Abstract
Purpose:
To identify the morbidity patterns causing blindness in children attending schools for the blind in Chennai and comparing our data with similar studies done previously.
Methods:
A cross-sectional prevalence study was carried out in two schools for the blind in Chennai. Blind schools were visited by a team of ophthalmologists and optometrists. Students with best-corrected visual acuity (BCVA) worse than 3/60 in the better eye were included and relevant history was noted. Every student underwent anterior segment evaluation and detailed fundus examination. Morbidity of the better eye was taken as cause of blindness. Health records maintained by the school were referred to wherever available.
Results:
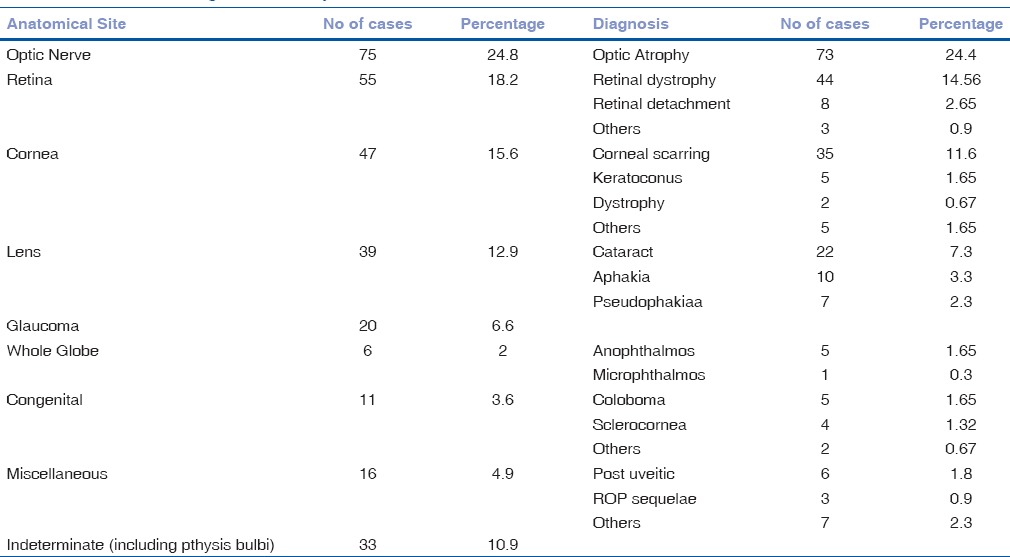
The anatomical causes of blindness include optic nerve disorders in 75 (24.8%) cases, retinal disorders in 55 (18.2%), corneal disorders in 47 (15.6%), lens-related disorders in 39 (12.9%), congenital anomalies in 11 (3.6%), and congenital glaucoma in 20 (6.6%) cases. The whole globe was involved in six cases (1.99%). Among conditions causing blindness, optic atrophy seen in 73 (24.17%) cases was the most common, followed by retinal dystrophy in 44 (14.56%), corneal scarring in 35 (11.59%), cataract in 22 (7.28%), and congenital glaucoma in 20 (6.6%) cases.
Conclusion:
It was found that avoidable causes of blindness were seen in 31% of cases and incurable causes in 45%. Optic nerve atrophy and retinal dystrophy are the emerging causes of blindness, underlining the need for genetic counseling and low vision rehabilitation centers, along with a targeted approach for avoidable causes of blindness.
Key words: Blind school, childhood blindness, ocular morbidity
Blindness is a worldwide problem with a significant social and economic impact on society. The WHO has defined blindness as visual acuity worse than 3/60 in the better eye with best correction.[1] Childhood blindness is an important cause contributing to the burden of blindness worldwide.[2] Data on the prevalence and causes of blindness in children are required for planning preventive and curative services. As per a 2001 survey, the prevalence of childhood blindness in India is 0.8/1000,[3] with almost half of the causes being preventable or treatable.
