Abstract
Introduction
Noise pollution in the operating rooms is one of the remaining challenges. Both patients and physicians are exposed to different sound levels during the operative cases, many of which can last for hours. This study aims to evaluate the noise pollution in the operating rooms during different surgical procedures.
Materials and methods
In this cross-sectional study, sound level in the operating rooms of Hamadan University-affiliated hospitals (totally 10) in Iran during different surgical procedures was measured using B&K sound meter. The gathered data were compared with national and international standards. Statistical analysis was performed using descriptive statistics and one-way ANOVA, t-test, and Pearson’s correlation test.
Results
Noise pollution level at majority of surgical procedures is higher than national and international documented standards. The highest level of noise pollution is related to orthopedic procedures, and the lowest one related to laparoscopic and heart surgery procedures. The highest and lowest registered sound level during the operation was 93 and 55 dB, respectively. Sound level generated by equipments (69 ± 4.1 dB), trolley movement (66 ± 2.3 dB), and personnel conversations (64 ± 3.9 dB) are the main sources of noise.
Conclusion
The noise pollution of operating rooms are higher than available standards. The procedure needs to be corrected for achieving the proper conditions.
Keywords: noise pollution, operating room, hospitals, Iran, sound
Introduction
Noise pollution is an unwanted or undesirable sound in peripheral environment. In other words, it is indefinite and irregular combination of sounds [1]. Noise pollution has many effects on humans, including hearing loss, emotion effects (feeling of physical discomfort in ears), impaired communication, psychosomatic effects on physical well-being, and inappropriate effects on the psychological states of people [2]. Much noise can also leave adverse effects on work efficiency and events. It can also cause impaired sleep and behavior, increased gastric intestinal activity, heart rate, blood pressure, respiratory rate, and oxygen consumption [3, 4]. One of the places where high levels of noise can have a significant effect on public health is hospitals. The first important phase to control noise pollution that is very important nowadays is to measure noise pressure level and the considered parameters and to compare it with standard parameters [5, 6].
In various parts of the world, the allowable noise has been defined at two levels. The first level is standards determined for various types of environment with different users and it depends naturally on kind of behavior, culture, and other factors involved in the given country. The second level is standards developed for noise-producing sources [2–6]. Fortunately, much attention has been paid to noise pollution in Iran in recent years, so that, according to Article 2 of the executive regulations to prevent noise pollution in 1999, any attempt causing noise pollution is prohibited [7]. It is worth mentioning that Article 2 of the regulation to prevent noise pollution approved in June 4, 2008 by board of ministers has determined the allowed outdoor noise pressure as 65 dB in Iran [8].
The mean noise level in the operating rooms in various studies is around 65–60 dB (A), but it may even exceed 100 dB (A) [9]. Much noise can affect patient care and disrupt the concentration during surgery. However, the most important adverse effect of excessive noise in the operating rooms is on staff dialogue. Unnecessary dialogue noise interferes with the performance of operations, since this type of noise mainly causes confusion, and it might hide the main and required noise [10].
The International Noise Council has stipulated that noise level in intensive care units of hospitals should not exceed the mean level of 45 dB during the day, 40 dB at sunset, and 30 dB at night [5]. US Environmental Protection Agency recommends that noise level in hospitals during the day should not be more than 35 dB. Association of Australian Acoustical Consultants also recommends that the background noise should not exceed 30 dB (A) [10].
If no action is taken in the operating rooms, background sound is about 13 dB (A). The highest noise in the operating rooms is the stage of preparation for surgery. During surgery, continuous noise caused by anesthesia ventilator is estimated to be 65 dB (A), 73 dB in surgical suction (A), and 70 dB in anesthesia device cleaner system (A). Intermittent noise sources include diathermy device and displacement of surgery devices [10]. To control noise pollution, it is very important to measure noise level and the considered parameters and to compare it with standard parameters. Noise pollution in the operating rooms, in addition to disturbing the anesthesia of patients, could reduce hearing level of staff and increase the possibility of errors in the conversations between the surgeon and staff. In addition, no comprehensive study has been conducted to date on noise pollution in the operating rooms of hospitals. Therefore, this study was conducted to evaluate the noise pollution in the operating rooms during the various surgeries in educational hospitals of Hamadan city in Iran. It also compared the obtained results with current standards.
