Abstract
Objective
Chronic pain is reported by 15–25% of children. Growing evidence from clinical samples suggests that complementary and alternative medicine (CAM) therapies are desired by families and may benefit some children with pain conditions. The objective of this study is to provide estimates of CAM use by children with pain in the United States.
Methods
We analyzed data from the 2012 National Health Interview Survey (NHIS) to estimate patterns, predictors, and perceived benefits of CAM use among children 4–17 years of age with and without painful conditions in the US. We used χ2 tests to compare the prevalence rates of CAM use among children with pain to CAM use among children without pain. Multivariable logistic regression was used to examine factors associated with CAM use within the group of children with pain conditions.
Results
Parents reported that 26.6% of children had pain conditions (e.g. headache, abdominal, musculoskeletal pain) in the past year; of these children, 21.3% used CAM. In contrast only 8.1% of children without pain conditions used CAM (χ2: p<.001). CAM use among children with pain was associated with female sex (adjusted odds ratio (aOR)=1.49, p=0.005), higher income (aOR=1.61, p=0.027), and presence of 4+ comorbidities (aOR=2.01, p=0.013). Among children with pain who used CAM the 2 most commonly used CAM modalities were biologically-based therapies (47.3%) (e.g., special diets and herbal supplements) and manipulative or body-based therapies (46.3%) (e.g., chiropractic and massage).
Conclusions
CAM is frequently used by children with pain in the USA and many parents report benefits for their child’s symptoms.
Keywords: Complementary and alternative medicine, integrative medicine, pain
Introduction
Pediatric pain is a significant public health concern. Pain affects 15–25% of children in the United States, and economic expenditures on pediatric pain are estimated at around $11.5 billion annually.1, 2 Evidence suggest that complementary and alternative medicine (CAM) therapies may be effective for treating pain3, 4. However the prevalence, patterns, and perceived benefits of CAM use by children with pain in the United States are unknown.
The 2007 National Health Interview Survey estimated that approximately 11.8% of children in the United States use CAM for treating a variety of symptoms and health conditions, including back or neck pain (6.7%) and other musculoskeletal problems (4.2%).5 Hospital pediatric pain management programs often offer one or more CAM approaches for patients,6 and many pediatric providers discuss or recommend a CAM approach to their patients.7 Thus far, two studies have explored the use of CAM and attitudes towards CAM in multidisciplinary pediatric pain clinics: Vinson and colleagues found that a significant portion of their patients (42%) had previously tried a CAM modality prior to attending pain clinic,3 while in a sample of children presenting to pain clinic for initial assessment, the majority of patients (61.2%) elected to include a CAM approach as part of their treatment plan.4
While these studies provide estimates of CAM utilization in clinical samples of children with pain, no large nationally representative studies have yet been published on CAM use by children with pain in the United States. This is a major gap in knowledge because a better understanding of patterns, predictors, and perceived benefits of CAM use may allow clinicians and healthcare policymakers to understand the demand for these modalities and to more widely incorporate CAM within conventional treatment approaches.
Therefore, the primary of this study was to compare prevalence rates of CAM use among children with pain conditions to children without pain conditions in the United States. Our primary hypothesis was that rates of CAM use would be higher in children with pain conditions as compared to children without pain conditions. The secondary aims of this study were to determine, among children with pain: which CAM therapies were used most often; which factors were associated with CAM use; and perceived benefits of and reasons associated with CAM use. We hypothesized that among children with pain, CAM use would be associated with higher income, private health insurance, and female sex. Furthermore we expected to find that children with pain would report benefit from using CAM.
Methods
Participants and Procedure
For this cross-sectional analysis we used data from the 2012 National Health Interview Surveys (NHIS). The NHIS are an annually conducted set of cross sectional surveys intended to provide nationally-representative data on the health and health care utilization of the civilian, non-institutionalized child and adult population in the United States. NHIS uses a complex, multistage sample design with oversampling of minorities. By applying survey weights, estimates are representative of the United States population. The 2012 version of the NHIS was accompanied by a child complementary and alternative supplement (NHIS-CAM). This supplement is not available with later years of NHIS. Funding for NHIS-CAM was provided by the National Center for Complementary and Integrative Health (NCCIH) of the National Institutes of Health. Data collection and management for NHIS-CAM was conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention. NHIS-CAM was designed to collect information on 34 CAM health services, products, and practices commonly used in the United States. Further information about NHIS and NHIS-CAM is available online.8 The 2012 NHIS-CAM contained data on 10,281 children 4–17 years of age (parents of children 0–3 years of age were not asked about CAM use). We extracted variables related to CAM use, pain-related conditions, and sociodemographic background information. Because all data are publically available, this study was deemed exempt from review by the Institutional Review Board at Seattle Children’s Hospital.
