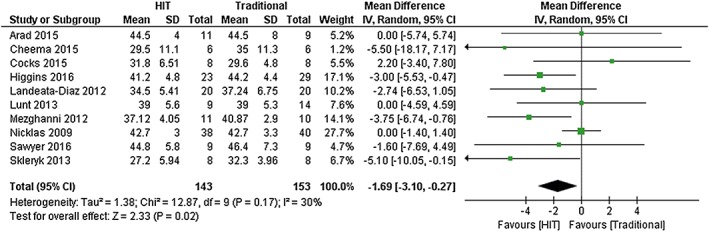
Forest plot of comparison: HIT vs. traditional exercise. Outcome: %body fat
Subgroup analysis
Subgroup analysis for HIT compared to baseline physical activity revealed a significant effect for VO2max in favour of HIT (MD 4.32, 95% CI 2.39, 6.26, p<0.005; I2=0%). Also, HIT compared to medium intensity training showed a significant effect for VO2max in favour of HIT (MD 1.20, 95% CI 0.12, 2.28, p=0.03, I2=11%).
Sensitivity analysis
Sensitivity analysis by excluding studies with an intervention period shorter than 4 weeks did not change the results for VO2max or other outcomes 25, 34. Also, excluding studies with less than 20 participants did not change the results for VO2max or other outcomes 21, 24, 25, 26.
Meta‐regression
Duration of the intervention period (VO2max: β=0.014, p=0.979; %body fat: β=0.16, p=0.132), intensity of intervention (VO2max: β=‐1.34, p=0.602; %body fat: β= ‐0.11, p=0.887), intervals (VO2max: β=‐0.04, p=0.372; %body fat: β=0.01, p=0.290), number of repetitions (VO2max: β=‐0.203, p=0.763; %body fat: β=‐0.39, p=0.262) and baseline BMI (VO2max: β= ‐0.66, p=0.087; %body fat: β=0.12, p=0.708) were not significantly associated with the treatment effects for VO2max and %body fat between HIT and traditional intervention. In addition, studies with a younger study population (VO2max: β=‐0.06, p=0.721; %body fat: β=0.049, p=0.192), male study population (VO2max: β= 1.93, p=0.237; %body fat: β= 0.06, p=0.960) and recent studies (VO2max: β=‐4.15, p= 0.093; %body fat: β=0.46 p=0.766) were not associated with the treatment effects for VO2max en %body fat.
Discussion
In this review and meta‐analysis, the effectiveness of high intensity training in terms of cardiopulmonary fitness and body composition was compared to other forms of exercise in adults with obesity. Based on the results of this meta‐analysis we can conclude that training at high intensity is a better method to improve cardiopulmonary fitness in the obese population than traditional, lower intensity continuous training. In addition, when high intensity interval training was compared with other forms of exercise, we found a significant better improvement of VO2max.To our knowledge, this is the first meta‐analysis comparing high intensity training with other forms of exercise in adults with obesity. Previous studies in normal weight adults (BMI < 25 kg/m2) showed significant improvements in cardiopulmonary fitness 11 after an HIIT intervention compared to medium intensity continuous training 41. In a randomized controlled trial in overweight patients with metabolic syndrome, Tjonna et al. showed a significant higher increase in VO2max after HIIT compared to continuous moderate exercise (CME) (35% vs. 16%). Moreover, HIIT was superior compared to CME in reducing risk factors for metabolic syndrome, such as reduction in blood glucose and lipogenesis in adipose tissue and enhancing endothelial function. There was no difference between HIIT and CME groups with regard to weight reduction 14. Different mechanisms underlying the increase of VO2max in HIIT are an increased ATP generation by phosphocreatine degradation during HIIT and muscle glycogenolysis 15, 42, improvement in vascular/endothelial function 43, an increase in cardiac output by enhanced cardiac contractility and an increased muscle oxidative capacity by upregulation of mitochondrial activity 10, 44. However, it is unclear whether these adaptations are different in the people with obesity. With regard to body composition, this meta‐analysis showed a significant reduction in the percentage of body fat in favour of HIT compared to traditional exercise. Moreover, HIIT showed the same effect compared to lower intensity continuous exercise. This finding implies a direct effect of high intensity (interval) training on fat oxidation, and was confirmed by a previous study of Trapp et al. who showed significantly more reduction in subcutaneous fat in young healthy women who performed HIIT (3/week, 15 weeks) compared to a continuous exercise training 13. However, in the present meta‐analysis, there was no difference in the amount of weight loss, BMI or waist circumference between HIT or traditional exercise. This may be explained by the absence of an accompanying significant dietary intervention. For example, in a randomized controlled trial with asthma patients with obesity, Scott et al. showed that after 10 weeks of either dietary intervention, exercise intervention or combined dietary/exercise invention, only patients who received dietary or combined intervention did have a statistically significant amount of weight loss 45. This study emphasises the importance of a dietary intervention on top of exercise. However, in this meta‐analysis, studies with diet as an intervention were excluded, because the aim was to focus on the effect of HIT. Another issue is that the most included studies did not provide data on equal energy expenditure between HIT and traditional exercise forms. Only one study controlled