Abstract
Background:
Psychocardiological researches have suggested a central role of 5-hydroxytryptamine (5-HT) on psychocardiological mechanism. This study aimed to further explore the central role of 5-HT and pretreatment effects of XinLingWan on rats with myocardial infarction (MI) and/or depression.
Methods:
Ninety Sprague-Dawley rats were randomly divided into three groups: MI group, depression group, and MI + depression group (n = 30 in each group). Each group was then divided into three subgroups (n = 10 in each subgroup): a negative control subgroup (NCS), a Western medicine subgroup (WMS), and a traditional Chinese medicine subgroup (TCMS), which were received pretreatment once a day for 4 weeks by saline, 20 mg/kg sertraline mixed with 2 ml saline, and 40 mg/kg XingLingWan mixed with 2 ml saline, respectively. Different rat models were established after different pretreatments. Rats were then sacrificed for detection of serum 5-HT, platelet 5-HT, 5-HT2A receptors (5-HT2AR), and serotonin transporter (SERT). Data were analyzed by one-way analysis of variance (ANOVA) and least-significant difference (LSD) testing.
Results:
MI group: compared with NCS, there was a significant increase in WMS and TCMS of serum 5-HT (176.15 ± 11.32 pg/ml vs. 334.50 ± 29.09 pg/ml and 474.04 ± 10.86 pg/ml, respectively, both P = 0.000), platelet 5-HT (129.74 ± 27.17 pg/ml vs. 322.24 ± 11.60 pg/ml and 340.4 5 ± 17.99 pg/ml, respectively, both P = 0.000); depression group: compared with NCS, there was a significant increase in WMS and TCMS of serum 5-HT (194.69 ± 5.09 pg/ml vs. 326.21 ± 39.98 pg/ml and 456.33 ± 23.12 pg/ml, respectively, both P = 0.000), platelet 5-HT (175.15 ± 4.07 pg/ml vs. 204.56 ± 18.59 pg/ml and 252.03 ± 22.26 pg/ml, respectively, P = 0.004 and P = 0.000, respectively); MI + depression group: compared with NCS, there was a significant increase in both WMS and TCMS of serum 5-HT (182.50 ± 10.23 pg/ml vs. 372.55 ± 52.23 pg/ml and 441.76 ± 23.38 pg/ml, respectively, both P = 0.000) and platelet 5-HT (180.83 ± 11.08 pg/ml vs. 221.12 ± 22.23 pg/ml and 265.37 ± 29.49 pg/ml, respectively, P = 0.011 and P = 0.000, respectively).
Conclusions:
By elevating the amount of 5-HT and modulating 5-HT2AR and SERT levels in serum and platelets, XinLingWan and sertraline were found to exert pretreatment effect on rat models of MI and/or depression.
Keywords: 5-Hydroxytryptamine, Depression, Myocardial Infarction, Selective Serotonin Reuptake Inhibitors, Traditional Chinese Medicine
INTRODUCTION
Over the past 20 years, the perspective of psychocardiology, according to which there are relationships between psychiatric and cardiac manifestations of disease, has been increasingly important in clinical practice. Psychiatric and cardiac symptoms often occur together, for example, coronary heart disease (CHD) combined with depression, heart failure or hypertension comorbid anxiety, symptoms of heart disease with panic attacks, or anxiety/depression arise after percutaneous coronary intervention.[1] Normally, the co-occurrence often poses a substantial adverse impact on the health and quality of life of patients.[1] This study was aimed to further characterize the role played by 5-hydroxytryptamine (5-HT) in psychocardiological mechanism, and the pretreatment effect of XinLingWan on rats with myocardial infarction (MI) and/or depression.
CHD, due to consequent myocardial ischemia, is the leading cause of death worldwide. Several risk factors, both long established and newly discovered, have been shown to contribute to the incidence of CHD. Of the newly discovered factors, the importance and prognostic relevance of depression have been proven in several large, prospective studies.[2,3] A meta-analysis[1] by the National Institutes of Health reported that, among patients with coronary disease, approximately 20% had been diagnosed with major depression and 47% suffered from depression at the time of the study. In addition, it has been reported that the depression morbidity of patients who have sustained MI is as high as 20%,[4] and that, in patients with stable CHD, the relationship between depression and cardiac mortality may last for more than 20 years.[5]
There are three possible ways of demonstrated association between depression and CHD: CHD may cause depression, depression may cause CHD, or both diseases may share an underlying cause.[6] The precise mechanism accounting for the association remains unknown, but an important role of 5-HT has been proposed: excessive 5-HT in depression may increase platelet activity and trigger platelet aggregation, which may trigger the plaque formation associated with CHD.[2,7,8]
Selective serotonin reuptake inhibitors (SSRIs), a type of antidepressant, can reduce platelet activation by depleting serotonin storage. It can do so because it possesses a high affinity for the serotonin transporter (SERT), a pharmacological mechanism that appears to be unique among antidepressants. It is widely recognized that, in addition to managing depression, SSRIs are associated with a reduced likelihood of sustaining MI. Data from the Sertraline Antidepressant Heart Attack Randomized Trial (SADHART), and from the Enhancing Recovery in Coronary Heart Disease (ENRICHD) study, have demonstrated that SSRIs may not only be effective in the treatment of depression, but also may reduce the risk of cardiac events and improve cardiac outcomes.[9] Specifically, the SADHART study suggested that cardiovascular parameters were improved after treatment with sertraline (a SSRI). Furthermore, mortality and recurrence rates were lower in patients given sertraline than in those who did not receive this treatment.[10] In the ENRICHD study, 1849 patients with depression after MI were given SSRIs and followed up for 29 months. Compared with patients who were not given SSRIs, these patients showed a 43% decrease in mortality and/or recurrent infarction.[11] Thus, it is reasonable to conclude that SSRIs can manage psychocardiological disease.
