Abstract
A robust body of scientific evidence indicates that being embedded in high-quality close relationships and feeling socially connected to the people in your life is associated with decreased risk for all-cause mortality as well as a range of disease morbidities. Despite mounting evidence that the magnitude of these associations is comparable to many leading health determinants (that receive significant public health resources), government agencies, healthcare providers and associations, and public/private healthcare funders are slow to recognize human social relationships as either a health determinant or health risk marker in a manner that is comparable to other public health priorities. This article evaluates current evidence (on social relationships and health) according to criteria commonly used in determining public health priorities. The piece discusses challenges for reducing risk in this area and outlines an agenda for integrating social relationships into current public health priorities. Social Relationships and Public Health
“The secret of getting ahead is getting started.”
- Attributed to Mark Twain; remains unsourced
Broad-based epidemiological studies provide clear and compelling evidence that social relationship status and functioning predict an array of important health outcomes and risk for premature mortality (House, Landis, & Umberson, 1988; Holt-Lunstad, Smith & Layton, 2010; Sbarra, Law, & Portley, 2011; Robles, Slatcher, Trombello, & McGinn, 2014; Shor & Roelfs, 2015). There is also a rich literature documenting the potential mechanisms that connect relationships to health outcomes (e.g., Uchino, 2006). Academics in interdisciplinary fields (e.g., epidemiology, psychology, sociology) have known about these findings for decades, but this work and its implications have only recently begun to trickle into the discussions of major health organizations. Most notably, the World Health Organization (WHO) now lists “Social Support Networks” as a determinant of health (WHO, n.d.) and the United Kingdom (UK) Minister of Health has established loneliness as a health priority (UK Department for Work & Pensions, 2015). Despite these laudable efforts, social relationships remain notably missing from the lists of currently accepted determinants of health for most major U.S. government agencies, healthcare providers and associations, and public/private healthcare funders 1 (e.g., Centers for Disease Control [CDC], Healthy People 2020, American Heart Association), and largely unrecognized or underappreciated by the general public. These facts raise important questions: Why are social relationships not adequately acknowledged and what steps may be necessary to update national public health priorities in a manner that is more consistent with the empirical research in this area? This paper addresses these questions and outlines an agenda for integrating social relationships into current public health priorities moving forward.
Many people—from psychologists to public health officials— will assume that public health prioritization refers to large-scale interventions and/or social engineering that somehow legislates “better relationships” for all; understandably, this perspective may lead to reactance and concerns that any public health focus on social relationships is premature, naïve, or a form of unnecessary government involvement in matters of personal choice. However, quite simply, greater public health prioritization refers to directing “resources, time, and energy to those issues that are deemed most critical and practical to address” (CDC). Such resources can be directed toward education, basic and applied research, surveillance, containment and prevention efforts, public health policy, interventions, and even, if the data supports it, social engineering.
Criteria for Establishing Public Health Priorities
How are public health priorities established? With an increasing range of pressing health issues and limited resources, public and private health organizations must establish priorities according to an established method that is fair, reasonable, and relatively easy to calculate. Although a number of methods exist, this article relies on the Basic Priority Rating System (BPRS; Vilnius & Dandoy, 1990; CDC: Prioritizing Health Problems, 2013), which is consistent with the WHO’s Health Impact Assessment. The primary criteria used to prioritize public health concerns are the Size and Seriousness of the problem. According to these criteria, there is sufficient evidence to prioritize social relationships in public health. Of course, the body of evidence in this area is neither complete nor perfect—it is fraught with gaps in the literature, issues of multiple causality, and disappointing interventions. However, similar challenges exist for other behavioral risk factors that receive considerable public health prioritization including diet, physical activity, tobacco use, etc. Thus, despite these challenges, the analysis below articulates key evidence suggesting prioritization is both justified and necessary to improve public health.
Defining the Problem
When it comes to social relationships, what exactly is the problem? Having too few relationships? Lacking social contact, interaction, or perceived support? Being lonely? Lacking a close intimate partner or someone in the home to rely on in times of need? Having strained or unsupportive relationships? Even from this incomplete list, it is clear that the multi-factorial conceptualization and measurement of social relationships may be a barrier to prioritization.
One way to address this barrier is to define the problem as lacking social connection. The umbrella term social connection (or social connectedness) represents a multi-factorial construct that includes structural, functional, and qualitative aspects of social relationships (Table 1), all of which contribute to risk and protection. Epidemiological research generally focuses on the structural (e.g., social network size/density, marital status, living arrangements) or functional aspects of social relationships (e.g., received and perceived social support, perceived loneliness), and some work includes multi-dimensional approaches (i.e., a combination of structural and functional aspects; Berkman, Glass, Brissette, & Seeman, 2000). Further, researchers examine the positive and negative qualities of the relationships above and beyond the functions they serve (e.g., Robles et al., 2014). Importantly, measures in each of these domains independently predict morbidity and mortality; and, given weak correlations among them, each may influence health through different pathways (Cohen, Underwood, & Gottlieb, 2000). Thus, as an organizing construct, social connection encompasses the variety of ways we can connect to others socially— through physical, behavioral, social-cognitive, and emotional channels.
Table 1. Social Connection: Component Definitions and Effect on Reduced Risk for Mortality.
The extent to which an individual is socially connected takes a multifactorial approach including (1) connections to others via the existence of relationships and their roles; (2) a sense of connection that results from actual or perceived support or inclusion; and (3) the sense of connection to others that is based on positive and negative qualities.
| Domains | Measures and descriptions | Effect sizes based on meta-analytic data
|
||
|---|---|---|---|---|
| k | OR/HR | 95% CI | ||
| Structural | (1) The existence and interconnections among differing social ties and roles. | |||
| Marital Status: | ||||
| Married vs. Divorced | 1041 | 1.30 (HR) | 1.27, 1.49 | |
| Married vs. Widowhood | 1232 | 1.23 (HR) | 1.19, 1.28 | |
| Never Married | 963 | 1.24 (HR) | 1.19, 1.30 | |
| Social Networks | ||||
| network density or size, number of social contacts | 714 | 1.45 | 1.32, 1.59 | |
| Social Integration | ||||
| Participation in a broad range of social relationships; includes active engagement in a variety of social activities/relationships, and sense of communality and identification with one’s social roles. | 454 | 1.52 | 1.36, 1.69 | |
| Social Contact Frequency | 915 | 1.13 (HR) | ||
| Living Alone vs. living with others | ||||
| Living Alone vs. living with others | 256 | 1.32 | 1.14, 1.53 | |
| Social Isolation: | ||||
| Pervasive lack of social contact, communication, participation in social activities, or confidant | 146 | 1.29 | 1.06, 1.56 | |
|
| ||||
| Functional | (2) Functions provided or perceived to be available by social relationships | |||
| Received support: | ||||
| Self-reported receipt of emotional, informational, tangible, or belonging support. | 94 | 1.22 | 0.91, 1.63 | |
| Perceptions of social support: | ||||
| Perception of availability of emotional, informational, tangible, or belonging support if needed. | 734 | 1.35 | 1.22, 1.49 | |
| Perception of loneliness: | ||||
| Feelings of isolation, disconnectedness, and not belonging | 136 | 1.26 | 1.04, 1.53 | |
|
| ||||
| Quality | (3) Perceptions of positive and negative aspects of social relationships | |||
| Marital Quality: | ||||
| Subjective ratings of satisfaction, adjustment, cohesion in couples | 77 | 1.49 | 1.16, 1.94 | |
| Relationship Strain: | ||||
| Subjective ratings of conflict, distress, or ambivalence | - | - | - | |
|
| ||||
| Multi-Dimensional | Complex Measures of Social Integration: | |||
| A single measure that assesses multiple components of social integration such as marital status, network size and network participation. | 304 | 1.91 | 1.63, 2.23 | |
| Multiple measures obtained that assess more than one of the above conceptualizations. | 148 | 1.50 | 1.42, 1.59 | |
Note. k=number of studies. OR = odds ratio. HR=Hazards Ratio. Effect size =1 indicates no difference, > 1 indicates increased survival.