this well, showing that sprint interval training resulted to a greater decrease of fat mass and led to a nearly 2‐fold greater increase in VO2max compared to medium intensity continuous training with equal exercise energy expenditure 28. Another possibility for the absence of positive effects on BMI is that the variable duration of the exercise intervention could have influenced the results. However, excluding articles with an intervention period of <4 weeks did not change the results. A recent meta‐analysis of Jelleyman et al. demonstrated that HIIT was associated with modest weight loss (‐1.3kg, p<0.001) compared to a non‐exercising control group, but not compared to continuous training. However, the primary aim of the mentioned study was to investigate the effect of HIIT on glucose regulation 46. Although this review shows that high intensity (interval) training has favorable effects on cardiopulmonary fitness and body composition in adults with obesity, the results should be interpreted with caution. An important limitation is that most included studies only reported the pre‐ and post‐intervention parameters, but not the change from baseline, or the corresponding 95% CI or p‐values of that change. Therefore, we were only able to compare post‐intervention values. Although, only randomized controlled trials were included, there were some imbalances in baseline values between the intervention and control groups in some of the studies. The small sample sizes in these studies could be the reason for these imbalances and this could result in a bias. Nevertheless, excluding studies with small sample sizes from analysis did not change the results. Secondly, the primary outcome in some studies was different from VO2max and body composition. Moreover, small size studies may be underpowered to show a significant effect on these parameters. Different methods were used to determine outcome parameters which could lead to variation heterogeneity in outcomes and outcome assessment. Also, the risk of bias was unclear in most domains, especially with regard to selection bias (randomization/allocation) and reporting bias. In addition, excluding comorbidities like diabetes and cardiovascular problems in these studies could result in an important selection bias. However, in this review and meta‐analyses we were able to summarize the available data about high intensity (interval) exercise intervention in the obese population. There are some issues that should be considered about high intensity exercise in the obese. Performing exercise at high intensity is very demanding and could be a potential risk for knee‐ and other injuries in the obese. However, only three of the 18 included studies reported adverse events related to the intensity of the exercise. Also, 13 of the 18 studies excluded patients with hypertension and cardiac comorbidity, conditions that are usually present in the obese population. VO2max is recognized as one of the best predictors of mortality among cardiac patients and several studies have noted that high intensity interval training is safe and effective in cardiac patients 47, 48. Moreover, some studies reported that HIIT results in greater improvements in VO2max compared to moderate intensity continuous training 47, 49, 50, 51. Another issue is the motivation for an exercise program in persons with obesity. Depression, a negative body image and embarrassment are factors that can influence the decision to participate in an exercise program. Therefore, attention to these psychological should be given in addition to exercise training in this group of patients 7. In the included studies, most of the exercises were performed on a cycle ergometer or on a treadmill. Little is known about the effect or risk of other exercise modalities, like running (outdoor) or swimming. Future studies are needed to investigate which type of HIT is most suitable for the obese with regard to side effects, risk of injuries, but also with regard to long‐term adherence and effects. In addition, patients with obesity and with different comorbidities (cardiovascular, pulmonary, diabetes) should be included in these kind of studies to investigate the feasibility and effects in this group of patients. In conclusion, HIT is, 1) superior to traditional exercise in improving cardiopulmonary fitness, which is an important indicator of health, 2) superior to traditional exercise in reducing the percentage of body fat 3) feasible and well‐tolerated in persons with obesity. Larger, well‐designed randomized controlled trials are required to confirm the findings and to design optimal (HIT) training programs for the obese population.
Potential Conflicts of interest
Authors declare that there are no potential conflicts of interest regarding to this manuscript
Supporting information
Data S1. Supplemental file
Data S2. Supporting info item
Acknowledgements
We thank J.W. Schoones (Walaeus Library, Leiden University Medical Center, Leiden, The Netherlands) for his help in performing the search.
