Abstract
Emerging data suggest that during childhood, close family relationships can ameliorate the impact that adversity has on lifespan physical health. To explain this phenomenon, a developmental stress buffering model is proposed in which characteristics of family relationships including support, conflict, obligation, and parenting behaviors evolve and change from childhood to adolescence. Together, these characteristics govern whether childhood family relationships are on balance positive enough to fill a moderating role in which they mitigate the effects that childhood adversities have on physical health. The benefits of some family relationship characteristics are hypothesized to stay the same across childhood and adolescence (e.g., the importance of comfort and warmth from family relationships) whereas the benefits of other characteristics are hypothesized to change from childhood to adolescence (e.g., from a need for physical proximity to parents in early childhood to a need for parental availability in adolescence). In turn, close, positive family relationships in childhood operate via a variety of pathways, such as by reducing the impact that childhood stressors have on biological processes (e.g., inflammation) and on health behaviors that in turn can shape physical health over a lifetime.
The relationships that children and adolescents have early in life have important ramifications for health across the lifespan. In particular, family members (typically parents) remain the foundation for close, important relationships throughout childhood and adolescence (Smetana, Campione-Barr, & Metzger, 2006; Collins & Laursen, 2004). Emotionally significant, comforting relationships during childhood are linked to better physiological and health profiles in infancy, childhood, and adulthood (Gunnar, Brodersen, Nachmias, Buss, & Rigatuso, 1996; Maunder & Hunter, 2001). Conversely, conflictual or abusive relationships in childhood predict a host of adverse health outcomes across the lifecourse (Repetti, Taylor, & Seeman, 2002; Miller, Chen, & Parker, 2011). A number of excellent previous reviews (see below) have already covered the links between adverse family relationships and physical health, and as well have articulated models for how social support (e.g., from family members) may serve as a buffer that protects individuals from the negative health consequences of stress. The present article briefly provides an overview of these literatures in the next sections below, and then advances this literature by focusing on the need for incorporating a developmental perspective into the stress buffering model. In brief, this model proposes that characteristics of family relationships including support, conflict, obligation, and parenting behaviors evolve and change from childhood to adolescence. These characteristics, when considered in conjunction and as well, together with developmental needs, govern whether childhood family relationships are on balance positive enough to fill a moderating role in which they mitigate the effects that childhood adversities have on physical health.
Childhood Family Relationships and Physical Health: Main Effects
The previous literature on the main effects of childhood family relationships on health has convincingly demonstrated that a variety of adversities experienced during childhood are associated with a host of poor health outcomes later in life including greater risk of cardiovascular diseases, autoimmune conditions, respiratory diseases, and some cancers (Miller et al., 2011). The specific types of childhood relationship-oriented adversities linked to poor health include child emotional, physical, or sexual abuse, parent mental health and substance abuse problems, and parental divorce (Miller et al., 2011; Dong et al., 2004; Anda et al., 2009). One meta-analysis documented a .5 SD increase in risk across cardiovascular, respiratory, metabolic, autoimmune, and musculoskeletal conditions in adults abused as children compared to a control group (Wegman & Stetler, 2009). Another review documented adverse effects of marital conflict or divorce on a variety of child health outcomes, ranging from health status to physical symptoms, illnesses, injuries, and hospitalizations (Troxel & Matthews, 2004). In addition, a seminal paper by Repetti, Taylor and Seeman (2002) characterized ‘risky families’ (families with high conflict and aggression and cold, unsupportive, and neglectful relationships) as being more likely to have children with disruptions in stress-responsive biological systems, poorer health behaviors, and increased risk factors for chronic illnesses like heart disease (Repetti et al., 2002).
In terms of positive family characteristics, though there are fewer studies on main effects, there are some that support the notion of positive family characteristics being associated with better health. For example, in a retrospective study, higher levels of childhood parental emotional support were associated with fewer chronic conditions in adulthood (Shaw, Krause, Chatters, Connell, & Ingersoll-Dayton, 2004). Longitudinal studies of adolescents demonstrate that as perceived parental support increases, physical health symptoms (e.g., aches, coughs) decreased over time (Wickrama, Lorenz, & Conger, 1997). Another longitudinal study found that higher levels of parental caring in college-age adolescents predicted a lower likelihood of having cardiovascular disease, ulcers, and other chronic conditions 35 years later (Russek & Schwartz, 1997). In addition, studies that have examined relationship histories have found associations of positive childhood family relationships with lower levels of physiological risk (allostatic load) in adulthood (Singer & Ryff, 1999; Seeman, Singer, Ryff, Dienberg Love, & Levy-Storms, 2002).
How Would Childhood Family Relationships Alter Health Across the Lifespan?
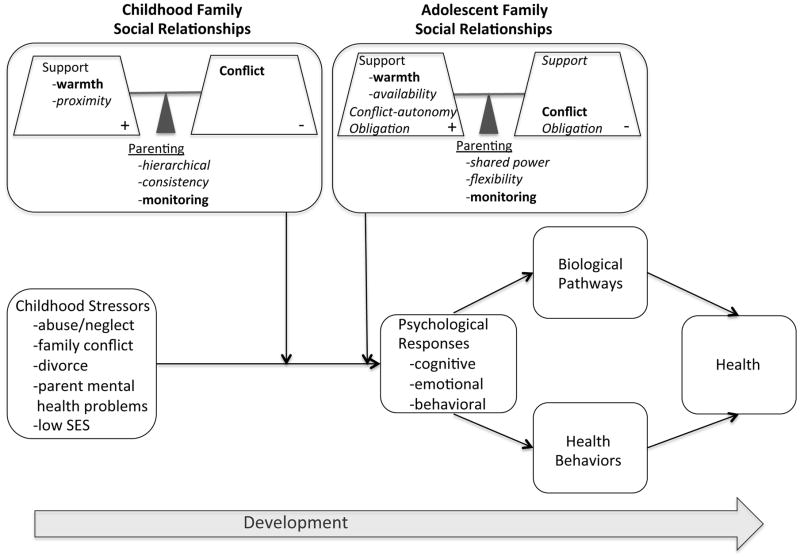
The above associations raise a challenging mechanistic question of explaining how family relationships experienced during childhood might continue to exert lasting effects on physical health decades later. In Figure 1, a typical stress-health model is depicted (horizontal row), in which stressors (external environmental demands) result in individual psychological responses that in turn have biological and health behavior effects, which over the long-term can have implications for physical health. Relevant to this article, stressors related to parent-child relationships elicit cognitive, emotional and behavioral responses in children. While there are a variety of specific psychological responses that might be elicited by stressful parent-child interactions, one illustrative example is where high levels of family conflict threaten children’s feelings of emotional security in the family (Cummings & Davies, 2002). Over time, this may lead to children developing difficulties with regulating their emotions, cognitively to the development of hostility and mistrust, and behaviorally to aggressive actions, all of which have implications for child psychopathology and physiological response systems (Cummings & Miller-Graf, 2015; El Sheikh & Harger, 2001). Also over time, lifespan models posit that as difficult parent-child interactions recur, they begin to create more pervasive interactional styles (with concomitant beliefs, emotions, and behaviors) that get perpetuated in how individuals interact with not only with parents, but also with peers and romantic partners into adulthood (Smith, Baron, & Grove, 2014; Shaver & Mikulincer, 2011; Ehrensaft, Knous-Westfall, & Cohen, 2011). Hence childhood relationships can also have implications for the nature of adult close relationships, which in turn have their own effects on adult health (Holt-Lunstad, Smith, & Layton, 2010; Kiecolt-Glaser & Newton, 2001).
