Abstract
Purpose
To assess the specificity of simulation-based virtual reality ophthalmic cataract surgery training on the Eyesi ophthalmic virtual reality surgical simulator, and test the hypothesis that microsurgical motor learning is highly specific.
Methods
Retrospective educational interventional case series. The rates of vitreous loss and retained lens material, and vitreous loss and retained lens material associated with an errant continuous curvilinear capsulorhexis (CCC) were assessed among 1037 consecutive cataract surgeries performed during four consecutive academic years at a teaching hospital. The data were grouped by Eyesi use and capsulorhexis intensive training curriculum (CITC) completion. The main intervention was the completion of the CITC on the Eyesi.
Results
In the Eyesi simulator experience-based stratification, the vitreous loss rate was similar in each group (chi square p=0.95) and was not preceded by an errant CCC in 86.2% for “CITC done at least once”, 57.1% for “CITC not done, but some Eyesi use”, and 48.9% for “none” training groups (p=4×10−5). Retained lens material overall and occurring among the errant CCC cases was similar among training groups (p=0.82 and p=0.71, respectively).
Conclusions
Eyesi capsulorhexis training was not associated with lower vitreous loss rates overall. However, non-errant CCC associated vitreous loss was higher among those who underwent Eyesi capsulorhexis training. Training focused on the CCC portion of cataract surgery may not reduce vitreous loss unassociated with an errant CCC. It is likely that surgical training is highly specific to the task being trained. Residents may need to be trained for all surgical steps with adequate intensity to minimize overall complication rates.
INTRODUCTION
The optimal method for teaching surgery to residents remains elusive as teaching methods and efficiency continue to evolve. Currently, reported rates of posterior capsular rupture and vitreous loss range from 1.9% to more than 10%, a fairly large range for a serious cataract surgery complication.1–9 In an era of increasing accountability for outcomes and complications, maximizing resident surgical skill outside of the operating room prior to operating on patients is not just optimal, but necessary. Virtual reality ophthalmic surgical simulation technology, such as the Eyesi ophthalmic surgery simulator (VR Magic, Mannheim, Germany), is available at many ophthalmology teaching institutions and offers an opportunity to allow residents to get a large amount of practice, improve surgical skill and possibly improve surgical outcomes. Construct validity of the cataract surgery modules of the simulator has been established. 10–13 The value of the simulation surgical training on in-operating room performance on real patients continues to be demonstrated. 14–19
We have previously shown that Eyesi-based capsulorhexis training is associated with a dramatic improvement of operating room performance of capsulorhexes by ophthalmology residents.19 The effect of the capsulorhexis training on the rest of the cataract surgical procedure has not been previously assessed. It stands to reason that if the resident is trained to perform the capsulorhexis very well, the following surgical steps may also benefit from improved microsurgical skill acquired during capsulorhexis training, a phenomenon sometimes referred to as “cross training.” Collectively, the improved skill and lower errant capsulorhexis rates should result in lower vitreous loss rates, esp. since an errand capsulorhexis is considered to be a strong risk factor vitreous loss.
However, to date there is little understanding of the specificity or lack of specificity (i.e. cross training) of virtual reality cataract surgery training. In other words, it has not been clearly demonstrated whether or not cross training occurs when residents train certain steps of cataract surgery. Jonas and colleagues showed no significant difference between a group of novices trained on a virtual reality simulator and a group of novices not trained on the simulator when completing surgical task that were different than the training tasks in a wet lab on pig eyes. However they argue in their discussion that there was a trend toward trained novices performing better, and that a more powerful study would likely reveal a significant training effect.20 Similarly, Feldman and colleagues suggest that there may be crossover in skill development from one microsurgical skill to another, though in their study the results were not statistically significant.21 On the other hand, motor learning theory suggests that skill development is highly specific, and crossover to similar but different tasks might be limited.22
At this time, it is not understood whether training certain intraocular microsurgical steps, such as the CCC, results in an overall skill effect that increases performance on the whole surgery, i.e. other microsurgical steps, or reduces complications, for steps not specifically trained. Based on motor learning theory, previous work and our preliminary observations, we hypothesize that microsurgical motor learning is highly specific, and that limited skill crossover should be evident. In this study we aim to evaluate this hypothesis by assessing vitreous loss rates during cataract surgery performed by residents with different levels of virtual reality simulation training limited to the surgical step of CCC.
METHODS
The study was conducted in accordance with the United States Health Insurance Portability and Accountability Act (HIPAA) of 1996. The Investigational Review Board (IRB) of Harbor-UCLA Medical Center granted an exemption to mine an anonymized database used for an ongoing cataract surgery quality improvement project. The database contains data from all cataract surgeries performed at Harbor-UCLA Medical Center during the academic years beginning in the July of 2008. The data in the database was abstracted from the operative reports.