We thank E. Birnie (Franciscus Gasthuis, Rotterdam, The Netherlands) for his help in statistical analysis.
Türk, Y. , Theel, W. , Kasteleyn, M. J. , Franssen, F. M. E. , Hiemstra, P. S. , Rudolphus, A. , Taube, C. , and Braunstahl, G. J. (2017) High intensity training in obesity: a Meta‐analysis. Obesity Science & Practice, 3: 258–271. doi: 10.1002/osp4.109.
References
- 1. Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2012; 2: 1143–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Global Recommendations on Physical Activity for Health . WHO Guidelines Approved by the Guidelines Review Committee. Geneva 2010.
- 3. Allender S, Foster C, Boxer A. Occupational and nonoccupational physical activity and the social determinants of physical activity: results from the Health Survey for England. J. Phys. Act. Health 2008; 5: 104–116. [DOI] [PubMed] [Google Scholar]
- 4. Sherwood NE, Jeffery RW. The behavioral determinants of exercise: implications for physical activity interventions. Annu. Rev. Nutr. 2000; 20: 21–44. [DOI] [PubMed] [Google Scholar]
- 5. Lidegaard LP, Schwennesen N, Willaing I, Faerch K. Barriers to and motivators for physical activity among people with Type 2 diabetes: patients' perspectives. Diabet. Med. 2016; 33: 1677–1685. [DOI] [PubMed] [Google Scholar]
- 6. Egan AM, Mahmood WA, Fenton R, et al. Barriers to exercise in obese patients with type 2 diabetes. QJM. 2013; 106: 635–638. [DOI] [PubMed] [Google Scholar]
- 7. Sarwer DB, Polonsky HM. The Psychosocial Burden of Obesity. Endocrinol. Metab. Clin. North Am. 2016; 45: 677–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. De Feo P. Is high‐intensity exercise better than moderate‐intensity exercise for weight loss? Nutr. Metab. Cardiovas. Dis. 2013; 23: 1037–1042. [DOI] [PubMed] [Google Scholar]
- 9. Gillen JB, Gibala MJ. Is high‐intensity interval training a time‐efficient exercise strategy to improve health and fitness? Appl. Physiol. Nutr. Metab. 2014; 39: 409–412. [DOI] [PubMed] [Google Scholar]
- 10. Gibala MJ, McGee SL. Metabolic adaptations to short‐term high‐intensity interval training: a little pain for a lot of gain? Exerc. Sport Sci. Rev. 2008; 36: 58–63. [DOI] [PubMed] [Google Scholar]
- 11. Helgerud J, Hoydal K, Wang E, et al. Aerobic high‐intensity intervals improve VO2max more than moderate training. Med. Sci. Sports Exerc. 2007; 39: 665–671. [DOI] [PubMed] [Google Scholar]
- 12. Nybo L, Sundstrup E, Jakobsen MD, et al. High‐intensity training versus traditional exercise interventions for promoting health. Med. Sci. Sports Exerc. 2010; 42: 1951–1958. [DOI] [PubMed] [Google Scholar]
- 13. Trapp EG, Chisholm DJ, Freund J, Boutcher SH. The effects of high‐intensity intermittent exercise training on fat loss and fasting insulin levels of young women. Int. J. Obes. (Lond) 2008; 32: 684–691. [DOI] [PubMed] [Google Scholar]
- 14. Tjonna AE, Lee SJ, Rognmo O, et al., Stolen TO . Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: a pilot study. Circulation 2008; 118: 346–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Boutcher SH. High‐intensity intermittent exercise and fat loss. Journal of obesity. 2011; 2011: 868305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bartlett JD, Close GL, MacLaren DP, Gregson W, Drust B, Morton JP. High‐intensity interval running is perceived to be more enjoyable than moderate‐intensity continuous exercise: implications for exercise adherence. J. Sports Sci. 2011; 29: 547–553. [DOI] [PubMed] [Google Scholar]
- 17. Kong Z, Fan X, Sun S, Song L, Shi Q, Nie J. Comparison of High‐Intensity Interval Training and Moderate‐to‐Vigorous Continuous Training for Cardiometabolic Health and Exercise Enjoyment in Obese Young Women: A Randomized Controlled Trial. PLoS One 2016; 11: e0158589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 2009; 62: e1–34. [DOI] [PubMed] [Google Scholar]
- 19. Higgins JPT, Green S. (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. John Wiley & Sons, Ltd: Oxford, UK: The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org. [Google Scholar]