Nevertheless, the possibility of unintended side effects of SSRI administration must be considered. There have been case reports and retrospective studies that have implicated SSRIs in various bleeding risks, such as bruising, spontaneous ecchymoses, and increased bleeding time.[12] After comprehensive analysis of the methodology of several of these studies, it is premature to conclude that SSRIs are a safe treatment in patients with heart disease.
Using certain traditional Chinese herbs, however, it may be possible to realize the benefits of psychocardiological treatment with SSRIs without acquiring this risk of bleeding. Panax notoginseng, for example, can promote the clotting of blood and improve its circulation. To provide evidence of the benefit of traditional Chinese medicine (TCM) for the treatment of psychocardiological disease, we performed a pretreatment intervention experiment with XinLingWan by modern pharmacological study methodology.
XinLingWan is a type of TCM that is composed of musk, toad venom, bear gall, synthetic bovine bezoar, borneol, pearl, ginseng, and P. notoginseng. It was developed many years ago to treat patients with CHD, dysfunctional heart disease, arrhythmia, and hypertension, but there is currently a lack of data concerning the mechanism by which it carries out its therapeutic function. This study was designed to provide such data by analyzing the levels of 5-HT, 5-HT2A receptors (5-HT2AR), and SERT in the rat models of psychocardiological disease, which were pretreated with XinLingWan, sertraline, or saline.
METHODS
Ethical approval
All animals were managed according to the relevant guidelines. The experiment was approved by the Medical Ethics Committee of Beijing Anzhen Hospital.
Experimental animals
Ninety Sprague-Dawley rats, weighing between 180 g and 220 g, were purchased from the Jiangsu Medical Laboratory Animal Center. The rats were randomized to three disease model groups (n = 30 in each group): a MI group, a depression group, and an MI with comorbid depression (MI + depression) group. Each group was then further divided into three different pretreatment subgroups (n = 10 in each subgroup): a negative control subgroup (NCS), a Western medicine subgroup (WMS), and a traditional Chinese medicine subgroup (TCMS). After 4 weeks of pretreatment, procedures were performed on the rats to generate the three disease models. Rats were then sacrificed, and the levels of serum 5-HT, platelet 5-HT, 5-HT2AR, and SERT were detected.
Pretreatment method
In NCS, rats were given 2 ml saline by gavage. In WMS, rats were given 20 mg/kg sertraline (Huirui Co. Ltd. Dalian, China), dissolved in 2 ml saline, by gavage. In TCMS, rats were given 40 mg/kg XinLingWan (Guangdong Tai’an Tang Co. Ltd., Guangdong, China) by gavage. All pretreatments were administered once daily for 4 weeks.
Establishment of myocardial infarction model
To induce MI, rats were first anesthetized by intramuscular injection with ketamine (40 mg/kg) and xylazine (1 mg/kg). MI induction surgery was then performed according to the procedure described by Akbayand Onur:[13] the left chest was incised to expose the anterior surface of the heart after anesthesia, the left anterior descending artery was cauterized at the midpoint between its origin and the cardiac apex, and the chest was then closed.
Establishment of depression model
The forced swimming test (FST) was administered according to the Porsolt method which was designed to screen antidepressants.[14,15] Rats were put into a cylindrical PYREX tank (46 cm in height, 20 cm in diameter, and 30 cm in depth) which contained water, maintained at 23–25°C. They underwent a 15-min swimming test, and then were dried (under a warm air current). After 24 h, the rats were given another 5-min swimming test, during which movement frequency was assessed.
Establishment of myocardial infarction + depression model
The rats were firstly conducted with MI surgery as described above.[13] Three days after MI was induced by the method described above,[13] FST was administered.[14,15]
5-hydroxytryptamine, 5-hydroxytryptamine 2A receptor, and serotonin reuptake transporter detection
All rats were sacrificed after 12 h fasting. Two milliliter heart blood was collected into chilled tubes containing ethylenediaminetetraacetic acid K2 (BD Co., Ltd.). The blood was centrifuged at 1000 ×g for 15 min at room temperature to obtain platelet-rich plasma (PRP). To discard supernatant and to collect platelets, the PRP was centrifugated at 1000 ×g and 4°C for 10 min.