Measures
Complementary and alternative medicine use
The 2012 NHIS-CAM asked parents whether their child used or saw a provider for the following CAM therapies over the preceding 12 months: acupuncture, Ayurveda, biofeedback, chelation therapy, chiropractic and osteopathic manipulation, craniosacral therapy, special diets (Atkins, macrobiotic, Pritkin, Ornish, vegan/vegetarian), energy therapy, herbal or non-vitamin supplements, homeopathic medicine, hypnosis, massage therapy, naturopathy, movement or exercise techniques (Alexander technique, Feldenkrais, Pilates, Trager psychophysical integration), guided imagery, homeopathy, meditation (mantra, mindfulness, spiritual), progressive relaxation, qi gong, tai chi, traditional healers, and yoga. In addition to these CAM therapies NHIS-CAM also includes data on vitamins and minerals; however for this study we excluded data on vitamins and minerals due to lack of specificity about use among children and adolescents. The 2012 NHIS-CAM did not ask about prayer. To ease interpretability and to maintain large enough sample sizes for comparative analyses, we categorized CAM modalities into four groups as employed by the National Center for Complementary and Integrative Health NCCIH)5: 1) alternative medical systems/energy healing therapies (acupuncture, Ayurveda, homeopathic medicine, naturopathy, traditional healers, energy healing therapy); 2) biologically-based therapies (chelation therapy, herbal or non-vitamin supplements, special diets); 3) manipulative and body-based therapies (chiropractic and osteopathic manipulation, massage therapy, craniosacral therapy, movement or exercise techniques); and 4) mind-body therapies (biofeedback, hypnosis, meditation, guided imagery, progressive relaxation, yoga, tai chi, qi gong).5 Parents were asked to name the top 3 CAM modalities used by their children and to state whether these were used to treat specific health conditions or symptoms. The National Center for Health Statistics have previously analyzed data from the 2012 NHIS- CAM and found that the most common indications for CAM in children included: back or neck pain (8.8%, head or chest cold (6.5%), other musculoskeletal problems (5%), anxiety or stress (4.4%), attention deficit and hyperactivity disorder (ADHD) (2.3%), and insomnia (2%)9.
Reasons and perceived benefits associated with CAM use
For each of the 3 top CAM modalities, parents were also asked about the perceived benefits and reasons for CAM use. The specific perceived benefits and reasons for CAM use are listed in figures 1 and 2 respectively. For each of these variables, parents were asked to respond “Yes” or “No”.
Figure 1.
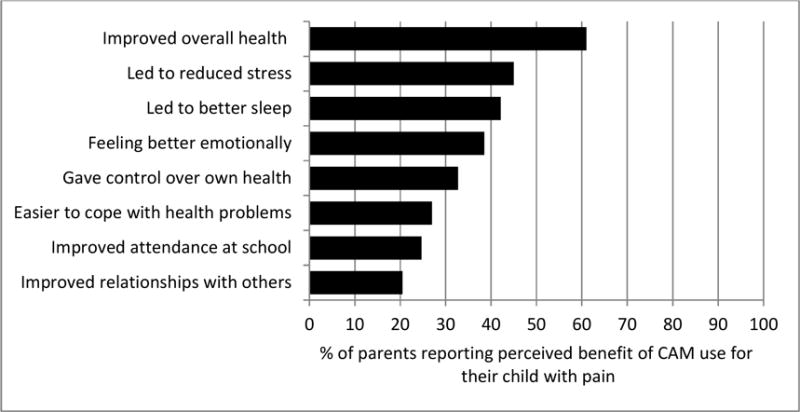
Perceived benefits from CAM use reported by parents of children with pain. This figure presents the percentage of the top 3 CAM modalities used by children with pain and the perceived benefits reported by parents (n=565).
Figure 2.
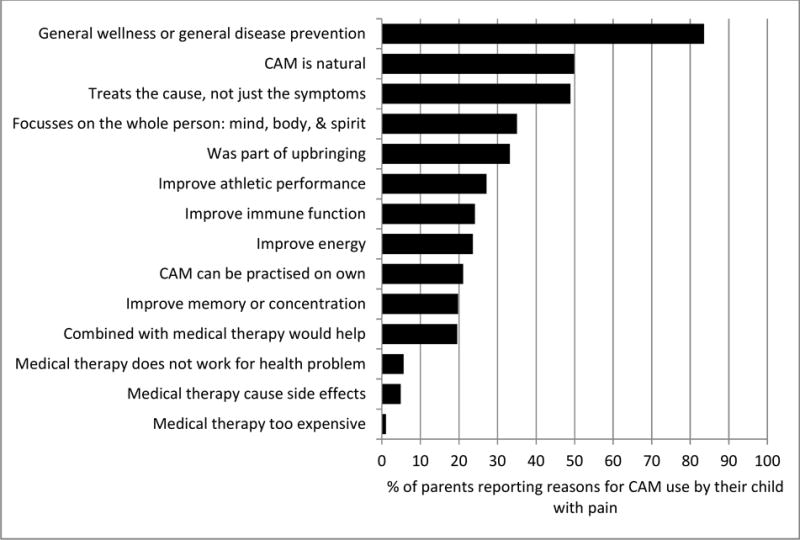
Reasons reported for CAM use by children with pain. This figure shows the percent of the top 3 CAM modalities used to address painful conditions that were used for the reasons given (n=565).