- 20. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003; 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cheema BS, Davies TB, Stewart M, Papalia S, Atlantis E. The feasibility and effectiveness of high‐intensity boxing training versus moderate‐intensity brisk walking in adults with abdominal obesity: a pilot study. BMC Sports Sci Med Rehabil. 2015; 7: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lunt H, Draper N, Marshall HC, et al. High Intensity Interval Training in a Real World Setting: A Randomized Controlled Feasibility Study in Overweight Inactive Adults, Measuring Change in Maximal Oxygen Uptake. PLoS One 2014; 9: e83256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nicklas BJ, Wang X, You T, et al. Effect of exercise intensity on abdominal fat loss during calorie restriction in overweight and obese postmenopausal women: a randomized, controlled trial. Am. J. Clin. Nutr. 2009; 89: 1043–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cocks M, Shaw CS, Shepherd SO, et al. Sprint interval and moderate‐intensity continuous training have equal benefits on aerobic capacity, insulin sensitivity, muscle capillarisation and endothelial eNOS/NAD(P)Hoxidase protein ratio in obese men. J. Physiol. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Skleryk JR, Karagounis LG, Hawley JA, Sharman MJ, Laursen PB, Watson G. Two weeks of reduced‐volume sprint interval or traditional exercise training does not improve metabolic functioning in sedentary obese men. Diabetes Obes. Metab. 2013; 15: 1146–1153. [DOI] [PubMed] [Google Scholar]
- 26. Sawyer BJ, Tucker WJ, Bhammar DM, Ryder JR, Sweazea KL, Gaesser GA. Effects of high‐intensity interval training and moderate‐intensity continuous training on endothelial function and cardiometabolic risk markers in obese adults. J. Appl. Physiol. 2016; 121: 279–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Arad AD, DiMenna FJ, Thomas N, et al. High‐intensity interval training without weight loss improves exercise but not basal or insulin‐induced metabolism in overweight/obese African American women. J. Appl. Physiol. 2015; 119: 352–362. [DOI] [PubMed] [Google Scholar]
- 28. Higgins S, Fedewa MV, Hathaway ED, Schmidt MD, Evans EM. Sprint interval and moderate‐intensity cycling training differentially affect adiposity and aerobic capacity in overweight young‐adult women. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme 2016; 41: 1177–1183. [DOI] [PubMed] [Google Scholar]
- 29. Jakicic JM, Marcus BH, Gallagher KI, Napolitano M, Lang W. Effect of exercise duration and intensity on weight loss in overweight, sedentary women: a randomized trial. JAMA 2003; 290: 1323–1330. [DOI] [PubMed] [Google Scholar]
- 30. Jung ME, Bourne JE, Beauchamp MR, Robinson E, Little JP. High‐intensity interval training as an efficacious alternative to moderate‐intensity continuous training for adults with prediabetes. J Diabetes Res. 2015; 2015: 191595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Keating SE, Hackett DA, Parker HM, et al. Effect of aerobic exercise training dose on liver fat and visceral adiposity. J. Hepatol. 2015; 63: 174–182. [DOI] [PubMed] [Google Scholar]
- 32. Landaeta‐Diaz L, Fernandez JM, Da Silva‐Grigoletto M, et al. Mediterranean diet, moderate‐to‐high intensity training, and health‐related quality of life in adults with metabolic syndrome. Eur. J. Prev. Cardiol. 2013; 20: 555–564. [DOI] [PubMed] [Google Scholar]
- 33. Mezghanni N, Chaabouni K, Chtourou H, et al. Effect of exercise training intensity on body composition, lipid profile, and insulin resistance in young obese women. Afr. J. Microbiol. Res. 2012; 6: 2481–2488. [Google Scholar]
- 34. Robinson E, Durrer C, Simtchouk S, et al. Short‐term high‐intensity interval and moderate‐intensity continuous training reduce leukocyte TLR4 in inactive adults at elevated risk of type 2 diabetes. J. Appl. Physiol. 2015; 119: 508–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Trilk JL, Singhal A, Bigelman KA, Cureton KJ. Effect of sprint interval training on circulatory function during exercise in sedentary, overweight/obese women. Eur. J. Appl. Physiol. 2011; 111: 1591–1597. [DOI] [PubMed] [Google Scholar]
