TO THE EDITOR
Cow’s milk is the causal food in 2.5% of children with food allergy and approximately 75% of allergies to milk resolve by the early teenage years (1). The vast majority of individuals who develop IgE-mediated immediate (type I) hypersensitivity to cow’s milk, do so during infancy; the development of immediate hypersensitivity to cow’s milk after the age of 3 years is unusual (2,3). In one study, only 8 of 66 children who developed IgE-mediated immediate hypersensitivity to cow’s milk did so after the age of 240 days (3). All 8 of these subjects had a preceding diagnosis of food protein induced enterocolitis syndrome (FPIES) suggesting that de novo development of IgE-mediated immediate hypersensitivity to cow’s milk after infancy is very rare (3). The identification of conditions that predispose to the development of IgE-mediated immediate hypersensitivity is of interest to our understanding of the pathophysiology of allergic disease and to the management of patients with food allergies.
IgE-mediated immediate hypersensitivity to foods and eosinophilic esophagitis (EoE) are thought to have related but distinct pathophysiologic mechanisms (4). However, recent studies suggest that IgE-mediated immediate hypersensitivity to food allergens may predispose to the development of EoE to the same food (5). Here we discuss the case of a patient who developed IgE-mediated immediate hypersensitivity to cow’s milk several years after cow’s milk was identified as the causative agent for the patient’s EoE. This observation suggests that EoE may predispose to the development of IgE-mediated immediate hypersensitivity to the same food.
At 14 months of age, a boy presented to our practice due to feeding difficulties, vomiting and reflux symptoms. The boy was the product of a full-term, uncomplicated pregnancy, was on a milk-based formula as an infant, and had a past medical history of developmental delay and eczema. The patient developed reflux symptoms as an infant and was transiently on ranitidine, which was subsequently discontinued. At nine months of age, the patient developed problems with progression of food textures; refusing stage III baby foods with gagging and spitting. The patient also developed the behavior of placing his finger in his mouth, which resulted in vomiting. The patient was started on omeprazole therapy without resolution of his symptoms. Initial studies including a single contrast upper GI examination and gastric emptying study were notable only for reflux.
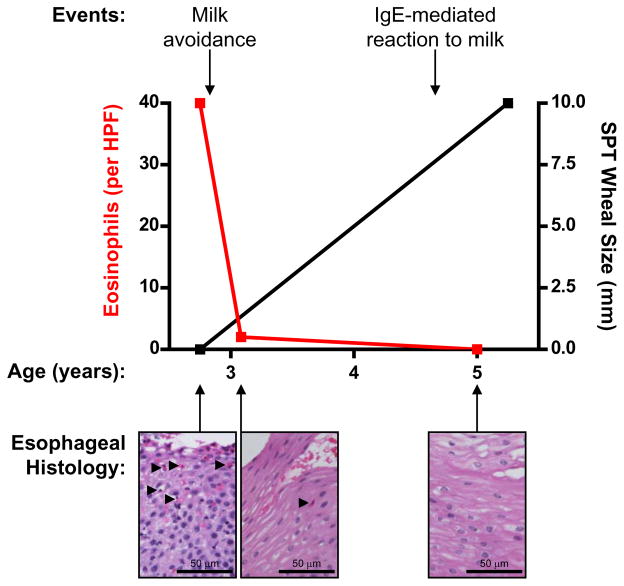
At 33 months of age, the patient underwent an esophagogastroduodenoscopy and biopsy that was notable for 40 eosinophils per high power field on tissue sections of the esophagus. The patient was on an optimal omeprazole dose at the time confirming the diagnosis of EoE. At that time, the patient was avoiding egg and peanut (due to suspected IgE-mediated reactions) and was drinking milk on a regular basis. Subsequent IgE-mediated skin prick testing was positive to egg, peanut, fish and wheat and negative to multiple other foods including milk (0 mm wheal, 0 mm flare). Patch skin testing was positive to oat and barley and equivocal to cow’s milk. The patient’s mother was advised to continue avoidance of egg and peanut due to documented reactions and positive testing. In addition, given that milk is the most common cause of eosinophilic esophagitis and there is a 40% false-negative testing rate (6), the patient’s family was advised to remove dairy from the patient’s diet. Repeat esophagogastroduodenoscopy and esophageal biopsy at 37 months of age (three months after removal of dairy from the patient’s diet) revealed the absence of esophageal eosinophils. With continued avoidance of dairy (in addition to egg, peanut and fish), the patient was able to discontinue omeprazole therapy without recurrence of his symptoms.
