Abstract
Background
Greater hospital case volumes are associated with improved outcomes for high-risk procedures. The hospital-outcome association for complex but low mortality procedures and the association between surgeon versus hospital case volume and surgical outcomes has been less explored. We examined the association between surgeon and hospital volume and the success for free tissue transfer (free flap) surgery. We hypothesized that there would be positive associations between hospital and surgeon volume, and the success of free flap surgery.
Methods
The study design was a cross-sectional analysis of adults 18–64 years of age who underwent free flap surgery. We used 100% of all free flap operations between 2001 and 2012 using Taiwan’s national data that cover the entire population of 23 million in the country. We applied hierarchical regression modeling to analyze volume-outcome associations.
Results
The association between hospital volume and a free flap success was small but positive (OR=1.007; CI=1.00–1.01). For surgeons, their years of experience had a positive association with success of the operation (OR=1.04; CI=1.02–1.06) rather than their annual case volume. Compared with low-volume surgeons (<11 annual cases) working in low-volume hospitals (<95 annual cases), high-volume surgeons (> 25 annual cases), working in high-volume hospitals (>156 annual cases) showed greater odds of operation success (OR=2.97; CI=1.21–7.29).
Conclusions
Higher volume hospitals and more experienced surgeons, regardless of their annual volume, showed better outcomes. Increasing demand for high-quality care and Taiwan’s national policies toward centralization of complex surgical procedures have increased competition among hospitals.
The volume-outcome association was first introduced in 1979 by Luft et al., who asserted that there was an inverse relationship between surgical volume and in-hospital mortality.1 Since then, over 400 articles have been published on this topic over a wide variety of medical procedures including coronary angioplasties, cancer surgeries, surgical treatment for acute myocardial infarctions, and pancreatectomies.2–9 The majority of these studies conclude that there is an association between surgical volume and lower mortality rates. Many proponents of the volume-outcome association suggest that healthcare policies should encourage regionalization of high-risk, complex surgeries to high-volume medical centers. For example, Gordon et al. followed in-hospital mortality after Whipple procedures over a twelve-year period over which the Johns Hopkins Hospital went from performing 20% of these procedures to 58% and the in-hospital mortality rate dropped from 17% to 5%.2 The authors estimated that the majority of the decline in the mortality rate was attributed to the centralization of care in Maryland.2
Despite many unresolved challenges, the regionalization and systematic coordination of care for many high-profile surgical operations has garnered increased attention.10 The complexity of free flap operation suggests that if these procedures are predominantly performed at higher-volume centers, it might improve patient outcomes. The success rate of free flap ranges between 65–90%.11–14 The majority of studies that test the volume-outcome hypothesis examine high mortality procedures.15–18 Little is known about the association between the outcome of complex but low mortality procedures such as free flap and hospital-volume. Furthermore, the observed association between volume and outcome may be that high-volume hospitals tend to have surgeons who are more experienced with specific procedures.16 Although many studies have explored the association between hospital or surgeon volumes and outcome measures independently, relatively few have examined the associations between both hospital and surgeon volumes and outcome measures simultaneously.19
Using the 2001–2012 National Health Insurance Research Database (NHIRD) of Taiwan, we examined the associations between hospital- and surgeon-volumes, and the success of free flap. Owing to Taiwan’s universal single-payer healthcare system, its national data are ideal for examining the volume-outcome associations. In this study, we used all free flaps performed in Taiwan over the study period. Our specific aims were to (1) determine the surgical success of the free flap in high-volume compared with low-volume hospitals; (2) examine the operation success among high-volume compared with low-volume surgeons; and (3) assess the operation success among high-volume surgeons working in high-volume hospitals compared with other combinations of hospital- and surgeon-volumes. We hypothesized that greater volume surgeons and hospitals have a higher probability of success. The impact of this study is to translate the Taiwan experience in free flap to improve outcomes of this complex reconstructive procedure in the U.S.
Methods
Data
We used the 2001–2012 NHIRD of Taiwan to examine the probability of success, defined as survival of the first attempted free flap, adjusting for patient, surgeon, and hospital characteristics. The NHIRD covers the use of all medical services and prescription drugs for over 23 million people, or more than 99% of Taiwan’s population. Additionally, we merged the NHIRD data files with additional registry files: (1) the registry of board certified surgeons and (2) the registry of contracted medical facilities to obtain further information on surgeon and hospital characteristics. The internal review boards of University of Michigan and Chang Gung Memorial Hospital (CGMH) approved this study. Finally, to examine the validity of our data, we compared medical chart data of all free flap patients in CGMH with their corresponding records in NHIRD in 2012. No significant variation is observed (See Table, Supplemental Digital Content 1, which shows the Overall Statistics for all Free Flap Operations in Chang Gung Memorial Hospital in 2012, INSERT LINK.).
Study Sample
All patients who had received a free flap (procedure codes 62032B to 62038B, except 62034B) between 2001 and 2012 were included in the study. Initially, 1,694 surgeons performed 41,761 free flap operations in 133 hospitals during the study period. We excluded burn patients (international Classification of Diseases, Ninth Revision, clinical modification code 948) from the study sample because of other confounding issues affecting success of free flap. Additionally, if more than one free flap operation was performed at the same time, we only included the first operation. Otherwise, because the data may not have been entered chronologically with specific date, determining the success or failure of free flap would not have been possible. Our final sample size, after different exclusion criteria had been applied, included 877 surgeons who performed 25,327 surgeries in 127 hospitals (Figure 1).
