Abstract
Background
Dissection of aorta is a rare, but fatal complication of aortic cannulation in cardiac surgery can be caused by the sudden rise in blood pressure and hemodynamic variations.
Methods
In this study, 90 patients aged 18 years or older undergoing cardiac surgery were divided into two equal groups. Under similar conditions, trial group received 1.5 mg/kg of lidocaine for 90 s before cannulation and control group received normal saline. Hemodynamic parameters of patients including systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), heart rate (HR), and central venous pressure before cannulation and 1, 3, and 5 min after cannulation were recorded in a form. Consumed nitroglycerin (TNG) rate was also measured and recorded.
Results
In the lidocaine group, compared with the placebo group, mean SBP, DBP, and MAP significantly reduced after cannulation (P < 0.05). During the follow-up period, mean HR (P = 0.649) and TNG usage (P = 0.527) were similar in two groups.
Conclusion
Intravenous lidocaine, 1.5 mg/kg, 90 s before cannulation leads to a reduction in SBP, DBP, and MAP, up to 5 min after cannulation, so it can decrease risk of aortic dissection.
Keywords: lidocaine, hemodynamic, aortic cannulation, pressure, saline
Introduction
Cardiac surgery and use of cardiopulmonary bypass require cannulation of main arterial and venous systems. Arterial cannulation allows blood flow from cardiopulmonary pump into arterial system. For this purpose, subclavian artery was used initially. However, the use of this artery was forbidden because of the difficulty in access and damage to blood supply to upper limbs; hence, femoral or iliac arteries were used, which were also forbidden because of a number of complications including dissection, retroperitoneal hemorrhage, stenosis, ischemia of the limb, and traumatic aneurysms [1–3]. Currently, ascending aorta is the site of choice for arterial cannulation [4, 5]. Rising blood pressure during aortic cannulation is one of the causes of aortic dissection, and therefore, mean arterial pressure (MAP) should be maintained below 80 mmHg [6, 7]. Despite its rarity, some cases have even been reported in aortic cannulation in infants.
To reduce hemodynamic variations and responses in stressful circumstances, especially in patients undergoing cardiac surgery, various techniques and medications are recommended, including opioids, topical anesthetics, and sympatholytics. Amid, lidocaine is of interest as a topical anesthetic [8]. Currently, it is hypothesized whether intravenous lidocaine can reduce hemodynamic variations at aortic cannulation. According to research into other surgical procedures, it can be observed that lidocaine can reduce some of the unwanted hemodynamic responses. In this study, the effect of intravenous lidocaine on reducing hemodynamic variations at aortic cannulation was compared with that of a placebo.
Materials and Methods
After approval from the research council and the medical ethics committee of Rajaie Cardiovascular Medical & Research Center in Tehran, Iran, this study was conducted on 90 patients aged 18 years or older undergoing cardiac surgery as a double-blind, randomized clinical trial.
Emergent surgery, patients with G6PD deficiency, uncontrolled head and neck tumors, and vascular problems were excluded.
After filling out consent forms, all patients were divided into lidocaine and placebo groups using paired block randomization. Patients were visited a day before surgery, and with equal pre-medication, they were administered 1 mg of oral lorazepam the night before surgery and 1 mg in the morning of surgery, 2 h before transfer to operating room. Also, 2 h before surgery, all patients were intramuscularly injected with 0.1 mg/kg of morphine. Once placed on the operating table, patients’ vital signs were measured and recorded using space-lab monitor.
After installing intravenous cannula No. 18 in the right cubital area and administering 6 ml/kg of ringer solution, arterial catheter No. 20 was inserted in left radial artery after local anesthesia with 1% lidocaine. All patients equally received 30 μg of sufentanil for over 1 min, and then, about 3 min after, 0.2 mg/kg of etomidate was given to patients for over 60–90 s. After disappearance of the eyelash reflex and response to verbal commands, patients were administered 0.5 mg/kg of atracurium for over 30 s, and 3 min after, patients were given 20 μg of sufentanil and intubated 30 s later.
Central venous catheter was inserted from right internal jugular vein, and central venous pressure (CVP) was measured and recorded.