Data elements available in the quality improvement database and collected for the study included resident postgraduate year (PGY) level at time of surgery, academic year of surgery, attending name, capsulorhexis completions status, method of surgery, and whether vitreous loss and or retained lens material occurred. The capsulorhexis completion status was recorded as one of the following, CCC completed, attempted CCC that resulted in the attending taking over, radialization of the capsulorhexis, conversion to can-opener capsulorhexis. An errant CCC was defined as any of the three latter aforementioned conditions. Vitreous loss was defined to have occurred if the operative report clearly indicated that an anterior vitrectomy was done by any means (e.g., anterior vitrectomy pack opened and used, Wechsel sponge vitrectomy, etc.). The primary outcome measures for this study were the rate of vitreous loss stratified by Eyesi use. Secondary outcome measures were rate of retained lens material and rate of vitreous loss and retained lens material further sub-stratified by whether or not there was an errant CCC in the same case. Statistical analyses were performed using two sided Fisher’s exact test or Pearson’s chi square analysis.
As part of this study, the Eyesi ophthalmic microsurgical virtual reality simulator from VR Magic, Manheim, Germany with software versions 2.4, and 2.5 was used. CCC training was accomplished using the Capsulorhexis Intensive Training Curriculum (CITC) for the Eyesi, which was developed by the study author (CAM). 10 Cases in which the resident initiated the capsulorhexis can-opener style, planned non-phaco procedures, and cases that were aborted or cancelled for any reason before the capsulorhexis was initiated were excluded. The data were grouped based on the Eyesi training experience of the resident. Each resident was assigned to one of three categories of Eyesi use. (1) If the resident had not used the Eyesi, the assigned category was “None.” (2) Residents who completed the CITC at least once were categorized as “CITC done at least once”, and (3) the remainder of the residents were placed into an intermediate category of “CITC not done, but some Eyesi use.” It is important to note that the simulator experience other than the CITC was unstructured and without specific requirements, although the standard training modules and curricula from the manufacturer were available on the simulator and not readily accessible by the residents.
RESULTS
One thousand thirty-seven cataract surgeries met inclusion criteria during the study period and were included in the study. Cataract grade was available for 184 of the 1037 cases (17.7%). Brunescent or dense white cataracts were described in 115 of the 184 (62.5%) cases with a cataract description, representing 11% of the total case volume.