Participants with pain conditions
Children and adolescents with pain conditions were identified by parental responses to questions in the 2012 NHIS Sample Child file1. Parents were asked whether their child had any of the following pain conditions in the last 12 months: 1) frequent headaches or migraines; 2) recurrent headaches other than migraines; 3) abdominal pain; 4) pain in/around a joint over the past 30 days; 5) neck pain; 6) lower back pain; 7) other muscle or bone pain; 8) severe sprains or strains; 9) dental pain; or 10) other chronic pain. These pain conditions have previously been used in publications of data from NHIS1. While parents did not report on the duration of pain in their children, these 10 pain conditions were specified as chronic conditions in NHIS. We also identified a subgroup of children who did not endorse one of the 10 painful conditions but still reported specifically using CAM to treat one of the 10 mentioned pain conditions. For analyses, this subgroup of children (n = 39) was also coded as having a pain condition during the previous 12 months.
Sociodemographic and health status variables
We used the Andersen Behavioral Model of Health Service Use to specify covariates for inclusion in our regression analyses.10 The Andersen model has been extensively used in studies investigating health service use, including estimating national healthcare use and costs for children and adults with pain related conditions.1,11 According to this model, health service use is determined by three sets of factors: predisposing characteristics, enabling resources, and need factors. Predisposing factors include social and demographic characteristics that influence a person’s health services use. We included age group (4–6, 7–11, 12–17 years), gender, and race/ethnicity (white non-Hispanic, black non-Hispanic, Hispanic, other) to represent predisposing factors. Enabling resources are those that facilitate or impede healthcare use. We included insurance status, income, United States census region, and whether the study participant had a usual source of health care to represent enabling resources. Need factors refer to comorbid health conditions influencing the actual or perceived need for children’s health care. The National Health Interview Survey asks about several health conditions in children including: depression, anxiety, asthma, ADHD, allergies, infections, autism, muscular dystrophy, diabetes mellitus, neurodevelopmental delay, Down’s syndrome, cystic fibrosis, seizures, and hypertension. We decided a priori to control for comorbid conditions by assigning participants to one of four categories representing number of comorbidities (0, 1, 2–3, and 4 or more comorbid conditions).
Statistical analysis
All analyses were conducted with Stata version 12.1;12 α level was set at .05. We adjusted for the complex probability survey design of NHIS using sampling weights, stratification, and clustering to provide nationally-representative estimates of the USA childhood population. To address aim 1, we used χ2 tests to compare the prevalence rates of CAM use among children with pain to CAM use among children without pain. We also performed multivariate logistic regression analysis to determine the odds ratio of using CAM between children with pain as compared to children without pain. In multivariate logistic regression analysis we controlled for predisposing, enabling, and need factors as specified by the Andersen model. To address aim 2, we calculated frequencies of use of the four types of CAM approaches among children with pain. To address aim 3, we performed multivariate logistic regression to examine factors associated with CAM use within the group of children with pain conditions. Control variables in this multivariate regression analysis included the predisposing, enabling, and need factors as specified by the Anderson model. In addition, we also controlled for additional need factors: sleep disturbances, perceived stress, and fatigue, that are common symptom complaints in children with pain conditions and may be independently associated with CAM use. Finally, to address aim 4, we provide descriptive information (percentages) concerning how beneficial parents felt the CAM approaches were for their children. NHIS contains <1% missing data and we therefore did not adjust for missing data.
Results
Sample characteristics
We included data on all 10,218 children 4–17 years of age participating in the 2012 NHIS-CAM. After applying complex survey weights, these 10,218 participants represented 57.8 million children in the USA, which is consistent with estimates of the child and adolescent population in the USA in 2012 according to the US Census Bureau.13 The mean age of children in the sample was 10.5 years. Our sample contained a slight preponderance of males (51.1%) and most participants were white, non-Hispanic (53.7%), which is also consistent with findings from the US Census Bureau. In the overall sample, parents reported that 11.6% (representing 6.7 million) of surveyed children used CAM in the previous year.
Of the total sample, 2,795 children (26.6%), weighted to represent 15.4 million children nationwide, were reported by parents to have at least one pain-related condition in the past 12 months. Pain conditions reported included (in order of prevalence): dental pain (8.4%); abdominal pain (7.9%); recurring headaches other than migraines (7.3%); other muscle or bone pain (6.7%); frequent headaches or migraines (6.4%); joint pain (6.3%); severe sprains or strains (4.9%); lower back pain (4.7%); neck pain (3.3%); and other chronic pain (0.9%). There was significant overlap among pain conditions, 54.5% of children with pain had one pain condition, 34.5% had 2–3 pain conditions, while the remaining 11% had 4 or more pain conditions.
Sociodemographic and clinical characteristics of participants revealed several statistically significant differences between children with pain conditions as compared to children without pain (see Table 1). Pain was more common in youth who were older, female, white, non-Hispanic, and in those whose parents had higher education levels. Youth from the Northeast United States reported less pain than those from other regions. There were also significant differences between groups regarding number of comorbidities in that children with pain had more comorbid conditions (for example asthma, attention deficit and hyperactivity disorder) as compared to children without pain. There were no differences in income or insurance status between children with and without pain.
Table 1.