Although the prevalence of blindness in children is relatively low compared to adult populations, it negatively affects the development, education and employment opportunities of children, as well as the quality-adjusted life years of society as a whole. This can have far-reaching implications for the quality of life of children and the affected families.[4]
Information on the major causes of blindness in children is required to plan effective programs for prevention of the same.[5] Population-based accurate data on the causes of childhood blindness are difficult to obtain in a developing country like India, as very large sample sizes would be required for cross-sectional surveys. Examination of children in specialty institutions and tertiary care centers has been used to provide data on childhood blindness, but possible sources of bias must be borne in mind due to regional differences in the population under study.
The variability in the major causes of blindness in children from different parts of the world is determined by socioeconomic development and the availability of primary eye care services.
In developed countries, lesions of the optic nerve predominate as the cause of blindness, whereas corneal scarring is the major cause in low-income countries.[6] The most frequently affected parts are the whole globe, cornea, retina, optic nerve, and lens.[7] India has around 320,000 children with blindness, and hence childhood blindness has been given special priority in the Vision 2020 program.[8] Periodic population-based surveys are thus important to track changing trends in the causes of blindness and evaluate the effectiveness of preventive programs.
Methods
This cross-sectional study was conducted by visiting the following schools for the blind in Chennai.
Little Flower Convent, T Nagar, Chennai
St. Louis school for the Blind, Adyar, Chennai.
After getting clearance from the Institutional Ethics Committee, the schools were visited. Written informed consent for the study was obtained from the headmaster/principal of the school and the parents of the students.
The UNICEF defines childhood as lasting till the age of 16 years. As per the WHO, blindness is defined as visual acuity of worse than 3/60 in the better eye.[1] Inclusion criteria included students up to 16 years of age with BCVA of worse than 3/60 in the better eye. A total of 302 students satisfied the criteria and were included in the study.
A team comprising ophthalmologists and optometrists visited the school premises to examine the students. Detailed history of all students, including family history, was noted. Visual acuity testing using Snellen chart and tumbling E chart was done. For children unable to comprehend E chart, ability to count fingers and to perceive light was assessed. Anterior segment examination was done using a torch with magnifying loupe and slit lamp. This was followed by a detailed fundus examination after dilatation with indirect ophthalmoscope. Children were examined in the presence of their class teachers. Health records maintained by the school were assessed wherever possible.
The children were classified on the basis of the anatomical site of their defect. Congenital anomalies comprising involvement of various anatomical structures were grouped separately.
In cases where both eyes had different conditions, the diagnosis of the better eye was taken as the cause of blindness. Cases in which primary pathology could not be ascertained were put in a separate group. SPSS 11.0 was used for data entry and analysis.
Definitions
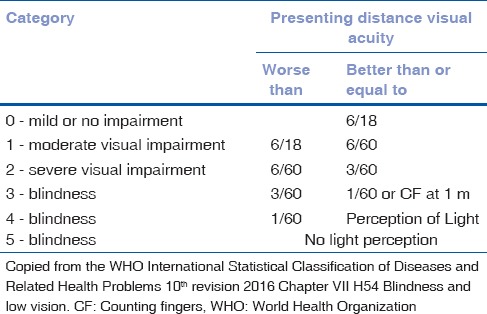
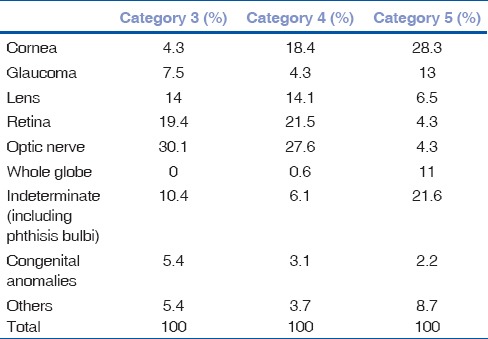
The WHO classifies blindness as best-corrected visual acuity (BCVA) worse than 3/60 in better eye.[1] It can be further categorized. Category 3 includes BCVA worse than 3/60 but better than 1/60. Category 4 includes BCVA worse than 1/60 up till perception of light. Category 5 includes absolute blindness [Table 1].