At nearly five years of age, after two and a half years of continued avoidance of dairy, the patient had an accidental ingestion of 1/3 of a cup of whole milk resulting in symptoms of oropharyngeal edema requiring therapy with anti-histamines. Repeat esophagogastroduodenoscopy and esophageal biopsy again revealed the absence of esophageal eosinophils. Subsequent skin prick testing was positive to milk (10 mm wheal, 20 mm flare). At the time of publication of this report, the patient had not developed IgE-mediated immediate hypersensitivity to any additional foods.
We report a case of a patient who developed IgE-mediated immediate hypersensitivity to cow’s milk after the identification of cow’s milk as the causative agent for the patient’s eosinophilic esophagitis. Animal models of EoE display increased levels of thymic stromal lymphopoietin, interleukin-4 and other type 2 cytokines in the inflamed esophagus (4). These cytokines, in the presence of food allergens, may promote T helper type 2 cell differentiation, B cell class-switching and the generation of food-specific IgE resulting in the potential for immediate hypersensitivity reactions. A positive association between EoE and the subsequent development of IgE-mediated immediate hypersensitivity may influence clinical practice. However, additional studies are necessary to determine whether EoE is associated with higher rates of development of immediate hypersensitivity to the same or other foods.
Figure 1.
Depiction of the clinical timeline for a patient who developed IgE-mediated food allergy to cow’s milk after cow’s milk had been identified as the causal agent for the patient’s eosinophilic esophagitis. Maximum eosinophil count per high power field (HPF) indicated on the left axis (red). Wheal skin test size (mm) indicated on the right axis (black). Clinical history and hematoxylin and eosin staining of esophageal tissue sections shown above and below the graph respectively (eosinophils marked with black arrows).
CLINICAL IMPLICATIONS.
We discuss a patient who developed IgE-mediated immediate (type I) hypersensitivity to a food previously identified as the causative agent for eosinophilic esophagitis (EoE). Further studies may be warranted to determine whether EoE predisposes to the development of immediate hypersensitivity.
Acknowledgments
FUNDING:
We acknowledge the Stuart E. Starr Chair in Pediatrics, the Department of Defense (W81XWH-11-1-0507), and the Institute for Translational Medicine and Therapeutics (UL1-RR024134) for funding support. The authors declare that they have no relevant conflicts of interest.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Spergel JM. Natural history of cow’s milk allergy. J Allergy Clin Immunol. 2013 Mar;131(3):813–814. doi: 10.1016/j.jaci.2013.01.027. [DOI] [PubMed] [Google Scholar]
- 2.Eller E, Kjaer HF, Host A, Andersen KE, Bindslev-Jensen C. Food allergy and food sensitization in early childhood: results from the DARC cohort. Allergy. 2009 Jul;64(7):1023–1029. doi: 10.1111/j.1398-9995.2009.01952.x. [DOI] [PubMed] [Google Scholar]
- 3.Katz Y, Rajuan N, Goldberg MR, Eisenberg E, Heyman E, Cohen A, et al. Early exposure to cow’s milk protein is protective against IgE-mediated cow’s milk protein allergy. J Allergy Clin Immunol. 2010 Jul;126(1):77–82. e1. doi: 10.1016/j.jaci.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 4.Noti M, Wojno ED, Kim BS, Siracusa MC, Giacomin PR, Nair MG, et al. Thymic stromal lymphopoietin-elicited basophil responses promote eosinophilic esophagitis. Nat Med. 2013 Aug;19(8):1005–1013. doi: 10.1038/nm.3281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maggadottir SM, Hill DA, Ruymann K, Brown-Whitehorn TF, Cianferoni A, Shuker M, et al. Resolution of acute IgE-mediated allergy with development of eosinophilic esophagitis triggered by the same food. J Allergy Clin Immunol. 2014 May;133(5):1487–1489. e1. doi: 10.1016/j.jaci.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 6.Spergel JM, Brown-Whitehorn TF, Cianferoni A, Shuker M, Wang ML, Verma R, et al. Identification of causative foods in children with eosinophilic esophagitis treated with an elimination diet. J Allergy Clin Immunol. 2012 Aug;130(2):461–7. e5. doi: 10.1016/j.jaci.2012.05.021. [DOI] [PubMed] [Google Scholar]