Sociodemographic and clinical characteristics of children 4–17 years of age with pain conditions as compared to children without pain conditions in the United States. Datasource: 2012 National Health Interview Survey.
| Total sample (n=10,218) Weighted % | Pain Condition
|
|||
|---|---|---|---|---|
| Yes (n=2,795) Weighted % | No (n=7,423) Weighted % | χ2 p-value | ||
| Estimated US population | 57,829,791 | 15,399,414 | 42,430,377 | |
| Estimated proportion | 100 | 26.6 | 73.4 | |
| CAM used last 12 months (excluding all vitamins and minerals) | <.0001 | |||
| Yes | 11.6 | 21.3 | 8.1 | |
| No | 88.4 | 78.7 | 91.9 | |
| Age | <.0001 | |||
| 4–6 | 20.8 | 5.0 | 26.5 | |
| 7–11 | 36.3 | 35.8 | 36.5 | |
| 12–17 | 42.9 | 59.2 | 37.0 | |
| Sex | 0.006 | |||
| Male | 51.1 | 47.9 | 52.3 | |
| Female | 48.9 | 52.1 | 47.7 | |
| Race/Ethnicity | <.0001 | |||
| White | 53.7 | 58.5 | 52.0 | |
| Black | 13.4 | 12.1 | 13.9 | |
| Hispanic | 23.5 | 21.2 | 24.3 | |
| Other | 9.4 | 8.2 | 9.8 | |
| Income | 0.9 | |||
| $0–$34,999 | 31.9 | 31.9 | 31.9 | |
| $35,000–$74,999 | 30.0 | 30.5 | 29.8 | |
| $75,000–$99,999 | 13.3 | 12.9 | 13.5 | |
| $100,000 and over | 24.8 | 24.7 | 24.8 | |
| Insurance Status | 0.5 | |||
| Uninsured | 7.5 | 7.9 | 7.3 | |
| Any private | 55.4 | 55.8 | 55.2 | |
| Public only | 37.1 | 36.3 | 37.5 | |
| Parental education | 0.009 | |||
| Bachelor’s or higher | 36.1 | 34.6 | 36.7 | |
| Some college | 34.5 | 37.4 | 33.3 | |
| HS or less | 29.4 | 28.0 | 30.0 | |
| Region | 0.007 | |||
| Northeast | 16.7 | 14.3 | 17.5 | |
| Midwest | 22.7 | 24.3 | 22.1 | |
| South | 36.9 | 36.2 | 37.2 | |
| West | 23.7 | 25.2 | 23.2 | |
| Comorbidities | <.0001 | |||
| 0 | 47.6 | 28.8 | 54.4 | |
| 1 | 27.7 | 30.0 | 26.8 | |
| 2–3 | 20.8 | 31.8 | 16.8 | |
| 4+ | 4.0 | 9.4 | 2.0 | |
| Has a personal healthcare provider | 0.08 | |||
| Yes | 82.7 | 84.2 | 82.2 | |
| No | 17.3 | 15.8 | 17.8 | |
Prevalence of CAM use among children with pain conditions
Children with pain were more likely to use CAM than children without pain. Of the children reported to have pain conditions in the last 12 months, 21.3% used CAM while among those children without pain conditions only 8.1% used CAM (χ2 p<0.001; Table 1). In our multivariate logistic regression analysis adjusting for predisposing, enabling, and need factors, having a pain condition was associated with an increased odds of CAM use (adjusted odds ratio (aOR) =2.38, 95% confidence interval (CI) 1.96–2.91, p<.001)(supplemental Table A). Parents of children with pain conditions using CAM were also asked whether they sought CAM to treat a specific health condition in their child. About one-third of these children (n=175, 33.9%), representing 1.1 million children nationwide, specifically used CAM to treat a pain-related condition. The remaining sample either did not report a specific reason for their CAM use or did not use CAM to specifically treat their pain.
CAM modalities most often used by children with pain
Among children with pain who used CAM, the most commonly used CAM modality was biologically-based therapies (47.3%), followed by manipulative or body-based therapies (46.3%), mind-body therapies (27.9%), and alternative medical systems (19.5%) (Table 2). There was some overlap in use of multiple CAM therapy categories. Among children with pain who used CAM, 70% used 1 modality, 21.8% used 2 modalities, and 8.2% used 3 or more modalities.
Table 2.
Complementary and alternative medicine (CAM) modalities used by children with pain who reported any CAM use (n=565). Column totals add up to >565 because some participants used several CAM modalities. CAM modalities used by fewer than 30 participants where collapsed into combined categories.
| CAM modality | n (Weighted %) |
n (Weighted %) |
|---|---|---|
| Biologically-based therapies | 255 (47.3) | |
| Herbal or non-vitamin supplements | 233 (42.8) | |
| Special diets | 33 (6.4) | |
| Manipulative or body-based therapies | 259 (46.3) | |
| Chiropractic or osteopathic manipulation | 201 (37.5) | |
| Massage therapy | 78 (12.1) | |
| Other (craniosacral therapy & exercise therapy) | 33 (6.7) | |
| Mind-body therapies | 175 (27.9) | |
| Meditation | 35 (5.3) | |
| Yoga | 136 (22.4) | |
| Other (biofeedback, hypnosis, guide imagery, progressive relaxation, tai chi, qi gong) | 81 (13.0) | |
| Alternative medical systems | 106 (19.5) | |
| Homeopathic medicine | 74 (15.9) | |
| Other (acupuncture, ayurveda, naturopathic medicine, traditional healers, energy therapy) | 61 (9.2) |
We also examined CAM use among those children with pain who used CAM to specifically treat a painful condition. Among this group, the most commonly used CAM to specifically treat pain was manipulative or body-based therapies (87.4%), followed by biology based therapies (33.5%), alternative medical systems (25%), and mind-body therapies (17.2%).
