Abstract
Background
In this study, the results of the partial lateral facetectomy of the patella to better patellofemoral motion and congruence are compared with the results of the osteophyte removal of the patella and neurectomy only in total knee arthroplasty (TKA).
Methods
Data from 55 patients undergoing TKA with osteophytes removal of the patella and neurectomy only, and those undergoing osteophytes removal of the patella and neurectomy and partial lateral facetectomy were reviewed retrospectively. Clinical outcomes were evaluated by knee society score (KSS) and functional score of knee. Clinical anterior knee pain (AKP) rating and knee range of motion and extension lag were assessed for each patient.
Results
There was significant difference between two groups in AKP (p < 0.05), and the mean range of motion of the knee in groups 1 and 2 was 117° ± 9° and 116.6° ± 8.2°, respectively. Three (13%) patients of the reshaped patella group and three (11%) patients of the non-reshaped patella group had extension lag <10°, respectively. The mean KSS and knee functional scores showed no statistical difference between groups (p > 0.05).
Conclusion
Partial lateral facetectomy of the patella can decrease AKP and can be used routinely for every patient that surgeon does not decide to resurface the patella.
Keywords: arthroplasty, replacement, knee, patellofemoral pain syndrome, subchondral
Introduction
Patellar resurfacing during total knee arthroplasty (TKA) remains controversial. Many surgeons perform patellar resurfacing routinely, in order to decrease the incidence of anterior knee pain (AKP) and the rate of revision caused by patellofemoral problems [1–5].
Patellar resurfacing can result in complications (including fracture, patellar component failure, osteonecrosis, instability, tendon rupture, and patellar clunk syndrome) [6, 7]. Numerous controlled clinical trials have compared TKA outcomes between patellar non-resurfacing and resurfacing procedures, but results have been inconclusive, particularly regarding AKP and revision rate. Therefore, now, some surgeons prefer patellar non-resurfacing procedures. In several uncontrolled trials, compared with other procedures, patellar partial lateral facetectomy and circumpatellar denervation were reported to achieve better therapeutic effects and reduce postoperative AKP in patients with isolated patellofemoral osteoarthritis [8], but research into the therapeutic effects of these procedures in TKA is limited.
In this study, the results of the osteophyte removal of the patella and neurectomy were compared with the results of the partial lateral facetectomy in TKA.
Materials and Methods
Data from patients with osteoarthritis, who underwent primary unilateral TKA at a university hospital between December 2010 and June 2013, were reviewed retrospectively. The indication for the surgery was degenerative osteoarthritis that was severe enough to warrant TKA after an adequate trial of non-operative therapy. Exclusion criteria were a history of patellar fracture, patellectomy, and high tibial or distal femoral osteotomy; any surgery involving the extensor mechanism; septic arthritis of the knee or osteomyelitis. Those undergoing surgery between 2010 and 2011 underwent osteophytes removal of the patella and neurectomy only, whereas those undergoing surgery between December 2011 and December 2012 underwent osteophytes removal of the patella and neurectomy and partial lateral facetectomy. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Patients’ anonymity was persevered.
All surgeries were performed by two surgeons in Rasul Akram Hospital. The surgical technique was similar in all cases using a medial parapatellar approach. Bone cuts and soft-tissue balancing were performed in the same sequence. Femoral component rotation is detected by transepicondylar axis, whiteside line, and posterior femoral condyle axis. Rotation of the tibial component is determined by Akagi line. In group 1, all osteophytes of the patella were removed and partial facetectomy of the lateral facet was performed by oscillating saw. In group 2, all osteophytes around the patella were removed and neurectomy by electrocauter was performed.
The patella was reshaped to match the trochlea of the femoral prosthesis (Figs 1 and 2).
Fig. 1.

Osteoarthritis of patella
Fig. 2.
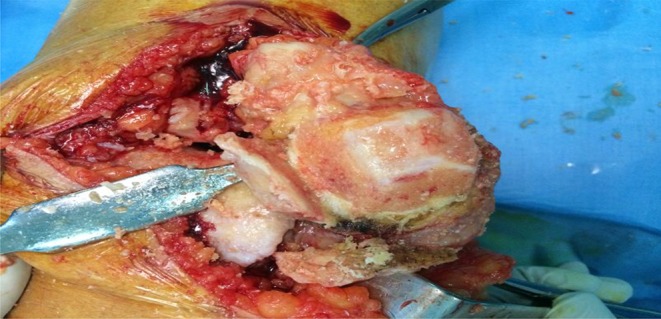
Partial lateral facetectomy of the patella
A standardized, perioperative regimen was used for all patients. Continuous passive movement was used postoperatively for 2 weeks. Active isometric quadriceps exercise, initiative straight-leg raising, and extending–flexing motion were encouraged in the immediate postoperative period. Walking with partial weight bearing was permitted 24 h postoperatively under the supervision of a physical therapist.