Before cannulation, and also after 1, 3, and 5 min, hemodynamic details of all the patients were recorded including diastolic blood pressure (DBP), MAP, heart rate (HR), CVP, and systolic blood pressure (SBP). At the site of ascending aorta, patients were cannulated with No. 21 cannula.
Patients in the lidocaine group were administered 1.5 mg/kg of 1% lidocaine 90 s before aortic cannulation (KINGODIC; 1% lidocaine, Caspian Tamin Pharmaceutical, Rasht, Iran), and patients in the placebo group received normal saline. All patients with SBP less than 110 mmHg were cannulated. To reduce patients’ blood pressure, 5% nitroglycerin (TNG) was used (Trinitrosan 5 mg/ml, Merck KGaA, Darmstadt, Germany).
Quantitative data were analyzed as mean and standard deviation (SD) using SPSS-17 software, and qualitative data were presented as frequency and percentage frequency. To compare a variable in the two groups, t-test was used after ensuring normal distribution. Also, chi-square test was used to determine the significance of qualitative variables.
Results
In this study, 45 patients in the lidocaine group and 45 patients in the placebo group were investigated. Demographic and clinical details of patients, at entry to study, are presented in Table I. The two groups had insignificant differences in terms of age, gender, and body mass index (BMI). Furthermore, the difference was also insignificant between the two groups in terms of history of underlying diseases such as hypertension, diabetes mellitus, hyperlipidemia, smoking and opioids use, and cardiovascular medications such as beta-blockers, calcium channel blockers, and angiotensin-converting enzyme (ACE) inhibitors and diuretics (P > 0.05) (Table I).
Table I.
Patients demographic and clinical details at entry to study
| Group studied | Lidocaine | Placebo | P value |
|---|---|---|---|
| Number of patients in each group | 46 | 45 | |
| Age, mean ± SD (years) | 62.1 ± 5.49 | 71.6 ± 3.53 | 0.345 |
| Gender: male/female | 22-3 | 23-2 | 0.813 |
| BMI, mean ± SD | 9.5 ± 1.25 kg/cm2 | 10.5 ± 1.25 | 0.947 |
| Frequency of hypertension (%) | 14 (30%) | 19 (43%) | 0.210 |
| Frequency of diabetes mellitus (%) | 13 (28%) | 11 (24%) | 0.680 |
| Frequency of hyperlipidemia (%) | 15 (33%) | 13 (29%) | 0.701 |
| Frequency of smoking (%) | 8 (17%) | 9 (20%) | 0.750 |
| Frequency of opioids use (%) | 6 (13%) | 9 (20%) | 0.371 |
| Frequency of beta-blockers use (%) | 30 (67%) | 32 (71%) | 0.649 |
| Frequency of use of calcium channel blockers (%) | 6 (13%) | 5 (11%) | 0.748 |
| Frequency of use of ACE inhibitors (%) | 27 (60%) | 26 (58%) | 0.830 |
| Frequency of use of diuretics (%) | 10 (22%) | 5 (11%) | 0.157 |
As shown in Figs 1–3, in this study, SBP, DBP, and MAP were not significantly different prior to cannulation (P > 0.05). Yet, mean of all three blood pressure indicators significantly decreased in the lidocaine group compared with the placebo during the first to fifth minutes. And mean SBP showed a significant reduction during 1–5-min follow-up (P = 0.01).
Fig. 1.