Materials and Methods
To evaluate and measure noise levels in the operating rooms of hospitals affiliated to Hamadan University of Medical Sciences located in the city of Hamadan in Iran (Besat, Farshchian, Ekbatan, Fatemieh, and Shahid Beheshti), noise level gauge (available in physics laboratory of health department) was used. According to previous similar studies conducted in this area, measurements were performed in the range of 110–30 dB.
For this purpose, the project executors in each educational hospital participated in surgery procedures for 3 days and noise indicators and noise pollution level (NPL) in the operating rooms were measured at the location of surgeons and staff of operating rooms.
Noise parameters evaluated in this study include:
LAeq: noise level
L10: level that noise pressure level was higher than it was in 10% of the total measurement period.
L50: level that noise pressure level was higher than it was in 50% of the total measurement period.
L90: level that noise pressure level was higher than it was in 90% of the total measurement period.
- NPL: level of noise pollution calculated by the following equation for each of the locations.
Noise level gauge was calibrated daily before starting to measure and when the device was idle, using existing calibrator system.
The data relating to the measurement of noise level were collected from hospital operating rooms and when performing surgical procedures during 5-min three periods (5 min in start of surgery, 5 min middle of surgery, and 5 min at the end stage of surgery). After transferring of data to the computer and determining each of the noise indicators, data were analyzed using statistical descriptive tests in SPSS software. Comparison of NPL in the various operating rooms was performed using one-way ANOVA, and comparison of NPL and types of surgery was compared using Pearson’s correlation test. Comparison of noise pollution values with existing standards was conducted using t-test.
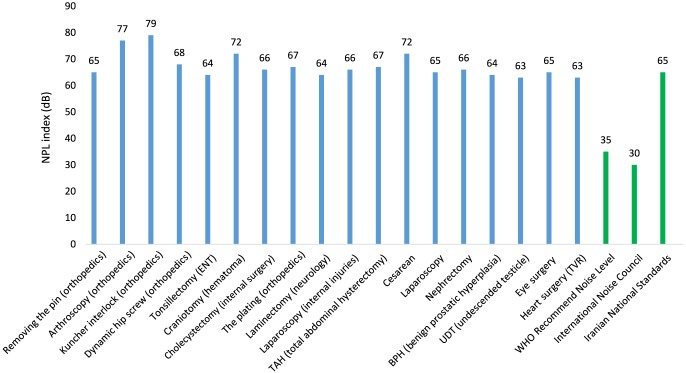
The International Noise Council has stipulated that noise level in intensive care units of hospital should not exceed 45 dB during the day, 40 dB at sunset, and 30 dB at night [5]. US Environmental Protection Agency and World Health Organization (WHO) recommend that noise level in hospitals during the day should not be more than 35 dB. Association of Australian Acoustical Consultants also recommends that background noise should be more than 30 dB (A) [10]. According to Article 2 of the regulation preventing noise pollution passed by board of ministers, outdoor noise level has been determined 65 dB in Iran [8]. The levels recommended by different organizations were compared with NPLs during various surgeries in selected hospitals in this study (Fig. 1 ).
Fig. 1.
Comparing allowed levels recommended by different organizations with NPLs during various surgeries
Results
According to the findings of this study (Table I ), the main sources of noise in each of operating rooms of Besat, Fatemieh, Shahid Beheshti, Farshchian, and Ekbatan Hospitals were “the noise of trolley movement in the corridor” (70 ± 4.5 dB); “noise of autoclave system” (67 ± 3.6 dB); “autoclave noise during dehydration” (71 ± 4.1 dB); “trolley movement noise in corridors” (71 ± 2.5 dB); and “trolley movement noise in corridors” (64 ± 3.1 dB), respectively.
Table I.