Factors associated with CAM use among children with pain
Among children with pain, being female, having higher income, and higher parental education levels were all significantly associated with increased CAM use (Table 3). White, non-Hispanic children with pain had higher CAM use than Hispanic and black children, but there were no significantly different rates of CAM use between white, non-Hispanic youth and “other” racial/ethnic categories. Additionally, child age was not associated with CAM use. Among clinical characteristics, having symptoms of sleep disturbances, stress, depression, and fatigue were not statistically associated with increased CAM use; however, having 4 or more comorbid conditions was strongly associated with CAM use among children with pain conditions. We also found that region of the United States was associated with CAM use for pain: participants from the South had much lower CAM use than those from other regions. Further examination revealed that participants from the South were overall less likely to use CAM for any condition (including participants without pain) as compared to other regions: 7.9% versus 13.8% (p<0.0001) (data not presented in tables).
Table 3.
Multivariate logistic regression analysis (adjusting for predisposing, enabling, and need factors) estimating the association between CAM use and sample sociodemographic and clinical characteristics among only children with pain (n=2,795).
| CAM use Weighted % | aOR | CI | p | |
|---|---|---|---|---|
| Age | ||||
| 4–6 | 23.1 | (ref) | ||
| 7–11 | 18.6 | 0.64 | 0.34–1.20 | 0.165 |
| 12–17 | 22.8 | 0.72 | 0.39–1.34 | 0.296 |
| Sex | ||||
| Male | 18.4 | (ref) | ||
| Female | 23.9 | 1.49 | 1.13–1.98 | 0.005 |
| Race/Ethnicity | ||||
| White | 25.2 | (ref) | ||
| Black | 11.8 | 0.70 | 0.43–1.14 | 0.155 |
| Hispanic | 12.9 | 0.68 | 0.51–0.92 | 0.013 |
| Other | 29 | 1.39 | 0.87–2.21 | 0.167 |
| Income | ||||
| $0–$34,999 | 12.5 | (ref) | ||
| $35,000–$74,999 | 20.5 | 1.40 | 0.97–2.02 | 0.068 |
| $75,000–$99,999 | 25.4 | 1.37 | 0.86–2.19 | 0.186 |
| $100,000 and over | 30.4 | 1.61 | 1.06–2.46 | 0.027 |
| Insurance Status | ||||
| Uninsured | 14.7 | (ref) | ||
| Any private | 26.7 | 1.08 | 0.63–1.85 | 0.79 |
| Public only | 14.1 | 0.83 | 0.48–1.45 | 0.515 |
| Parental education | ||||
| Bachelor’s or higher | 30.4 | (ref) | ||
| Some college | 20.9 | 0.69 | 0.50–0.94 | 0.02 |
| HS or less | 10.6 | 0.38 | 0.24–0.60 | <0.0001 |
| Region | ||||
| Northeast | 21.5 | (ref) | ||
| Midwest | 25.6 | 1.41 | 0.94–2.11 | 0.099 |
| South | 14.8 | 0.77 | 0.52–1.14 | 0.184 |
| West | 26.2 | 1.68 | 1.11–2.55 | 0.015 |
| Comorbidities | ||||
| 0 | 17.8 | (ref) | ||
| 1 | 21 | 1.15 | 0.82–1.59 | 0.418 |
| 2–3 | 22.4 | 1.34 | 0.95–1.90 | 0.094 |
| 4+ | 29.1 | 2.01 | 1.16–3.50 | 0.013 |
| Has a personal healthcare provider | ||||
| No | 15.4 | (ref) | ||
| Yes | 22.5 | 1.06 | 0.70–1.62 | 0.772 |
| Insomnia | ||||
| No | 19.6 | (ref) | ||
| Yes | 28.4 | 1.35 | 0.92–1.99 | 0.123 |
| Depression | ||||
| No | 21.2 | (ref) | ||
| Yes | 23.8 | 0.76 | 0.44–1.32 | 0.331 |
| Stress | ||||
| No | 19.2 | (ref) | ||
| Yes | 29.2 | 1.21 | 0.84–1.73 | 0.302 |
| Fatigue | ||||
| No | 19.8 | (ref) | ||
| Yes | 29.6 | 1.32 | 0.87–2.00 | 0.185 |
aOR: adjusted Odds Ration; CI: 95% Confidence Interval
Perceived benefits and reasons for CAM use among children with pain conditions
A large proportion (61%) of parents of children with pain reported that CAM use led to improved overall health for their child. Other perceived benefits for CAM use included reduced stress (reported by 55%), better sleep (42%), and feeling better emotionally (39%) (see Figure 1). The main reason for CAM use was for improved overall general wellness and disease prevention (83% of participants) (Figure 2). Other common reasons that parents reported using CAM therapies for their children with pain included that the treatment was perceived as natural (50%), it treats the cause and not just the symptoms (49%), it focuses on the whole person: body, mind, & spirit (35%), and the treatment was part of their upbringing (33%).