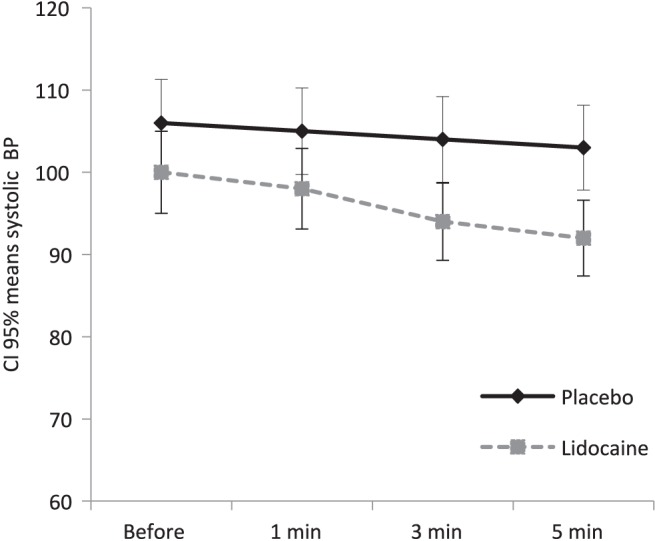
Confidence interval of 95%, mean SBP in lidocaine and placebo groups during follow-up period. According to repeat-measure ANOVA, administration of lidocaine significantly reduces mean SBP over time (P = 0.01)
Fig. 3.
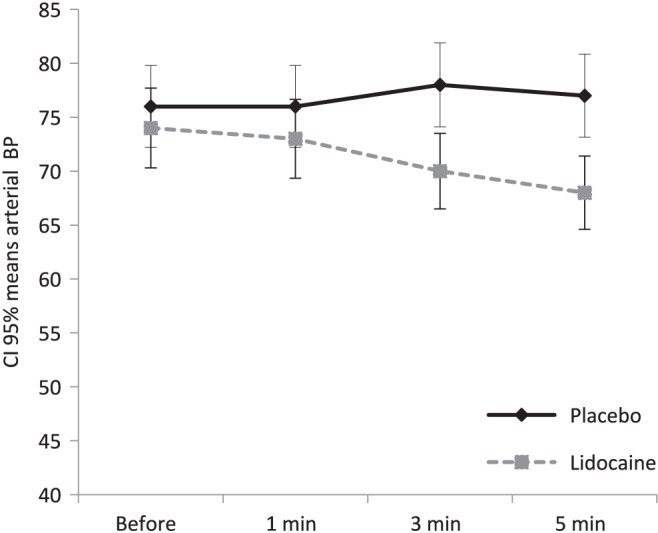
Confidence interval of 95%, mean arterial blood pressure in the lidocaine and placebo groups during follow-up period. According to repeat-measure ANOVA, administration of lidocaine significantly reduces mean arterial blood pressure over time (P = 0.006)
Mean DBP in the lidocaine group shows a significant reduction during 1–5-min follow-up (P = 0.016) (Fig. 2).
Fig. 2.
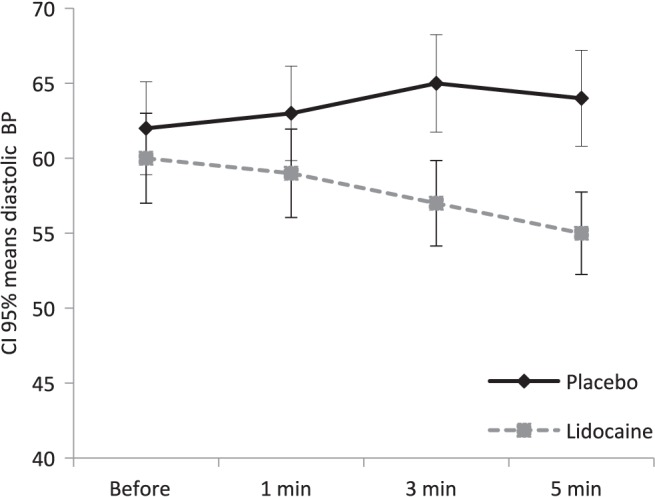
Confidence interval of 95%, mean DBP in lidocaine and placebo groups during follow-up period. According to repeat-measure ANOVA, administration of lidocaine significantly reduces mean DBP over time (P = 0.016)
Also, mean HR during follow-up period was similar in the two groups, and the difference was insignificant (P = 0.649) (Fig. 4). Mean CVP in the two groups during follow-up (except in the third minute) showed insignificant differences (P = 0.492) (Fig. 5).
Fig. 4.