Figure 1.
Figure 1 depicts the Developmental Stress Buffering Model. The main effects model (bottom row) depicts childhood stressors having an impact on lifespan health through psychological responses to stress and biological and health behavior pathways. The moderator model states that childhood family relationships can serve in a stress-buffering capacity, but an assessment of relationships has to balance both the positive and negative features of close relationships (hence the scales with +/− signs), and also has to acknowledge developmental changes in relationships. Here the importance of certain characteristics of family relationships is proposed to stay the same (bold), while others change in importance from childhood to adolescence (italics).
On the biological end, there are a number of ways in which childhood family stress may manifest biologically to create enduring physical health effects into adulthood. One model is a type of pathways model, by which short-term responses to stressful childhood family experiences impact intermediate psychological and biological precursors that in turn affect distal health outcomes into adulthood (Repetti, Robles, & Reynolds, 2011). For example, exposure to negative parenting, family conflict, and parent psychopathology are all associated with short-term changes in the release of the hormone cortisol; over time, patterns of cortisol release can become dysregulated (e.g., blunted in response to chronic stress; Miller, Chen, & Zhou, 2007), and this can alter outcomes such as allostatic load, a multi-system indicator of risk that is thought to reflect cumulative wear-and-tear on physiological systems, and that predicts risk for cardiovascular and other mortality (McEwen, 1998; Repetti et al., 2011). A second model - the biological embedding model - proposes that stress that occurs at specific points during development (such as early in childhood) can calibrate how physiological systems operate going forward in time (Miller et al., 2011; Miller & Chen, 2013; Hertzman, 1999). For example, stressors experienced early in life may program how certain cells of the immune system function and respond to threats, and this type of programming of biological systems may remain in place even if the stressor ends. Thus when a child experiences adversity early in life, their monocytes and macrophages (types of white blood cells) become calibrated to respond to future threats with a heightened pro-inflammatory phenotype (a potentially adaptive response in the face of a high degree of threats) – both by mounting more aggressive inflammatory responses to microbes and by developing an insensitivity to signals that normally turn off inflammatory responses. Over a lifetime, however, this pro-inflammatory phenotype results in a persistent state of low-grade inflammation that drives forward both disease mechanisms such as atherosclerosis (eventually contributing to the development of cardiovascular disease; Nathan & Ding, 2010) and allostatic load (McEwen, 1998).
In addition to inflammatory pathways, early life adversity may have effects on the activity of hormonal systems that regulate organs and tissues in the body (Gunnar & Quevedo, 2007; Lupien, McEwen, Gunnar, & Heim, 2009). For example, the hormone cortisol (released by the hypothalamic pituitary adrenal axis) is an important regulator of monocytes and macrophages, and at high doses conveys anti-inflammatory signals to these cells. However, upon repeated exposure to stress, these cells become less sensitive to cortisol signaling, which in turn allows chronic inflammatory states to persist (Miller, Cohen, & Ritchey, 2002; Miller et al., 2008). Cortisol also has effects on other biological systems that have implications for health, including the cardiovascular, metabolic, and neural systems (Sapolsky, Romero, & Munck, 2000). Similarly, the hormones epinephrine and norepinephrine (released by the sympathetic nervous system as part of the fight-or-flight response to threats) are known to upregulate the expression of pro-inflammatory genes in monocytes and macrophages (Cole et al., 2010). These hormones also have direct effects on cardiovascular, pulmonary, and other systems relevant to health (Gunnar & Quevedo, 2007; Wright, 2010).
Another biological hypothesis is that stressors experienced early in life ‘weather’ individuals’ physiological systems, resulting in a premature aging of cells, and eventually leading to a shortened life expectancy (this theory was first proposed with respect to racial disparities in health; Geronimus, Hicken, Keene, & Bound, 2006, but here it is applied to adversity experienced early in life when systems may be more vulnerable). Indications of premature aging of cells include telomere length (telomeres being repetitive DNA sequences that cap and protect the ends of chromosomes from DNA damage) and epigenetic aging (a measure derived from the DNA methylation profiles of cells, which reflects the disparity between an individual’s biological and chronological age). Childhood adversity has been associated with shorter telomere length and faster epigenetic aging in childhood, adolescence, and adulthood (here, because of the small number of studies on this topic, stressors outside of the realm of family stressors are also included, such as exposure to violence and discrimination in childhood; Shalev et al., 2013; O’Donovan et al., 2011; Brody, Miller, Yu, Beach, & Chen, 2016).
Yet another pathway is that childhood family relationships are important because they shape the health behaviors that children develop and learn early in life, which are important predictors of chronic diseases later in life. Parents serve as important role models and teachers of health promoting behaviors (Morrongiello, Corbett, & Bellissimo, 2008). Higher levels of parent support are associated with higher levels of adolescent physical activity (Raudsepp, 2006), and with less heavy drinking and drug use in adolescence (Barnes & Farrell, 1992). Conversely, adverse childhood relationships may serve as a source of stress and have been associated with riskier health behaviors into adulthood, including smoking, drug use, and alcohol dependence (Felitti et al., 1998). Thus if these types of health behaviors become ingrained early in life, this may represent another pathway by which childhood family relationships can impact health decades later.
Childhood Family Relationships and Health: Moderator Effects
Apart from the main effects of childhood family relationships on health, a number of researchers have also explored whether childhood family relationships may moderate relationships between childhood stress and health. That is, close, positive childhood family relationships may be important to health because they can help buffer children from the detrimental effects of adversities experienced early in life. One explanation for why social support would be beneficial to health is the stress-buffering theory, which states that social support operates during times of stress to mitigate the effects that stress has on health-related outcomes (via the biological and behavioral pathways outlined above), and hence that one would expect to see effects of social support during high stress, but not low stress, times (Cohen & Wills, 1985). A developmental perspective on this theory, in terms of what kinds of social support amidst stress might be most beneficial to health at different stages of childhood and adolescence, has not been well-articulated. Thus this article will first provide a brief overview of studies that address childhood family relationships moderating the effects of early life stress on health, and then discuss the developmental stress buffering model as a way to incorporate a more nuanced and developmentally informed perspective into stress buffering theories.