An independent investigator evaluated all the patients. Postoperative follow-up assessments were performed at 3, 6, 12, and 18 months. Data collected at 18 months postoperatively were analyzed in this study. Clinical outcomes were evaluated by knee society score (KSS) and functional score of the knee by clinical AKP rating (Table I), and knee range of motion and extension lag were assessed for each patient. All clinical evaluations were performed by a surgeon who was unaware as to whether patients had patellar facetectomy or not. Radiographic findings were evaluated in anteroposterior, lateral, and skyline views of the knee (Fig. 3).
Table I.
Clinical anterior knee pain rating
| Rating | Description |
|---|---|
| 0 | No pain |
| I | Mild pain that does not intrude on daily activities |
| II | Moderate pain that is a nuisance; patient not considering further surgery |
| III | Severe pain; patient considering further surgery |
Fig. 3.

Skyline view of the patella after partial lateral facetectomy
All data were analyzed using the SPSS software package. An unpaired Student’s t-test was used to compare pre- and postoperative KSSs between the two groups. Fisher’s exact test was used to assess nominal data including incidence of AKP or revision rate. Differences at a level of p < 0.05 were considered to be statistically significant.
Results
Data from 55 patients were reviewed. Nine patients were excluded. Five patients had at least one of the exclusion criteria and four patients did not complete follow-up program. Forty-six patients (51 knees) were followed up for at least 18 months. Twenty-two patients with patella reshaping by partial lateral patella facetectomy (group 1) were compared with 24 patients without facetectomy (the control group; group 2), matched for age and follow-up (Table II). Patients in both groups had no statistically significant differences in age and follow-up (p > 0.05). Two of the 22 (9%) cases in the reshaping group were bilateral total knee replacement, whereas 91% were unilateral. Three of the 24, or 12% of cases, in the non-reshaping group were bilateral. Lateral retinacular release was performed in three patients in the non-reshaping patella group and in one patient in the reshaping patella group, with no significant between-group differences. AKP in both groups was presented in Table III. Two patients of the group 2 had a score of 2 suggesting presence of moderate pain that is a nuisance; patients not considering further surgery. There was significant difference between two groups in AKP (p < 0.05). Two patients in group 1 and one patient in group 2 had crepitation in anterior knee, respectively. Thus, there was no significant difference between two groups with regard to anterior knee crepitation (p > 0.05). The mean range of motion of the knee in groups 1 and 2 was 117° ± 9° and 116.6° ± 8.2°, respectively. Three (13%) patients of the reshaped patella group and three (12%) patients of the non-reshaped patella group had extension lag <10°, respectively. The mean KSS and knee functional scores were calculated for both groups: reshaping and non-reshaping (Table IV). Eighteen months after the operation, there were no significant differences between two groups in knee society pain score and functional score (p > 0.05).
Table II.
Demographic data of patients
| Group 1 | Group 2 | |
|---|---|---|
| Age (years) | 62.8 ± 6.23 | 63.4 ± 6.13 |
| Male/female | 14/8 | 11/13 |
| Follow-up (months) | 12.1 ± 1.2 | 12.52 ± 1.95 |
Table III.
Clinical anterior knee pain rating in both groups based on Fig. 1
| Rating | Group 1 | Group 2 |
|---|---|---|
| 1 | 2 | 4 |
| 2 | 0 | 2 |
Table IV.