Figure 1.
Schematic Flow for Patient Selection
Source: 2001–2012 National Health Insurance Research Database in Taiwan
Hospital and Surgeon Volume Group
Within the NHIRD, a unique national identifier is assigned to each hospital and surgeon. The final principal physician is the one who is responsible for discharging the patient. In cases where more than two surgeons identified as principal surgeons, we chose the one with a plastic surgery specialty because most free flaps are performed by plastic surgeons. In the absence of a plastic surgeon, we chose the attending surgeon who the patient saw within the first three months after the surgery. To define the volume groups for surgeons and hospitals, we sorted their corresponding volumes (number of free flap operations) in ascending order into three approximately equal groups.15,16,20,21 For hospitals the three categories were: less than 95, between 95 and 156, and more than 156 operations per year; for surgeons the three categories were less than 11, between 11 and 25, and more than 25 operations per year.
Variables
Dependent Variable
The main outcome of interest was the survival of the free flap (See Table, Supplemental Digital Content 2, which shows the List of Free Flap Codes, INSERT LINK.). We measured success of the operation using the algorithm defined in detail in Table SDC 3 (See Table, Supplemental Digital Content 3, which shows the Algorithm for Free Flap Failure. Note: A free flap failure is defined by presence of any of the four conditions on the left + any of the two conditions on the right, INSERT LINK.) Briefly, if within three months of initial procedure, CPT codes indicated re-exploration (69001B, 69003B, 69005B), debridement (48001C–48006C), bleeding (69029B), or anastomosis of vessels (69008B, 690032C) followed by the performance of another flap (62032B–62038B), or a local flap (62045B–62047B, 62049B, 62051B–62056B, 62058B–62060B), we considered that the original free flap had failed; otherwise, we classified the operation as successful.
The main explanatory variables were the average annual volume of operations performed among surgeons and hospitals after controlling for patient, surgeon, and hospital characteristics. For patient characteristics, we included age at the time of surgery, gender, number of comorbid conditions within a year of the operation (based on the Elixhauser algorithm), and whether the operation was categorized as emergency or planned. Hospital characteristics included the status of the hospital as being public vs. private, its teaching status, and its geographic location. Finally, we controlled for each surgeon’s years of experience and case volume.
Statistical Analysis
Our main analyses focused on the associations between surgeon and hospital volumes, and success of the operation, as defined above. We performed analyses using both hospital and surgeon volumes as continuous variables. Additionally, in order to perform additional sensitivity analyses and also to examine the interaction effects of different hospital and surgeon volumes on success of the operation, we ran our regression models using categorical variables for volume. We used a Generalized Linear Mixed Model (GLMM) with a logistic link function and specified a hospital- and surgeon-level random effect to account for repeated measures and potential correlation among patients treated by the same surgeon or in the same hospital. To fully establish and explore the associations between providers and patient outcomes, we performed a series of step-in, multi-level regression models: (1) analyzing the association between success of the operation and hospital volume adjusting for patient characteristics only, (2) analyzing the association between success of the operation and hospital volume, adjusting for patient and hospital characteristics, and (3) analyzing the association between success of the operation and hospital characteristics adjusting for surgeon volume and years of experience. We adjusted for the effect of clustering of patients (level 1) within surgeons (level 2) and clustering of the surgeons within hospitals (level 3).
Finally, we created a Receiver Operating Characteristic (ROC) curve using our completely adjusted regression model. We used Youden’s J statistics method to calculate the best cutoff volume for hospitals. Youden’s J statistics is a common method for calculating the optimal cutoff point for the target continuous variable. The cutoff point showed the minimum hospital volume to achieve the best sensitivity and specificity. By looking for the optimal value with the highest Youden’ J statistics (J=sensitivity+specificity-1), we assumed that sensitivity and specificity had the same important in our study.
All analyses were done at a patient level. We used SAS statistical package (version 9.3; SAS Institute, Inc., Cary, N.C) for all analyses.
Results
Table 1 presents patient and provider characteristics by stratifying them into three mutually exclusive groups based on annual hospital volume (< 95; between 95 and 156; and > 156 cases). Patients were evenly distributed among the three groups (30–35% in each group). The mean age of free flap patients was about 46 years, with 86% being male. On average, the patients had two chronic conditions. More than 97% of all free flap cases were scheduled rather than being emergency surgeries. There were two times more emergent cases in low-volume hospitals compared with medium or high-volume centers. Out of 877 surgeons performing free flaps, more than half (56%) were working in hospitals with less than 95 annual free flaps (low volume hospitals); these surgeons had fewer annual operations compared with surgeons working in hospitals with more than 156 free flaps (high-volume hospitals) (4 vs. 11 surgeries) and had fewer years of experience (7 vs. 10 years). About 90% of 127 hospitals that performed free flaps had less than 95 annual operations; in contrast, only 3 hospitals had more than 156 annual operations. The majority of the hospitals in our sample were private (63%), teaching (85%) hospitals. Higher volume hospitals had more beds and more plastic surgeons. For example, on average, high-volume hospitals had 3,285 beds and 41 plastic surgeons compared to 1,131 beds and 10 plastic surgeons at low-volume hospitals (p < 0.001 for both). Although statistically significant, the unadjusted difference in free flap success between the low-volume (94%) and high-volume (96%) hospital groups was minimal (2%; p < 0.001).