The section above on main effects focused on childhood stressors related to family relationship characteristics. In this section, however, because childhood family relationships are now the moderator of interest, studies of childhood stress that are broader than just family stressors are included (e.g., childhood poverty). A number of studies have examined whether positive childhood family relationships can buffer children or adults from the typical effects that stressors have on health. In infants, those who are securely attached are less likely to show elevations in cortisol during an acute stressor (e.g., laboratory stressor; Gunnar & Quevedo, 2007; Gunnar et al., 1996). Later in childhood, greater cumulative stressors (e.g., poverty, crowding) are associated with greater allostatic load among adolescents who experienced low maternal responsiveness, but not among those who experienced high maternal responsiveness (Evans, Kim, Ting, Tesher, & Shannis, 2007). Among older adolescents, greater increases in neighborhood poverty over time (stressor) were associated with higher allostatic load among adolescents who received low levels of emotional support (including from parents), but not among those who received high emotional support (Brody, Lei, Chen, & Miller, 2014). In addition, family support has been found to moderate effects of childhood stress (experiences of discrimination) on epigenetic aging among African American adolescents (Brody et al., 2016), and as well a parenting intervention was found to eliminate the relationship between unsupportive parenting (stressor) and telomere length in adolescents (Brody, Yu, Beach, & Philibert, 2015). In adulthood, childhood maternal warmth buffers the effects of a variety of childhood stressors including the effects of maltreatment on adult allostatic load (Carroll et al., 2013), the effects of low childhood socioeconomic status on adult genomic pro-inflammatory signalling profiles (Chen, Miller, Kobor, & Cole, 2011), and on adult metabolic profiles (Miller, Lachman, Chen, Gruenewald, & Seeman, 2011), and the effects of childhood parental loss on adult cardiovascular and cortisol acute stress responses (Luecken, Rodriguez, & Appelhans, 2005; Luecken, 1998).
How Do Children’s Relationship Needs Change Across Childhood and Adolescence?
The literature reviewed above has tended to characterize childhood family relationships along fairly static dimensions – that is, support and conflict being respectively good and bad for health. However, parent-child relationships evolve across childhood and adolescence. Children have different needs at different developmental stages, and so support and conflict may not just be good or bad, but rather one may need to consider how the characteristics of a relationship match with the needs of a child at a particular developmental stage, and how parent-child relationships change over time as children age. In some cases, the specific needs that children have for their parents may change from childhood to adolescence. In other cases, the change may come from the same parental behavior being relatively beneficial during one developmental period but relatively detrimental during another. Hence the developmental stress buffering model evolved with the goal of presenting a more nuanced view of the nature of parent-child relationships across childhood and adolescence. See Figure 1. Note that in this model, the idea of the changing value of different qualities of parent-child relationships at different developmental stages could apply to both the main effects and the moderator portions of the model.
Certain needs of children remain the same across childhood and adolescence, while others change as children develop. What remains the same about parent-child relationships throughout childhood and adolescence? For one, the importance of the relationship to both children and adolescents (Collins & Laursen, 2004). Throughout childhood, adolescence, and even into the college years, parents – primarily mothers – remain the most frequently identified primary attachment figure for youth, with friends or romantic partners mentioned only about ¼ as often as mothers even during the high school and college years (Rosenthal & Kobak, 2010). A second constant is the parent as a source of comfort during times of stress. Early in childhood, the parent as an attachment figure serves to comfort a child and reduce his/her distress (Bowlby, 1969). But even into adolescence, many youth report turning to parents during times of high stress (Steinberg, 1990). Children and adolescents who expect support to be available from parents in a predictable manner are more likely to seek it out when they experience a stressor (Davies, Winter, & Cicchetti, 2006). In addition, support from parents can help children and adolescents to develop more benign attributions when they experience stressful events (Dodge, Pettit, & Bates, 1994), which in turn reduces physiological responses to acute stressors (Chen, Langer, Raphaelson, & Matthews, 2004). A third constant is that parents serve as a source of external monitoring (parental behaviors involving attention to and tracking of children’s whereabouts and activities) throughout childhood and adolescence. In the early years, parental monitoring is necessary as a source of protection for children (Bowlby, 1969; Cassidy, 2008). But even as children mature, high levels of parental monitoring remain an important factor that predicts adolescent health behaviors such as drug use, as well as other behavioral problems (Steinberg & Silk, 2002).
If these needs remain constant, what, then, is different about the parent-child relationship across childhood and adolescence? Despite the importance of parental relationships, youth spend progressively less time with parents and more time with peers, and warmth and closeness with parents does decline during adolescence (Larson, Richards, Moneta, Holbeck, & Duckett, 1996). Thus in terms of what children need from their parents, the role of parents shifts from one that serves a need of proximity (a need to be physically close to a parent, often with distress upon separation) to one that serves a need of availability (the importance to an adolescent of knowing that a parent is available if they need them) (Kerns, 2008).
A second feature that shifts during adolescence is the meaning of conflict. One prominent feature of adolescence is the striving for increased autonomy (independence). This often can be accompanied by an increased intensity of conflict between parents and children during adolescence (Laursen, Coy, & Collins, 1998). However, in this case what may be changing is the utility of conflict. While some types of conflict will always be detrimental (e.g., emotional abuse), other types of conflict may serve as a normative part of child development, and a way for adolescents to achieve greater individuation from their parents (Smetana et al., 2006). In fact, secure attachment in adolescence is characterized by a combination of conflict over autonomy strivings balanced by behaviors aimed at maintaining relationships with parents (Allen, 2008). Thus although conflict may be distressing in the moment, during the adolescent period it may serve a purpose related to adolescent autonomy, and hence may have less negative repercussions for health than conflict during other periods.
Another shift that can occur is parent-child relationships changing from more hierarchical (with the parent being the one clearly in a position of power and the one establishing rules) to more shared-power relationships (greater amounts of joint parent-adolescent decision making) in adolescence (Collins & Laursen, 2004). The shift in parent-child relationships from more hierarchical to more of a shared-power model as children mature also means that parenting behaviors may need to change. In earlier years, more hierarchical relationships mean that consistency may be most important for children. Consistency encompasses the idea of both implementing predictable daily routines (day-to-day regularity in family practices and behaviors) as well as predictable responses to children’s behaviors (rules and punishments that stay the same across time and situations). In line with this idea, inconsistent parenting (punishing one time but not another for the same offense, often assessed together with harsh parenting) has been associated with greater inflammation and cortisol variability in youth (Miller, Brody, Yu, & Chen, 2014; Marceau et al., 2013). Conversely, predictable family routines have been found to buffer youth facing adversity (low socioeconomic status) from heightened inflammatory profiles (Schreier, Roy, Frimer, & Chen, 2014). While certain aspects of consistency (e.g., regarding punishments) likely have value throughout childhood and adolescence, the ability to demonstrate flexibility in parenting may become more important later in adolescence. Here, flexibility refers to the ability to adapt behaviors to an adolescent’s changing needs, to negotiate evolving rules, and to maintain open communication and cooperation. These qualities become important components of strong parent-adolescent bonds that may have implications for adolescent and adult health (Allen, 2008).