Discussion
In a nationally-representative sample in the United States, parents reported greater use of CAM for their children with pain conditions compared to parents of children without pain conditions. The most common CAM modalities used by children with pain were biologically-based therapies, such as herbal supplements and special dietary plans, followed by manipulative or body-based therapies (e.g., chiropractic, massage). We also found that, among children with pain conditions, CAM use was associated with female sex, higher parental income, and higher parental education. The majority of parents reported that their children benefited from CAM use.
This is the first study to evaluate CAM use in a nationally representative sample of children with and without pain conditions. Results indicated that a significant portion of children with pain conditions (21.3%) pursue CAM treatments for symptom management. However, this rate is lower than rates of CAM use reported in previous studies among clinical populations of children with pain presenting to multidisciplinary pain clinics (40–60%;3, 4), rheumatology clinics (64%;14), headache clinics (76%15), or gastroenterology clinics (64–95%;16). The discrepancy in rates between our study and others may be related to greater disease severity and disability found in clinical populations or other selection biases in small clinical samples as compared to our nationally-representative population.
CAM use was most prevalent among females, those with higher income, and those from families with higher parental education. However, CAM was least prevalent among participants from the South region of the United States. Further research is needed to understand potential reasons for this pattern. For example, there may be less access and insurance coverage for CAM approaches available to children in lower income households. Furthermore previous studies have found less availability of CAM services in the Southern United States17. These factors should be explored in future studies. We also found that CAM use was higher among children with pain conditions who had multiple co-morbidities compared to those with a single condition, which is consistent with previous literature finding that CAM use is more prevalent in children with complex health care needs.18, 19 This information may help better focus efforts to study CAM therapies in children with pain conditions; it is likely to lead to more generalizable findings if studies are designed to include children with multiple co-morbidities.
Among children with pain conditions, we found that biologically-based and manipulative/body-based therapies were most commonly used, with lower reported use of either mind-body therapies or alternative medical systems. This perhaps reflects that even though families are seeking a CAM treatment, there is still a preference for approaches that maintain a strong connection to Western thought and conventional medical approaches (i.e., separation of mind and body, relief is best obtained from an particular medication/supplement rather than behavioral methods) versus those approaches that involve a fundamentally different conceptualization. On the other hand biology-based and manipulative/body based therapies may be more readily available or less costly for families, explaining increased use.
Limitations
Results should be considered within the context of several limitations of this study. First, pain intensity, duration, and interference were not captured in the database. Inclusion of those specifiers beyond just the presence or absence of a painful condition could have possibly yielded additional information about the use of CAM to treat pain. Second, because this is a secondary cross-sectional analysis of an existing database we are unable to causally link pain and CAM use. Second, pain intensity, duration, and interference were not captured in the database. Inclusion of those specifiers beyond just the presence or absence of a painful condition could have possibly yielded additional information about the use of CAM to treat pain. Third, respondents for this survey were restricted to parents only, and we recognize that including child-report of the perceived benefits and reasons for using CAM would have contributed valuable perspectives. Future research should include child self-report where possible. Fourth, this study focusses on children receiving outpatient care and therefore results may not be generalizable to children who have pain during hospitalizations. Fifth, data on dose of each CAM therapy is not provided in this study, which may bias some of our findings on perceived benefits. For example patients may report more benefit if they received multiple acupuncture treatments versus only one. Additionally, there is a lack of definitional clarity within the CAM field as what approaches are conceptually considered “complementary” and “alternative.” For example, mind-body therapies such as biofeedback, relaxation, and mindfulness meditation could very well be included within a psychotherapy framework, which is already considered a significant part of the standard of care for pediatric pain.20–22 Despite these limitations, this study provides an important estimation of general use of CAM approaches in children with pain-related conditions in the U.S. that may guide future research and clinical service coordination for these vulnerable youth.
Future directions
Pain can be difficult to treat with conventional medical treatment. Multidisciplinary clinics that provide access to a range of professionals and treatment approaches are considered optimal for treating complex pediatric pain-related conditions, although access to such specialized care is not readily available to children in most communities.20 In both community and clinical settings, children may benefit from incorporation of CAM approaches in the treatment of pain symptoms; however, there are a number of important considerations. Although many CAM approaches have shown to be promising or probably efficacious for various pain-related disorders in children,23 the evidence base consists mainly of pilot or uncontrolled trials with limited evidence from randomized controlled trials on any CAM modality24, 25. Reasons for limited evidence from randomized CAM trials for chronic pain include that they are difficult to conduct, due to barriers associated with recruitment and retention (e.g.,26, 27). Furthermore even for CAM treatments with established empirical efficacy, there is a lack of understanding about the mechanisms of treatment effects (e.g.,28). Consequently there is a clear need for large-scale and rigorous trials to better understand which CAM approaches work, for whom, and in what setting, as well as any iatrogenic or interactive effects CAM treatments may have with conventional approaches.