Table 1.
Characteristics of Patients (18–64 Years), Surgeons, and Hospitals for Free Flap Procedures between 2001–2012 in Taiwan†
| Characteristics | Low-Volume Hospitals (≤94) | Medium-Volume (95–156) | High (>156) | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| # (%) | Mean (SD) | # (%) | Mean (SD) | # (%) | Mean (SD) | # (%) | Mean (SD) | p-value | |
| Patient Characteristics | |||||||||
|
| |||||||||
| N of patients=25327 | 8,744 | 7,829 | 8,754 | 25,327 | |||||
| Male | 7,532 (86%) | 6,976 (89%) | 7,376 (84%) | 21,884 | <0.001* | ||||
| Age (Year) | 46 (11) | 48 (10) | 45 (11) | 46 (11) | <0.001* | ||||
| Elixhauser Comorbidity | 1.67 (1.44) | 1.93 (1.35) | 1.64 (1.35) | 1.74 (1.39) | <0.001* | ||||
| Income | <0.001* | ||||||||
| Low | 2,359 (27%) | 2,006 (26%) | 2,114 (24%) | 6,479 (26%) | |||||
| Middle | 4,202 (48%) | 3,836 (49%) | 4,197 (48%) | 12,235 (48%) | |||||
| High | 918 (11%) | 799 (10%) | 1,056 (12%) | 2,773 (11%) | |||||
| Family | 1,265 (14%) | 1,188 (15%) | 1,387 (16%) | 3,840 (15%) | |||||
| Emergency Admission | 496 (6%) | 142 (2%) | 229 (3%) | 867 (3%) | <0.001* | ||||
|
| |||||||||
| Surgeon Characteristics | |||||||||
|
| |||||||||
| N of surgeons=877 | 490 | 237 | 150 | 877 | |||||
| Mean of surgeon annual volume over 12 years | 4.19 (6) | 7 (8) | 11 (19) | 6 (10) | <0.001* | ||||
| Surgeon Experience (Year) | 7 (6) | 9 (6) | 10 (7) | 9 (6) | <0.001* | ||||
|
| |||||||||
| Hospital Characteristics | |||||||||
|
| |||||||||
| N of hospitals=127 | 115 | 9 | 3 | 127 | |||||
| Mean of hospital annual volume | 12 (21) | 122 (20) | 425 (287) | 30 (80) | <0.001* | ||||
| Ownership | 0.406 | ||||||||
| Public | 43 (37%) | 3 (33%) | 0 (0%) | 46 (36%) | |||||
| Private | 72 (63%) | 6 (67%) | 3 (100%) | 81 (64%) | |||||
| Teaching hospital | 98 (85%) | 9 (100%) | 3 (100%) | 110 (87%) | 0.359 | ||||
| Geographic location | 0.798 | ||||||||
| Northern | 46 (40%) | 3 (33%) | 1 (33%) | 50 (39%) | |||||
| Central | 29 (25%) | 2 (22%) | 0 (0%) | 31 (24%) | |||||
| Southern | 35 (30%) | 3 (33%) | 2 (67%) | 40 (32%) | |||||
| Eastern | 5 (4%) | 1 (11%) | 0 (0%) | 6 (5%) | |||||
| Average number of beds | 1,131 (696) | 2,207 (857) | 3,285 (1,574) | 1,411 (991) | <0.001* | ||||
| Average # of plastic surgeons | 10 (8) | 15 (8) | 41 (18) | 22 (18) | <0.001* | ||||
| Successful free flaps | 8,272(94%) | 7,399(94%) | 8,420(96%) | 24,091(95%) | <0.001* | ||||
From Taiwan’s National Health Insurance Research Database 2001–2012
Significantly different among hospital volume groups at the 95% confidence interval.
Table 2 presents our three step-in regression results. First, we included only patient characteristics in the model; second, we added hospital characteristics; and third, we included surgeon characteristics. Our aim was to see the influence of other variables in the association between hospital volume and the rate of successful surgical outcome. In terms of specific patient characteristics, the number of comorbid conditions and whether the operation was emergent or planned both had an inverse association with the success of the free flap operation (OR=0.94, CI=0.90–0.98; and OR=0.59, CI=0.45–0.78, respectively). Among the hospital characteristics analyzed, being a public hospital rather than private was associated with higher odds of success (OR=1.73, CI=1.08–2.77). The association between average number of hospital beds and free flap success was statistically significant, but trivial. Although minimal, as we added hospital and surgeon characteristics to our first model, hospital volume consistently showed a positive association with success of free flap operations (OR=1.007; CI=1.00–1.01). Finally, surgeons’ years of experience (and not their annual volume) had a small but positive association with the success of free flap (OR=1.04; CI=1.02–1.06).
Table 2.