Shor, Roelfs, & Bougy (2012);
Holt-Lunstad, Smith, Baker, Harris, & Stephenson (2015);
Computed from Robles, Slatcher, Trombello, & McGinn (2014)
The Size of the Problem
To become a public health priority, an accurate estimate of the size of the problem is needed. What percentage of the population lacks social connection? Although precise prevalence estimates are difficult because of the multi-factorial nature of the construct, lack of social connection may be indicated in any of the domains outlined in Table 1. Relevant social indicators are regularly collected as part of census data. For example, more than a quarter of the US population (27%) lives alone, over half the U.S. adult population is unmarried, and 1 in 5 have never married (US Census Bureau, 2012). The divorce rate in the US continues to hover around 40% of first marriages (US Census Bureau, 2011). Although caution must be used in suggesting single, widowed, or divorced adults are less socially connected than those who are married, these structural dimensions provide robust indications of health risk, as does variability in relationship quality and perceptions of embeddedness within one’s community. Between 20% and 43% of U.S. adults over age 60 experience frequent or intense loneliness—higher than the prevalence of merely living alone (Perissinotto, Stijacic Cenzer, & Covinsky, 2012). Among married couples, 3 in 10 relationships are severely discordant (Whisman, Beach, & Snyder, 2008). In a now classic analysis, Putnam (2000) argued that social disconnection was a defining feature of contemporary American life, and recent analyses suggest that widespread smartphone use has diminished the quality of interpersonal exchanges, so much so that the problem of being alone together has emerged as a meaningful cultural reference (Turkle, 2011). At this juncture, the extant data indicates that social disconnection is highly prevalent; however, the full scope of the problem will remain unclear until public health surveillance systems begin tracking indictors of social disconnection in a systematic and representative way.
The Seriousness of the Problem
Higher public health prioritization also is given to more serious health issues. The seriousness is determined by the urgency, severity, and economic loss associated with the problem. When these criteria are applied, social connection demonstrates a level of seriousness comparable to other “leading health determinants,” and other social determinants of health (www.healthypeople.gov).
Urgency
Seriousness is influenced by whether the problem is getting worse or may get worse over time. The average size of core social networks has declined by one-third since 1985, and networks have become less diverse; they are less likely to include non-kin (Pew Research Center, 2009). Average household size has decreased and there has been 10% increase in single occupant households (US Census Bureau, 2011). Census data also reveal trends in decreased marriage rates, fewer children per household, and increased rates of childlessness (US Census Bureau, 2011). Taken together with an aging population, smaller families and greater mobility reduces the ability to draw upon familial sources of informal support in old age (Lafreniere et al, 2003; Rook, 2009). Decreased community involvement is evidenced by falling rates of volunteerism (US Department of Labor, Bureau of Statistics, 2016) and an increasing percentage of Americans reporting no religious affiliation (Pew Research Center, 2015). Given that the incidence of loneliness is known to increase with age (Dykstra, van Tilburg, & de Jong Gierveld, 2005), and that social (particularly friendship) networks shrink with age (Wrzus, Wagner, Hanel, & Neyer, 2013), the prevalence of loneliness is estimated to increase with increased population aging. Taken together, these trends suggest that Americans are becoming less socially connected.
Severity
Across measurement approaches (structural, functional, multi-dimensional), being socially connected is associated with a 50% reduced risk of early death (Holt-Lunstad, Smith & Layton, 2010), demonstrating that social disconnection is indeed a severe problem. Meta-analytic data for specific indicators of social connections and their effect on mortality risk are shown in Table 1. Although the relative effect varies across social indicators, there is a consistent and significant effect on mortality risk. Of note, measurement approaches that consider multiple aspects of relationships are the strongest predictors of mortality risk. These findings also account for potential confounds (e.g., age and initial health status), and thus also rule out reverse causality. Consistent across measurement approaches, gender, age, country of origin, those who are less socially connected are at greater risk for earlier mortality.
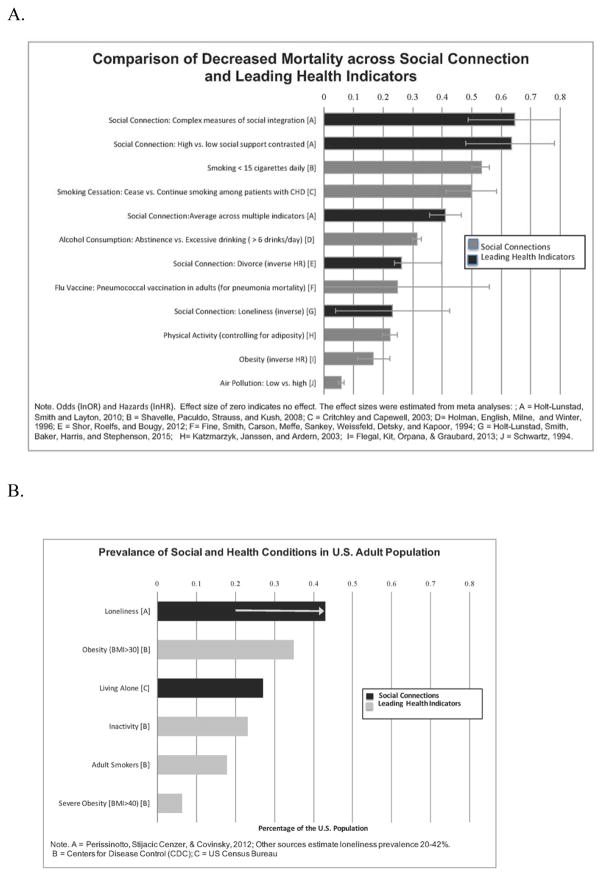
The effect of social relationships can be benchmarked against other well-established lifestyle risk factors. As shown in Figure 1a, the magnitude of effect of social connection on mortality risk is comparable, and in many cases exceeds, that of other well-accepted risk factors. Prevalence rates or the proportion of the population affected, are also comparable with well-established risk factors (Figure 1b). In evaluating these statistics, it is important to note that structural and functional measures are weakly correlated (20–30% shared variance) suggesting that (1) these measures tap into different aspects of relationships with potentially different pathways to health; (2) there may be a larger prevalence of those who lack social connectedness on at least one dimension; and, (3) those who lack social connectedness on multiple dimensions may carry greater risk. Thus, current estimates of severity are conservative and assessing the risk conferred by lack of social connections should be done in a multi-factorial manner.