Finally, adolescence is also a period filled with increasing responsibility. For some adolescents, this involves obligations to the family that place the adolescent in more of an adult role – e.g., taking care of younger siblings, getting a job to contribute money to the family. These obligations represent a new dimension of parent-child relationships that comes online in adolescence, and they also represent a factor that may have both positive and negative features associated with it. On the one hand, having family obligations may be positive in providing adolescents with a sense of meaning and value, as well as increasing feelings of closeness with family members (Fuligni, Tseng, & Lam, 1999). On the other hand, obligations may be experienced as a burden among adolescents. These two facets are indicated by a daily diary study that revealed on the one hand, that greater time spent helping the family was associated with higher levels of inflammatory markers (e.g., C reactive protein) in adolescents (Fuligni et al., 2009), suggesting that obligations can be a burden. On the other hand, among those adolescents who found greater meaning (felt more fulfilled by their role as a son/daughter) levels of inflammatory markers were lower among those who spent more time helping family compared to those who spent comparable time helping family but with low levels of role fulfillment (Fuligni et al., 2009). On the other hand, feeling close to one’s family could increase the burden adolescents experience from family obligations. Adolescents who are close with their parents, for example, may feel greater pressure to contribute to the family and may experience greater competing demands between spending time assisting their family and spending time on their own academic goals or social pursuits. One study in support of this idea found that among those adolescents who had closer relationships with their families, more frequent family demands were associated a heightened pro-inflammatory profile (i.e., greater production of inflammatory cytokines in response to bacterial stimulation) (Levine, Hoffer, & Chen, under submission). Thus in the period of adolescence, greater closeness in family relationships may also have a cost in terms of the obligations and demands that come with that closeness, and these obligations may have both positive and negative aspects to them.
The above discussion focuses largely around how the relational needs of children and adolescents change by developmental stage. In addition, the quality of parent-child relationships may also be dynamic; that is, family relationships may not be able to be characterized as positive or negative during all of childhood (as many retrospective questionnaires suggest), but rather, may themselves change over time. Relationships that at one time are positive may become negative later on, or vice versa (perhaps depending on how the fit of child needs with parenting practices changes over time), or certain qualities of parent-child relationships may have both a simultaneously positive and negative side to them. As well, significant events (e.g., divorce) may change the family structure or dynamics and in turn shift the characteristics and quality of parent-child relationships over time.
A Developmental Stress Buffering Model
Tying together the literature above, a developmental stress buffering model for childhood family relationships and health is presented in this article (Figure 1). The model starts with the premise that childhood stressors have an impact on lifespan health via both biological and behavioral pathways (main effects). This association is present across the lifecourse (as indicated by the arrow labeled ‘development’). Close family relationships can serve in a stress-buffering capacity to mitigate this relationship during childhood and adolescence (moderator effects). However, an assessment of family relationships must balance the positive with the negative, and identify the particular constellation of family relationship characteristics that are beneficial during childhood and adolescence. This is potentially relevant to both the main effects and moderator effects in the model.
Figure 1 depicts both the idea of the balance of positive and negative features of close relationships, as well as of certain characteristics of family relationships staying the same (in bold), versus others changing from childhood to adolescence (in italics). Balance refers to the idea that both the positives and negatives within a relationship must be considered (hence the scales with +/− signs drawn in Figure 1) in order to determine whether that relationship can serve in a buffering capacity during times of stress. In childhood, the supportive aspects of family relationships are shown being balanced against the conflict experienced in the family. In adolescence, obligations are added to the model, and all three characteristics are drawn on both the positive and negative sides of the scale to illustrate the idea that these qualities may have both benefits and costs to them. For example, obligations may be beneficial in providing adolescents with a sense of meaning, but may be detrimental in creating a feeling of burden. Some types of conflict will be detrimental in adolescence, but other types may not be if they also help adolescents establish autonomy. The support portion of the scale in Figure 1 indicates multiple dimensions of support that should be assessed in childhood and adolescent family relationships, with certain aspects being hypothesized to stay the same across childhood and adolescence (e.g., the benefits of emotional warmth and comfort during distress), and other aspects being hypothesized to change (e.g., the need for physical proximity to parents vs. the need to know one’s parents are available if needed). In adolescence, support is generally beneficial but could also be perceived as stifling or overprotective as adolescents are working to establish autonomy, with implications for health problems such as somatic symptoms (Janssens, Oldehinkel, & Rosmalen, 2009).
In addition, in childhood, parenting is hypothesized to be most beneficial to health when it is consistent – that is, with established rules and routines that create stability and predictability in children’s lives. In adolescence, parenting is hypothesized to be beneficial when it is flexible – that is, when parents are able to adapt to adolescents’ evolving goals and autonomy desires by adjusting rules through open communication and mutual understanding. In contrast, high levels of monitoring are hypothesized to remain important and beneficial to children’s health throughout childhood and adolescence.
The idea behind the model in Figure 1 is that all of these aspects of support, conflict, obligation, and parenting are important to assess in childhood family relationships in order to determine the extent to which a particular relationship has the potential to mitigate the adverse effects of childhood stress on health. While the notion of supportive relationships is key to a buffering hypothesis, what constitutes developmentally appropriate expressions of support may change over time (heterotypic continuity; Conger & Donnellan, 2007).
Future research, then, will need to incorporate more nuanced measurements of childhood family relationships, which in turn may shed greater light on several issues. For example, when might supportive family relationships not be beneficial (e.g., if there is high conflict in addition to high support, or if high support comes along with high obligations during adolescence?). A developmental consideration of childhood family relationships may also shed light on why family relationships change over time and what the implications are for health. For example, certain family relationships may be beneficial at one time but not another across childhood and adolescence (e.g., if children’s needs evolve, but parenting approaches remain largely the same). Finally, developmental research could also illuminate whether certain types of family support operate through different pathways at different periods of development (e.g., high levels of parental monitoring might reduce the physiological consequences of stressors early in childhood but in adolescence have more of an impact on health behaviors).
Connecting the Developmental Stress Buffering Model to Previous Research
How does the developmental stress buffering model expand upon previous theories? In contrast to the original stress buffering model, the developmental stress buffering model postulates that support and conflict characteristics are not always good or bad but instead depend on developmental stage and context. For example, in certain families, emotional support and closeness may increase obligations and adult responsibilities in ways that create added burdens or stress on adolescents. Or support during adolescence that is accompanied by certain types of conflict may actually be better than support in the absence of conflict in terms of furthering autonomy goals, with implications for health behaviors and/or physiological profiles.