Insurance carriers are increasingly covering CAM modalities for pediatric patients,29 and existing research shows that pediatric providers often do discuss and even recommend CAM treatments to their patients,30 but there is little communication or integration of care plans with CAM providers.7 Increasing communication between CAM and conventional providers will be an important next step for providing comprehensive, high-quality care that considers patient choice.31
Our study has some general clinical implications for health providers treating children with pain conditions. Providers in conventional, multidisciplinary, or integrative settings or practices should be cognizant that many children with pain use CAM and should inquire about the use of CAM when designing treatment plans, especially as families may not voluntarily mention their use of CAM treatments.15, 18 Since families are interested in using CAM treatments and they may be helpful for symptom management, health providers should familiarize themselves with referral options for CAM therapies in their communities32. However, additional research is urgently needed to better understand which CAM therapies are most efficacious for childhood pain conditions and for whom.
In conclusion, this study demonstrated that a significant portion of children with painful conditions use CAM strategies as part of their symptom management. Use of CAM by children with pain is associated with perceived benefit. While a growing body of literature supports the use of CAM in pediatric pain management, there is an urgent need to develop evidence based research with collaboration between CAM providers and conventional practitioners.
Supplementary Material
What’s new.
The current epidemiology of CAM use by children with pain is unknown. Overall, 26.6% of children in the United States have pain. Children with pain were much more likely to use CAM therapies as compared to children without pain.
Acknowledgments
CBG was supported by National Institutes of Health Ruth L. Kirschstein National Research Service Award Institutional Research Training Grant T32GM086270 (PI: TMP). TMP was partially supported by National Institutes of Health 2K24HD060068. JAR was supported by National Institutes of Health K23HD078239.
Funding source: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. CBG was supported by National Institutes of Health Ruth L. Kirschstein National Research Service Award Institutional Research Training Grant T32GM086270 (PI: TMP). TMP was partially supported by National Institutes of Health 2K24HD060068. JAR was supported by National Institutes of Health K23HD078239.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: The authors have no conflicts of interest to disclose.
Contributions: All authors contributed extensively to the work presented in this manuscript. C.B.G., J.A.R., and T.M.P. conceived the study. C.B.G. and J.A.R. designed the study and analyzed the data. C.B.G., S.E.B.E, and J.R.W drafted the paper. J.A.R. and T.M.P. critically revised the paper. All authors discussed the results and implications of the paper at all stages.
References
- 1.Groenewald CB, Wright DR, Palermo TM. Health care expenditures associated with pediatric pain-related conditions in the United States. Pain. 2015;156:951–957. doi: 10.1097/j.pain.0000000000000137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.King S, Chambers CT, Huguet A, et al. The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain. 2011;152:2729–2738. doi: 10.1016/j.pain.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 3.Vinson R, Yeh G, Davis RB, Logan D. Correlates of complementary and alternative medicine use in a pediatric tertiary pain center. Acad Pediatr. 2014;14:491–496. doi: 10.1016/j.acap.2014.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsao JC, Meldrum M, Kim SC, Jacob MC, Zeltzer LK. Treatment Preferences for CAM in children with chronic pain. Evid Based Complement Alternat Med. 2007;4:367–374. doi: 10.1093/ecam/nel084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008:1–23. [PubMed] [Google Scholar]
- 6.Lin YC, Lee ACC, Kemper KJ, Berde CB. Use of complementary and alternative medicine in pediatric pain management service: A survey. Pain Med. 2005;6:452–458. doi: 10.1111/j.1526-4637.2005.00071.x. [DOI] [PubMed] [Google Scholar]
- 7.Kundu A, Tassone RF, Jimenez N, Seidel K, Valentine JK, Pagel PS. Attitudes, Patterns of Recommendation, and Communication of Pediatric Providers About Complementary and Alternative Medicine in a Large Metropolitan Children’s Hospital. Clin Pediatr. 2011;50:153–158. doi: 10.1177/0009922810384724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mistry R, Babu GR, Mahapatra T, McCarthy WJ. Cognitive mediators and disparities in the relation between teen depressiveness and smoking. Drug and Alcohol Dependence. 2014;140:56–62. doi: 10.1016/j.drugalcdep.2014.03.022. [DOI] [PubMed] [Google Scholar]
- 9.Black LI, Clarke TC, Barnes PM, Stussman BJ, Nahin RL. Use of complementary health approaches among children aged 4–17 years in the United States: National Health Interview Survey, 2007–2012. Natl Health Stat Report. 2015:1–19. [PMC free article] [PubMed] [Google Scholar]