Figure 1.
Benchmarking social connection with leading health indicators on (A) decreased odds for mortality; and (B) prevalence in the population.
Economic loss
Clearly, economics play a major role in determining how best to allocate limited resources. Despite the mixed success of social support interventions, both informal social support and programmatic interventions may be associated with economic benefits. For example, in addition to improving quality of life, total health care costs were significantly lower among breast cancer patients randomized to psychosocial support in addition to standard care compared to those who only received standard care (Arving, Brandberg, Feldman, Johansson, & Glimelius, 2014; Gillespie, O’Shea, Paul, O’Dowd, & Smith, 2012). Similarly, comprehensive postpartum social support interventions result in lower normal newborn readmission rates and lower costs (Barilla, Marshak, Anderson & Hopp, 2010). Considering informal social support, being more socially connected (higher family cohesion, martial status, and living with someone else) is associated with greater adherence to medical recommendations (DiMatteo, 2004), which result in better treatment outcomes and lowered medical costs. Importantly, social connections influence a number of health-relevant behaviors that are already widely recognized for their economic costs to the individual, family, and the broader health care system. However, large-scale estimates of the economic cost associated with lacking social connection are still needed.
Prioritization Summary
In sum, a significant portion of the US population lack social connections, which places them at greater risk for premature mortality and underlying morbidity—and the magnitude of this risk is comparable currently recognized leading health determinants. Importantly, although social relationships are closely related to existing health priorities (i.e., close relationships shape important health behaviors), most epidemiological evidence controls for these effects— suggesting that being socially connected contributes to risk independent of these other health determinants. Examining potential moderating factors (e.g., gender, age, country of origin) reveals remarkably consistent and widespread effects across the human population. Changes in US demographic trends further point to an exacerbation of social disconnection, suggesting an increasing urgency. Thus, based on these commonly accepted BPRS core criteria, there is sufficient evidence to support prioritizing social connection in public health.
Targeting Social Relationships to Promote Public Health
The CDC identifies “public health priorities with large-scale impact on health and known effective strategies to address them” as Winnable Battles (CDC, 2015). Currently, the list includes: Tobacco; Nutrition, Physical Activity and Obesity; Food Safety; Healthcare-Associated Infections; Motor Vehicle Injuries; Teen Pregnancy; and HIV. Does the evidence point to the need for adding “Social Connection” to the Winnable Battles list? There appear to be two criteria (1) a large-scale impact on health; and (2) known effective strategies to address the problem. As reviewed above, the data are quite clear that social relationships have a “large-scale impact on health.” Moreover, social relationships shape interpersonal interactions and intrapersonal experiences that alter health-relevant physiology across the lifespan (Hostinar, Sullivan, & Gunnar, 2014; Uchino, 2006) and provide a context for many important health behaviors, including other recognized health determinants (Umberson, Crosnoe, & Reczek, 2010). In this way, a public health focus on social relationships has the potential to make the CDC’s winnable battles more winnable. However, when considering whether social connections have “known effective strategies to address them” the data is mixed and less compelling, largely because attention remains relatively limited.
Drawing parallels to other established health priorities can help determine if the evidence warrants elevating social connection as a public health priority. Many of the Winnable Battles are multiply determined, and identifying modifiable causal pathways is often difficult; the gap between provocative observational science findings and the implementation of successful (experimental) interventions is large; early prevention is key for health promotion; and, ultimately, behavior change exists in an ecological context and must occur across multiple levels of analysis, from social policies to individual action. Moreover, lessons learned in more visible public health initiatives can be applied to the study of social connection. This section briefly discusses each of these topics and draws parallels to Nutrition, Physical activity, and Obesity as public health exemplars that help highlight ways forward. A key undercurrent of this analysis is that the challenges for elevating social connection as a public health priority are not wholly different from the challenges faced in advancing other currently identified winnable battles.
Multiply-determined Risk Factors
The CDC lists “Nutrition, Physical Activity, and Obesity” under a single umbrella heading as a winnable battle, and similar to social connection, these are inter-related constructs, each of which is independently linked to risk/protection. Obesity is the outcome of a series of health behaviors (poor nutrition and decreases in physical activity) that act in combination with a range of biological predispositions. Each risk factor is multiply determined and, ultimately, only some are potentially modifiable targets for public health intervention (Ebbeling, Pawlak, & Ludwig, 2002). For example, genetics and early life experience (e.g., undernutrition) can result in physiological changes that increase obesity. Furthermore, saturated and trans fat intake, refined carbohydrate consumption, portion size, and highly available “fast” and “junk” food are deeply intertwined with socio-cultural variables (e.g., food deserts; school lunches) that make the presence of high-calorie and nutritionally limited food intake more likely (Ebbeling et al., 2002). Thus, poor nutrition as a causal risk factor for obesity is multiply determined and some risk factors are largely immutable (e.g., early life experiences and genetics). Indeed, there is no single causal mechanism to easily intervene upon.
Social connection (low social integration, loneliness, and relational distress) is multiply determined as well. For example, the heritability of loneliness is roughly 40% (Goossens, van Roekel, Verhagan, et al., 2015) suggesting genetics play a large role in sensitivity to perceptions of social standing. Psychologically, there appear multiple pathways toward chronic loneliness, including intimate, relational, and collective loneliness, each of which attends to a different dimension of one’s social standing (Cacioppo, Grippo, London, et al., 2015). Social isolation may result from intrapersonal, behavioral, or environmental factors. From this brief analysis, it quickly becomes apparent a key task for elevating the status of social connection as a public health priority is demonstrating that a portion of these risk factors are modifiable and can be targeted for effective intervention; a growing literature indicates that this is indeed the case.