Other researchers have proposed the notion that both the positive and the negative sides of social relationships need to be considered simultaneously, though this has largely been from an adult perspective (Rook, 2015). For example, positive aspects of social relationships may buffer the negative aspects of social relationships (Brooks & Dunkel Schetter, 2011), or the experience of both positive and negative qualities within one relationship may be important. For example, Uchino et al. have demonstrated that having a greater number of ambivalent social ties (where relationships are characterized by both high positivity and high negativity) is associated with greater blood pressure reactivity during an acute stressor (Birmingham, Uchino, Smith, Light, & Sanbonmatsu, 2009). In addition, the relationship between more ambivalent ties and heightened inflammation (e.g., elevated C reactive protein levels) was found for family members, but not friends (Uchino et al., 2015). These studies have been conducted in adults, but have yet to be tested in the context of parent-child relationships.
In addition, previous theories have raised the notion that the same qualities may be beneficial in one context but detrimental in other contexts – for example, the differential susceptibility theory and the biological sensitivity to context theory, which raise the notion that some individuals are more susceptible to not only negative environments, but also to positive ones as well (Belsky & Pluess, 2009; Boyce & Ellis, 2005). These theories fit broadly with the developmental stress buffering model’s idea that certain characteristics of family relationships might be beneficial at one developmental stage but not another. However, the differential susceptibility and biological sensitivity models tend to focus more on how environmental impacts are moderated by individual characteristics (e.g., genetics, temperament, physiological reactivity), as opposed to relationship characteristics or developmental stages.
Previous theories also exist addressing the role that attachment plays in health. For example, inter-parental conflict has been theorized to alter parenting practices and threaten emotional security in the parent-child subsystem, resulting in a host of negative outcomes, such as internalizing and externalizing problems in children (Cummings & Davies, 2002). Insecure childhood relationships may also set the stage for adult avoidant and anxious/ambivalent relationships that in turn have implications for adult mental health and well-being (Mikulincer & Florian, 2003). These theories, however, have typically been framed as main effects models – that is, the idea that family conflict affects children’s emotional security, which then has implications for their mental or physical health. The developmental stress buffering model, in contrast, focuses on the role that positive, close childhood family relationships play in terms of buffering the effects that childhood stressful life experiences typically have on health. In addition, unlike theories built around attachment principles, which assume that children develop stable internal representations of their caregivers, this model emphasizes the dynamic nature of parent-child relationships, and how the optimal balance for health varies across development.
Future Research
A number of future research directions are important to articulate here. First is the idea of linking family intervention work to health. While numerous parenting interventions have been tested in the developmental literature, few have examined effects on health-related outcomes. Brody et al’s Strong African American Families parenting intervention is one of the few to have tested effects on pro-inflammatory cytokines, catecholamine levels, and telomere length in youth (Miller et al., 2014; Brody, Yu, Chen, & Miller, 2014; Brody, Yu, Beach, & Philibert, 2014). Fisher et al have documented effects of a parenting intervention for foster children on cortisol levels in children (Fisher, Gunnar, Chamberlain, & Reid, 2000). In addition, effects of a preventive intervention for divorced mothers and children were found for children’s cortisol reactivity to a laboratory stress task (Luecken et al., 2015). With intervention work being one of the only ways that causality can be established between childhood family relationships and health, additional future research is needed testing the potential health effects of other effective parenting programs, such as the Family Check-Up Program (Connell, Dishion, Yasui, & Kavanagh, 2007), the Triple P program (Positive Parenting Program) (Sanders, 2012), and the Incredible Years program (Webster-Stratton, 2005). In addition, prevention programs designed to promote coping in children of divorce (Luecken et al., 2015) and to help children navigate the loss of a parent (Sandler, Tien, & Ayers, 2016) could also potentially confer health benefits.
Second, longitudinal studies are critical for tracking the effects of family relationships on trajectories of biological and clinical health outcomes into adulthood so that there is not as much need to rely on retrospective accounts of childhood family relationships in health research and so that the impact of childhood family relationships on clinically meaningful health outcomes into adulthood can be assessed.
In addition, future research needs to take into account other factors related to family roles and family structure in the context of health. The first is the changing roles of fathers in family relationships. The vast majority of previous literature has focused on maternal characteristics such as maternal warmth. Yet, there have been dramatic shifts in the role of fathers across the twentieth century. For example, whereas fathers in 1965 spent ¼ of the time that mothers did engaged in child care, fathers in 2011 spent ½ the time that mothers did (Parker & Wang, 2013). 71% of children under 6 are eating dinners together with their fathers every day, which is fairly comparable to the 80% of children eating dinners together with their mothers every day (Bureau, 2010). These changing norms mean that it will be increasingly important for researchers to focus on the role of fathers as support buffers as well. For example, in previous research that has found a buffering role of maternal but not paternal warmth on adult health, is that because fathers increasingly play a different role in children’s lives today than they did several decades ago (and hence that in today’s generation of children, paternal warmth would have a similar buffering effect on children’s health), or is it because mothers and fathers serve different functions for their children and that fathers’ impact on children’s health would be evident in different ways?
Finally, the increasing complexity of family structures in today’s households needs to be better recognized in health research. Whereas two-parent, married, biological parents used to be the norm, today less than ½ of children grow up in this type of family structure (Carlson & Meyer, 2014). Instead, family units have become more complex over time, with dissolution of relationships, new relationships, and children from multiple relationships becoming more the norm (Andersson, 2002). This suggests that more and more children today have multiple parental figures in their lives. Research in health psychology needs to better acknowledge this complexity when measuring family relationships, and needs to understand how these multiple relationships affect child health. For example, does parental warmth that comes from a two parent family serve as a stronger or weaker buffer of children’s health compared to parental warmth that comes from a complex, blended family? On the one hand, parental warmth in a complex family environment might have less strong effects, as a parent’s attention and time is more limited by the multiple partners and children involved in a complex family environment. On the other hand, parental warmth in a complex family environment might have stronger effects if a child has multiple options of parents (or even older siblings that function as parents) to turn to during times of stress.
In sum, close, positive childhood family relationships can serve in a stress buffering role, much the same way that social relationships such as marital relationships do at other points in the lifecourse. However, what may be unique to the period of childhood and adolescence is the evolving nature of the parent-child relationship, and the ways in which parenting, support, conflict, and obligations may shift from childhood to adolescence, resulting in different factors across development contributing to high quality childhood family relationships that can help mitigate the effects that childhood stressors have on health across the lifecourse.
Acknowledgments
This article was supported by grants from the National Institute of Child Health and Human Development (R01 HD030588), National Heart, Lung, and Blood Institute (R01 HL108723, HL122328), and National Institute on Drug Abuse (P30 DA027827).
Contributor Information
Edith Chen, Northwestern University, Institute for Policy Research & Department of Psychology.