Postoperative KSSs between the two groups
| KSS | Group 1 | Group 2 |
|---|---|---|
| Knee score | 86.1 ± 3.1 | 84.1 ± 7.6 |
| Function score | 86 ± 5 | 85 ± 8.8 |
Discussion
TKA is an operation with a high gain in quality-of-life [9]. Patellofemoral pain (PFP) in particular is a common complication after TKA and is often responsible for revision surgery. Sensi et al. [10] reported an incidence of 8% for AKP after TKA. In particular, increasing and localized contact pressure and patella maltracking are held accountable for PFP, but the reasons are various. After 1960s, changes in the femoral component such as addition of a trochlear flange improved the clinical results and decreased anterior discomforts in TKA. These changes encouraged some surgeons to resurface patella in TKA. The largest study of patellar resurfacing is that of Yeganeh et al. [2]. The complication rate was 4% in the resurfaced group, compared with 12% in the non-resurfaced group. The most prevalent complication in the non-resurfaced group was continuing chronic knee pain. This was retrospective and involved 10 surgeons, but the authors considered that the two groups of patients were essentially similar. In a recent annual report of the National Joint Registry of England and Wales 2013, 67% of primary total knee replacements were performed without patellar resurfacing, as the majority of surgeons believed that the benefits did not outweigh the risks [11]. In a prospective randomized study, Feller et al. [11] provided no evidence to support the routine resurfacing of the patella at a TKA for osteoarthritis. Controversy remains regarding whether the procedure should include patellar resurfacing or not [1, 2, 5, 6]. This uncertainty has led to three approaches to patellar resurfacing in total knee replacement: always resurface, never resurface, or selectively resurface [12]. Advanced destructive osteoarthritis of the patellofemoral joint (PFJ) results in AKP symptoms [13, 14]. A problem without patellar resurfacing TKA is chondrolysis of the patella [13]. It should be remembered that patellar tracking, contact area, and pressure distribution are significantly different between native and prosthetic knees. According to the theory of Dye [15], each knee having a unique “envelope of function”; a potential range of activity in which it maintains a homeostasis of all surrounding tissues. A prosthetic knee can be viewed as a knee functioning with a combined biologic and artificial transmission with a limited potential range of activity. Artificial products containing metals and polyethylene are harder and less flexible than the original cartilage, and therefore, make it unlikely that the knee will return fully to its pre-injury/pre-arthritis state. It is known that the structures in and around the PFJ are very sensitive to pain, being full of nociceptors such as subchondral bone of patellae affected with degenerative disease are all richly supplied with type IVa free nerve endings and fibers containing Substance P [16]. There was a significant difference of mean retropatellar pressure between natural knee and after TKA, which may be one important reason for AKP after TKA in vivo [17].
Some surgeons prefer non-resurfacing patella, but they remove osteophytes around the patella and reshape the patella [6, 21]. It results in decrease of AKP. Lateral patella facetectomy had improved clinical results in patients with isolated patellofemoral arthritis [18–22].
Some clinicians encouraged to perform lateral patella facetectomy in TKA for treatment of patellofemoral osteoarthritis. Zhang et al. [23] demonstrated that partial lateral facetectomy is an effective way to improve the function of patellar-retaining TKA in patients with primary osteoarthritis. Patients who underwent partial lateral facetectomy showed more significant improvements in the scores and fewer lateral patellar osteophytes in radiographs. In some studies, partial lateral facetectomy had better results compared with lateral release for correction of patellar tracking [24]. A partial lateral facetectomy may have the ability to increase congruency and to accommodate small mismatches or small errors in the lateral facet [23].
Lateral facetectomy also can decrease the rate of lateral release and reduce the rate of damage of the lateral geniculate artery [15–17]. We thought that lateral facetectomy can decrease AKP over constraining the PFJ is incompatible with freedom of motion in recent prosthesis. Thus, partially conforming surfaces may provide reasonable motion, laxity, and stability. In our experience, lateral facetectomy can provide partial conformity and decrease patellofemoral shear force.
In this study, 22 patients who underwent lateral facetectomy of the patella (group 1) were compared with 24 patients who underwent osteophytes removal of the patella (group 2) in TKA. Patients in group 1 had less AKP than patients in group 2. But there were no significant difference between two groups in knee society pain score and functional score. In our small series, partial lateral facetectomy of the patella had no significant effect on knee range of motion.
Conclusion
Partial lateral facetectomy of the patella can decrease AKP and can be used routinely for every patient that surgeon does not decide to resurface the patella.
Authors’ contribution
All authors had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Their roles on all works of study were equal. All authors read and approved the final version of this manuscript.
Conflict of interest
The authors declare no conflict of interest.