The level of 5-HT in serum and levels of 5-HT, 5-H2AR, and SERT in platelets were assayed by enzyme-linked immunosorbent assay (ELISA), as recommended by the Immuno-Biological Laboratory.[16] The ELISA kit was purchased from Nanjing Yifeixue Biotech Co., Nanjing, China (No. EFXER 00123).
Statistical analysis
Statistical analysis was performed with SPSS software (Version 19.0; IBM Corp., Chicago, IL, USA). Data were represented as mean ± standard deviation (SD). Different outcomes produced by the three pretreatments were compared with one-way analysis of variance (ANOVA). Comparisons with least-significant difference testing (LSD) were performed between the NCS and WMS or TCMS and between the WMS and TCMS. A value P < 0.05 was considered statistically significant.
RESULTS
5-hydroxytryptamine level in serum
Myocardial infarction group
Compared to NCS, there was a significant increase in WMS and TCMS of serum 5-HT (176.15 ± 11.32 pg/ml vs. 334.50 ± 29.09 pg/ml and 474.04 ± 10.86 pg/ml, respectively, both P = 0.000). 5-HT concentration in the serum of TCMS was significantly higher than that in WMS (474.04 ± 10.86 pg/ml vs. 334.50 ± 2 9.09 pg/ml, respectively, P = 0.000).
Depression group
Compared to NCS, there was a significant increase in WMS and TCMS of serum 5-HT (194.69 ± 5.09 pg/ml vs. 326.21 ± 39.98 pg/ml and 456.33 ± 23.12 pg/ml, respectively, both P = 0.000). 5-HT concentration in the serum of TCMS was significantly higher than that in WMS (456.33 ± 23.12 pg/ml vs. 326.21 ± 39.98 pg/ml, respectively, P = 0.000).
Myocardial infarction + depression group
Compared to NCS, there was a significant increase in WMS and TCMS of serum 5-HT (182.50 ± 10.23 pg/ml vs. 372.55 ± 52.23 pg/ml and 441.76 ± 23.38 pg/ml, respectively, both P = 0.000). 5-HT concentration in the serum of TCMS was significantly higher than that in WMS [441.76 ± 23.38 pg/ml vs. 372.55 ± 52.23 pg/ml, respectively, P = 0.004; Figure 1].
Figure 1.
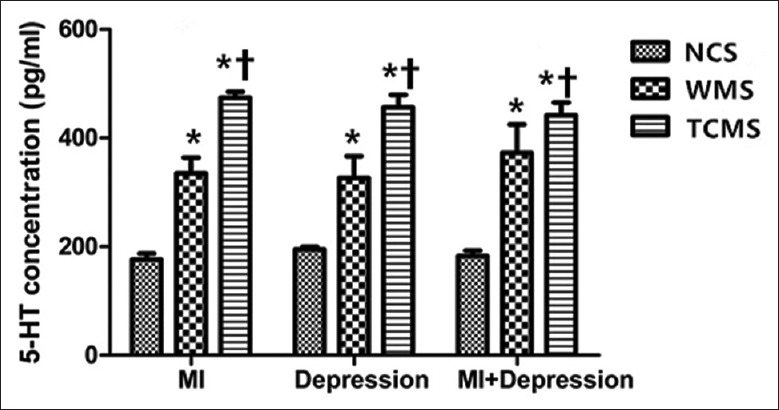
Serum 5-HT comparison in different subgroups (n = 10). *P < 0.05, compared with NCS. †P < 0.05, compared with WMS. 5-HT: 5-hydroxytryptamine; NCS: Negative control subgroup; WMS: Western medicine subgroup; TCMS: Traditional Chinese medicine subgroup; MI: Myocardial infarction; MI + depression: Myocardial infarction combined with depression.
5-hydroxytryptamine level in platelets
Myocardial infarction group
Compared to NCS, there was a significant increase in WMS and TCMS of platelet 5-HT (129.74 ± 27.17 pg/ml vs. 322.24 ± 11.60 pg/ml and 340.45 ± 17.99 pg/ml, respectively, both P = 0.000). 5-HT concentration in the platelets of TCMS was insignificantly higher than that in WMS (340.45 ± 17.99 pg/ml vs. 322.24 ± 11.60 pg/ml, respectively, P = 0.098).
Depression group
Compared to NCS, there was a significant increase in WMS and TCMS of platelet 5-HT (175.15 ± 4.07 pg/ml vs. 204.56 ± 18.59 pg/ml, and 252.03 ± 22.26 pg/ml, respectively, P = 0.004 and P = 0.000, respectively). 5-HT concentration in the platelets of TCMS was significantly higher than that in WMS (252.03 ± 22.26 vs. 204.56 ± 18.59 pg/ml, respectively, P = 0.000).