Gene H. Brody, University of Georgia, Center for Family Research, Institute for Behavioral Research
Gregory E. Miller, Northwestern University, Institute for Policy Research & Department of Psychology
References
- Allen JP. The attachment system in adolescence. In: Cassidy J, Shaver PR, editors. Handbook of Attachment (2nd edition) New York, NY: Guilford Press; 2008. pp. 419–435. [Google Scholar]
- Anda RF, Dong M, Brown DW, Felitti VJ, Giles WH, Perry GS, … Dube SR. The relationship of adverse childhood experiences to a history of premature death of family members. BMC Public Health. 2009;9:106. doi: 10.1186/1471-2458-9-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G. Children’s experience of family disruption and family formation: Evidence from 16 FFS countries. Demographic Research. 2002;7:343–364. [Google Scholar]
- Barnes GM, Farrell MP. Parental support and control as predictors of adolescent drinking, delinquency, and related problem behaviors. Journal of Marriage and Family. 1992;54:763–776. [Google Scholar]
- Belsky J, Pluess M. Beyond diathesis stress: differential susceptibility to environmental influences. Psychological Bulletin. 2009;135(6):885–908. doi: 10.1037/a0017376. [DOI] [PubMed] [Google Scholar]
- Birmingham W, Uchino BN, Smith TW, Light KC, Sanbonmatsu DM. Social ties and cardiovascular function: an examination of relationship positivity and negativity during stress. International Journal of Psychophysiology. 2009;74(2):114–119. doi: 10.1016/j.ijpsycho.2009.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss: Vol. 1. Attachment. New York, NY: Basic Books; 1969. [Google Scholar]
- Boyce WT, Ellis BJ. Biological sensitivity to context: I. An evolutionary-developmental theory of the origins and functions of stress reactivity. Development and Psychopathology. 2005;17(2):271–301. doi: 10.1017/s0954579405050145. [DOI] [PubMed] [Google Scholar]
- Brody GH, Yu T, Beach SRH, Philibert RA. Prevention ameliorates the prospective association between nonsupportive parenting and diminished telomere length. Prevention Science. 2014;16:171–180. doi: 10.1007/s11121-014-0474-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Lei MK, Chen E, Miller GE. Neighborhood poverty and allostatic load in African American youth. Pediatrics. 2014;134(5):e1362–e1368. doi: 10.1542/peds.2014-1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Miller GE, Yu T, Beach SR, Chen E. Supportive family environments ameliorate the link between racial discrimination and epigenetic aging: A replication across two longitudinal cohorts. Psychological Science. 2016;27(4):530–541. doi: 10.1177/0956797615626703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Yu T, Beach SR, Philibert RA. Prevention effects ameliorate the prospective association between nonsupportive parenting and diminished telomere length. Prevention Science. 2015;16(2):171–180. doi: 10.1007/s11121-014-0474-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Yu T, Chen E, Miller GE. Prevention moderates associations between family risks and youth catecholamine levels. Health Psychology. 2014;33(11):1435–1439. doi: 10.1037/hea0000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks KP, Dunkel Schetter C. Social negativity and health: Conceptual and measurement issues. Social and Personality Psychology Compass. 2011;5:904–918. [Google Scholar]
- Carlson M, Meyer D. Family complexity: Setting the context. Annals of the American Academy of Political and Social Science. 2014;654:6–11. [Google Scholar]
- Carroll JE, Gruenewald TL, Taylor SE, Janicki-Deverts D, Matthews KA, Seeman TE. Childhood abuse, parental warmth, and adult multisystem biological risk in the Coronary Artery Risk Development in Young Adults study. Proceedings of the National Academy of Sciences of the United States of America. 2013;110(42):17149–17153. doi: 10.1073/pnas.1315458110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy J. The nature of the child’s ties. In: Cassidy J, Shaver PR, editors. Handbook of Attachment. 2. New York, NY: Guilford Press; 2008. pp. 3–22. [Google Scholar]
- Chen E, Miller GE, Kobor MS, Cole SW. Maternal warmth buffers the effects of low early-life socioeconomic status on pro-inflammatory signaling in adulthood. Molecular Psychiatry. 2011;16(7):729–737. doi: 10.1038/mp.2010.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Langer DA, Raphaelson YE, Matthews KA. Socioeconomic status and health in adolescents: The role of stress interpretations. Child Development. 2004;75(4):1039–1052. doi: 10.1111/j.1467-8624.2004.00724.x. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Cole SW, Arevalo JM, Takahashi R, Sloan EK, Lutgendorf SK, Sood AK, … Seeman TE. Computational identification of gene-social environment interaction at the human IL6 locus. Proceedings of the National Academy of the Sciences of the United States of America. 2010;107(12):5681–5686. doi: 10.1073/pnas.0911515107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins WA, Laursen B. Parent-adolescent relationships and influences. In: Lerner RM, Steinberg L, editors. Handbook of adolescent psychology. 2. New York, NY: Wiley; 2004. pp. 331–361. [Google Scholar]
- Conger RD, Donnellan MB. An interactionist perspective on the socioeconomic context of human development. Annual Review of Psychology. 2007;58:175–199. doi: 10.1146/annurev.psych.58.110405.085551. [DOI] [PubMed] [Google Scholar]
- Connell AM, Dishion TJ, Yasui M, Kavanagh K. An adaptive approach to family intervention: linking engagement in family-centered intervention to reductions in adolescent problem behavior. Journal of Consulting and Clinical Psychology. 2007;75(4):568–579. doi: 10.1037/0022-006X.75.4.568. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Miller-Graf LE. Emotional Security Theory: An emerging theoretical model for youths’ psychological and physiological responses across multiple developmental contexts. Current Directions in Psychological Science. 2015;24:208–213. [Google Scholar]
- Cummings EM, Davies PT. Effects of marital conflict on children: recent advances and emerging themes in process-oriented research. Journal of Child Psychology and Psychiatry. 2002;43(1):31–63. doi: 10.1111/1469-7610.00003. [DOI] [PubMed] [Google Scholar]
- Davies PT, Winter MA, Cicchetti D. The implications of emotional security theory for understanding and treating childhood psychopathology. Development and Psychopathology. 2006;18(3):707–735. doi: 10.1017/s0954579406060354. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Pettit GS, Bates JE. Socialization mediators of the relation between socioeconomic status and child conduct problems. Child Development. 1994;65:649665. [PubMed] [Google Scholar]
- Dong MX, Giles WH, Felitti VJ, Dube SR, Williams JE, Chapman DP, Anda RF. Insights into causal pathways for ischemic heart disease: Adverse childhood experiences study. Circulation. 2004;110(13):1761–1766. doi: 10.1161/01.CIR.0000143074.54995.7F. [DOI] [PubMed] [Google Scholar]