Funding Statement
Funding sources: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Waters TS, Bentley G: Patellar resurfacing in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am 85-A, 212–217 (2003) [DOI] [PubMed] [Google Scholar]
- 2.Yeganeh A, Mahmodi M, Farahini H, Moghtadaei M: Short-term outcomes of induced membrane technique in treatment of long bone defects in Iran. Med Arch 70, 284–287 (2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moghtadaei M, Farahini H, Faiz SH, Mokarami F, Safari S: Pain management for total knee arthroplasty: Single-injection femoral nerve block versus local infiltration analgesia. Iran Red Crescent Med J 16, e13247 (2014) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Farahini H, Moghtadaei M, Bagheri A, Akbarian E: Factors influencing range of motion after total knee arthroplasty. Iran Red Crescent Med J 14, 417–421 (2012) [PMC free article] [PubMed] [Google Scholar]
- 5.Muoneke HE, Khan AM, Giannikas KA, Hägglund E: Secondary resurfacing of the patella for persistent anterior knee pain after primary knee arthroplasty. J Bone Joint Surg Br 85-B, 675–678 (2003) [PubMed] [Google Scholar]
- 6.Liu ZT, Fu PL, Wu HS, Zhu Y: Patellar reshaping versus resurfacing in total knee arthroplasty – Results of a randomized prospective trial at a minimum of 7 years’ follow-up. Knee 19, 198–202 (2012) [DOI] [PubMed] [Google Scholar]
- 7.Karrholm J, Jonsson H, Nilsson KG, Soderqvist I: Kinematics of successful knee prostheses during weight-bearing: Three-dimensional movements and positions of screw axes in the Tricon-M and Miller–Galante designs. Knee Surg Sports Traumatol Arthrosc 2, 50–59 (1994) [DOI] [PubMed] [Google Scholar]
- 8.Wetzels T, Bellemans J: Patellofemoral osteoarthritis treated by partial lateral facetectomy: Results at long-term follow up. Knee 19, 411–415 (2012) [DOI] [PubMed] [Google Scholar]
- 9.Norman-Taylor FH, Palmer R, Villa RN: Quality-of-life improvement compared after hip and knee replacement. J Bone Joint Surg Br 78-B, 74–77 (1996) [PubMed] [Google Scholar]
- 10.Sensi L, Buzzi R, Giron F, De Luca L, Aglietti P: Patellofemoral function after total knee arthroplasty: Gender-related differences. J Arthroplasty 26, 1475–1480 (2011) [DOI] [PubMed] [Google Scholar]
- 11.Feller JA, Barlett RJ, Lang DM: Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br 78-B, 226–228 (1996) [PubMed] [Google Scholar]
- 12.Pilling RWD, Moulder E, Allgar V, Stat C, Messner J, Sun Z: Patellar resurfacing in primary total knee replacement: A meta-analysis. J Bone Joint Surg Am 94, 2270–2278 (2012) [DOI] [PubMed] [Google Scholar]
- 13.Petersen W, Rembitzki IV, Brüggemann GP: Anterior knee pain after total knee arthroplasty: A narrative review. Int Orthop 38, 319–328 (2014) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Scuderi GR, Insall J, Scott N: Patellofemoral pain after total knee arthroplasty. J Am Acad Orthop Surg 2, 239–246 (1994) [DOI] [PubMed] [Google Scholar]
- 15.Dye SF: The knee as a biologic transmission with an envelope of function: A theory. Clin Orthop Relat Res 325, 10–18 (1996) [DOI] [PubMed] [Google Scholar]
- 16.Moghtadaei M, Otoukesh B, Bodduhi B, Ahmadi K, Yeganeh A: Evaluation of patellar position before and after medial opening wedge high tibial osteotomy: Radiographic and computed tomography findings. Med Arch 70, 293–295 (2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steinbrück A, Schröder C, Woiczinski M, Fottner A, Müller E: Patellofemoral contact patterns before and after total knee arthroplasty: An in vitro measurement. Biomed Eng Online 12, 58 (2013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nilsson KG, Karrholm J, Ekelund L: Knee motion in total knee arthroplasty. A roentgen stereophotogrammetric analysis of the kinematics of the Tricon-M knee prosthesis. Clin Orthop Relat Res 256, 147–161 (1990) [PubMed] [Google Scholar]
- 19.Victor J, Labey L, Wong P, Innocenti B, Bellemans J: The influence of muscle load on tibiofemoral knee kinematics. J Orthop Res 28, 419–428 (2010) [DOI] [PubMed] [Google Scholar]
- 20.Dennis DA, Komistek RD, Mahfouz MR, Walker SA, Tucker A: A multicenter analysis of axial femorotibial rotation after total knee arthroplasty. Clin Orthop Relat Res 428, 180–189 (2004) [DOI] [PubMed] [Google Scholar]
- 21.Junlin H, Zheng H, Guilin O, Lianbo X: Effect of patella reshaping in total knee arthroplasty of rheumatoid arthritis on patellar motion trace and anterior knee pain. J Biomechanical 13, 220–225 (2013) [Google Scholar]
- 22.Paulos LE, O’Connor DL, Karistinos A: Partial lateral patellar facetectomy for treatment of arthritis due to lateral patellar compression syndrome. Arthroscopy 24, 547–551 (2008) [DOI] [PubMed] [Google Scholar]
- 23.Zhang LZ, Zhang XL, Jiang Y, Wang Q, Chen YS, Shen H: Lateral patellar facetectomy had improved clinical results in patients with patellar-retaining total knee arthroplasty. J Arthroplasty 27, 1442–1447 (2012) [DOI] [PubMed] [Google Scholar]
- 24.Lakstein D, Naser M, Adar E, Atoun E, Edelman A, Hendel D: Partial lateral patellar facetectomy as an alternative to lateral release in total knee arthroplasty (TKA). J Arthroplasty 29, 2146–2149 (2014) [DOI] [PubMed] [Google Scholar]