Myocardial infarction + depression group
Compared to NCS, there was a significant increase in WMS and TCMS of platelet 5-HT (180.83 ± 11.08 vs. 221.12 ± 22.23 pg/ml and 265.37 ± 29.49 pg/ml, respectively, P = 0.011 and P = 0.000, respectively). 5-HT concentration in the platelets of TCMS was significantly higher than that in WMS [265.37 ± 29.49 vs. 221.12 ± 22.23 pg/ml, respectively, P = 0.005; Figure 2].
Figure 2.
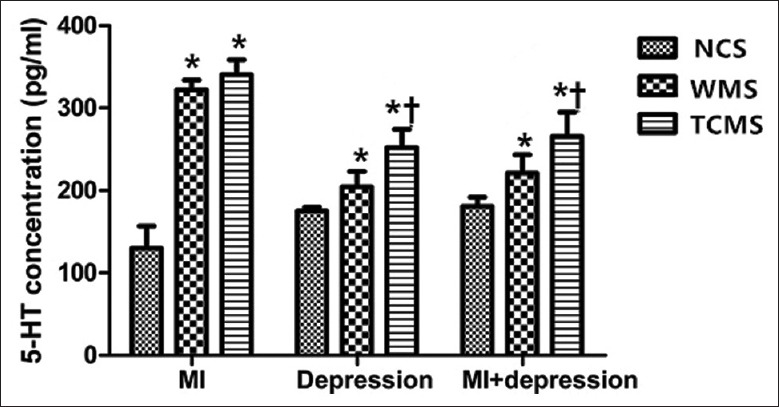
Platelet 5-HT comparison in different subgroups (n = 10). *P < 0.05, compared with NCS. †P < 0.05, compared with WMS. 5-HT: 5-hydroxytryptamine; NCS: Negative control subgroup; WMS: Western medicine subgroup; TCMS: Traditional Chinese medicine subgroup; MI: Myocardial infarction; MI + depression: Myocardial infarction combined with depression.
5-hydroxytryptamine 2A receptor level in platelet
Myocardial infarction group
Compared to NCS, there was a significant increase in WMS and TCMS of 5-HT2AR concentration (197.49 ± 11.60 vs. 345.07 ± 25.85 pg/ml and 255.25 ± 34.18 pg/ml, respectively, P = 0.000 and P = 0.001). Platelet 5-HT2AR concentration in TCMS was significantly lower than that in WMS significantly (255.25 ± 34.18 vs. 345.07 ± 25.85 pg/ml, respectively, P = 0.000).
Depression group
Compared to NCS, there was a significant increase in WMS and TCMS of 5-HT2AR concentration (193.15 ± 17.88 vs. 243.89 ± 12.73 and 291.14 ± 12.07 pg/ml, respectively, both P = 0.000). Platelet 5-HT2AR concentration in TCMS was significantly higher than that in WMS (291.14 ± 12.07 vs. 243.89 ± 12.73 pg/ml, respectively, P = 0.000).
Myocardial infarction + depression group
Compared to NCS, there was an insignificant increase in WMS of 5-HT2AR concentration (205.84 ± 15.19 vs. 230.64 ± 13.33 pg/ml, P = 0.181) and a significant increase in TCMS of 5-HT2AR concentration (205.84 ± 15.19 vs. 281.07 ± 48.99 pg/ml, P = 0.001). Platelet 5-HT2AR concentration in TCMS was significantly higher than that in WMS [281.07 ± 48.99 vs. 230.64 ± 13.33 pg/ml, P = 0.012; Figure 3].
Figure 3.
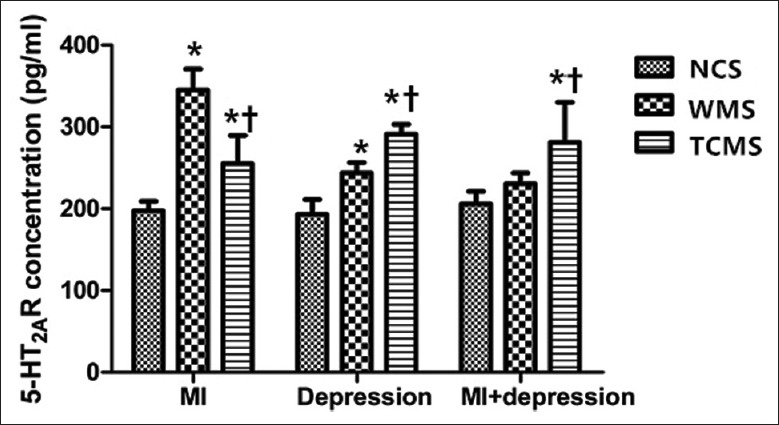
Platelet 5-HT2A receptor comparison in different subgroups (n = 10). *P < 0.05, compared with NCS. †P < 0.05, compared with WMS. 5-HT: 5-hydroxytryptamine; NCS: Negative control subgroup; WMS: Western medicine subgroup; TCMS: Traditional Chinese medicine subgroup; MI: Myocardial infarction; MI + depression: Myocardial infarction combined with depression.