Thirty-eight residents performed surgery at Harbor UCLA Medical Center during the study period and met inclusion criteria. Fourteen residents did not use the Eyesi and performed 408 cataract surgeries, 4 residents used the Eyesi some but did not complete the CITC and performed 114 cataract surgeries, and 20 residents used the Eyesi, completed the CITC at least once and performed 515 cataract surgeries. Utilization of the Eyesi training other than the CITC were minimal in this cohort.
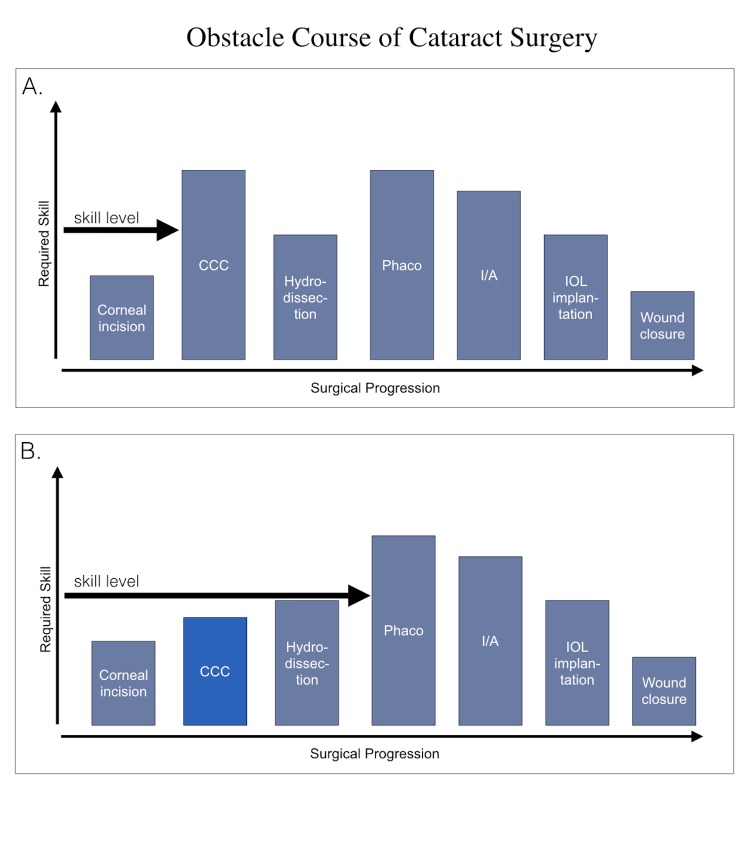
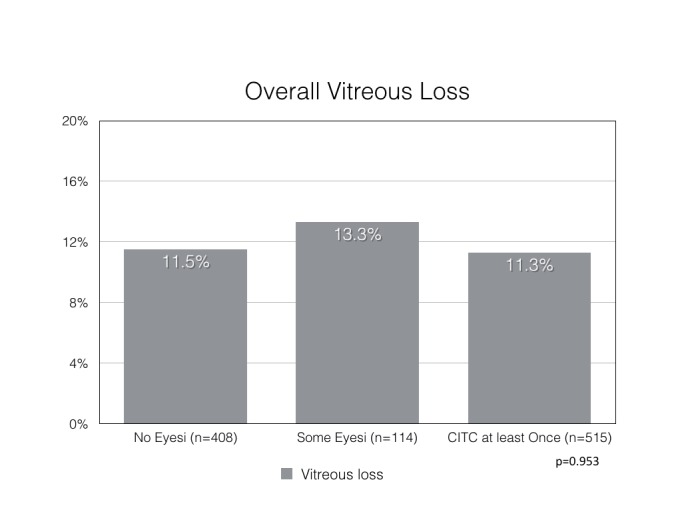
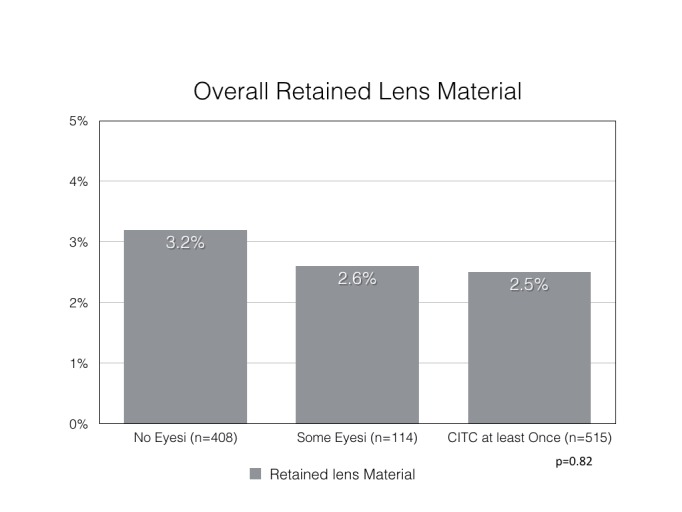
Vitreous loss occurred in 47 of 408 (11.5%) cases in the “No Eyesi” group, in 14 of 114 (13.3%) in the “CITC not done, but some Eyesi use” group, and 58 of 515 (11.3%) in the “CITC done at least once” group (p=0.953) (Figure 1). Retained lens material occurred in 13 of 408 (3.2%) cases in the “No Eyesi” group, in 3 of 114 (2.6%) in the “CITC not done, but some Eyesi use” group, and 13 of 515 (2.5%) in the “CITC done at least once” group (p=0.82)(Figure 2). Among cases of vitreous loss, a preceding errant CCC was occurred in 24 of 47 (51.1%) in the “No Eyesi” group, in 6 of 14 (42.9%) in the “CITC not done, but some Eyesi use” group, and 8 of 58 (13.8%) in the “CITC done at least once” group (p=0.00016)(Figure 3). Retained lens material occurred among the errant CCC cases in 4 of 55 (7.3%) cases in the “No Eyesi” group, in 2 of 14 (14%) in the “CITC not done, but some Eyesi use” group, and 3 of 31 (9.6%) in the “CITC done at least once” group (p=0.706) (Figure 4). Retained lens material occurred among vitreous loss cases in 12 of 47 (26%) cases in the “No Eyesi” group, in 3 of 14 (21%) in the “CITC not done, but some Eyesi use” group, and 12 of 58 (21%) in the “CITC done at least once” group (p=0.835) (Figure 5).
FIGURE 1.
Overall vitreous loss rates. Overall vitreous loss rate is stratified by Eyesi use. The chi square p-value is 0.958 demonstrating no difference in vitreous loss rates between stratification groups.#
FIGURE 2.
Overall retained lens material rate. Overall retained lens material rate is stratified by Eyesi use. The chi square p-value is 0.82 demonstrating no difference in vitreous loss rates between stratification groups.#
FIGURE 3.
Vitreous loss rate among errant CCC cases. The vitreous loss rates among errant CCC cases are stratified by Eyesi use. The stratification group “CITC done at least once” demonstrates significantly lower rate of vitreous loss associated with an errant CCC compared to the other two stratification groups (chi square p=0.00016).
FIGURE 4.
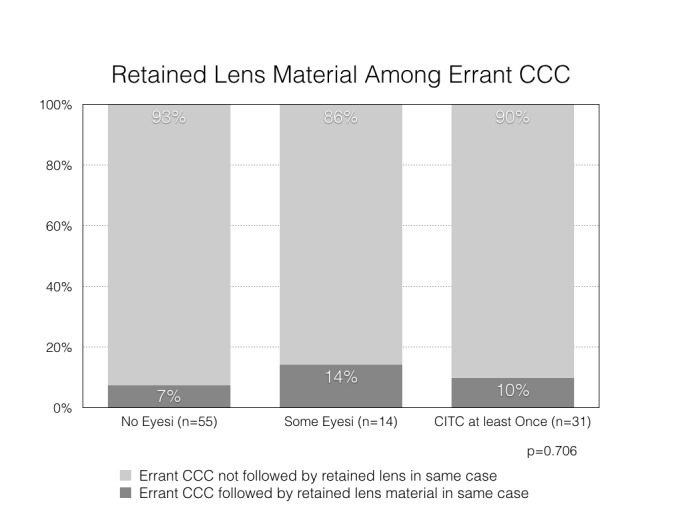
Retained lens material rate among errant CCC cases. The retained lens material rates among errant CCC cases are stratified by Eyesi use demonstrating no difference between stratification groups (chi square p=0.706).