- Ehrensaft MK, Knous-Westfall HM, Cohen P. Direct and indirect transmission of relationship functioning across generations. Journal of Family Psychology. 2011;25(6):942–952. doi: 10.1037/a0025606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Sheikh M, Harger J. Appraisals of marital conflict and children’s adjustment, health, and physiological reactivity. Developmental Psychology. 2001;37(6):875–885. [PubMed] [Google Scholar]
- Evans GW, Kim P, Ting AH, Tesher HB, Shannis D. Cumulative risk, maternal responsiveness, and allostatic load among young adolescents. Developmental Psychology. 2007;43(2):341–351. doi: 10.1037/0012-1649.43.2.341. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. American Journal of Preventive Medicine. 1998;14(4):245–245. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Fisher PA, Gunnar MR, Chamberlain P, Reid JB. Preventive intervention for maltreated preschool children: impact on children’s behavior, neuroendocrine activity, and foster parent functioning. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(11):1356–1364. doi: 10.1097/00004583-200011000-00009. [DOI] [PubMed] [Google Scholar]
- Fuligni AJ, Tseng V, Lam M. Attitudes toward family obligations among American adolescents with Asian, Latin American, and European backgrounds. Child Development. 1999;70:1030–1044. [Google Scholar]
- Fuligni AJ, Telzer EH, Bower J, Irwin MR, Kiang L, Cole SW. Daily family assistance and inflammation among adolescents from Latin American and European backgrounds. Brain, Behavior, and Immunity. 2009;23(6):803–809. doi: 10.1016/j.bbi.2009.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnar M, Quevedo K. The neurobiology of stress and development. Annual Review of Psychology. 2007;58:145–173. doi: 10.1146/annurev.psych.58.110405.085605. [DOI] [PubMed] [Google Scholar]
- Gunnar MR, Brodersen L, Nachmias M, Buss K, Rigatuso J. Stress reactivity and attachment security. Developmental Psychobiology. 1996;29(3):191–204. doi: 10.1002/(SICI)1098-2302(199604)29:3<191::AID-DEV1>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- Hertzman C. The biological embedding of early experience and its effects on health in adulthood. Annals of the New York Academy of Sciences. 1999;896:85–95. doi: 10.1111/j.1749-6632.1999.tb08107.x. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Medicine. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssens KA, Oldehinkel AJ, Rosmalen JG. Parental overprotection predicts the development of functional somatic symptoms in young adolescents. The Journal of Pediatrics. 2009;154(6):918–23e1. doi: 10.1016/j.jpeds.2008.12.023. [DOI] [PubMed] [Google Scholar]
- Kerns KA. Attachment in middle childhood. In: Cassidy J, Shaver PR, editors. Handbook of Attachment. 2. New York, NY: Guilford Press; 2008. pp. 366–382. [Google Scholar]
- Kiecolt-Glaser JK, Newton TL. Marriage and health: His and hers. Psychological Bulletin. 2001;127(4):472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Larson RW, Richards MH, Moneta G, Holbeck G, Duckett E. Changes in adolescents’ daily interactions with their families from ages 10–18: Disengagement and transformation. Developmental Psychology. 1996;32:744–754. [Google Scholar]
- Laursen B, Coy KC, Collins WA. Reconsidering changes in parent-child conflict across adolescence: a meta-analysis. Child Development. 1998;69(3):817–832. [PMC free article] [PubMed] [Google Scholar]
- Levine CS, Hoffer LC, Chen E. Moderators of the relationship between frequent family demands and inflammation. doi: 10.1037/hea0000469. (under submission) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luecken LJ. Childhood attachment and loss experiences affect adult cardiovascular and cortisol function. Psychosomatic Medicine. 1998;60(6):765–772. doi: 10.1097/00006842-199811000-00021. [DOI] [PubMed] [Google Scholar]
- Luecken LJ, Hagan MJ, Mahrer NE, Wolchik SA, Sandler IN, Tein JY. Effects of a prevention program for divorced families on youth cortisol reactivity 15 years later. Psychology & Health. 2015;30(7):751–769. doi: 10.1080/08870446.2014.983924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luecken LJ, Rodriguez AP, Appelhans BM. Cardiovascular stress responses in young adulthood associated with family-of-origin relationship experiences. Psychosomatic Medicine. 2005;67(4):514–521. doi: 10.1097/01.psy.0000160466.10397.18. [DOI] [PubMed] [Google Scholar]
- Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nature Reviews Neuroscience. 2009;10(6):434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- Marceau K, Ram N, Neiderhiser JM, Laurent HK, Shaw DS, Fisher P, … Leve LD. Disentangling the effects of genetic, prenatal and parenting influences on children’s cortisol variability. Stress. 2013;16(6):607–615. doi: 10.3109/10253890.2013.825766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder RG, Hunter JJ. Attachment and psychosomatic medicine: developmental contributions to stress and disease. Psychosomatic Medicine. 2001;63(4):556–567. doi: 10.1097/00006842-200107000-00006. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- Mikulincer M, Florian V. Attachment style and affect regulation: Implications for coping with stress and mental health. In: FGJO, Clark MS, editors. Blackwell Handbook of Social Psychology: Interpersonal Processes. Malden, MA: Blackwell Publishers; 2003. pp. 537–557. [Google Scholar]
- Miller GE, Brody GH, Yu T, Chen E. A family-oriented psychosocial intervention reduces inflammation in low-SES African American youth. Proceedings of the National Academy of Sciences. 2014;111:11287–11292. doi: 10.1073/pnas.1406578111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Lachman ME, Chen E, Gruenewald TL, Seeman TE. Pathways to resilience: Maternal nurturance as a buffer against childhood poverty’s effects on metabolic syndrome at midlife. Psychological Science. 2011;22:1591–1599. doi: 10.1177/0956797611419170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E. The biological residue of childhood poverty. Child Development Perspectives. 2013;7(2):67–73. doi: 10.1111/cdep.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychological Bulletin. 2011;137(6):959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Sze J, Marin T, Arevalo JM, Doll R, … Cole SW. A functional genomic fingerprint of chronic stress in humans: blunted glucocorticoid and increased NF-kappaB signaling. Biological Psychiatry. 2008;64(4):266–272. doi: 10.1016/j.biopsych.2008.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, Zhou E. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychological Bulletin. 2007;133:25–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- Miller GE, Cohen S, Ritchey AK. Chronic psychological stress and the regulation of pro-inflammatory cytokines: A glucocorticoid resistance model. Health Psychology. 2002;21:531–541. doi: 10.1037//0278-6133.21.6.531. [DOI] [PubMed] [Google Scholar]