The main sources of noise in the operating rooms
| Hospital | Row | Sources of noise | Level of noise pollution (dB) |
|---|---|---|---|
| Besat | 1 | Trolley movement in the corridor | 70 ± 4.5 |
| 2 | Staff conversation | 69 ± 5.8 | |
| 3 | Hammering in the orthopedic operating room [dynamic hip screw (DHS)] | 64 ± 3.2 | |
| 4 | Suction while working | 64 ± 1.59 | |
| 5 | Pulse oximeter system | 61 ± 4.4 | |
| 6 | Drill during plating | 61 ± 4.2 | |
| Fatemieh | 1 | Noise of autoclave system | 67 ± 3.6 |
| 2 | Staff conversation | 62 ± 4.8 | |
| 3 | Staff and companions in the corridors | 60 ± 5.8 | |
| 4 | Suction while working | 59 ± 2.2 | |
| 5 | Opening the means and preparing the equipment for operation | 56 ± 4.5 | |
| 6 | Cautery system | 55 ± 3.2 | |
| Shahid Beheshti | 1 | Autoclave during dehydration | 71 ± 4.1 |
| 2 | Staff conversation | 62 ± 3.9 | |
| 3 | Suction while working | 56 ± 5.6 | |
| 4 | Trolley movement in corridors | 54 ± 2.1 | |
| 5 | Cautery system | 51 ± 4.4 | |
| 6 | Related to lighting system | 50 ± 1.4 | |
| Farshchian | 1 | Trolley movement noise in corridors | 71 ± 2.5 |
| 2 | Suction while working | 64 ± 3.1 | |
| 3 | Staff conversation | 63 ± 5.1 | |
| 4 | Active autoclave | 58 ± 4.4 | |
| 5 | UPS system | 56 ± 2.3 | |
| 6 | Related to phacoemulsification systems in eye surgery | 53 ± 2.2 | |
| Ekbatan | 1 | Trolley movement noise in corridors | 64 ± 3.1 |
| 2 | Opening and closing the equipment | 61 ± 5.7 | |
| 3 | Staff conversation | 56 ± 4.6 | |
| 4 | Cautery system in tricuspid valve repair/replacement (TVR) surgery | 56 ± 3.9 | |
| 5 | Suction while working | 54 ± 4.0 | |
| 6 | Related to phacoemulsification systems in eye surgery | 53 ± 4.2 |
The highest NPL related to orthopedic surgery and lowest noise pollution related to heart surgery (TVR) and laparoscopy. NPL index was about 79 dB for Kuncher interlock (orthopedics), 77 dB for arthroscopy (orthopedics), and 72 dB for cesarean section (hematoma) (Table II ).
Table II.
Comparing the NPL in various surgeries
| Row | Types of surgery | NPL index (in terms of dB) |
|---|---|---|
| 1 | Kuncher interlock (orthopedics) | 79 |
| 2 | Arthroscopy (orthopedics) | 77 |
| 3 | Craniotomy (hematoma) | 72 |
| 4 | Cesarean | 72 |
| 5 | DHS (orthopedics) | 68 |
| 6 | The plating (orthopedics) | 67 |
| 7 | TAH (total abdominal hysterectomy) | 67 |
| 8 | Cholecystectomy (internal surgery) | 66 |
| 9 | Laparoscopy (internal injuries) | 66 |
| 10 | Nephrectomy | 66 |
| 11 | Removing the pin (orthopedics) | 65 |
| 12 | Laparoscopy | 65 |
| 13 | Eye surgery | 65 |
| 14 | Tonsillectomy (ENT) | 64 |
| 15 | Laminectomy (neurology) | 64 |
| 16 | Benign prostatic hyperplasia | 64 |
| 17 | UDT | 63 |
| 18 | Heart surgery (TVR) | 63 |
Pearson’s correlation test also indicated a correlation between the types of surgery and the level of noise pollution. NPL index in laparoscopy surgery (internal injuries), cardiac surgery (TVR), and undescended testicle (UDT) was 61, 62, and 63 dB, respectively.
Discussion
Both patients and hospital staff benefit from quiet environment. In a quiet environment, fatigue and mental stress of health team staff are reduced, and patients do not suffer from physiological and psychological stress and their well-being improves. In a study conducted by Sener et al. [11] in 2010 in Turkey, the effect of noise on anxiety of patients who underwent surgery was studied. They stated that increased level of noise causes increased anxiety in patients, whereas background noise, especially music, can reduce the anxiety of patients.