Generalized Linear Mixed Models for Probability of Success of Free Flap, 2001–2012 in Taiwan†
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Parameter | Odds Ratio | 95% CI | P-value | Odds Ratio | 95% CI | P-value | Odds Ratio | 95% CI | P-value |
| No. of patients, 25327 | |||||||||
| Gender | |||||||||
| Female | 0.995 | 0.84–1.18 | 0.955 | 0.967 | 0.81–1.15 | 0.711 | 1.004 | 0.84–1.20 | 0.965 |
| Male (ref) | |||||||||
| Patient age | 1.003 | 1.00–1.01 | 0.345 | 1.006 | 1.00–1.01 | 0.054 | 1.004 | 1.00–1.01 | 0.207 |
| Elixhauser | 0.939 | 0.90–0.98 | 0.004* | 0.957 | 0.92–1.00 | 0.050* | 0.938 | 0.90–0.98 | 0.005* |
| Emergency | |||||||||
| Yes | 0.463 | 0.36–0.60 | <.001* | 0.469 | 0.36–0.61 | <.001* | 0.593 | 0.45–0.78 | <.001* |
| No (ref) | |||||||||
| Surgeon experience (year) | 1.038 | 1.02–1.06 | <.001* | ||||||
| Surgeon volume | 0.994 | 0.99–1.00 | 0.054 | ||||||
| Hospital type | |||||||||
| Public | 1.777 | 1.11–2.85 | 0.017* | 1.728 | 1.08–2.77 | 0.024* | |||
| Private (ref) | |||||||||
| Teaching hospital | |||||||||
| Yes | 0.813 | 0.17–3.93 | 0.796 | 0.895 | 0.18–4.52 | 0.894 | |||
| No (ref) | |||||||||
| Geographic location | |||||||||
| Central | 0.807 | 0.49–1.34 | 0.407 | 0.852 | 0.50–1.45 | 0.553 | |||
| Eastern | 1.032 | 0.38–2.84 | 0.951 | 0.966 | 0.35–2.64 | 0.947 | |||
| Southern | 1.012 | 0.64–1.61 | 0.958 | 1.062 | 0.67–1.69 | 0.799 | |||
| Northern (ref) | |||||||||
| Average number of beds | 0.999 | 1.00–1.00 | <.001* | 0.999 | 1.00–1.00 | <.001* | |||
| Average number of plastic surgeons | 0.988 | 0.97–1.01 | 0.268 | 0.980 | 0.96–1.00 | 0.099 | |||
| Hospital volume | 1.001 | 1.00–1.00 | 0.429 | 1.006 | 1.00–1.01 | <.001* | 1.007 | 1.00–1.01 | <.001* |
From Taiwan’s National Health Insurance Research Database 2001–2012
Significantly at the 95% confidence interval.
Figure 2 shows our ROC curve. The area under the ROC curve (AUC) represents the accuracy of the model. AUC values range from 0.5 to 1, with higher values indicating better accuracy; our AUC was 0.8. The optimal cutoff point with the highest Youden’ J value was 131 annual free flap cases at the hospital; the sensitivity and specificity of our model were 70.2% and 72%, respectively. Accordingly, the success rate of free flap in hospitals with 131 annual operations is expected to be 94%. Moreover, a higher success rate can be expected if the hospital’s annual volume is higher than 131 cases because we have shown that hospital volume has a significantly positive influence on the success rate of operation.
Figure 2.
Receiver operating characteristic (ROC) curve
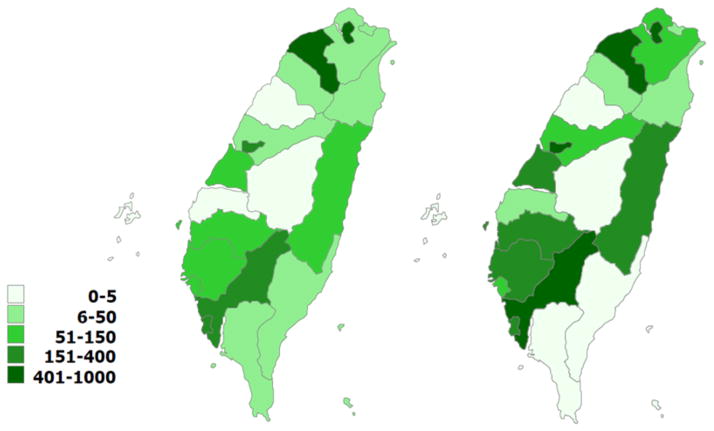
Figure 3 presents the distribution of hospitals for free flap in Taiwan. Between 2001 and 2012, concentration of hospitals based on their annual volume changed. In 2001, hospitals with different annual volume distributed more evenly across the country. In 2012, there were more hospitals with greater than 150 annual free flaps, regionalized across Taiwan.
Figure 3.
Distribution of Hospitals, by Volume, for Free Flap Surgery in Taiwan in 2001 (left) and in 2012 (right)
Source: 2001and 2012 National Health Insurance Research Database in Taiwan
Sensitivity analysis
In addition to using continuous variables for surgeon and hospital volumes, we used categorical variables for both hospitals and surgeons to examine associations between volume and outcome and hospital/surgeon volumes interactions. The results are presented in Tables, SDC 4 and SDC 5. (See Table, Supplemental Digital Content 4, which shows the Generalized Linear Mixed Model for Probability of Success of Free Flap, 2001–2012 in Taiwan (Categorical Volume) †
†From Taiwan’s National Health Insurance Research Database 2001–2012
*Significantly at the 95% confidence interval, INSERT LINK.) (See Table, Supplemental Digital Content 5, which shows the Generalized Linear Mixed Model for Probability of Success of Free Flap, 2001–2012 in Taiwan (with Interaction Terms Between Hospital and Surgeon Volumes) †
†From Taiwan’s National Health Insurance Research Database 2001–2012
*Significantly at the 95% confidence interval, INSERT LINK.) Compared with being treated in low-volume hospitals (< 95 annual operations), being treated in medium-(between 95–156 annual operations) and high-volume (> 156 annual operations) hospitals increased odds of operation success by 2.40 (CI=0.24–4.64; p=0.009) and 6.18 (CI=2.01–18.97; p=0.002), respectively. Finally, we examined simultaneous contribution of hospital and surgeon volumes to the success of free flap (See Table, Supplemental Digital Content 5, INSERT LINK). Our results show that high-volume surgeons working in high-volume hospitals compared with low-volume surgeons working in low-volume hospitals had higher odds of operational success (OR=2.97; CI=1.21–7.29; p=0.018).