Serotonin transporter level in platelet
Myocardial infarction group
Compared to NCS, there was a significant decrease in WMS and TCMS of platelet SERT (322.84 ± 36.39 pg/ml vs. 227.91 ± 12.67 pg/ml and 214.81 ± 18.29 pg/ml, respectively, P = 0.000). Platelet SERT concentration in TCMS was insignificantly lower than that in WMS (214.81 ± 18.29 pg/ml vs. 227.91 ± 12.67 pg/ml, P = 0.295).
Depression group
Compared to NCS, there was a significant decrease in WMS and TCMS of platelet SERT (278.21 ± 19.71 pg/ml vs. 182.82 ± 9.96 pg/ml and 127.67 ± 8.07 pg/ml, respectively, P = 0.000). The platelet SERT concentration in TCMS was significantly lower than that in WMS (127.67 ± 8.07 pg/ml vs. 182.82 ± 9.96 pg/ml, P = 0.000).
Myocardial infarction + depression group
Compared to NCS, there was a significant decrease in WMS and TCMS of platelet SERT (281.82 ± 22.21 pg/ml vs. 179.86 ± 5.38 pg/ml and 180.20 ± 6.74 pg/ml, respectively, both P = 0.000). The platelet SERT concentration in TCMS was insignificantly higher than that in WMS [180.20 ± 6.74 pg/ml vs. 179.86 ± 5.38 pg/ml, P = 0.966; Figure 4].
Figure 4.
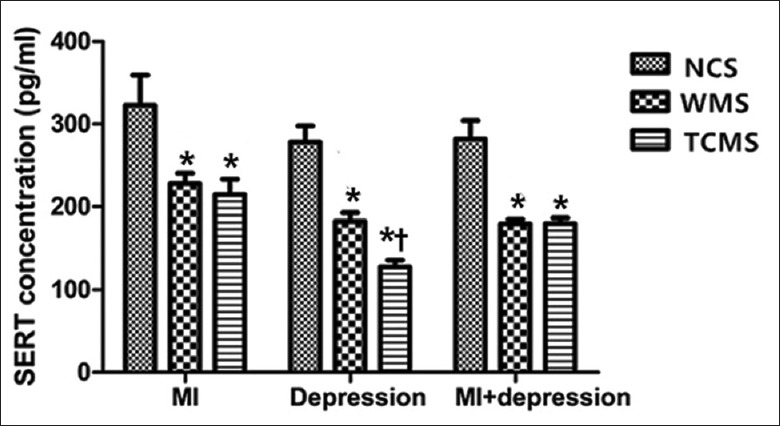
Platelet serotonin transporter comparison in different subgroups (n = 10). *P < 0.05, compared with NCS. †P < 0.05, compared with WMS. 5-HT: 5-hydroxytryptamine; NCS: Negative control subgroup; WMS: Western medicine subgroup; TCMS: Traditional Chinese medicine subgroup; MI: Myocardial infarction; MI + depression: Myocardial infarction combined with depression.
DISCUSSION
In the recent years, the elevated comorbidity rates between cardiovascular disease and depression have occasioned several investigations on the link between them.[17,18] Our previous studies[19,20] showed that 5-HT-enhanced platelet activation emerged from this work as a leading candidate explanation of the elevated cardiac risk that attended a diagnosis of major depression.
Since its discovery and isolation from beef serum almost 50 years ago, 5-HT has been determined to function as both vasoactive substance (hence its common name, serotonin) and neurotransmitter. Over 95% of 5-HT is synthesized in the enterochromaffin cells of the intestine; other synthetic sites include the raphe nuclei of the brain and the neuroendothelial cells that line the lung.[21] In the peripheral circulation, 99% of 5-HT is stored in platelets.[22] When this 5-HT is excreted excessively, it is known that platelet activity and aggregation are enhanced and promote clotting and coronary vasoconstriction. However, the precise mechanisms by which 5-HT modulates the function of the cardiac and central nervous systems are still under debate. In the meantime, there is consensus that 5-HT receptors and transporters play a critical role in the regulation of 5-HT concentration and function. Thus, given the light that platelet-based 5-HT regulation may shed on its counterpart in the central nervous system, our study focused on 5-HT system modulation in serum and platelets.
The 5-HT2AR figures in this modulation. 5-HT2AR is a G-protein coupled receptor found both on the plasma membrane and intracellularly. Binding with 5-HT of this receptor activates a series of biochemical responses that result in the release of cytoplasmic 5-HT, and ultimately, platelet aggregation.[23] By itself, 5-HT is a relatively weak agonist of platelet aggregation, but it can powerfully reinforce aggregation in the presence, of other agonists, such as thrombin, adrenaline, adenosine diphosphate, or collagen, even at low concentrations.[24] A study by Kim et al.[25] shed light on the relevance of 5-HT2AR to the aggregatory function of 5-HT: lower concentrations of extracellular serotonin were found to bind with 5-HT2AR and lead to increased platelet activation that was strongly associated with the onset of CHD. By contrast, when platelets were stimulated with higher concentrations of 5-HT, there was a significant decrease in platelet activation following the attainment of the peak level of 5-HT concentration.[25] Moreover, it has been shown that these effects can be inhibited by 5-HT2AR blockers such as ketanserin, which suppresses 5-HT release and protects the heart against ischemia.[26,27,28] Since elevations of platelet 5-HT2AR have been found in depressed patients, these studies suggest that 5-HT2AR may constitute the pathophysiological cause of co-occurring MI and depression.