Identifying modifiable causal pathways
Identifying intervention targets to improve health via promoting and improving relationships has proven difficult (Cohen & Janicki-Deverts, 2009). Critical to this task is identifying causal risk factors that can be modified through targeted intervention (see Kraemer et al., 1997). Similar to obesity, some pathways may be more easily modifiable than others. Part of the difficulty is that as intervention targets, social relationships may appear too far upstream to exert causal effects on health-relevant physiology. Indeed, links between physical activity and health are easier to see because physical activity seems to influence health-relevant processes more directly. This perspective, however, relies on an outdated, dualistic mind-body model. Clear experimental evidence, particularly in animal models, shows that social connections are causally associated with health-relevant biological pathways at multiple levels from gene expression to neural functioning (Cacioppo et al., 2015).
One way to study causal effects of human relationships on health is to experimentally manipulate some aspect of social functioning in the laboratory, then track corresponding changes in cardiovascular, neuroendocrine or immune functioning (Hostinar, Sullivan, & Gunnar, 2014). The general finding is that the presence of a supportive person or even thinking about supportive others can attenuate cardiovascular and neuroendocrine responses to stress. A parallel line of work indicates social rejection has damaging effects for psychological and physical well-being through biologically plausible pathways (Slavich & Irwin, 2014). This line of experimental research is conceptually similar to the controlled laboratory research that contributed to and underpins current physical activity recommendations (Blair, LaMonte, & Nichaman, 2004).
Randomized controlled trials (RCTs)
To demonstrate that altering social relationships can ultimately improve health, RCTs are the gold standard (Cohen & Janicki-Deverts, 2009). A large meta-analysis of psychosocial interventions for chronic illness that target family relationships (Martire, Lustig, Schulz, Miller, & Helgeson, 2004) found small to moderate effects for depressive symptoms, but inconsistent effects on disease outcomes. A similar, yet more recent meta-analysis involving over 8,000 patients with chronic illness reported moderate effect sizes for both patients’ physical and mental health (Hartmann, Bäzner, Wild, Eisler, & Herzog, 2010). The pooled effect for family member interventions relative to treatment as usual reflect a 72–84% chance of improved mental or physical health compared to treatment as usual.
Given that social connection encompasses both the interpersonal and intrapersonal, “relationship interventions” can exist on many levels (see S. Cacioppo et al., 2015; Ickovics et al., 2011); however, current evidence is primarily restricted to individual, dyadic and group levels, with societal level interventions almost non-existent. This is important to note, given that efforts aimed at smoking and obesity treatment and prevention have been far more successful at a societal level than individual level approaches (e.g., Lemmens, Oenema, Knut, & Brug, 2008). Further, interventions that target one component of social connection (e.g., social isolation) may not be effective in reducing risk across components (e.g., perceived loneliness or relationship quality). Indeed, it is widely known within public health that effective intervention must operate across multiple levels of analysis in an integrated and systematic way (Glasgow, Vogt, & Boldes, 1998); such work is sorely needed in promoting social connection.
Because social relationships influence many different health-relevant pathways, attempts to reduce broader effects to a single causal pathway are shortsighted at best and ill informed at worst. Overall, the experimental research—from animal studies to human RCTs—is clear in demonstrating that several dimensions of social relationships can be targeted and altered; however, because of the mixed success of interventions it is also clear that additional work is needed to establish effective public health solutions. As the field grapples with these issues, one way forward in this area is to heed the lessons of prior intervention efforts.
From Observational Science to Intervention Science
Translating observational findings into interventions that can reliably prevent or lessen the risk is notoriously challenging in public health. Most causal chains in public health— especially around social determinants of health—are complex (Victoria, Habicht, & Bryce, 2004). For example, across numerous observational studies, greater physical activity shows a robust association with decreased cardiovascular mortality (Nocon, Hiemann, Müller-Riemenschneider, et al., 2008); yet, implementing successful physical activity interventions, especially with children and adolescents, has proven exceptionally difficult (Metcalf, Henley, & Wilkin, 2012). Given that translation and implementation difficulties bedevil many areas of public health intervention, how might the field proceed when it comes to the study of social connection? One approach is to study and distill useful lessons from past intervention efforts. The Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) study, for example, was a large RCT designed to increase perceived social support and treat depression following acute myocardial infarction (MI; Berkman et al., 2003). A major rationale for ENRICHD was correlational data demonstrating that the absence of social support was a risk factor for poor outcomes, including death, among patients with coronary heart disease. The trial randomly assigned over 2000 adults (within 6 months of a MI) to either usual care or cognitive behavioral therapy targeting depression and strengthening social network ties. Intervention patients reported increased social support and decreased depression compared to control patients, but the intervention failed to increase event-free survival (Berkman et al., 2003).
In retrospect, the ENRICHD trial was based largely on a top-down logic of building an intervention around correlational findings without first demonstrating that strengthening social network ties was causally tied to the clinical markers of interest in experimental studies. Systematic “bottom-up” approaches may be more ideal for relationship scientists interested in translating basic findings into interventions. For example, the Multiphase Optimization Strategy starts with conducting a series of well-planned experiments testing specific intervention components (Collins et al., 2011). Those experiments are followed by factorial designs combining different components, and the results inform development of a multi-component treatment that is built from the bottom-up based on basic research. Recent examples of experimental studies testing specific intervention components include work on friendship formation, relationship distress prevention, and social belonging (summarized in Walton, 2014).
Early Intervention and Prevention are Critical for Health Promotion
The US health system relies largely on tertiary prevention—i.e., interventions that reduce the worsening of existing morbidities, such as the ENRICHD trial. However, the importance of primary prevention and early intervention are increasingly recognized (Anderson, Shinn, Fullilove, et al., 2003), especially as the participants in the first early intervention studies reach adulthood. For example, the Carolina Abecedarian Project indicates that improving cognitive and social stimulation in early life (birth to age 5), and early intervention in school, reduces the likelihood of cardiovascular and metabolic diseases in the mid-30s (Campbell, Conti, Heckman, et al., 2014). Research on the prevention of childhood obesity via school-based interventions (promoting physical activity and improved diet) suggests that multi-faceted interventions lasting 1–4 years and involve parents can yield meaningful differences in children’s body mass (Sobol-Goldberg, Rabinowitz, & Gross, 2013). Although effect sizes are generally small (e.g., a standardized mean difference in BMI = −.076 for intervention relative to control group across > 50,000 children), major public health campaigns are designed around increasing physical activity in schools (see: www.letsmove.gov/schools). This point buttresses the notion that other areas of public health have a more developed evidence base and are thus riper for large-scale interventions than social connection. The available evidence does not support this conclusion.
One of the most robust early intervention programs to target social relationships (parenting) is the Nurse-Family Partnership (NFP) program. The NFP provides monthly nurse home visits to low-income and unmarried pregnant women from the prenatal period across the first two years of their children’s lives, is widely recognized to influence several important maternal and child outcomes, including reductions in child abuse and neglect (Coalition for Evidence-Based Policy, 2014). Importantly, the NFP suggests that targeting early social relationships (e.g., promoting parent-child bonding consistent with Attachment Theory) while bolstering the social support mothers receive from family and friends can have durable effects on both maternal and child health outcomes. Thus, a key lesson of the NFP is that theoretically-informed prevention programs that target social relationships directly can have considerable promise for promoting public health. Furthermore, when it comes to early intervention and prevention, the NFP and Abecedarian Project targeted at-risk groups suggesting that who is targeted may be as important as what is targeted.