- Morrongiello BA, Corbett M, Bellissimo A. “Do as I say, not as I do”: family influences on children’s safety and risk behaviors. Health Psychology. 2008;27(4):498–503. doi: 10.1037/0278-6133.27.4.498. [DOI] [PubMed] [Google Scholar]
- Nathan C, Ding A. Nonresolving inflammation. Cell. 2010;140(6):871–882. doi: 10.1016/j.cell.2010.02.029. [DOI] [PubMed] [Google Scholar]
- O’Donovan A, Epel E, Lin J, Wolkowitz O, Cohen B, Maguen S, … Neylan TC. Childhood trauma associated with short leukocyte telomere length in posttraumatic stress disorder. Biological Psychiatry. 2011;70(5):465–471. doi: 10.1016/j.biopsych.2011.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker K, Wang W. Modern parenthood: Roles of moms and dads converge as they balance work and family. Pew Research Center; 2013. www.pewresearch.org. [Google Scholar]
- Raudsepp L. The relationship between socio-economic status, parental support and adolescent physical activity. Acta Paediatrica. 2006;95(1):93–98. doi: 10.1080/08035250500323772. [DOI] [PubMed] [Google Scholar]
- Repetti RL, Robles TF, Reynolds B. Allostatic processes in the family. Development and Psychopathology. 2011;23(3):921–938. doi: 10.1017/S095457941100040X. [DOI] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, Seeman T. Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128:330–366. [PubMed] [Google Scholar]
- Rook KS. Social networks in later life: Weighing positive and negative effects on health and well-being. Current Directions in Psychological Science. 2015;24:45–51. doi: 10.1177/0963721414551364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal NL, Kobak R. Assessing Adolescents’ Attachment Hierarchies:Differences Across Developmental Periods and Associations With Individual Adaptation. Journal of Research on Adolescence. 2010;20(3):678–706. doi: 10.1111/j.1532-7795.2010.00655.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russek LG, Schwartz GE. Feelings of parental caring predict health statusin midlife: a 35-year follow-up of the Harvard Mastery of Stress Study. Journal of Behavioral Medicine. 1997;20(1):1–13. doi: 10.1023/a:1025525428213. [DOI] [PubMed] [Google Scholar]
- Sanders MR. Development, evaluation, and multinational dissemination of the triple P-Positive Parenting Program. Annual Review of Clinical Psychology. 2012;8:345–379. doi: 10.1146/annurev-clinpsy-032511-143104. [DOI] [PubMed] [Google Scholar]
- Sandler IN, Tien JY, Ayers SL. The effects of the Family Bereavement Program to reduce suicidal ideation and/or attempts of parentally bereaved children six and fifteen years later. Suicide and Life Threatening Behavior. 2016;46:S32–S38. doi: 10.1111/sltb.12256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocrine Reviews. 2000;21(1):55–89. doi: 10.1210/edrv.21.1.0389. [DOI] [PubMed] [Google Scholar]
- Schreier HM, Roy LB, Frimer LT, Chen E. Family chaos and adolescent inflammatory profiles: the moderating role of socioeconomic status. Psychosomatic Medicine. 2014;76(6):460–467. doi: 10.1097/PSY.0000000000000078. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Singer BH, Ryff CD, Dienberg Love G, Levy-Storms L. Social relationships, gender, and allostatic load across two age cohorts. Psychosomatic Medicine. 2002;64(3):395–406. doi: 10.1097/00006842-200205000-00004. [DOI] [PubMed] [Google Scholar]
- Shalev I, Moffitt TE, Sugden K, Williams B, Houts RM, Danese A, … Caspi A. Exposure to violence during childhood is associated with telomere erosion from 5 to 10 years of age: a longitudinal study. Molecular Psychiatry. 2013;18(5):576–581. doi: 10.1038/mp.2012.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaver PR, Mikulincer M. An attachment-theory framework for conceptualizing interpersonal behavior. In: Horowitz LM, Strack S, editors. Handbook of interpersonal psychology: Theory, research, assessment, and therapeutic interventions. Hoboken, NJ: Wiley; 2011. pp. 15–35. [Google Scholar]
- Shaw BA, Krause N, Chatters LM, Connell CM, Ingersoll-Dayton B. Emotional support from parents early in life, aging, and health. Psychology and Aging. 2004;19(1):4–12. doi: 10.1037/0882-7974.19.1.4. [DOI] [PubMed] [Google Scholar]
- Singer B, Ryff CD. Hierarchies of life histories and associated health risks. Annals of the New York Academy of Science. 1999;896:96–115. doi: 10.1111/j.1749-6632.1999.tb08108.x. [DOI] [PubMed] [Google Scholar]
- Smetana JG, Campione-Barr N, Metzger A. Adolescent development in interpersonal and societal contexts. Annual Review of Psychology. 2006;57:255–284. doi: 10.1146/annurev.psych.57.102904.190124. [DOI] [PubMed] [Google Scholar]
- Smith TW, Baron CE, Grove JL. Personality, emotional adjustment, and cardiovascular risk: marriage as a mechanism. Journal of Personality. 2014;82(6):502–514. doi: 10.1111/jopy.12074. [DOI] [PubMed] [Google Scholar]
- Steinberg L. Interdependency in the family: Autonomy, conflict, and harmony in the parent-adolescent relationship. In: Feldman SS, Elliott G, editors. At the Threshold: The Developing Adolescent. Cambridge, MA: Harvard University Press; 1990. pp. 255–276. [Google Scholar]
- Steinberg L, Silk J. Parenting adolescents. In: Bornstein MH, editor. Handbook of Parenting. 2. Mahwah, NJ: Erlbaum; 2002. pp. 103–133. [Google Scholar]
- Troxel WM, Matthews KA. What are the costs of marital conflict and dissolution to children’s physical health? Clinical Child and Family Psychology Review. 2004;7(1):29–57. doi: 10.1023/b:ccfp.0000020191.73542.b0. [DOI] [PubMed] [Google Scholar]
- Bureau USC. Facts for Features: Father’s Day Centennial: June 20, 2010. CB10-FF.11. Washington D.C: 2010. www.census.gov/newsroom/releases/pdf/cb10-ff11.pdf. [Google Scholar]
- Uchino BN, Ruiz JM, Smith TW, Smyth JM, Taylor DJ, Allison M, Ahn C. The Strength of Family Ties: Perceptions of Network Relationship Quality and Levels of C-Reactive Proteins in the North Texas Heart Study. Annals of Behavioral Medicine. 2015 doi: 10.1007/s12160-015-9699-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster-Stratton C. The Incredible Years: A trouble shooting guide for parents of children ages 2–8. Seattle, WA: Incredible Years; 2005. [Google Scholar]
- Wegman HL, Stetler C. A meta-analytic review of the effects of childhood abuse on medical outcomes in adulthood. Psychosomatic Medicine. 2009;71:805–812. doi: 10.1097/PSY.0b013e3181bb2b46. [DOI] [PubMed] [Google Scholar]
- Wickrama KA, Lorenz FO, Conger RD. Parental support and adolescent physical health status: a latent growth-curve analysis. Journal of Health and Social Behavior. 1997;38(2):149–163. [PubMed] [Google Scholar]
- Wright RJ. Perinatal stress and early life programming of lung structure and function. Biological Psychology. 2010;84(1):46–56. doi: 10.1016/j.biopsycho.2010.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]