FIGURE 5.
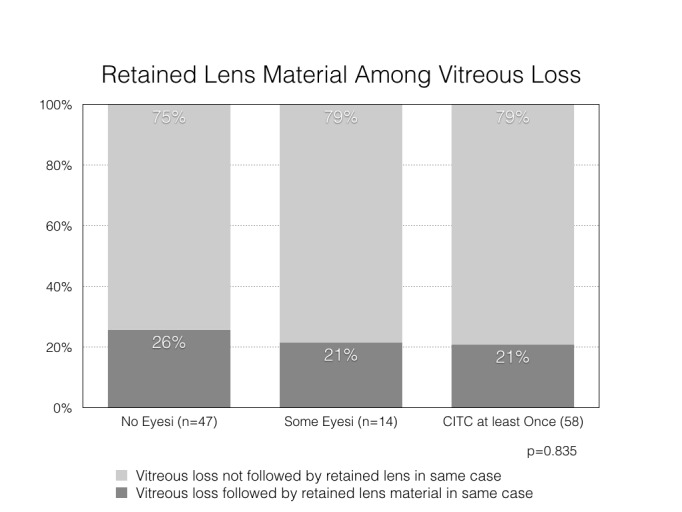
Retained lens material rate among vitreous loss cases. The retained lens material rates among vitreous loss cases are stratified by Eyesi use demonstrating no difference between stratification groups (chi square p=0.835).
DISCUSSION
Virtual reality surgical simulator training using the Eyesi and the CITC curriculum for the surgical step CCC resulted in a higher portion of vitreous loss to not be associated with an errant CCC, while the overall vitreous loss rates were similar between training groups. Furthermore, there was no difference in rates of retained nuclear material overall, among errant CCCs or vitreous loss cases. These data suggest that microsurgical motor learning is highly specific, and that limited skill crossover from CCC training to other surgical steps occurs; there is no evidence for the occurrence of cross training. Thus the hypothesis that limited or no crossover skill development occurs between training for microsurgical steps is supported.
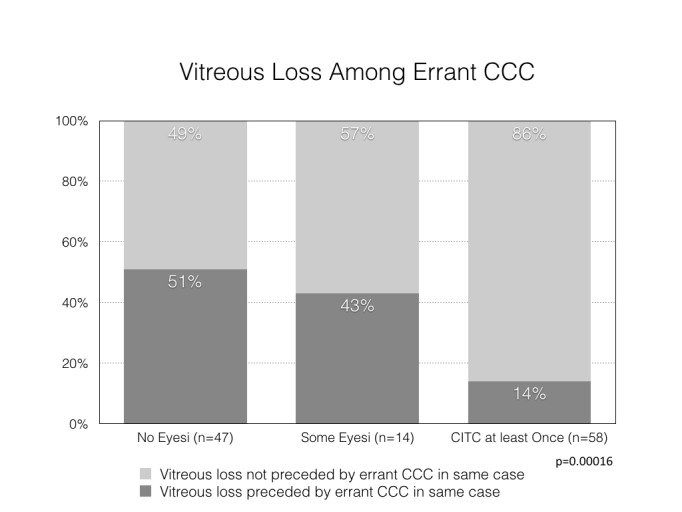
Unexpectedly, the proportion of vitreous loss unassociated with errant CCC increased among those trained with the CITC on the simulator. This finding may result from the lack of skill development of the surgical steps other than CCC due to the high specificity of the skill development. The intense focus on the CCC resulted in an insufficient focus on the other aspects surgical learning, such as practicing other steps with similar intensity. The possible reduction in relative difficulty of the CCC portion of cataract surgery, through CITC training on the Eyesi, resulted in the surgeons “passing the first hurdle” to “only trip up” later in the surgery (Figure 6). However, only if there is cross training achieved by CCC preparation to other steps could there be any expectation for the learning surgeon to perform at a higher level than untrained learners on other steps. Thus, as the surgery progresses, the learner encounters challenges for which s/he is not adequately prepared with a resultant complication rate higher than for the step they were specifically prepared for. I.e. the reduction in in errant CCCs did not result in lower vitreous loss rates because difficulty with other steps of the surgery became responsible for the vitreous loss which then cumulatively was no different than the learners that had not been similarly prepared for the CCC and had more vitreous loss associated with the errant CCC. Following this line of thought, if learners were similarly and intensively trained for each step of cataract surgery, an overall reduction in vitreous loss would be expected; relative difficulty of each step would be reduced, allowing for progression through all cataract surgery steps with a lesser chance of complications occurring.
FIGURE 6.
Panel A shows a theoretical “obstacle course of cataract surgery” with relative difficulties of the steps represented by the column height. The surgeon risks to fail (have complication) when the skill level is lower than the column height for a particular surgical step. Of note, the height of the columns do not represent a scientific measure of difficulty, but are varied for illustrative purpose only, to convey the idea of an obstacle course. Panel B shows the CCC column relatively lowered by virtue of skill development for the step, thus the relative difficulty decreases. The other columns remain at the same height as in this illustration there is the assumption that there is no skill development for the other steps of cataract surgery. As a result, the learner can pass over the CCC column but has a risk of failure (complication) as s/he passes along the path of surgery with inadequate skill to pass over the columns representing the other surgical steps.