The International Noise Council has stipulated that noise level in intensive care units of hospital should not exceed 45 dB during the day, 40 dB at sunset, and 30 dB at night [5]. US Environmental Protection Agency and WHO recommend that noise level in hospitals should not exceed 35 dB during the day. Association of Australian Acoustical Consultants also recommends that background noise should be more than 30 dB (A) [10]. According to Article 2 of the regulation preventing noise pollution passed by board of ministers, outdoor noise level should not exceed 65 dB in Iran [8].
A sudden noise that is 30 dB higher than the background noise (A) can cause jumping reflux among staff. This may affect patient care and disturb the concentration during surgery. Unexpected and non-controllable noise, even at low levels, also can cause impairment in performing complex surgical acts. In any case, the most important adverse effect of excessive noise in the operating rooms could lead to loss of reliability in conversation of staff. The background noise of the unnecessary dialogues affects surgery procedures more than other noises, since this type of noise mainly causes confusion, and it might hide the effects of main and required noise. West et al. [9] in their research to assess the rate of noise pollution and its reduction methods in the operating rooms of some hospitals in the USA in 2008 stated that many people’s hearing accuracy reduces and error in the conversations of staff increases under the conditions of excessive noise pollution. Finally, researchers state that it is necessary to use appropriate acoustic materials in the operating rooms to reduce noise pollution. Stringer and Haines [12] in their studies conducted in 2006 in Canada stated that by increasing noise in the operating rooms, the minimum noise intensity and the desired noise intensity by nurses increased from 62.8 to 64 dB and from 65.1 to 67.3 dB, respectively.
In line with the results of this study, Tsiou et al. [13] in their study to assess the level of noise pollution in a number of operating rooms in hospitals of Greece suggested that the level of noise in different surgeries is very different and the mean noise level (LAeq) in some surgeries reaches to maximum level of 71.9 dB. A study conducted by Zonouzi et al. [14] in 2006 on noise pollution in the neonatal intensive care units showed that sound pressure level (SPL) of all devices was 54–13 dB higher than the permitted limit. When devices are turned on, the background SPL increases by 6–9 dB, and staff activity increases background SPL by 2–8 dB.
It is worth noting that according to the findings of this study, the noise of falling objects was the main source of noise pollution with maximum intensity of 93 dB, followed by noise of hammering in the operating rooms and alarm of devices with intensity of about 77 and 78 dB, respectively. West et al. [9] in their research conducted in 2008 estimated the NPL up to 100 dB in some surgery procedures. In addition, Fritsch et al. [15] in 2010 in USA stated that the noise of some devices in the operating rooms increases up to 131 dB.
The results of this study indicated that the highest NPL related to orthopedic surgery, and the lowest NPL related to cardiac surgery (TVR) and laparoscopic surgery. NPL index was about 79 dB for Kuncher interlock (orthopedics) and 77 dB for arthroscopy (orthopedics). In addition, NPL index in laparoscopy surgery (internal injuries), cardiac surgery (TVR), and UDT was 61, 62, and 63 dB, respectively.
In line with the findings of this study, Kracht et al. [16] in their study to investigate noise levels in the operating rooms of Johns Hopkins Hospital in USA in 2006 suggested that the mean noise level in orthopedic surgeries is higher when compared with the other types of surgeries and it was approximately 66 dB, whereas noise level in other surgeries, such as cardiology, urology, and neurosurgery, was measured around 62–65 dB.
The level of daily exposure to noise should be kept as low as possible. This is accomplished by isolating the sources of noise, placing noise barriers, increasing absorption of walls and ceilings, or decreasing the time exposure of professionals involved.
To eliminate excess noise in the operating rooms, it may be necessary to adopt a multidisciplinary approach. An improvement in environment (background noise levels), the implementation of effective standards, and the focusing of the surgical team on noise matters are considered necessary changes.
Conclusion
The main sources of noise in each of operating rooms included the noise of trolley movement in the corridor, noise of hospital equipment, and staff conversation noise. The maximum noise level related to orthopedic surgery and the lowest NPL related to cardiac (TVR) and laparoscopy surgeries, respectively. Based on our findings, the noise of falling objects was the main source of noise pollution with maximum intensity of 93 dB, followed by noise of hammering in the operating rooms and alarm of devices with intensity of about 77 and 78 dB.