Table 1.
The World Health Organization classification of visual impairment/blindness
Results
A total of 302 students fulfilling the inclusion criteria were included in the study. Out of the 302 students, 141 were male (46.7%) and 161 were female (53.3%). The mean age of participants was 9.2 years with minimum age being 5 years and maximum being 16 years.
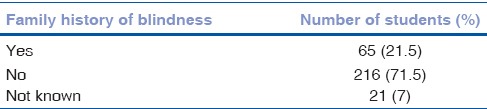
Out of 302 students, two had albinism whereas one had associated congenital talipes equinovarus. A total of 65 students (21.5%) had a history of blindness in the family, whereas 216 students (71.5%) did not [Table 3].
Table 3.
Family history statistics
All participants included in the study had BCVA of < 3/60 (the WHO criteria for blindness) and were classified into WHO categories as per visual acuity in the better eye.
Of 302 students, 46 (15.2%) had absolute blindness with no PL (Category 5). Among the remaining, 93 (30.8%) were in the WHO Category 3 whereas 163 (53.4%) had Category 4 visual impairment [Table 2].
Table 2.
Categories of blindness in students
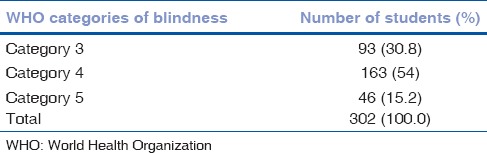
Among patients with no PL vision, 7 (15.2%) had a positive family history of blindness.
Among students giving positive family history, 7 (10.2%) had absolute blindness, 37 (56.92%) had Category 4 visual impairment, and 21 (32.3%) falling in Category 3.
Among the anatomical causes of blindness, the optic nerve was found to be the affected site in 75 (24.8%) cases, whereas retinal disorders were seen in 55 (18.2%). Other sites included cornea in 47 (15.6%) cases, lens in 39 (12.9%) cases, congenital anomalies in 11 (3.6%) cases, and whole globe anomalies in 6 (2%) cases. Congenital glaucoma and buphthalmos were found in 20 (6.6%) cases. Students for whom the primary cause of blindness could not be made out were grouped separately as indeterminate: 33 (10.9%) cases. This included conditions such as phthisis bulbi for which primary etiology was not known [Table 4].
Table 4.
Anatomical categories and major causes of blindness in children
Corneal disorders, whole globe anomalies, and indeterminate causes contributed more to Category 5 blindness, whereas optic nerve lesions and retinal disorders contributed primarily to Category 3 and Category 4 [Table 5].
Table 5.
Contribution of each anatomical cause in different categories of visual impairment
Among conditions causing blindness, optic atrophy (73) (24.17%) was the most common cause of blindness, followed by retinal dystrophy in 44 (14.56%), corneal scarring in 35 (11.59%), cataract in 22 (7.28%), congenital glaucoma in 20 (6.6%), aphakia in 10 (3.3%), pseudophakia in 7 (2.3%), retinal detachment in 8 (2.65%), and microphthalmos in 5 (1.66%). Other miscellaneous causes were seen in 16 (5.29%) cases including retinopathy of prematurity and postuveitic sequelae.
Discussion
This study of data regarding childhood blindness is important as it reflects the burden of the problem in our country. Of the 407 million children in the pediatric age group, 320,000 are blind apart from 9.2 million children who have refractive errors.[9]
There are regional variations in the data collected from across the country due to unequal distribution of health-care services. In previous studies, corneal scarring due to Vitamin A deficiency and measles were the most common causes of blindness.[10] However, later studies have demonstrated a change in trend with globe anomalies and retinal causes becoming more common.[11,12,13] This change can be attributed partly to successful immunization programs implemented in the country, although bias due to different population samples must be borne in mind.