Alternatively, it is possible that residents developing surgical skill or confidence, due to their mastery of the CCC, out of proportion to overall cataract surgery skill. In such a scenario, the learning surgeons may have approached the surgical steps following the CCC with more confidence than their skill justified, leading to higher complications at those subsequent steps. A proper awareness of such a possible phenomenon might have avoided complications during those surgical steps by fostering a more cautious approach.
The discovery of the probable specificity of microsurgical surgical training is very important to consider in surgical curriculum design. It is likely that all microsurgical steps must be specifically trained to achieve the best training results and shortest in-operating room learning curves for microsurgery, such as cataract surgery. Furthermore, this specificity of training likely extends to other microsurgical surgical procedures and fields, expanding it’s overall importance and it’s considerations’ impact on surgical training in general.
There are no other studies on simulation cataract surgery training that that have assessed training of a single surgical step, and attempted to assess the effect of such training on the overall cataract surgery skill development. There are several studies that report the impact of the Eyesi on surgical performance, but none to date have shown an overall significant reduction in complications, such as vitreous loss.14–19 However, in several studies phacoemulsification or operative times were shorter in in the simulation group. Belaya and colleagues showed significantly lower phacoemulsification times in the simulator-trained group compared to those trained conventionally.15 Pokroy and colleagues demonstrated shorter mean operative times for only operative cases 11–50 for simulator trained residents, and a higher percentage of long cases among non-simulator trained residents. When a greater number of cases for each resident were considered, there was no demonstrable difference.14 Thomsen and colleagues demonstrated a correlation between surgical experience, as measured by number of cases performed by the surgeon, and Eyesi scores on on various specific training modules.23
The science on motor learning suggests some possible explanations for the specificity of the CCC training. 22 If one considered all intraocular cataract surgery steps to be governed by a common generalized motor program (GMP) (memory of a sequence of movements), and the different steps of surgery are only variations, then the intense practice of the CCC should result in an overall improvement of skill for all steps. However, intense training of only a portion of the steps of cataract surgery might result in an “especial skill.”22,24–27 The especial skill is a highly refined skill among almost identical skills. This concept was first demonstrated with basketball players. The players were disproportionately skilled in throwing a basket from the free-throw distance compared to any other distance. Since most basketball players practice intensely throwing from the free-throw line, they develop an especial skill applicable to the exact distance of the free throw line to the basket within the generalized motor program of throwing a basket. Thus, when performing the especial skill, the performance is much better than the very similar skills, i.e. throwing a basket form a different distance. Another example might be typing username and password on a computer keyboard. Computer users can often type their username and password at typing speeds that far exceed their overall typing speed due the high frequency of repetition of typing those credentials. Analogously, practicing CCC might result in an especial skill of CCC within the generalized motor program of cataract surgery. However, with this theory, it would be expected that the skill of cataract surgery would improve overall, with the best improvement for the most practiced step, i.e. the CCC. Thus, it is unlikely that cataract surgery is governed by a single generalized motor program, as the CITC training appeared to only improve the CCC, and focusing training on the CITC resulted in more complications at other steps of surgery.
Alternatively, cataract surgery might be governed by a series of GMPs. The GMP for CCC would then be only one among the series of GMPs, i.e. there may be a GMP each for CCC, hydrodissection, phacoemulsification divide and conquer, phacoemulsification chopping, irrigation-aspiration, lens insertion etc. There would not be any expectation that a very different generalized motor program governing e.g. phacoemulsification, moving the phacoemulsification probe skillfully within the eye, would inherently be benefited from CCC training, using forceps in a careful and stereotypic manner in the anterior chamber; in other words there would be limited expectation of cross training or cross-over skill.
In the science of kinesiology, sports training and motor learning, it is widely understood that there is a great deal of specificity with regards to training and learning. This is in part derived from the aforementioned science of motor learning but also from physiological studies. 26–8 Much of modern sports training follows the principle of specificity, which essentially states that to become better at a particular exercise or skill, one must train that exact exercise or skill. And inversely, that cross training, or skill or endurance cross over, is limited by the specificity of the skill, movement, or endurance. For example, there is limited cross-over in skill and endurance from running to swimming, so for a triathlete to train running will not substantially improve the swim, and vice versa, though there may be some limited benefit from overall endurance improvement.29–31 Furthermore, even within a sport, e.g. swimming, training the swim stroke does not help the skill of jumping off the starting block optimally or sighting in open water swimming; the start and sighting must each be practiced separately and specifically.32 While in surgery some aspects important in sports, e.g. endurance and strength, are of far lesser importance, the specific muscle engagement and skill development required for each surgical step are very likely analogous to sports skills. Thus, it is plausible and very likely that the principle of specificity applies to surgery similarly as it does to sports, and motor learning in general.