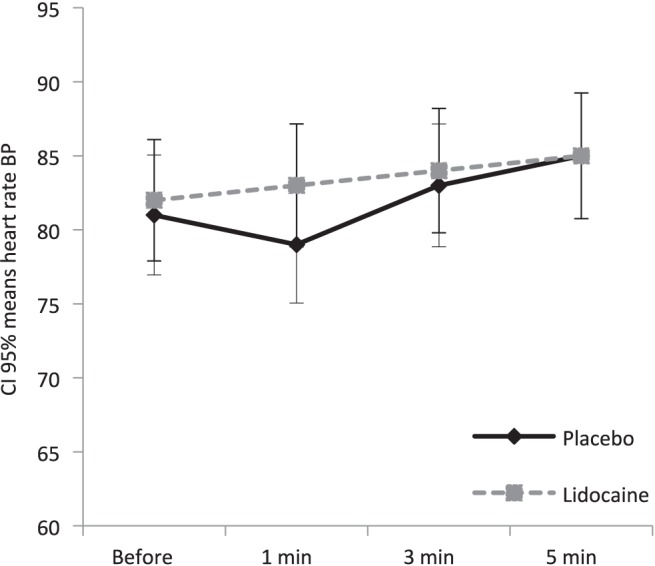
Confidence interval of 95%, mean HR in the lidocaine and placebo groups during follow-up period. According to repeat-measure ANOVA, administration of lidocaine led to similar mean HRs and insignificant variations in the two groups (P = 0.649)
Fig. 5.
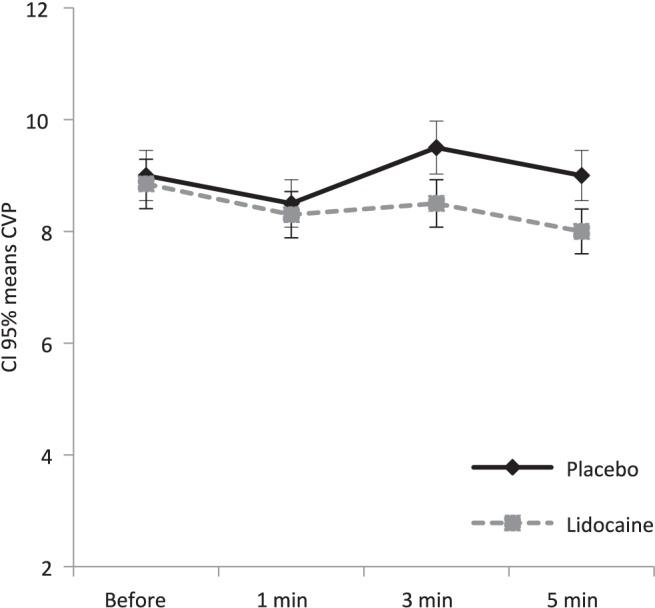
Confidence interval of 95%, mean CVP in the lidocaine and placebo groups during follow-up period. According to repeat-measure ANOVA, administration of lidocaine led to similar mean CVPs and insignificant variations in the two groups (P = 0.492)
Also, mean use of TNG was similar in the two groups and showed insignificant differences in the period after cannulation (P = 0.527) (Fig. 6).
Fig. 6.
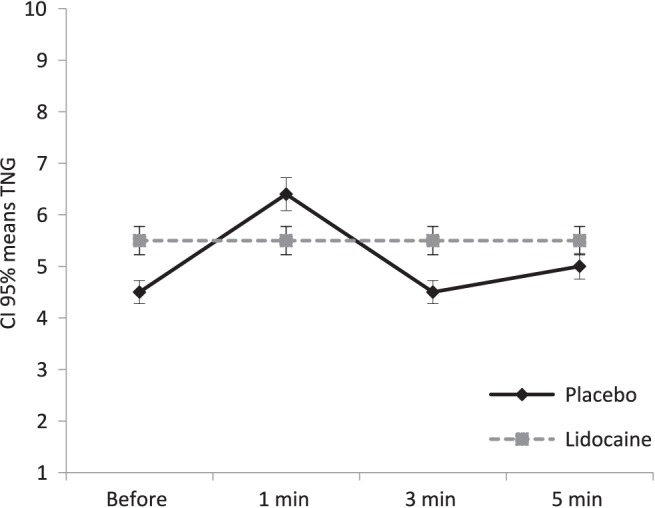
Confidence interval of 95%, mean TNG in the lidocaine and placebo groups during follow-up period
According to repeat-measure analysis of variance (ANOVA), administration of lidocaine led to similar mean TNG use and insignificant variations in the two groups (P = 0.527).