Discussions
Our study yielded three main findings. First, regardless of hospital volume, free flap success rate was high in Taiwan. Our results, however, still indicate a small but positive association between hospital annual volume and success of free flap. Second, surgeon experience rather than volume was more closely associated with operation success. Finally, the combination of high-volume surgeons working in high-volume hospitals yielded higher odds of success in free flap compared to other surgeon-hospital combinations.
Although free flap is a complex and resource intensive surgical procedure, it can provide substantially better functional and aesthetic restoration.22 When flaps fail, however, it not only has devastating consequences on the patient, but also wastes valuable resources.23 The high success rate of free flaps in Taiwan may be attributed to three potential factors: (1) the widespread use of free flaps, especially for the treatment of head and neck cancer, which is more prevalent in Taiwan24 than in other countries; (2) incentivized national healthcare policies towards regionalization of care for complex surgeries such as free flaps;25,26 and (3) high-quality and intense microsurgery training in Taiwan.27,28
Taiwan’s National Health Insurance Program (NHIP) is one of the most successful single-payer health systems providing health coverage to more than 99% of Taiwan’s 23 million residents.25,29,30 Consistent economic prosperity in Taiwan along with a substantial rise in demand for medical care due to the implementation of the NHIP in 1995 have yielded a highly competitive environment among hospitals in Taiwan.26 The high rate of free flap success in Taiwan may be explained by a series of comprehensive healthcare policies. Taiwan’s NHI payment system is based on fee-for-service payment system. Unlike other countries with a single-payer system, such as United Kingdom or Canada, Taiwanese patients are allowed and encouraged, without any gate-keeping policy, to choose their hospitals and physicians. Thus, it is not uncommon for patients to spend time shopping for a higher quality hospital before scheduling an operation. The majority of free flap operations in Taiwan between 2001 and 2012 were scheduled (non-urgent), which means patients may have had time to find the best provider.
Although our results did not show significant associations between teaching status or number of plastic surgeons and better outcomes, in the U.S., given the expenses required to maintain qualified monitoring personnel and equipment, and the lack of plastic surgery residents and microvascular fellows in non-teaching hospitals, free flap procedures are performed more often and with better results in large teaching hospitals.31–33 Potentially, through developing partnerships with large teaching hospitals, low-volume and non-teaching hospitals could gain access to some of the economically advantageous benefits of those hospitals.34–35 For example, low-volume hospitals may devise a referral arrangement to send complex cases to selected high-volume centers so that the patients can be treated efficiently. Finally, the comparison among different surgeon’s specialties in free flap success would have been an intriguing question; however, the high success rate in free flap procedures in Taiwan makes such comparison not particularly relevant.
Additionally, the hospital reimbursement system is based on each hospital’s capacity, patient volume, and services provided. After the implementation of Taiwan’s global budget in 2002,31 hospitals have been incentivized to increase their patients’ length of stay or intensity of provided care to receive better financial reimbursements.31 Under global budget cap, all hospitals share a limited budget and thus rigorously compete to increase their market share.31 Despite the high patient demand, because of the large number of healthcare providers, patient wait times in Taiwan are among the lowest among developed countries.26 For example, wait times for scheduling a hip and knee replacements are 12 and 18 days, respectively, compared to months if not years in Canada.26 Additionally, all insured patients in Taiwan have their personal “smart insurance cards,” containing their important medical information. These cards can be read by all hospitals in the country and used for hospital reimbursement. A combination of the above policies along with a growing standard of care due to Taiwan’s economic prosperity has increased the demand for high quality care. In Taiwan, competition among hospitals to attract patients is intense. As financial pressure from reduced government reimbursements continues to force smaller hospitals to exit the market, the number of hospitals is declining and they are becoming more specialized. For example, in 2012, only 133 out of 508 hospitals in Taiwan (about 25%) were performing free flap procedures. Therefore, although the hospital-volume effect was small, our findings agree with previous research, showing better outcomes among higher volume hospitals.15–18
Not surprisingly, the outcome of a surgical procedure depends how well the operation itself is performed. Contrary to previous literature,16,32,33 we did not find any association between surgeon volume and the success of free flap surgeries. That could be attributed to a few high volume surgeons having relatively higher complications with more residents involving at a teaching hospital. However, similar to other studies,34–36 our results indicate a positive association between surgeon experience and the success of an operation. For example, Schmidt et al. found that when performing pancreaticoduodenectomies, more experienced surgeons showed better outcomes (e.g. lower pancreatic leak rate, less intraoperative blood loss, or mean shorter operative time), regardless of their annual volume.37 The quality of a surgical operation is linked to surgeon’s experience; more experience is associated with shorter operating times, fewer surgical mistakes, and better outcomes in general.38–40
Furthermore, although previous studies have shown higher hospital volumes to be associated with improved outcomes,41 the interaction between surgeon versus hospital volume and contribution of each to surgical outcome has less explored.42 High-volume hospitals have more specialized surgeons, better-staffed intensive care units, and a broader range of technology-based services and superior postoperative monitoring system that may not be available to smaller or lower-volume hospitals.16 Although, the interaction between hospitals and surgeons in the success of an operation is important, hospital volume is a stronger measure of quality than surgeon volume. For instance, if an experienced surgeon operates in a low-volume hospital with fewer resources, even if the immediate result is a success, lower quality postoperative care may jeopardize the success of the operation. However, a high-volume hospital can provide excellent support to low-volume surgeons. Consistent with previous research,43–45 our results indicated that high-volume surgeons at high-volume hospitals had the highest odds of success for free flap operations.