An additional consideration might be the practice style. Different patterns of practicing or rehearsing, i.e. blocked versus random practice, may have an effect on motor learning.26 The completion of the CITC could be considered “blocked” practice. Blocked practice is said to occur when one skill is trained repetitively and exclusively, resulting in a high refinement of the GMP governing the specific skill, i.e. the circular tearing of the anterior capsule. This is considered to be very effective for early learning stages, but results in little crossover to similar motor tasks, and less adaptability than the alternative practice style referred to as random practice. In random practice, several generalized motor programs, or tasks, are trained in random sequence, e.g. a football player catching, throwing, and kicking in random order during practice session. Random practice is considered to result in high adaptability and skill crossover. Considering this information might also help explain why other portions of the cataract surgery had little or no benefit from the CCC training. Furthermore, it might be advisable to devise curricula that allow for random practice strategy once a minimum level of skill has developed. While such an approach is virtually impossible in an operating room environment, and at best very difficult in a wet lab, a simulator based surgical curriculum could easily be devised that allows for such an approach. Curricula with surgical steps in random order, including complication training, such as performing a “Little technique” to rescue a capsulorhexis,33 could result in a robust skill set not previously seen in beginning learners of cataract surgery.
It is important to note that the level of difficulty of cataract surgery cases in this particular healthcare setting may surpass the case complexity in many other settings. Brunescent or dense white cataracts were described in 115 of the 184 (62.5%) cases with a cataract description, and represented 11% of the total case volume. This suggests an overall high rate of advanced cataracts at this county hospital setting. Several studies have shown that very advanced cataracts are a risk factor for the development of cataract surgery complications, such as posterior capsular rupture and vitreous loss.34–37 Brazilikos and colleagues reported a 10% posterior capsular rupture rate among a series of 100 surgeries on dense white and brunescent cataracts.34 Similarly, Zare and colleagues report posterior capsular rupture rates of 14.5 to 16.4% for very advanced, such as dense white, cataracts. They also report a 5-fold higher complication rate among residents compared to attendings performing cataract surgery. 35
The main strength of this study is the relatively large number of residents studied, allowing for an adequate number of subjects in any one stratification group, either by academic year, or by Eyesi use experience. Also, the very challenging case mix and operative environment at the hospital where this study was conducted may have contributed to the risk of vitreous loss. This elevated challenge and risk may have provided an environment and opportunity to highlight differences in preparedness that a less challenging environment may not have.
Limitations of this study are several. The study is a cohort study that did not track all of the CCC training of residents, such as CCC training in the microsurgical practice laboratory as compared to the Eyesi training. Furthermore, in each stratification group, there are residents that contributed to both the PGY 3 and PGY 4 years, due to the nature of residency. Residents that contributed to both academic years’ data for stratification group may skew the data somewhat to those residents’ complication rates. It is possible that the residents with the least “surgical talent” spent the most time on the Eyesi performing the CITC. Such a situation could confound the results in that the “less talented surgeons” may have had more vitreous loss despite the CITC and because of their lesser intrinsic “surgical talent” and “more talented” residents may have not had the increase in vitreous loss despite lower rates of errant CCC. The relatively large number of residents studied would be expected to “dilute” out such theoretical confounder. Finally, improved performance due to subject knowledge that their results were being tracked in a quality improvement project may have played a confounding role (i.e. the Hawthorne effect).38 However, none of these limitations completely explain the findings in our report of a decline in vitreous loss associated with errant CCC, and an increase in vitreous loss not associated with an errant CCC among the residents that had the most intense simulator based CCC training. Thus it appears that the data may be representative for the intent of the study.
CONCLUSION
In conclusion, we offer support for the hypothesis that microsurgical motor learning is highly specific by demonstrating that intensive simulator CCC training using the CITC is not associated with decreased overall vitreous loss rates. However, vitreous loss associated with an errant capsulorhexis earlier in the case was lower among those residents that completed the CITC. The skills developed for CCCs do not seem to translate to other surgical steps as one might expect. There is a suggestion of surgeon over-confidence or too much attention to the CCC training task may explain higher complication rates during non-CCC portions of the surgery for those trained with the CITC. Thus, it is important that a robust curriculum for cataract surgery train all surgical steps adequately. Whether or not training modules other than the CITC achieve sufficient training effect remains to be demonstrated. The results of this report may be generalizable, and suggest that a group of learners only becomes good at what they are trained to become good at doing. Further research to more thoroughly determine the effects of simulation-based surgical training, and its specificity to the trained tasks compared to how much cross training occurs, may further improve understanding of the complexity of motor learning as it applies to cataract surgery teaching.
ACKNOWLEDGMENTS/DISCLOSURES
A. Funding/Support: Oppenheimer fund. Unrestricted grant form Research to Prevent Blindness, NY, NY, and the Jules Stein Eye Institute, Los Angeles, CA. The sponsors or funding organizations had no role in the design or conduct of this research.
B. Financial Disclosures: Dr. McCannel reports personal fees from Dutch Ophthalmic, grants from Genentech, personal fees from Santen, personal fees from Insight Instruments, outside the submitted work.
C. Contributions of Authors in each of these areas: All work was done by the study author.
D. Other Acknowledgments: The study author would like to acknowledge David C. Reed, MD, and Darin R. Goldman, MD who were residents at the UCLA’s Stein Eye Institute in Los Angeles, California and contributed to the data collection of the Quality Improvement database on which this study is based.