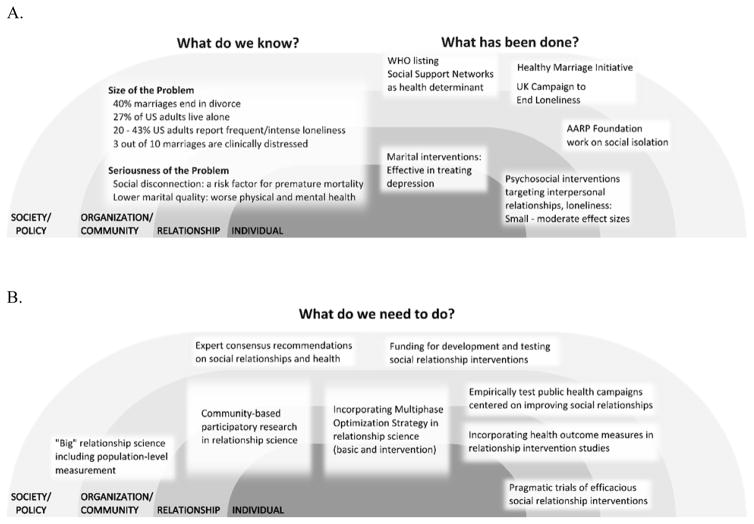
Ecological and Multilevel Models for Increasing Social Connections
For multiply-determined health behaviors, ecological models have the potential to integrate diverse theoretical perspectives, and this is certainly the case for multiple health risk factors, including physical activity (Bauman, Reis, Sallis, et al., 2012). This perspective “uses a comprehensive framework…, proposing that determinants at all levels—individual, social, environmental, and policy—are contributors. A key principle is that knowledge about all types of influence can inform development of multilevel interventions to offer the best chance of success” (p. 258, Bauman et al., 2012). From this perspective, large-scale intervention efforts that focus on a single level of analysis are likely to be hampered from the start. Figure 2A depicts the state of relationship and health science and attempts to translate that science, in the context of Bronfenbrenner’s social-ecological model of health that is frequently used by the CDC and other agencies to understand health determinants like violence, tobacco, and obesity (Sallis, Owen, & Fisher, 2008). The final section of the paper applies ecological thinking—which has proven successful in multiple area of public health—to make recommendations for elevating the status and study of social relationships within a public health framework.
Figure 2.
A) The state of relationships and health science embedded in a social ecological model. Text boxes are positioned in their respective levels of analysis (individual, relationship, organization/community, society/policy) and some boxes span multiple levels (i.e., individual and relationship). B) Recommendations for researchers, government agencies, health care providers and associations, and public/private health care funders to integrate social relationships into current public health priorities.
Recommendations and Future Policies
What objectives must be accomplished to achieve the overall goal of elevating social connections into the realm of a public health priority, and what specific resources and activities are needed to facilitate these objectives2? Continuing the analogy with nutrition/physical activity, the history of CDC efforts to address obesity (Dietz, 2015) provides a useful framework for identifying specific objectives for advancing social connection as a public health priority. Early efforts involved generating evidence-based recommendations, and implementing and improving surveillance that ultimately identified risk factors for poor health. Interventions became increasingly targeted to specific settings (schools, workplaces, communities). Throughout, coalitions were assembled at multiple levels, from local health departments to large non-profit foundations (e.g., Robert Wood Johnson Foundation) to government agencies (e.g., Institute of Medicine) to assemble the capability to mount large-scale policy and environmental changes.
Evidence-based Recommendations
Guidelines lay the foundation for goals, such as increasing the percentage of adults meeting physical activity guidelines from 43.5% to 47.9% in Healthy People 2020. Recommendations of specific levels of relationship quantity and quality would be naturally subject to criticism ranging from concerns about causality to public skepticism towards the social and behavioral sciences. Efforts to formulate recommendations for physical activity, which were primarily informed by prospective observational studies (whereas controlled intervention studies informed activity types and dose), faced and overcame similar challenges. Despite concerns about the validity of self-reported physical activity, and the multiple determining factors such as built environment and genetic factors (Blair et al., 2004), the first guidelines were released in 1975, with periodic revisions ever since (Haskell et al., 2007). For social connections and health, a similar consensus process (involving experts and stakeholders across disciplines) is needed to evaluate the literature and to make recommendations for the broader population and specific risk groups, all of which can be subject to periodic revision based on new evidence.
Surveillance: Toward a Social Connection “Risk Score”
Population-level surveillance serves three important functions: 1) determining progress towards goals; 2) developing “risk scores” that can be used to forecast risk of future problems; and 3) identifying at-risk populations based on demographics, health status, and location. Recent efforts to identify psychosocial “vital signs” for inclusion in electronic health records (EHRs; Institute of Medicine, 2014; Matthews, Adler, Forrest, & Stead, 2016) provide a template for selecting social connection measures. A multi-disciplinary committee evaluated several domains (social integration, social support, loneliness) and based on evidence and appropriateness for inclusion in all EHRs recommended the 4-item Berkman-Syme Social Network Index (Pantell et al., 2013). The measure received the same highest ratings on readiness and priority for inclusion in EHRs and usefulness for clinical, research, and population monitoring purposes as race/ethnicity, education, physical activity, tobacco use, and neighborhood characteristic measures. The same process could help identify measures in other domains, as brief scales assessing social connection-related constructs that are suitable for epidemiological studies are now available (Cyranowski et al., 2013; Hahn et al., 2010).
Accurately forecasting risk is critical for prevention efforts. For example, evidence-based “risk estimation scores” that incorporate multiple risk factors help guide cardiovascular disease (CVD) prevention and treatment. The Framingham risk score, European Society of Cardiology Systematic Coronary Risk Evaluation, and WHO/International Society of Hypertension scores are used by clinicians to predict the likelihood of a patient developing CVD over the next 10 years (reviewed in Goff, Lloyd-Jones, Bennett, et al., 2014). The scores incorporate clinical testing (total cholesterol, systolic blood pressure) and self-report information (age, gender, smoking status), and several have risk calculators available online. Similar efforts could be implemented with existing social epidemiology data, and would be greatly enhanced by population-level surveillance data (which notably, was not used to develop cardiovascular risk estimation scores). For readers skeptical that social connection data are useful for predicting health risk, a European Society of Cardiology task force reviewed the evidence for all purported CVD risk factors and recommended that psychosocial risk factors, including social isolation, should be assessed as a risk factor for future CVD (Authors/Task Force Members, Piepoli, Hoes, et al., 2016). Notably, the weight of evidence for psychosocial risk factors was (a) stronger than evidence for genetic testing and inflammatory biomarkers (neither were recommended), and (b) as strong as evidence for preclinical vascular damage assessments like carotid artery scanning.