The main limitation of this study was the lack of data to control for the severity of patients’ conditions or complexity of the flap. Additionally, using large data we were only able to measure survival, major complications, and failure of the free flap operation. It is equally important to analyze the association between provider volume and degree of functionality and aesthetic aspects of the operation. Finally, owing to differences in culture and healthcare policies, some of our findings may not be applicable to the U.S. Regardless, using entire Taiwan’s national data, we were able to examine the association between provider’s volume (for both surgeons and hospitals, and their interactions) and free flap outcome on a national scale. Successful systems of care, especially for complex surgeries with relatively higher rate of failure elsewhere, should be thoroughly examined. That was our goal in this study.
Our findings were consistent with previous research on hospital volume and surgical outcome associations. Despite an already centralized system of care for free flap, higher volume hospitals were associated with better operational success rates. We found that surgeon experience and not case volume is positively associated with higher probability of free flap success. Finally, only high-volume surgeons who worked in high-volume hospitals were associated with higher rate of success for free flap compared with other potential combinations.
Supplementary Material
Table, Supplemental Digital Content 1. Overall Statistics for all Free Flap Operations in Chang Gung Memorial Hospital in 2012, INSERT LINK.
Table, Supplemental Digital Content 2. List of Free Flap Codes, INSERT LINK.
Table, Supplemental Digital Content 3. Algorithm for Free Flap Failure
Note: A free flap failure is defined by presence of any of the four conditions on the left + any of the two conditions on the right, INSERT LINK.
Table, Supplemental Digital Content 4. Generalized Linear Mixed Model for Probability of Success of Free Flap, 2001–2012 in Taiwan (Categorical Volume)†
†From Taiwan’s National Health Insurance Research Database 2001–2012
*Significantly at the 95% confidence interval, INSERT LINK.
Table, Supplemental Digital Content 5. Generalized Linear Mixed Model for Probability of Success of Free Flap, 2001–2012 in Taiwan (with Interaction Terms Between Hospital and Surgeon Volumes)†
†From Taiwan’s National Health Insurance Research Database 2001–2012
*Significantly at the 95% confidence interval, INSERT LINK.
Acknowledgments
Funding: This work was supported by the Plastic Surgery Foundation National Endowment for Plastic Surgery Grant (to Dr. Elham Mahmoudi), a Midcareer Investigator Award in Patient-Oriented Research from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (2 K24-AR053120-06) (to Dr. Kevin C. Chung), and The Integration and Maintenance Program of Health Information Application and Collaborative Research (to Drs. Ming-Huei Cheng and Chee Jen Chang) (CIRPD1D0032)
References
- 1.Luft HS, Bunker JP, Enthoven AC. Should operations be regionalized? The empirical relation between surgical volume and mortality. The New England journal of medicine. 1979;301(25):1364–1369. doi: 10.1056/NEJM197912203012503. [DOI] [PubMed] [Google Scholar]
- 2.Gordon TA, Bowman HM, Tielsch JM, Bass EB, Burleyson GP, Cameron JL. Statewide regionalization of pancreaticoduodenectomy and its effect on in-hospital mortality. Annals of surgery. 1998;228(1):71–78. doi: 10.1097/00000658-199807000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hannan EL, Racz M, Ryan TJ, et al. Coronary angioplasty volume-outcome relationships for hospitals and cardiologists. Jama. 1997;277(11):892–898. [PubMed] [Google Scholar]
- 4.Ihse I. The volume-outcome relationship in cancer surgery: a hard sell. Annals of surgery. 2003;238(6):777–781. doi: 10.1097/01.sla.0000098616.19622.af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jollis JG, Romano PS. Volume-outcome relationship in acute myocardial infarction: the balloon and the needle. Jama. 2000;284(24):3169–3171. doi: 10.1001/jama.284.24.3169. [DOI] [PubMed] [Google Scholar]
- 6.McDermott AM, Wall DM, Waters PS, et al. Surgeon and breast unit volume-outcome relationships in breast cancer surgery and treatment. Annals of surgery. 2013;258(5):808–813. doi: 10.1097/SLA.0b013e3182a66eb0. discussion 813–804. [DOI] [PubMed] [Google Scholar]
- 7.Moxey PW, Hofman D, Hinchliffe RJ, et al. Volume-outcome relationships in lower extremity arterial bypass surgery. Annals of surgery. 2012;256(6):1102–1107. doi: 10.1097/SLA.0b013e31825f01d1. [DOI] [PubMed] [Google Scholar]
- 8.Tuggle CT, Patel A, Broer N, Persing JA, Sosa JA, Au AF. Increased hospital volume is associated with improved outcomes following abdominal-based breast reconstruction. Journal of plastic surgery and hand surgery. 2014;48(6):382–388. doi: 10.3109/2000656X.2014.899241. [DOI] [PubMed] [Google Scholar]