No particular side effect was recorded in the two groups of patients.
Discussion
This study demonstrated that administration of 1.5 mg/kg of lidocaine intravenously 90 s before aortic cannulation was effective in preventing SBP, DBP, and MAP rise, but no effect on HR or mean CVP during aortic cannulation.
In 1958, Nuunez and Bailey suggested aortic cannulation in cardiovascular bypass for the first time and applying this method gradually became commonplace [4]. In the late 1960s, femoral cannulation was proposed by Dewall and Levy and was widely used in Europe and United States.
Aortic cannulation had many advantages for cardiac surgery patients compared with other methods, including ease of application by shortening surgery time, arterial perfusion through the biggest cannulation size to stabilize cardiovascular bypass, and reduced risk of retrograde dissection in older patients. Currently, this technique is used in open heart surgeries [3]. Reported complications in this method include laceration and hemorrhage, hematoma, incorrect insertion, and aortic dissection. One of the causes of the latter case is sudden blood pressure rise and hemodynamic variations due to aortic cannulation that can lead to aortic dissection [5–7]. Aortic dissection due to aortic cannulation is rare, but is considered a fatal complication [8–10]. Incidence of this complication is about 0.16%, and despite its rarity, it has even been reported in infants [8]. As stated, hemodynamic variations can account for one of the predisposing factors of this complication. Sudden blood pressure rise and hemodynamic variations after cannulation, which is probably associated with cardiac sympathetic discharge due to cannulation during heart surgery, is considered one of the causes of aortic dissection. Although various methods are used to reduce in response to stress, such as systemic high-dose opioids, inhaling anesthetics, systemic drugs such as beta-blockers and alpha-2 agonists, and vasodilators, no specific study has been conducted on stress-reducing effect of lidocaine during cannulation thus far, which was investigated in this study.
Lidocaine is a local amide anesthetic drug considered for reducing stressful responses following cannulation [11]. Lidocaine is a strong inhibitor of abnormal cardiac activity, which seems to specifically affect sodium channels by blocking active and inactive sodium channels. Thus, lidocaine inhibits electrical activity of arrhythmia-producing depolarized tissues, with mild effect on electrical activity of normal tissues [12, 13].
-
(a)
In a study, using intratracheal lidocaine, cardiovascular effect of lidocaine in response to tracheal intubation was almost half compared with cases that did not use lidocaine.
-
(b)
Local use of lidocaine on aorta surface is a simple and effective method to reduce risk of sudden systemic blood pressure rising during aorta clamping.
-
(c)
Stretching receptors in aortic arch leads to responses at solitary nucleus (nucleus tractus solitaries) of cardiac center at medulla nucleus (medulla oblongata), which receives these messages through glossopharyngeal and vagus nerves. Stretching changes due to pressure cause baroreceptor reflexes, and intravenous lidocaine prevents increase in pressure by suppressing cardiovascular effects through baroreceptor reflex.
Thus, taking all these into account, a hypothesis whether intravenous lidocaine can reduce hemodynamic changes during aortic cannulation and reduce the risk of its complications is proposed. Some studies indicate that 1.5 mg/kg is the safe lidocaine dose, and hemodynamic responses can be reduced by administration of this dose [14]. Therefore, given the safety of this dose of lidocaine and importance of hemodynamic responses during aortic cannulation to reduce the risk of potential complications in patients undergoing heart surgery, in this study, the effect of 1.5 mg/kg dose of lidocaine during aortic cannulation was investigated. Various studies indicate that lidocaine stabilizes hemodynamics and reduces stress response in many cases. Accordingly, in this study, the effect of lidocaine at 1.5 mg/kg dosage, 90 s before aortic cannulation was investigated, and it is recommended that the effect of lidocaine be measured and compared at different times. It should be mentioned that some references report the maximum effect of lidocaine 3 min after injection.