Using big data to identify specific targets
Population surveillance, particularly when combined with “big data” from social media and smartphone apps, can help identify specific populations who may benefit from targeted interventions. Targeted interventions not only require knowing who is at risk in terms of demographics (age, gender, ethnicity, socioeconomic status) and/or health status, but where they are in terms of settings (school, work) and geographical location. At the same time, targeting requires adapting interventions for different cultures (for an example of failing to adapt, see Johnson, 2012; Campos & Kim, this volume). Such efforts, coupled with partnering with community stakeholders (advocacy groups, governmental agencies, etc.), can sharpen the focus of interventions (Sabir et al., 2009).
Assembling the Capability for Large-scale Changes
Partnering with community stakeholders allows for bridging gaps along the “pipeline” translating basic research to widespread practice (Glasgow, Green, Taylor, & Stange, 2012). Health settings are opportune environments to test and refine relationship interventions (Martire, this volume). Returning to obesity, building coalitions with non-profits resulted in funding and development of population-level interventions (e.g., community-based eating interventions supported by Kaiser Permanente), and partnerships that worked together on formulating policy recommendations (Dietz, 2015) and developing media campaigns. Such coalitions can also provide political capital needed to formulate and implement policy recommendations. For researchers, a key policy change will involve overcoming obstacles that impede large-scale funding for relationship science. One obstacle is funding priorities that focus on specific mental and physical health problems, rather than broad risk factors like social connection. Another hurdle is disappointing results from large intervention trials, including ENRICHD and the federal Healthy Marriages Initiative (large effectiveness trials of relationship education, reviewed in Johnson, 2012). The latter was considered “a major setback for the funding of such programs, regard for their efficacy…, and funding for future research” (p. 352, Lebow, 2013).
Combatting loneliness is a recent target for large-scale media campaigns (The Campaign to End Loneliness in older adults in the United Kingdom, Oprah Winfrey’s “Just Say Hello” campaign, and the AARP Foundation’s efforts to combat social isolation). Such campaigns have the potential to change behavior through several means, including changing cognitions and beliefs, helping people recognize unhealthy social norms, and recognize that positive emotions can come from changing behavior (Wakefield, Loken, & Hornik, 2010). Moreover, campaigns can increase the amount of discussion about the issue within social networks and may actually change social norms, leading to changes in behavior without necessarily changing individual attitudes or beliefs directly. As media campaigns are rolled-out to prevent isolation or loneliness, a critical step for sponsors (from local and national governments to non-profit community-service organizations) and scientists will be evaluating what works, in what contexts, and for whom. When it comes to media campaigns, and even health-oriented legislative changes, an obvious concern for prioritizing social connection is jumping to action ahead of the available data. Although such changes are laudable, meaningful public health benefits will only be realized when the existing intervention efforts—from individual-level changes to community and societal action—are deeply rooted in science and the pursuit of translatable research findings.
Conclusion
Humans need others to survive. Regardless of one’s sex, country or culture of origin, age or economic background, social connection is crucial to human development, health, and survival. The evidence (summarized in Figure 1 and 2A) supporting this contention is unequivocal. When considering the umbrella term of social connection and its constituent components, there are perhaps no other factors that can have such a large impact on both length and quality of life—from the cradle to the grave. Yet, social connection is largely ignored as a health determinant because public and private stakeholders are not entirely sure how to act. In addition, the pace of developing effective social relationship interventions is considerably slow; however, this is unlikely to change until social connection receive greater public health prioritization— in terms of both attention and resources.
Scientific progress is made through sustained efforts to find effective solutions, and the solutions for “how to act” are summarized in Figure 2B. Ultimately, to understand risk/protection, the causal mechanisms involved, and how to intervene to reduce risk and improve both physical and mental health, we must acknowledge influences (and conduct empirical research) at all levels of analysis. Just as we have come to better understand the factors that contribute to multifaceted public health problems ranging from violence to obesity, we must now consider the micro- (e.g., genetic markers of susceptibility, gene-environment interactions) to macro- (e.g., cultural norms, neighborhood characteristics) level processes through which social relationships influence physical health, as well as the pathways by which we may intervene to reduce risk and improve public health.
Supplementary Material
Biographies


Footnotes
Consistent with the WHO we view this as a global health priority; however, we focus primarily on public health prioritization in the United States
Readers with a public health background will recognize that the terms in this sentence come from a basic “logic model” used to depict the steps involved in planning, implementing, and improving public health programs (W. K. Kellogg Foundation, 2006).
Contributor Information
Julianne Holt-Lunstad, Brigham Young University.
Theodore Robles, University of California Los Angeles.
David A. Sbarra, University of Arizona.
References
- Anderson LM, Shinn C, Fullilove MT, Scrimshaw SC, Fielding JE, Normand J … Task Force on Community Preventive Services. The effectiveness of early childhood development programs - A systematic review. American Journal of Preventive Medicine. 2003;24(3):32–46. doi: 10.1016/s0749-3797(02)00655-4. [DOI] [PubMed] [Google Scholar]
- Arving C, Brandberg Y, Feldman I, Johansson B, Glimelius B. Cost-utility analysis of individual psychosocial support interventions for breast cancer patients in a randomized controlled study. Psycho-Oncology. 2014;23(3):251–258. doi: 10.1002/pon.3411. [DOI] [PubMed] [Google Scholar]
- Authors/Task Force Members. Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, … Verschuren WMM. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts). Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) European Journal of Preventive Cardiology. 2016;23:NP1–NP96. doi: 10.1177/2047487316653709. [DOI] [PubMed] [Google Scholar]
- Barilla D, Marshak HH, Anderson SE, Hopp JW. Can psychosocial support reduce newborn admissions? MCN: The American Journal Of Maternal/Child Nursing. 2010;35(1):33–39. doi: 10.1097/01.NMC.0000366808.75079.c. [DOI] [PubMed] [Google Scholar]
- Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJF, Martin BW. Correlates of physical activity: why are some people physically active and others not? The Lancet. 2012;380(9838):258–271. doi: 10.1016/S0140-6736(12)60735-1. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Blumenthal J, Burg M, Carney RM, Catellier D, Cowan MJ … Writing Committee, ENRICHD Investigators. Effects of treating depression and low-perceived social support on clinical events after myocardial infarction - The enhancing recovery in coronary heart disease patients (ENRICHD) randomized trial. Journal of the American Medical Association. 2003;289:3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Social Science & Medicine. 2000;51(6):843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- Blair SN, LaMonte MJ, Nichaman MZ. The evolution of physical activity recommendations: how much is enough? The American Journal of Clinical Nutrition. 2004;79(5):913S–920S. doi: 10.1093/ajcn/79.5.913S. [DOI] [PubMed] [Google Scholar]
- Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness Clinical Import and Interventions. Perspectives on Psychological Science. 2015;10(2):238–249. doi: 10.1177/1745691615570616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell F, Conti G, Heckman JJ, Moon SH, Pinto R, Pungello E, Pan Y. Early Childhood Investments Substantially Boost Adult Health. Science. 2014;343(6178):1478–1485. doi: 10.1126/science.1248429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos B, Kim HS. Culture, relationships and health: Incorporating the cultural diversity of family and close relationships into our understanding of health. American Psychologist. doi: 10.1037/amp0000122. under review. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Winnable battles. 2015 Retrieved from http://www.cdc.gov/winnablebattles/
- Centers for Disease Control and Prevention. Prioritization. APEXPH Assessment Protocol for Excellence in public Health. 2016 Retrieved from https://www.cdc.gov/nphpsp/documents/prioritization-section-from-apexph-inpractice.pdf.