Studies by other investigators have suggested that 5-HT2AR was not relevant to the efficacy of antidepressant drugs. For example, it has been reported by Hrdina et al.[29] that, since its concentration did not change following treatment with SSRIs, 5-HT2AR could not be responsible for the curative effects of these drugs. Another study, conducted by the same investigator with a collaborator, found an elevation in brain 5-HT following 3 weeks of treatment with fluoxetine; therefore, it was theorized that 5-HT elevations might account for antidepressant efficacy.[30] In this study, however, an increase in platelet 5-HT2AR was found to follow an increase in 5-HT. Some mechanisms that may account for this elevation are as follows: (1) the increase of 5-HT stimulated the upregulation in 5-HT2AR necessary to bind 5-HT and increase activation, but not sufficient to induce aggregation or (2) when 5-HT2AR became saturated with 5-HT, the left amount of 5-HT2AR available for further binding stimulated 5-HT2AR upregulation. In either case, our results suggested that 5-HT treatment course and dosage may influence 5-HT2AR levels, which should be considered in the study design.
The 5-HT transporter (SERT) may also be relevant to antidepressant drug efficacy. SERT is a transmembrane protein responsible solely for the transport of 5-HT across the plasma membrane. By varying the conformation of its binding sites, SERT can exert homeostatic control on the intra- and extra-cellular concentrations of 5-HT, by controlling its rate of uptake.[24] A study by Brenner et al.[31] confirmed it by showing that variation in SERT-binding sites was highly relevant to the extracellular concentration of 5-HT. In that study, a moderate increase in extracellular 5-HT led to a 35% increase in SERT density on the platelet membrane and 32% increase in SERT reuptake rate to facilitate 5-HT transport. A more dramatic increase in extracellular 5-HT, however, caused decreasing SERT density on the plasma membrane and a decreasing rate of reuptake. Although these findings contribute to the understanding of the relationship between 5-HT and SERT, the mechanism of this relationship remains unknown.
SSRIs can be employed in the treatment of depressed patients who cannot tolerate other antidepressant drugs. These drugs act by potently inhibiting the reuptake of 5-HT through the inhibition of the transport function of SERT; their effects on other receptors and transporters are weak. Demonstrated by the SADHART trial described above, sertraline is relatively safe and efficacious in depressed patients with ischemic heart disease.[10] It has also been demonstrated in our study that SSRIs have generally reduced the morbidity and mortality of depression with comorbid heart disease: pretreatment with sertraline resulted in an elevation of 5-HT in serum and platelets, presumably by inhibiting SERT, and therefore lead to a better treatment of MI with comorbid depression.
XinLingWan has long been employed clinically for psychocardiological treatment. Nevertheless, there is insufficient pharmacological data available to describe its mechanism of action. This insufficiency has significantly limited the development of XinLingWan as a recognized treatment. Thus, one of the goals of our study was to contribute to supplying the mechanistic data that were needed to develop this treatment. Before our study, it was understood that most of the components of XinLingWan, such as toad venom, ginseng, and P. notoginseng, were beneficial to cardiovascular regulation, serving as anti-ischemic and anti-anoxic agents by increasing blood flow. Our study, by analogy with 5-HT, contributed mechanistic detail to the knowledge of these effects; our results suggest that one of the XingLingWan's pharmacological functions involves the regulation of 5-HT, 5-HT2AR, and SERT.
Thus, as it may now be said to function similarly to sertraline, one effect of our results may be to bring interest in the psychocardiological efficacy of a famous Chinese remedy, XinLingWan, to a broader audience.
However, there are still some limitations in this study. First, we just focused on 5-HT in periphery, not in the brain. As 5-HT is a kind of neurotransmitter, it is necessary for us to explore the relationship between periphery 5-HT and central 5-HT. Second, for the complex components of XinLingWan, it is a big challenge for us to find the main substance which plays the most important role, that is what we will explore in our further study.
Financial support and sponsorship
The study was supported by a grant from the China International Medical Foundation (No. 201603).
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Many thanks to Prof. Ying-Bin Ge for his efforts in the animal experiment and Christopher R. Stone for his work in language revision.