- 9.Zevin B, Aggarwal R, Grantcharov TP. Volume-outcome association in bariatric surgery: a systematic review. Annals of surgery. 2012;256(1):60–71. doi: 10.1097/SLA.0b013e3182554c62. [DOI] [PubMed] [Google Scholar]
- 10.Mohan D, Rosengart MR, Farris C, Cohen E, Angus DC, Barnato AE. Assessing the feasibility of the American College of Surgeons’ benchmarks for the triage of trauma patients. Arch Surg. 2011;146(7):786–792. doi: 10.1001/archsurg.2011.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bewley BCaAF. Free flap monitoring: a review of the recent literature. Current Opinions Otolaryngol Head Neck Surg. 2015;23:393–398. doi: 10.1097/MOO.0000000000000189. [DOI] [PubMed] [Google Scholar]
- 12.Chang EI, Chang Eric I, MD, Soto-Miranda Miguel A, MD, Zhang Hong, PhD, Nosrati Naveed, MD, Ghali Shadi, MD, Chang David W., MD Evolution of Bilateral Free Flap Breast Reconstruction over 10 Years: Optimizing Outcomes and Comparison to Unilateral Reconstruction. Journal of Plastic and Reconstructive Surgery. 2015;135:946e–953e. doi: 10.1097/PRS.0000000000001233. [DOI] [PubMed] [Google Scholar]
- 13.Al-Dam A, Zrnc TA, Hanken H, et al. Outcome of microvascular free flaps in a high-volume training centre. J Craniomaxillofac Surg. 2014;42(7):1178–1183. doi: 10.1016/j.jcms.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 14.Tashiro J, Gerth DJ, Thaller SR. Pedicled Flap Reconstruction for Patients With Pressure Ulcers: Complications and Resource Utilization by Ulcer Site. JAMA surgery. 2015:1–2. doi: 10.1001/jamasurg.2015.3228. [DOI] [PubMed] [Google Scholar]
- 15.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. New England Journal of Medicine. 2002;346(15):1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 16.Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. New England Journal of Medicine. 2003;349(22):2117–2127. doi: 10.1056/NEJMsa035205. [DOI] [PubMed] [Google Scholar]
- 17.Carr WJ, Feldstein PJ. The relationship of cost to hospital size. Inquiry. 1967:45–65. [Google Scholar]
- 18.Dimick JB, Welch HG, Birkmeyer JD. Surgical mortality as an indicator of hospital quality: the problem with small sample size. JAMA : the journal of the American Medical Association. 2004;292(7):847–851. doi: 10.1001/jama.292.7.847. [DOI] [PubMed] [Google Scholar]
- 19.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Annals of internal medicine. 2002;137(6):511–520. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- 20.Birkmeyer JD, Finlayson SR, Tosteson AN, Sharp SM, Warshaw AL, Fisher ES. Effect of hospital volume on in-hospital mortality with pancreaticoduodenectomy. Surgery. 1999;125(3):250–256. [PubMed] [Google Scholar]
- 21.Dimick JB, Pronovost PJ, Cowan JA, Lipsett PA. Surgical volume and quality of care for esophageal resection: do high-volume hospitals have fewer complications? The Annals of thoracic surgery. 2003;75(2):337–341. doi: 10.1016/s0003-4975(02)04409-0. [DOI] [PubMed] [Google Scholar]
- 22.Wong CH, Wei FC. Microsurgical free flap in head and neck reconstruction. Head & neck. 2010;32(9):1236–1245. doi: 10.1002/hed.21284. [DOI] [PubMed] [Google Scholar]
- 23.Karp NS, Kasabian AK, Siebert JW, Eidelman Y, Colen S. Microvascular free-flap salvage of the diabetic foot: a 5-year experience. Plastic and reconstructive surgery. 1994;94(6):834–840. doi: 10.1097/00006534-199411000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Chen YJ, Chang JTC, Liao CT, et al. Head and neck cancer in the betel quid chewing area: recent advances in molecular carcinogenesis. Cancer science. 2008;99(8):1507–1514. doi: 10.1111/j.1349-7006.2008.00863.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jin-Li H, Yuan-Fu H. Technical efficiencies in large hospitals: A managerial perspective. International Journal of Management. 2004;21(4):506. [Google Scholar]
- 26.Cheng T-M. Reflections on the 20th anniversary of Taiwan’s single-payer national health insurance system. Health Affairs. 2015;34(3):502–510. doi: 10.1377/hlthaff.2014.1332. [DOI] [PubMed] [Google Scholar]
- 27.Chan W, Srinivasan J, Ramakrishnan V. Microsurgery training today and future. Journal of Plastic, Reconstructive & Aesthetic Surgery. 2010;63(6):1061–1063. doi: 10.1016/j.bjps.2009.11.038. [DOI] [PubMed] [Google Scholar]
- 28.Deek NFA, Lalonde DH. Fu-Chan Wei-Surgeon, Innovator, and Leader of the Legendary Chang Gung Microsurgery Center. Plastic and Reconstructive Surgery–Global Open. 2016 doi: 10.1097/GOX.0000000000001042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheng T-M. Taiwan’s new national health insurance program: genesis and experience so far. Health Affairs. 2003;22(3):61–76. doi: 10.1377/hlthaff.22.3.61. [DOI] [PubMed] [Google Scholar]