- Coalition for Evidence-Based Policy. Top Tier Evidence Initiative: Evidence summary for the Nurse-Family Partnership. 2014 Retrieved from http://evidencebasedprograms.org/1366-2/nurse-family-partnership.
- Cohen S, Janicki-Deverts D. Can We Improve Our Physical Health by Altering Our Social Networks? Perspectives on Psychological Science. 2009;4(4):375–378. doi: 10.1111/j.1745-6924.2009.01141.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Underwood LG, Gottlieb BH. Social support measurement and intervention: A guide for health and social scientists. New York, NY, US: Oxford University Press; 2000. [Google Scholar]
- Collins LM, Baker TB, Mermelstein RJ, Piper ME, Jorenby DE, Smith SS, Christiansen BA, Schlam TR, Cook JW, Fiore MC. The multiphase optimization strategy for engineering effective tobacco use interventions. Annals of Behavioral Medicine. 2011;41:208–26. doi: 10.1007/s12160-010-9253-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyranowski JM, Zill N, Bode R, Butt Z, Kelly MAR, Pilkonis PA, … Cella D. Assessing social support, companionship, and distress: National institute of health (NIH) toolbox adult social relationship scales. Health Psychology. 2013;32(3):293–301. doi: 10.1037/a0028586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietz WH. The response of the US Centers for Disease Control and Prevention to the obesity epidemic. Annual Review of Public Health. 2015;36:575–596. doi: 10.1146/annurevpublhealth-031914-122415. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR. Social Support and Patient Adherence to Medical Treatment: A Meta-Analysis. Health Psychology. 2004;23(2):207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- Dykstra PA, van Tilburg TG, de Jong Gierveld J. Changes in Older Adult Loneliness: Results From a Seven-Year Longitudinal Study. Research on Aging. 2005;27(6):725–747. doi: 10.1177/0164027505279712. [DOI] [Google Scholar]
- Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. The Lancet. 2002;360:473–482. doi: 10.1016/S0140-6736(02)09678-2. [DOI] [PubMed] [Google Scholar]
- Gillespie P, O’Shea E, Paul G, O’Dowd T, Smith SM. Cost effectiveness of peer support for type 2 diabetes. International Journal Of Technology Assessment In Health Care. 2012;28(1):3–11. doi: 10.1017/S0266462311000663. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Green LW, Taylor MV, Stange KC. An Evidence Integration Triangle for Aligning Science with Policy and Practice. American Journal of Preventive Medicine. 2012;42(6):646–654. doi: 10.1016/j.amepre.2012.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. American Journal of Public Health. 1999;89:1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, … Wilson PWF. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Journal of the American College of Cardiology. 2014;63(25):2935–2959. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goossens L, van Roekel E, Verhagen M, Cacioppo JT, Cacioppo S, Maes M, Boomsma DI. The genetics of loneliness: Linking evolutionary theory to genome-wide genetics, epigenetics, and social science. Perspectives on Psychological Science. 2015;10:213–226. doi: 10.1177/1745691614564878. [DOI] [PubMed] [Google Scholar]
- Hahn EA, DeVellis RF, Bode RK, Garcia SF, Castel LD, Eisen SV & PROMIS Cooperative Group. Measuring social health in the patient-reported outcomes measurement information system (PROMIS): item bank development and testing. Quality of Life Research. 2010;19(7):1035–1044. doi: 10.1007/s11136-010-9654-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann M, Bäzner E, Wild B, Eisler I, Herzog W. Effects of interventions involving the family in the treatment of adult patients with chronic physical diseases: a meta-analysis. Psychotherapy and psychosomatics. 2010;79(3):136. doi: 10.1159/000286958. [DOI] [PubMed] [Google Scholar]
- Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, … Bauman A. Physical activity and public health - Updated recommendation for adults from the American college of sports medicine and the American heart association. Circulation. 2007;116(9):1081–1093. doi: 10.1161/circulationaha.107.185649. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. Plos Medicine. 2010;7(7):e1000316–e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar CE, Sullivan RM, Gunnar MR. Psychobiological mechanisms underlying the social buffering of the hypothalamic–pituitary–adrenocortical axis: A review of animal models and human studies across development. Psychological Bulletin. 2014;140(1):256–282. doi: 10.1037/a0032671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Capturing social and behavioral domains and measures in electronic health records: Phase 2. Washington, DC: 2014. [PubMed] [Google Scholar]
- Johnson MD. Healthy Marriage Initiatives On the Need for Empiricism in Policy Implementation. American Psychologist. 2012;67(4):296–308. doi: 10.1037/a0027743. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, Kupfer DJ. Coming to terms with the terms of risk. Archives of general psychiatry. 1997;54(4):337–343. doi: 10.1001/archpsyc.1997.01830160065009. [DOI] [PubMed] [Google Scholar]
- Lebow JL. Editorial: Programs for Strengthening Families. Family Process. 2013;52(3):351–354. doi: 10.1111/famp.12046. [DOI] [PubMed] [Google Scholar]
- Lemmens V, Oenema A, Knut IK, Brug J. Effectiveness of smoking cessation interventions among adults: a systematic review of reviews. European Journal of Cancer Prevention. 2008;17:535–544. doi: 10.1097/CEJ.0b013e3282f75e48. [DOI] [PubMed] [Google Scholar]
- Martire LM, Helgeson VS. under review. [Google Scholar]
- Martire LM, Lustig AP, Schulz R, Miller GE, Helgeson VS. Is it beneficial to involve a family member? A meta-analysis of psychosocial interventions for chronic illness. Health Psychology. 2004;23(6):599–611. doi: 10.1037/0278-6133.23.6.599. [DOI] [PubMed] [Google Scholar]
- Matthews KA, Adler NE, Forrest CB, Stead W. Collecting psychosocial “vital signs” in electronic health records: Why now? What are they? What’s new for psychology? American Psychologist. 2016;71:497–504. doi: 10.1037/a0040317. [DOI] [PubMed] [Google Scholar]
- Metcalf B, Henley W, Wilkin T. Effectiveness of intervention on physical activity of children: systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54) BMJ. 2012;345:e5888. doi: 10.1136/bmj.e5888. [DOI] [PubMed] [Google Scholar]