Footnotes
Edited by: Ning-Ning Wang
REFERENCES
- 1.Liu MY, Lu L, Geng QS. Psycho-Cardiology. 1st ed. China: People's Medical Publishing House Co., Ltd; 2016. pp. 52–6. [Google Scholar]
- 2.Sanner JE, Frazier L, Udtha M. Effects of delayed laboratory processing on platelet serotonin levels. Biol Res Nurs. 2013;15:13–6. doi: 10.1177/1099800411416636. doi: 10.1177/1099800411416636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shively CA, Silverstein-Metzler M, Justice J, Willard SL. The impact of treatment with selective serotonin reuptake inhibitors on primate cardiovascular disease, behavior, and neuroanatomy. Neurosci Biobehav Rev. 2017;74:433–43. doi: 10.1016/j.neubiorev.2016.08.037. doi: 10.1016/j.neubiorev.2016.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Williams MS. Platelets and depression in cardiovascular disease: A brief review of the current literature. World J Psychiatry. 2012;2:114–23. doi: 10.5498/wjp.v2.i6.114. doi: 10.5498/wjp.v2.i6.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benyamini Y, Roziner I, Goldbourt U, Drory Y, Gerber Y, et al. Israel Study Group on First Acute Myocardial Infarction. Depression and anxiety following myocardial infarction and their inverse associations with future health behaviors and quality of life. Ann Behav Med. 2013;46:310–21. doi: 10.1007/s12160-013-9509-3. doi: 10.1007/s12160-013-9509-3. [DOI] [PubMed] [Google Scholar]
- 6.Wulsin LR, Musselman D, Otte C, Bruce E, Ali S, Whooley MA, et al. Depression and whole blood serotonin in patients with coronary heart disease from the heart and soul study. Psychosom Med. 2009;71:260–5. doi: 10.1097/PSY.0b013e31819cc761. doi: 10.1097/PSY.0b013e31819cc761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benedetti S, Bucciarelli S, Canestrari F, Cocchi M. Platelet's fatty acids and differential diagnosis of major depression and bipolar disorder through the use of an unsupervised competitive-learning network algorithm (SOM) Open J Depress. 2014;3:52–73. doi: 10.4236/ojd.2014.32011. [Google Scholar]
- 8.Meltzer HY. Role of serotonin in depression. Ann N Y Acad Sci. 2010;600:486–99. doi: 10.1111/j.1749-6632.1990.tb16904.x. doi: 10.1111/j.1749-6632.1990.tb16904.x. [DOI] [PubMed] [Google Scholar]
- 9.Steca P, Greco A, D’Addario M, Parati G. Relationship of illness severity with health and life satisfaction in patients with cardiovascular disease: The mediating role of self-efficacy beliefs and illness perceptions. J Happiness Stud. 2013;14:1585–99. doi: 10.1007/s10902-012-9397-4. [Google Scholar]
- 10.Serebruany VL, Glassman AH, Malinin AI, Nemeroff CB, Musselman DL, van Zyl LT, et al. Platelet/endothelial biomarkers in depressed patients treated with the selective serotonin reuptake inhibitor sertraline after acute coronary events: The sertraline anti Depressant heart attack randomized trial (SADHART) platelet substudy. Circulation. 2003;108:939–44. doi: 10.1161/01.CIR.0000085163.21752.0A. doi: 10.1161/01.CIR.0000085163.21752.0A. [DOI] [PubMed] [Google Scholar]
- 11.Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: The enhancing recovery in coronary heart disease patients (ENRICHD) randomized trial. JAMA. 2003;289:3106–16. doi: 10.1001/jama.289.23.3106. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- 12.Turner MS, May DB, Arthur RR, Xiong GL. Clinical impact of selective serotonin reuptake inhibitors therapy with bleeding risks. J Intern Med. 2007;261:205–13. doi: 10.1111/j.1365-2796.2006.01720.x. doi: 10.1111/j.1365-2796.2006.01720.x. [DOI] [PubMed] [Google Scholar]
- 13.Akbay E, Onur MA. A new modified myocardial infarction animal model. J Cardiovasc Surg. 2013;1:69–71. doi: 10.5455/jcvs.2013137. [Google Scholar]
- 14.Porsolt RD, Anton G, Blavet N, Jalfre M. Behavioural despair in rats: A new model sensitive to antidepressant treatments. Eur J Pharmacol. 1978;47:379–91. doi: 10.1016/0014-2999(78)90118-8. doi: 10.1016/0014-2999(78)90118-8. [DOI] [PubMed] [Google Scholar]
- 15.Hascoët M, Bourin M. The forced swimming test in mice: A suitable model to study antidepressants. Humana Press. 2009;42:85–118. doi: 10.1007/978-1-60761-303-9_6. [Google Scholar]
- 16.Immuno-Biological Laboratories. Instructions for Use: Serotonin ELISA. IB89546[DB/OL] [Last accessed on 2016 Jan 08]. Available from: http://www.iblamerica.com/pdf/elisa/IB89546.pdf .