In the present study, the most common cause of blindness was optic nerve atrophy (24.17%). This is in contrast with recent studies in which whole globe anomalies were the most common anatomical cause of blindness.[12,13] The reason for this difference is difficult to ascertain, but may be attributed to the fact that in our study, we have grouped conditions caused due to unknown etiology such as phthisis bulbi separately. Furthermore, many studies have taken inclusion criterion as vision worse than 6/60, but in our study, it was worse than 3/60, as defined by the WHO. As our study was conducted in an urban setting, regional bias might have played a part. Retinal dystrophies (14%) were the second most common cause and are hereditary in etiology and hence untreatable.
Preventable and treatable causes of blindness were present in a significant number of patients.
Of preventable causes, corneal scarring contributed to 11.59% of cases (35 out of 302). The exact cause of corneal scarring was difficult to gauge at this time but can be attributed to Vitamin A deficiency, measles, and trauma. Among treatable causes, lens-related causes and glaucoma contributed to 19.5% of cases.
Cause of blindness could not be established in 10.9% of cases. This reflects limitations due to the absence of proper blindness registers, lack of health records of the children as well as lack of examination of family members of some children. Retinopathy of prematurity was seen in three cases.
Overall, 31% of children had either preventable or treatable causes of blindness, which was comparable to previous studies.[14] These figures indicate the importance of health programs running at the primary level as well as need for continuous surveillance of these strategies. The incidence of preventable corneal blindness has come down in the past decade owing to effective immunization coverage, health education, and nutrition supplementation programs. A wider coverage and target-specific approach should be continued for the elimination of preventable causes of blindness, as per VISION 2020.
There is a need for pediatric ophthalmic services in India at the community level for treatable conditions such as cataracts, aphakia, and glaucoma. This can be achieved by providing pediatric eye care services with facilities for early screening and intervention. One pediatric eye care center per 10 million people is the recommended norm.[15]
Recent studies indicate that incurable conditions such as optic atrophy, retinal dystrophies, and congenital anomalies including whole globe anomalies are emerging as the major cause of blindness and visual impairment in children (44.3% of cases). This is in contrast to previous studies, as well as the data collected from underdeveloped countries, in which corneal causes, retinopathy of prematurity, and lens-related causes were important. The exact reason for the changing trend is difficult to ascertain, but increased health services might have a role to play. There might be regional differences in the trends depending on whether the study is conducted in a rural population in remote areas or an urban setup.
A total of 21.5% (65 out of 302) of children gave a history of at least one of the parents or siblings suffering from blindness. This is comparable with recent studies in India and Indonesia.[16]
In upcoming years, genetic counseling will play an important role, at least in preventing hereditary causes of blindness.
As VISION 2020 aims at eliminating preventable and treatable causes of blindness, a comprehensive approach is required for the effort. It should include monitoring and augmentation of the current screening and immunization programs at the primary level as well as establishment of pediatric ophthalmic surgery units.
A large population-based cluster study is required with a large sample size to confidently confirm the changing trends in childhood blindness patterns.
As avoidable causes of blindness are decreasing, a focus should also be placed on screening and rehabilitation of children with nonavoidable blindness. This can be done by providing rehabilitation and vocational training.[17]
Conclusion
Childhood blindness has been a special priority area in VISION 2020. The aim is to decrease the global level of childhood blindness from 7.5/10,000 children in 1997 to 4/10,000 children in 2020. Due to an active and aggressive approach, we have been able to bring down the incidence of avoidable causes of blindness to some extent. Still, more effort is required in terms of providing health-care services. Avoidable causes of blindness include corneal scarring due to Vitamin A deficiency, cataracts, glaucoma, and ROP, which have to be dealt with effectively.