- 36. Roxburgh BH, Nolan PB, Weatherwax RM, Dalleck LC. Is moderate intensity exercise training combined with high intensity interval training more effective at improving cardiorespiratory fitness than moderate intensity exercise training alone? J Sports Sci Med. 2014; 13: 702–707. [PMC free article] [PubMed] [Google Scholar]
- 37. Schjerve IE, Tyldum GA, Tjonna AE, et al. Both aerobic endurance and strength training programmes improve cardiovascular health in obese adults. Clin. Sci. 2008; 115: 283–293. [DOI] [PubMed] [Google Scholar]
- 38. Hansen D, Dendale P, Jonkers RA, et al. Continuous low‐ to moderate‐intensity exercise training is as effective as moderate‐ to high‐intensity exercise training at lowering blood HbA(1c) in obese type 2 diabetes patients. Diabetologia 2009; 52: 1789–1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am. Heart J. 1973; 85: 546–562. [DOI] [PubMed] [Google Scholar]
- 40. Lafortuna CL, Resnik M, Galvani C, Sartorio A. Effects of non‐specific vs individualized exercise training protocols on aerobic, anaerobic and strength performance in severely obese subjects during a short‐term body mass reduction program. J. Endocrinol. Invest. 2003; 26: 197–205. [DOI] [PubMed] [Google Scholar]
- 41. Milanovic Z, Sporis G, Weston M. Effectiveness of High‐Intensity Interval Training (HIT) and Continuous Endurance Training for VO2max Improvements: A Systematic Review and Meta‐Analysis of Controlled Trials. Sports Med. 2015; 45: 1469–1481. [DOI] [PubMed] [Google Scholar]
- 42. Trump ME, Heigenhauser GJ, Putman CT, Spriet LL. Importance of muscle phosphocreatine during intermittent maximal cycling. J. Appl. Physiol. 1996; 80: 1574–1580. [DOI] [PubMed] [Google Scholar]
- 43. Ramos JS, Dalleck LC, Tjonna AE, Beetham KS, Coombes JS. The impact of high‐intensity interval training versus moderate‐intensity continuous training on vascular function: a systematic review and meta‐analysis. Sports Med. 2015; 45: 679–692. [DOI] [PubMed] [Google Scholar]
- 44. Burgomaster KA, Howarth KR, Phillips SM, et al. Similar metabolic adaptations during exercise after low volume sprint interval and traditional endurance training in humans. J. Physiol. 2008; 586: 151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Scott HA, Gibson PG, Garg ML, et al. Dietary restriction and exercise improve airway inflammation and clinical outcomes in overweight and obese asthma: a randomized trial. Clinical and experimental allergy: journal of the British Society for Allergy and Clinical Immunology. 2013; 43: 36–49. [DOI] [PubMed] [Google Scholar]
- 46. Jelleyman C, Yates T, O'Donovan G, et al. The effects of high‐intensity interval training on glucose regulation and insulin resistance: a meta‐analysis. Obesity reviews: an official journal of the International Association for the Study of Obesity. 2015; 16: 942–961. [DOI] [PubMed] [Google Scholar]
- 47. Nilsson BB, Hellesnes B, Westheim A, Risberg MA. Group‐based aerobic interval training in patients with chronic heart failure: Norwegian Ullevaal Model. Phys. Ther. 2008; 88: 523–535. [DOI] [PubMed] [Google Scholar]
- 48. Kavanagh T, Mertens DJ, Hamm LF, et al. Prediction of long‐term prognosis in 12 169 men referred for cardiac rehabilitation. Circulation 2002; 106: 666–671. [DOI] [PubMed] [Google Scholar]
- 49. Cornish AK, Broadbent S, Cheema BS. Interval training for patients with coronary artery disease: a systematic review. Eur. J. Appl. Physiol. 2011; 111: 579–589. [DOI] [PubMed] [Google Scholar]
- 50. Rognmo O, Hetland E, Helgerud J, Hoff J, Slordahl SA. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. European journal of cardiovascular prevention and rehabilitation: official journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology. 2004; 11: 216–222. [DOI] [PubMed] [Google Scholar]
- 51. Warburton DE, McKenzie DC, Haykowsky MJ, et al. Effectiveness of high‐intensity interval training for the rehabilitation of patients with coronary artery disease. Am. J. Cardiol. 2005; 95: 1080–1084. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. Supplemental file
Data S2. Supporting info item