- 17.Colquhoun DM, Bunker SJ, Clarke DM, Glozier N, Hare DL, Hickie IB, et al. Screening, referral and treatment for depression in patients with coronary heart disease. Med J Aust. 2013;198:483–4. doi: 10.5694/mja13.10153. doi: 10.5694/mja13.10153. [DOI] [PubMed] [Google Scholar]
- 18.Sanner JE, Frazier L. The role of serotonin in depression and clotting in the coronary artery disease population. J Cardiovasc Nurs. 2011;26:423–9. doi: 10.1097/JCN.0b013e3182076a81. doi: 10.1097/JCN.0b013e3182076a81. [DOI] [PubMed] [Google Scholar]
- 19.He DF, Ren YP, Liu MY. Effects of ginseng fruit saponins on serotonin system in Sprague-Dawley rats with myocardial infarction, depression, and myocardial infarction complicated with depression. Chin Med J. 2016;129:2913–919. doi: 10.4103/0366-6999.195462. doi: 10.4103/0366-6999.195462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu MY, Ren YP, Zhang LJ, Ding JY. Pretreatment with ginseng fruit saponins affects serotonin expression in an experimental comorbidity model of myocardial infarction and depression. Aging Dis. 2016;7:680–86. doi: 10.14336/AD.2016.0729. doi: 10.14336/AD.2016.0729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patrick Davis R, Linder AE, Watts SW. Lack of the serotonin transporter (SERT) reduces the ability of 5-hydroxytryptamine to lower blood pressure. Naunyn Schmiedebergs Arch Pharmacol. 2011;383:543–6. doi: 10.1007/s00210-011-0622-1. doi: 10.1007/s00210-011-0622-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reikvam AG, Hustad S, Reikvam H, Apelseth TO, Nepstad I, Hervig TA, et al. The effects of selective serotonin reuptake inhibitors on platelet function in whole blood and platelet concentrates. Platelets. 2012;23:299–308. doi: 10.3109/09537104.2011.618852. doi: 10.3109/09537104.2011.618852. [DOI] [PubMed] [Google Scholar]
- 23.Shimizu Y, Minatoguchi S, Hashimoto K, Uno Y, Arai M, Wang N, et al. The role of serotonin in ischemic cellular damage and the infarct size-reducing effect of sarpogrelate, A 5-hydroxytryptamine-2 receptor blocker, in rabbit hearts. J Am Coll Cardiol. 2002;40:1347–55. doi: 10.1016/s0735-1097(02)02158-7. doi: 10.1016/S0735-1097(02)02158-7. [DOI] [PubMed] [Google Scholar]
- 24.Li Q. Cellular and molecular alterations in mice with deficient and reduced serotonin transporters. Mol Neurobiol. 2006;34:51–66. doi: 10.1385/mn:34:1:51. doi: 10.1385/MN:34:1:51. [DOI] [PubMed] [Google Scholar]
- 25.Kim DA, McClure WG, 3rd, Neighoff JB, Vaidya D, Williams MS. Platelet response to serotonin in patients with stable coronary heart disease. Am J Cardiol. 2014;114:181–6. doi: 10.1016/j.amjcard.2014.04.023. doi: 10.1016/j.amjcard.2014.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goyal RK, Umrani DN, Bodiwala DN, Dhalla NS. Usefulness of 5-Ht 2a, receptor antagonists for the treatment of cardiovascular complications in diabetes. Atherosclerosis, hypertension and diabetes. Springer US. 2003;8:317–26. doi: 10.1007/978-1-4419-9232-1_25. [Google Scholar]
- 27.Mercado CP, Kilic F. Molecular mechanisms of SERT in platelets: Regulation of plasma serotonin levels. Mol Interv. 2010;10:231–41. doi: 10.1124/mi.10.4.6. doi:10.1124/mi.10.4.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li X, Fan Y, Xiao S, Peng S, Dong X, Zheng X, et al. Decreased platelet 5-hydroxytryptamin (5-HT) levels: A response to antidepressants. J Affect Disord. 2015;187:84–90. doi: 10.1016/j.jad.2015.08.025. doi:10.1016/j.jad.2015.08.025. [DOI] [PubMed] [Google Scholar]
- 29.Hrdina PD, Bakish D, Ravindran A, Chudzik J, Cavazzoni P, Lapierre YD. Platelet serotonergic indices in major depression: Up-regulation of 5-HT 2A, receptors unchanged by antidepressant treatment. Psychiatry Res. 1997;66:73–85. doi: 10.1016/s0165-1781(96)03046-6. doi: 10.1016/S0165-1781(96)03046-6. [DOI] [PubMed] [Google Scholar]
- 30.Hrdina PD, Vu TB. Chronic fluoxetine treatment upregulates 5-HT uptake sites and 5-HT2 receptors in rat brain: An autoradiographic study. Synapse. 1993;14:324–31. doi: 10.1002/syn.890140410. doi: 10.1002/syn.890140410. [DOI] [PubMed] [Google Scholar]
- 31.Brenner B, Harney JT, Ahmed BA, Jeffus BC, Unal R, Mehta JL, et al. Plasma serotonin levels and the platelet serotonin transporter. J Neurochem. 2007;102:206–15. doi: 10.1111/j.1471-4159.2007.04542.x. doi: 10.1111/j.1471-4159.2007.04542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