Recent data have indicated an increasing prevalence of nonavoidable blindness. In such a scenario, there is an urgent need for rehabilitation programs for these children to enable them to lead a rewarding and self-dependent life in the future.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. International Statistical Classification of Diseases and Related Health Problems, (ICD-10) WHO Version for 2016. 10th Revision. Ch. 7. Geneva: World Health Organization; 2016. [Last accessed on 2017 May 15]. H54 blindness and low vision. Available from: http://www.who.int/classifications/icd/en/ [Google Scholar]
- 2.World Health Organization. WHO/NMH/PBD/12.01. Geneva: WHO; 2012. [Last accessed on 2017 May 15]. Global Data on Visual Impairments 2010. Available from: http://www.who.int/blindness/publications/globaldata/en . [Google Scholar]
- 3.Directorate General of Health Services, National Program for Control of Blindness. [Last accessed on 2017 Apr 19]. Available from: http://www.npcb.nic.in .
- 4.Rahi JS, Gilbert CE, Foster A, Minassian D. Measuring the burden of childhood blindness. Br J Ophthalmol. 1999;83:387–8. doi: 10.1136/bjo.83.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gilbert CE, Anderton L, Dandona L, Foster A. Prevalence of visual impairment in children: A review of available data. Ophthalmic Epidemiol. 1999;6:73–82. doi: 10.1076/opep.6.1.73.1571. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Prevention of Blindness and Visual Impairment: Priority Eye Diseases. [Last accessed on 2017 April 19]. Available from: http://www.who.int/blindness/causes/priority/en/index3.html .
- 7.Bhattacharjee H, Das K, Borah RR, Guha K, Gogate P, Purukayastha S, et al. Causes of childhood blindness in the Northeastern states of India. Indian J Ophthalmol. 2008;56:495–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Gilbert C, Rahi J, Quinn G. Visual impairment and blindness in children. In: Johnson G, Minassian D, Weale W, West S, editors. Epidemiology of Eye Disease. 2nd ed. UK: Arnold Publishers; 2003. [Google Scholar]
- 9.Office of the Registrar General and Census Commissioner, India. Population Projections for India and States 2001-2026. Report of the Technical Group on Population Projections Constituted by the National Commission on Population. (Revised; December, 2006) [Last accessed on 2017 Apr 05]. Available from: http://www.nrhm-mis.nic.in .
- 10.Rahi JS, Sripathi S, Gilbert CE, Foster A. Childhood blindness in India: causes in 1318 blind school students in nine states. Eye (Lond) 1995;9(Pt 5):545–50. doi: 10.1038/eye.1995.137. [DOI] [PubMed] [Google Scholar]
- 11.Gogate P, Deshpande M, Sudrik S, Taras S, Kishore H, Gilbert C. Changing pattern of childhood blindness in Maharashtra, India. Br J Ophthalmol. 2007;91:8–12. doi: 10.1136/bjo.2006.094433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hornby SJ, Adolph S, Gothwal VK, Gilbert CE, Dandona L, Foster A. Evaluation of children in six blind schools of Andhra Pradesh. Indian J Ophthalmol. 2000;48:195–200. [PubMed] [Google Scholar]
- 13.Bhalerao SA, Tandon M, Singh S, Dwivedi S, Kumar S, Rana J. Visual impairment and blindness among the students of blind schools in Allahabad and its vicinity: A causal assessment. Indian J Ophthalmol. 2015;63:254–8. doi: 10.4103/0301-4738.156930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gogate P, Kishore H, Dole K, Shetty J, Gilbert C, Ranade S, et al. The pattern of childhood blindness in Karnataka, South India. Ophthalmic Epidemiol. 2009;16:212–7. doi: 10.3109/09286580902999405. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. WHO/PBL/00.71. Geneva: WHO; 2000. Preventing Blindness in Children: Report of WHO/IAPB Scientific Meeting. Program for the Prevention of Blindness and Deafness. [Google Scholar]
- 16.Sitorus R, Preising M, Lorenz B. Causes of blindness at the “Wiyata Guna” school for the blind, Indonesia. Br J Ophthalmol. 2003;87:1065–8. doi: 10.1136/bjo.87.9.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gilbert C, Muhit M. Twenty years of childhood blindness: What have we learnt? Community Eye Health. 2008;21:46–7. [PMC free article] [PubMed] [Google Scholar]