- 30.Wu T-Y, Majeed A, Kuo KN. An overview of the healthcare system in Taiwan. London journal of primary care. 2010;3(2):115–119. doi: 10.1080/17571472.2010.11493315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cheng S-H, Chen C-C, Chang W-L. Hospital response to a global budget program under universal health insurance in Taiwan. Health Policy. 2009;92(2):158–164. doi: 10.1016/j.healthpol.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 32.Hughes RG, Hunt SS, Luft HS. Effects of surgeon volume and hospital volume on quality of care in hospitals. Medical care. 1987:489–503. doi: 10.1097/00005650-198706000-00004. [DOI] [PubMed] [Google Scholar]
- 33.McArdle C, Hole D. Impact of variability among surgeons on postoperative morbidity and mortality and ultimate survival. Bmj. 1991;302(6791):1501–1505. doi: 10.1136/bmj.302.6791.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sosa JA, Bowman HM, Tielsch JM, Powe NR, Gordon TA, Udelsman R. The importance of surgeon experience for clinical and economic outcomes from thyroidectomy. Annals of surgery. 1998;228(3):320. doi: 10.1097/00000658-199809000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lambert PM, Morris H, Ochi S. Positive effect of surgical experience with implants on second-stage implant survival. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 1997;55(12 Suppl 5):12–18. doi: 10.1016/s0278-2391(16)31192-2. [DOI] [PubMed] [Google Scholar]
- 36.Lawton MT, Du R. Effect of the neurosurgeon’s surgical experience on outcomes from intraoperative aneurysmal rupture. Neurosurgery. 2005;57(1):9–15. doi: 10.1227/01.neu.0000163082.20941.ef. [DOI] [PubMed] [Google Scholar]
- 37.Schmidt CM, Turrini O, Parikh P, et al. Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Archives of surgery. 2010;145(7):634–640. doi: 10.1001/archsurg.2010.118. [DOI] [PubMed] [Google Scholar]
- 38.Klein EA, Bianco FJ, Serio AM, et al. Surgeon experience is strongly associated with biochemical recurrence after radical prostatectomy for all preoperative risk categories. The Journal of urology. 2008;179(6):2212–2217. doi: 10.1016/j.juro.2008.01.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mittendorf E, McHenry C. Complications and sequelae of thyroidectomy and an analysis of surgeon experience and outcome. Surgical technology international. 2003;12:152–157. [PubMed] [Google Scholar]
- 40.Witt PD, Wahlen JC, Marsh JL, Grames LM, Pilgram TK. The Effect of Surgeon Experience on Velopharyngeal Functional Outcome following Palatoplasty: Is There a Learning Curve? Plastic and reconstructive surgery. 1998;102(5):1375–1384. doi: 10.1097/00006534-199810000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Schrag D, Panageas KS, Riedel E, et al. Hospital and surgeon procedure volume as predictors of outcome following rectal cancer resection. Annals of surgery. 2002;236(5):583–592. doi: 10.1097/00000658-200211000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Harmon JW, Tang DG, Gordon TA, et al. Hospital volume can serve as a surrogate for surgeon volume for achieving excellent outcomes in colorectal resection. Annals of surgery. 1999;230(3):404. doi: 10.1097/00000658-199909000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Konety BR, Dhawan V, Allareddy V, Joslyn SA. Impact of hospital and surgeon volume on in-hospital mortality from radical cystectomy: data from the health care utilization project. The Journal of urology. 2005;173(5):1695–1700. doi: 10.1097/01.ju.0000154638.61621.03. [DOI] [PubMed] [Google Scholar]
- 44.Courcoulas A, Schuchert M, Gatti G, Luketich J. The relationship of surgeon and hospital volume to outcome after gastric bypass surgery in Pennsylvania: a 3-year summary. Surgery. 2003;134(4):613–621. doi: 10.1016/s0039-6060(03)00306-4. [DOI] [PubMed] [Google Scholar]
- 45.Ko CY, Chang JT, Chaudhry S, Kominski G. Are high-volume surgeons and hospitals the most important predictors of inhospital outcome for colon cancer resection? Surgery. 2002;132(2):268–273. doi: 10.1067/msy.2002.125721. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table, Supplemental Digital Content 1. Overall Statistics for all Free Flap Operations in Chang Gung Memorial Hospital in 2012, INSERT LINK.
Table, Supplemental Digital Content 2. List of Free Flap Codes, INSERT LINK.
Table, Supplemental Digital Content 3. Algorithm for Free Flap Failure
Note: A free flap failure is defined by presence of any of the four conditions on the left + any of the two conditions on the right, INSERT LINK.
Table, Supplemental Digital Content 4. Generalized Linear Mixed Model for Probability of Success of Free Flap, 2001–2012 in Taiwan (Categorical Volume)†
†From Taiwan’s National Health Insurance Research Database 2001–2012
*Significantly at the 95% confidence interval, INSERT LINK.
Table, Supplemental Digital Content 5. Generalized Linear Mixed Model for Probability of Success of Free Flap, 2001–2012 in Taiwan (with Interaction Terms Between Hospital and Surgeon Volumes)†
†From Taiwan’s National Health Insurance Research Database 2001–2012
*Significantly at the 95% confidence interval, INSERT LINK.