- 10.Andersen RM. National health surveys and the behavioral model of health services use. Med Care. 2008;46:647–653. doi: 10.1097/MLR.0b013e31817a835d. [DOI] [PubMed] [Google Scholar]
- 11.Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012;13:715–724. doi: 10.1016/j.jpain.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 12.StataCorp. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- 13.Rabbitts JA, Groenewald CB, Jacob AK, Low PA, Curry TB. Postural orthostatic tachycardia syndrome and general anesthesia: a series of 13 cases. J Clin Anesth. 2011;23:384–392. doi: 10.1016/j.jclinane.2010.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hagen LE, Schneider R, Stephens D, Modrusan D, Feldman BM. Use of complementary and alternative medicine by pediatric rheumatology patients. Arthritis Rheum. 2003;49:3–6. doi: 10.1002/art.10931. [DOI] [PubMed] [Google Scholar]
- 15.Dalla Libera D, Colombo B, Pavan G, Comi G. Complementary and alternative medicine (CAM) use in an Italian cohort of pediatric headache patients: the tip of the iceberg. Neurol Sci. 2014;35(Suppl 1):145–148. doi: 10.1007/s10072-014-1756-y. [DOI] [PubMed] [Google Scholar]
- 16.Schurman JV, Friesen CA. Integrative treatment approaches: family satisfaction with a multidisciplinary paediatric Abdominal Pain Clinic. Int J Integr Care. 2010;10 doi: 10.5334/ijic.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davis MA, Yakusheva O, Gottlieb DJ, Bynum JP. Regional Supply of Chiropractic Care and Visits to Primary Care Physicians for Back and Neck Pain. J Am Board Fam Med. 2015;28:481–490. doi: 10.3122/jabfm.2015.04.150005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kemper KJ, Vohra S, Walls R, et al. American Academy of Pediatrics. The use of complementary and alternative medicine in pediatrics. Pediatrics. 2008;122:1374–1386. doi: 10.1542/peds.2008-2173. [DOI] [PubMed] [Google Scholar]
- 19.Young L, Kemper KJ. Integrative care for pediatric patients with pain. J Altern Complement Med. 2013;19:627–632. doi: 10.1089/acm.2012.0368. [DOI] [PubMed] [Google Scholar]
- 20.Odell S, Logan DE. Pediatric pain management: the multidisciplinary approach. J Pain Res. 2013;6:785–790. doi: 10.2147/JPR.S37434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eccleston C, Palermo TM, Williams AC, et al. Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev. 2014;5:CD003968. doi: 10.1002/14651858.CD003968.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sibinga EM, Kemper KJ. Complementary, holistic, and integrative medicine: meditation practices for pediatric health. Pediatr Rev. 2010;31:e91–103. doi: 10.1542/pir.31-12-e91. [DOI] [PubMed] [Google Scholar]
- 23.Tsao JC, Zeltzer LK. Complementary and Alternative Medicine Approaches for Pediatric Pain: A Review of the State-of-the-science. Evid Based Complement Alternat Med. 2005;2:149–159. doi: 10.1093/ecam/neh092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hesse T, Holmes LG, Kennedy-Overfelt V, Kerr LM, Giles LL. Mindfulness-Based Intervention for Adolescents with Recurrent Headaches: A Pilot Feasibility Study. Evid Based Complement Alternat Med. 2015;2015:508958. doi: 10.1155/2015/508958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Snyder J, Brown P. Complementary and alternative medicine in children: an analysis of the recent literature. Curr Opin Pediatr. 2012;24:539–546. doi: 10.1097/MOP.0b013e328355a214. [DOI] [PubMed] [Google Scholar]
- 26.Evans S, Lung KC, Seidman LC, Sternlieb B, Zeltzer LK, Tsao JCI. Iyengar Yoga for Adolescents and Young Adults With Irritable Bowel Syndrome. J Pediatr Gastr Nutr. 2014;59:244–253. doi: 10.1097/MPG.0000000000000366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mano KEJ, Salamon KS, Hainsworth KR, et al. A Randomized, Controlled Pilot Study of Mindfulness-based Stress Reduction for Pediatric Chronic Pain. Altern Ther Health M. 2013;19:8–14. [PubMed] [Google Scholar]
- 28.Vlieger AM, van den Berg MM, Menko-Frankenhuis C, Bongers MEJ, Tromp E, Benninga MA. No Change in Rectal Sensitivity After Gut-Directed Hypnotherapy in Children With Functional Abdominal Pain or Irritable Bowel Syndrome. Am J Gastroenterol. 2010;105:213–218. doi: 10.1038/ajg.2009.613. [DOI] [PubMed] [Google Scholar]
- 29.Bellas A, Lafferty WE, Lind B, Tyree PT. Frequency, predictors, and expenditures for pediatric insurance claims for complementary and alternative medical professionals in Washington State. Arch Pediatr Adolesc Med. 2005;159:367–372. doi: 10.1001/archpedi.159.4.367. [DOI] [PubMed] [Google Scholar]
- 30.Sawni A, Thomas R. Pediatricians’ attitudes, experience and referral patterns regarding Complementary/Alternative Medicine: a national survey. BMC Complement Altern Med. 2007;7:18. doi: 10.1186/1472-6882-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Medicine lo. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press; 2001. [PubMed] [Google Scholar]
- 32.Neri CM, Beeson T, Mead H, Darbari DS, Meier ER. Provider Perspective on Integrative Medicine for Pediatric Sickle Cell Disease-related Pain. Glob Adv Health Med. 2016;5:44–50. doi: 10.7453/gahmj.2015.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