Also, further studies should be conducted to measure the effect of lidocaine with other stress-reducing drugs.
Acknowledgement
The authors would like to thank all the individuals who participated in this study.
Funding Statement
Funding sources: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors’ contribution
All authors had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Their roles on all works of study were equal. All authors read and approved the final form of this manuscript.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1.Shimpo H, Miyake Y, Yada I: Cannulation of the distal descending thoracic aorta. Ann Thorac Surg 6, 2186–2187 (2000) [DOI] [PubMed] [Google Scholar]
- 2.Taguchi K, Mochizuki T, Takamura K, Matsumura M, Tsuchiya T: Aortic cannulation for cardiopulmonary bypass. Jpn J Surg 7, 44–47 (1977) [DOI] [PubMed] [Google Scholar]
- 3.Kuo J, Moorjani N, Unsworth-White J: Central cannulation through a standard left thoracotomy for surgery on the descending thoracic aorta. J Card Surg 21, 267–268 (2006) [DOI] [PubMed] [Google Scholar]
- 4.Hysi I, Guesnier L, Gautier L, Fabre O: Central venous cannulation and antegrade arterial perfusion for minimally invasive aortic valve surgery: Return to the basics. Int J Cardiol 186, 72–73 (2015) [DOI] [PubMed] [Google Scholar]
- 5.Osaki M, Caldarone CA, Dipchand AI: Extended aortic dissection following aortic cannulation in an infant. Pediatr Cardiol 29, 232–233 (2008) [DOI] [PubMed] [Google Scholar]
- 6.El-Tahan MR, Warda OM, Diab DG, Ramzy EA, Matter MK: A randomized study of the effects of perioperative i.v. lidocaine on hemodynamic and hormonal responses for cesarean section. J Anesth 23, 215–221 (2009) [DOI] [PubMed] [Google Scholar]
- 7.Liddicoat JE, Bekassy SM, DeBakey ME: Safe cannulation of the ascending aorta. Ann Thorac Surg 21, 70–71 (1976) [DOI] [PubMed] [Google Scholar]
- 8.Suenaga E, Sato M, Fumoto H, Kawasaki H, Koga S: Impact of transapical aortic cannulation for acute type A aortic dissection. Ann Thorac Cardiovasc Surg 21, 382–387 (2015) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benedetto U, Mohamed H, Vitulli P, Petrou M: Axillary versus femoral arterial cannulation in type A acute aortic dissection: Evidence from a meta-analysis of comparative studies and adjusted risk estimates. Eur J Cardiothorac Surg 48, 953–959 (2015) [DOI] [PubMed] [Google Scholar]
- 10.Terasaki T, Takano T, Fujii T, Seto T, Wada Y, Ohtsu Y, Komatsu K: Early and midterm results of transapical and right axillary artery cannulation for acute aortic dissection. J Cardiothorac Surg 10, 2 (2015) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jimenez N, Bradford H, Seidel KD, Sousa M, Lynn AM: A comparison of a needle-free injection system for local anesthesia versus EMLA for intravenous catheter insertion in the pediatric patient. Anesth Analg 102, 411–414 (2006) [DOI] [PubMed] [Google Scholar]
- 12.Çalış AS, Cagiran E, Efeoglu C, Ak AT, Koca H: Lidocaine versus mepivacaine in sedated pediatric dental patients: Randomized, prospective clinical study. J Clin Pediatr Dent 39, 74–78 (2014) [DOI] [PubMed] [Google Scholar]
- 13.Yoshie K, Tomita T, Takeuchi T, Okada A, Miura T, Motoki H, Ikeda U: Renewed impact of lidocaine on refractory ventricular arrhythmias in the amiodarone era. Int J Cardiol 176, 936–940 (2014) [DOI] [PubMed] [Google Scholar]
- 14.Khezri MB, Kayalha H: The effect of combined ephedrine and lidocaine pretreatment on pain and hemodynamic changes due to propofol injection. Acta Anaesthesiol Taiwan 49, 54–58 (2011) [DOI] [PubMed] [Google Scholar]