- Nocon M, Hiemann T, Müller-Riemenschneider F, Thalau F, Roll S, Willich SN. Association of physical activity with all-cause and cardiovascular mortality: a systematic review and meta-analysis. European Journal of Preventive Cardiology. 2008;15:239–246. doi: 10.1097/HJR.0b013e3282f55e09. [DOI] [PubMed] [Google Scholar]
- Pantell M, Rehkopf D, Jutte D, Syme SL, Balmes J, Adler N. Social Isolation: A Predictor of Mortality Comparable to Traditional Clinical Risk Factors. American Journal of Public Health. 2013;103(11):2056–2062. doi: 10.2105/ajph.2013.301261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Archives Of Internal Medicine. 2012;172(14):1078–1083. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center. America’s Changing Religious Landscape: Christians decline sharply as share of population; Unaffiliated and Other Faiths Continue to Grow. Pew Research Center; 2015. May 12, [Google Scholar]
- Pew Research Center. Social Isolation and New Technology. Pew Research Center; 2009. Nov 4, [Google Scholar]
- Putnam RD. Bowling alone: The collapse and revival of the American community. New York, NY: Simon & Schuster; 2000. [Google Scholar]
- Robles TF, Slatcher RB, Trombello JM, McGinn MM. Marital quality and health: A meta-analytic review. Psychological Bulletin. 2014;140(1):140–187. doi: 10.1037/a0031859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roelfs DJ, Shor E, Kalish R, Yogev T. The rising relative risk of mortality for singles: meta-analysis and meta-regression. American Journal Of Epidemiology. 2011;174(4):379–389. doi: 10.1093/aje/kwr111. [DOI] [PubMed] [Google Scholar]
- Rook KS. Gaps in social support resources in later life: An adaptational challenge in need of further research. Journal Of Social And Personal Relationships. 2009;26(1):103–112. doi: 10.1177/0265407509105525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabir M, Wethington T, Breckman R, Meador R, Reid MC, Pillemer K. A Community-Based Participatory Critique of Social Isolation Intervention Research for Community-Dwelling Older Adults. Journal of Applied Gerontology. 2009;28(2):218–234. doi: 10.1177/0733464808326004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. 4. San Francisco, CA: John Wiley & Sons, Inc; 2008. pp. 465–486. [Google Scholar]
- Sbarra DA, Law RW, Portley RM. Divorce and death: A meta-analysis and research agenda for clinical, social, and health psychology. Perspectives on Psychological Science. 2011;6(5):454–474. doi: 10.1177/1745691611414724. [DOI] [PubMed] [Google Scholar]
- Shor E, Roelfs DJ. Social contact frequency and all-cause mortality: A meta-analysis and meta-regression. Social Science & Medicine. 2015;128:76–86. doi: 10.1016/j.socscimed.2015.01.010. [DOI] [PubMed] [Google Scholar]
- Shor E, Roelfs DJ, Bugyi P, Schwartz JE. Meta-analysis of marital dissolution and mortality: Reevaluating the intersection of gender and age. Social Science & Medicine. 2012;75(1):46–59. doi: 10.1016/j.socscimed.2012.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich GM, Irwin MR. From stress to inflammation and major depressive disorder: A social signal transduction theory of depression. Psychological Bulletin. 2014;140:774–815. doi: 10.1037/a0035302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobol-Goldberg S, Rabinowitz J, Gross R. School-based obesity prevention programs: A meta-analysis of randomized controlled trials. Obesity. 2013;21(12):2422–2428. doi: 10.1002/oby.20515. [DOI] [PubMed] [Google Scholar]
- Turkle S. Alone together: why we expect more from technology and less from each other. New York, NY: Basic Books; 2011. [Google Scholar]
- Uchino BN. Social Support and Health: A Review of Physiological Processes Potentially Underlying Links to Disease Outcomes. Journal of Behavioral Medicine. 2006;29(4):377–387. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- Umberson D, Crosnoe R, Reczek C. Social relationships and health behavior across the life course. Annual Review Of Sociology. 2010:36139–159. doi: 10.1146/annurev-soc-070308-120011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau. Changing American Households. 2011. [Google Scholar]
- U. K. Department for Work & Pensions. 2010 to 2015 government policy: older people. 2015 Retrieved from https://www.gov.uk/government/publications/2010-to-2015-government-policy-older-people/2010-to-2015-government-policy-older-people.
- U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion. Healthy People 2020. from http://www.healthypeople.gov/ [PubMed]
- U.S. Department of Labor, Bureau of Statistics. http://www.bls.gov/news.release/volun.nr0.htm.
- Victoria CG, Habicht JP, Bryce J. Evidence-based public health: moving beyound randomized trials. American Journal of Public Health. 2004;94:400–405. doi: 10.2105/ajph.94.3.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilnius D, Dandoy S. A priority rating system for public health programs. Public Health Reports. 1990;105(5):463–470. [PMC free article] [PubMed] [Google Scholar]
- Wakefield MA, Loken B, Hornik RC. Use of mass media campaigns to change health behaviour. The Lancet. 2010;376(9748):1261–1271. doi: 10.1016/S0140-6736(10)60809-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton GM. The new science of wise psychological interventions. Current Directions in Psychological Science. 2014;23:73–82. doi: 10.1177/0963721413512856. [DOI] [Google Scholar]
- Whisman MA, Beach SRH, Snyder DK. Is marital discord taxonic and can taxonic status be assessed reliably? Results from a national, representative sample of married couples. Journal of Consulting and Clinical Psychology. 2008;76(5):745–755. doi: 10.1037/0022-006X.76.5.745. [DOI] [PubMed] [Google Scholar]
- W. K. Kellogg Foundation. W. K. Kellogg Foundation Logic Model development guide. 2006 Retrieved from https://www.wkkf.org/resource-directory/resource/2006/02/wk-kellogg-foundation-logic-model-development-guide.
- World Health Organization. The determinants of health. n.d Retrieved from http://www.who.int/hia/evidence/doh/en/
- Wrzus C, Wagner J, Hänel M, Neyer FJ. Social Network Changes and Life Events Across the Life Span: A Meta-Analysis. Psychological Bulletin. 2013;139(1):53–80. doi: 10.1037/a0028601. [DOI] [PubMed] [Google Scholar]
- Yang YC, Boen C, Gerken K, Li T, Schorpp K, Harris KM. Social relationships and physiological determinants of longevity across the human life span. Proceedings of the National Academy of Sciences. 2016;113:578–583. doi: 10.1073/pnas.1511085112. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.