E. Conflict of interest: There are no conflicting relationships for the author
REFERENCES
- 1.Noecker RJ, Allinson RW, Snyder RW. Resident phacoemulsification experience using the in situ nuclear fracture technique. Ophthalmic Surg. 1994;25:216–221. [PubMed] [Google Scholar]
- 2.Tarbet KJ, Mamalis N, Theurer J, Jones BD, Olson RJ. Complications and results of phacoemulsification performed by residents. J Cataract Refract Surg. 1995;21:661–665. doi: 10.1016/s0886-3350(13)80562-7. [DOI] [PubMed] [Google Scholar]
- 3.Corey RP, Olson RJ. Surgical outcomes of cataract extractions performed by residents using phacoemulsification. J Cataract Refract Surg. 1998;24:66–72. doi: 10.1016/s0886-3350(98)80076-x. [DOI] [PubMed] [Google Scholar]
- 4.Blomquist PH, Rugwani RM. Visual outcomes after vitreous loss during cataract surgery performed by residents. J Cataract Refract Surg. 2002;28(5):847–52. doi: 10.1016/s0886-3350(01)01117-8. [DOI] [PubMed] [Google Scholar]
- 5.Tan JH, Karwatowski WS. Phacoemulsification cataract surgery and unplanned anterior vitrectomy--is it bad news?[see comment] Eye. 2002;16(2):117–20. doi: 10.1038/sj.eye.6700015. [DOI] [PubMed] [Google Scholar]
- 6.Chan FM, Mathur R, Ku JJ, et al. Short-term outcomes in eyes with posterior capsule rupture during cataract surgery. J Cataract Refract Surg. 2003;29(3):537–41. doi: 10.1016/s0886-3350(02)01622-x. [DOI] [PubMed] [Google Scholar]
- 7.Quillen DA, Phipps SJ. Visual outcomes and incidence of vitreous loss for residents performing phacoemulsification without prior planned extracapsular cataract extraction experience. American Journal of Ophthalmology. 2003;135(5):732–3. doi: 10.1016/s0002-9394(02)02150-5. [DOI] [PubMed] [Google Scholar]
- 8.Dooley IJ, O’Brien PD. Subjective difficulty of each stage of phacoemulsification cataract surgery performed by basic surgical trainees. J Cataract Refract Surg. 2006;32(4):604–8. doi: 10.1016/j.jcrs.2006.01.045. [DOI] [PubMed] [Google Scholar]
- 9.Rogers GM, Oetting TA, Lee AG, et al. Impact of a structured surgical curriculum on ophthalmic resident cataract surgery complication rates. J Cataract Refract Surg. 2009;35(11):1956–60. doi: 10.1016/j.jcrs.2009.05.046. [DOI] [PubMed] [Google Scholar]
- 10.Mahr MA, Hodge DO. Construct validity of anterior segment anti-tremor and forceps surgical simulator training modules: attending versus resident surgeon performance. J Cataract Refract Surg. 2008;34(6):980–5. doi: 10.1016/j.jcrs.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 11.Selvander M, Asman P. Cataract surgeons outperform medical students in Eyesi virtual reality cataract surgery: evidence for construct validity. Acta Ophthalmol. 2013;91(5):469–74. doi: 10.1111/j.1755-3768.2012.02440.x. [DOI] [PubMed] [Google Scholar]
- 12.Waqar S, Park J, Kersey TL, et al. Assessment of fatigue in intraocular surgery: analysis using a virtual reality simulator. Graefes Arch Clin Exp Ophthalmol. 2011;249(1):77–81. doi: 10.1007/s00417-010-1531-6. [DOI] [PubMed] [Google Scholar]
- 13.Privett B, Greenlee E, Rogers G, Oetting TA. Construct validity of a surgical simulator as a valid model for capsulorhexis training. J Cataract Refract Surg. 2010;36(11):1835–8. doi: 10.1016/j.jcrs.2010.05.020. [DOI] [PubMed] [Google Scholar]
- 14.Pokroy R, Du E, Alzaga A, et al. Impact of simulator training on resident cataract surgery. Graefes Arch Clin Exp Ophthalmol. 2013;251(3):777–81. doi: 10.1007/s00417-012-2160-z. [DOI] [PubMed] [Google Scholar]
- 15.Belyea DA, Brown SE, Rajjoub LZ. Influence of surgery simulator training on ophthalmology resident phacoemulsification performance. J Cataract Refract Surg. 2011;37(10):1756–61. doi: 10.1016/j.jcrs.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 16.Baxter JM, Lee R, Sharp JA, et al. Intensive cataract training: a novel approach. Eye (Lond) 2013;27(6):742–6. doi: 10.1038/eye.2013.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Selvander M, Aman P. Virtual reality cataract surgery training: learning curves and concurrent validity. Acta Ophthalmol. 2012;90(5):412–7. doi: 10.1111/j.1755-3768.2010.02028.x. [DOI] [PubMed] [Google Scholar]
- 18.Saleh GM, Lamparter J, Sullivan PM, et al. The international forum of ophthalmic simulation: developing a virtual reality training curriculum for ophthalmology. Br J Ophthalmol. 2013;97(6):789–92. doi: 10.1136/bjophthalmol-2012-302764. [DOI] [PubMed] [Google Scholar]