Funding Statement
Funding sources: All credits of this project were funded by Research and Technology Deputy of Hamadan University of Medical Sciences in Iran.
Authors’ contribution
MDG wrote the manuscript. MDG, KGS, MA, and AV collected the data of the manuscript. MDG and KGS contributed in data analysis. HAS designed the study, supervised the group, and revised the manuscript prior to submission.
Conflict of interest
The authors declare no conflict of interest in relation to the work.
References
- 1. Barbosa ASM, Cardoso MRA: Hearing loss among workers exposed to road traffic noise in the city of São Paulo in Brazil. Auris Nasus Larynx 32, 17–21 (2005) [DOI] [PubMed] [Google Scholar]
- 2. Bahreyni T, Pour Sadegh M, Tamjidi A, Bazri A: Sound pollutants in the industrial environments of Mashhad. Med J Mashhad Univ Med Sci 40, 27–32 (1997) [Google Scholar]
- 3. Ehteshmzadeh S. (1997): Workers exposure to high noise level in environment and public place. Proceedings of the 1st Scientific Congress about Noise and Its Effect on Human, Tehran, Iran, pp. 36–36 [in Persian] [Google Scholar]
- 4. Gerhardt KJ, Abrams R: Fetal exposures to sound and vibroacoustic stimulation. J Perinatol 20, 21–30 (2000) [DOI] [PubMed] [Google Scholar]
- 5. Liu EH, Tan S-M: Patients’ perception of sound levels in the surgical suite. J Clin Anesth 12, 298–302 (2000) [DOI] [PubMed] [Google Scholar]
- 6. Way TJ, Long A, Weihing J, Ritchie R, Jones R, Bush M, Shinn JB: Effect of noise on auditory processing in the operating room. J Am Coll Surg 216, 933–938 (2013) [DOI] [PubMed] [Google Scholar]
- 7. IEPO (2005): Iranian Environmental Protection Organization Law and Regulation (2nd ed.) IRAN-EP0 Press, Tehran: [Google Scholar]
- 8. Kayvani N. (2004): National Environmental Protection Organization Environmental Criteria and Standards (1st ed). Dayereh Sabz Publications, Tehran, pp. 13–14 [in Persian] [Google Scholar]
- 9. West J, Busch‐Vishniac I, King J, Levit N: Noise reduction in an operating room: A case study. J Acoust Soc Am 123, 3677 (2008) [Google Scholar]
- 10. Kurmann A, Peter M, Tschan F, Mühlemann K, Candinas D, Beldi G: Adverse effect of noise in the operating theatre on surgical‐site infection. Br J Surg 98, 1021–1025 (2011) [DOI] [PubMed] [Google Scholar]
- 11. Sener E, Koylu N, Ustun F, Kocamanoglu S, Ozkan F: The effects of music, white noise and operating room noise on perioperative anxiety in patients under spinal anesthesia: 8AP3-3. Eur J Anaesthesiol 27, 133 (2010) [Google Scholar]
- 12. Stringer B, Haines T: Can operating room nurses accurately classify noise exposures? J Acoust Soc Am 120, 3199 (2006) [Google Scholar]
- 13. Tsiou C, Efthymiatos G, Katostaras T: Noise in the operating rooms of Greek hospitals. J Acoust Soc Am 123, 757–765 (2008) [DOI] [PubMed] [Google Scholar]
- 14. Zonouzi F, Ranjbarian M, Afjeie SA: Evaluation of noises in neonatal intensive care unit in Mofid Children’s Hospital. Med Sci J Islamic Azad Univ-Tehran Med Branch 16, 129–134 (2006) [Google Scholar]
- 15. Fritsch MH, Chacko CE, Patterson EB: Operating room sound level hazards for patients and physicians. Otol Neurotol 31, 715–721 (2010) [DOI] [PubMed] [Google Scholar]
- 16. Kracht J, Busch‐Vishniac IJ, West JE: Operating room noise at Johns Hopkins Hospital. J Acoust Soc Am 119, 3385 (2006) [DOI] [PubMed] [Google Scholar]