- 19.McCannel CA, Reed DC, Goldman DR. Ophthalmic Surgery Simulator Training Improves Resident Performance of Capsulorhexes in the Operating Room. Ophthalmology. 2013;120(12):2456–61. doi: 10.1016/j.ophtha.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 20.Jonas JB, Rabethge S, Bender HJ. Computer-assisted training system for pars plana vitrectomy. Acta Ophthalmol Scand. 2003;81:600–604. doi: 10.1046/j.1395-3907.2003.0078.x. [DOI] [PubMed] [Google Scholar]
- 21.Feldman BH, Ake JM, Geist CE. Virtual reality simulation. Ophthalmology. 2007;114(4):828 e1–4. doi: 10.1016/j.ophtha.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 22.Schmidt RA, Lee TD. Motor Control and Learning: A Behavioral Emphasis. 5th Edition. Champagne, IL: Human Kinetics; 2011. [Google Scholar]
- 23.Thomsen AS, Smith P, Subhi Y, Cour M, Tang L, Saleh GM, Konge L. High correlation between performance on a virtualreality simulator and real-life cataract surgery. Acta Ophthalmol. 2016 Sep 29; doi: 10.1111/aos.13275. [Epub ahead of print]. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 24.Keetch KM, Schmidt RA, Lee TD, Young DE. Especial skills: their emergence with massive amounts of practice. J Exp Psychol Hum Percept Perform. 2005;31(5):970–8. doi: 10.1037/0096-1523.31.5.970. [DOI] [PubMed] [Google Scholar]
- 25.Keetch KM, Lee TD, Schmidt RA. Especial skills: specificity embedded within generality. J Sport Exerc Psychol. 2008;30(6):723–36. doi: 10.1123/jsep.30.6.723. [DOI] [PubMed] [Google Scholar]
- 26.Schmidt RA, Wrisberg CA. Motor Learning and Performance: A Situation-based Learning Approach. Human Kinetics; 2008. [Google Scholar]
- 27.Magill RA, Anderson DI. Motor Learning and Control: Concepts and Applications. Tenth Edition. McGraw-Hill Press; New York, New York: 2014. [Google Scholar]
- 28.Young WB, McDowell MH, Scarlett BJ. Specificity of sprint and agility training methods. J Strength Cond Res. 2001;15(3):315–9. [PubMed] [Google Scholar]
- 29.Hendy HM1, Boyer BJ. Specificity in the relationship between training and performance in triathlons. Percept Mot Skills. 1995 Dec;81(3 Pt 2):1231–40. doi: 10.2466/pms.1995.81.3f.1231. [DOI] [PubMed] [Google Scholar]
- 30.Gergley TJ, McArdle WD, DeJesus P, Toner MM, Jacobowitz S, Spina RJ. Specificity of arm training on aerobic power during swimming and running. Med Sci Sports Exerc. 1984 Aug;16(4):349–54. [PubMed] [Google Scholar]
- 31.Magel JR, Foglia GF, McArdle WD, Gutin B, Pechar GS, Katch FI. Specificity of swim training on maximum oxygen uptake. J Appl Physiol. 1975 Jan;38(1):151–5. doi: 10.1152/jappl.1975.38.1.151. [DOI] [PubMed] [Google Scholar]
- 32.FLO Cycilng - Triathlon Swimming’s Golden Rules - An Interview with Gerry Rodrigues. [Accessed July 2, 2017]. Available at http://flocycling.blogspot.com/2012/02/flo-cycilng-triathlon-swimmings-golden.html.
- 33.Little BC, Smith JH, Packer M. Little capsulorhexis tear-out rescue. J Cataract Refract Surg. 2006 Sep;32(9):1420–2. doi: 10.1016/j.jcrs.2006.03.038. [DOI] [PubMed] [Google Scholar]
- 34.Brazitikos P, Tsinopoulos I, Papadopoulos N, et al. Ultrasonographic classification and phacoemulsification of white senile cataracts. Ophthalmology. 1999;106:2178–83. doi: 10.1016/S0161-6420(99)90502-X. [DOI] [PubMed] [Google Scholar]
- 35.Zare M, Javadi MA, Einollahi B, Baradaran-Rafii AR, Feizi S, Kiavash V. Risk Factors for Posterior Capsule Rupture and Vitreous Loss during Phacoemulsification. J Ophthalmic Vis Res. 2009;4(4):208–12. [PMC free article] [PubMed] [Google Scholar]
- 36.Briszi A, Prahs P, Hillenkamp J, et al. Complication rate and risk factors for intraoperative complications in resident-performed phacoemulsification surgery. Graefes Arch Clin Exp Ophthalmol. 2012;250(9):1315–20. doi: 10.1007/s00417-012-2003-y. [DOI] [PubMed] [Google Scholar]
- 37.Blomquist PH, Morales ME, Tong L, Ahn C. Risk factors for vitreous complications in resident-performed phacoemulsification surgery. J Cataract Refract Surg. 2012;38(2):208–14. doi: 10.1016/j.jcrs.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mayo E. The Human Problems of an Industrial Civilization. In: Thompson K, editor. The early sociology of management and organizations. VI. New York: Macmillan Co; 1933. p. 55e77. [Google Scholar]