Abstract
Olecranon fractures are common and often require surgical treatment when displaced. Traditional methods of stabilization using tension band wire fixation and plate fixation achieve adequate union and function but are associated with a high rate of re-operation and wound problems because of prominent metalwork. The purpose of the present article is to describe an all suture technique for fixation of simple olecranon fractures that maintains inter-fragmentary compression, provides bony union and reduces the rate of re-operation caused by prominent metalwork.
Keywords: fixation, fracture, olecranon, olecranon osteotomy, suture, tension band
Introduction
Olecranon fractures account for 0.9% of all fractures and 10% of all upper extremity fractures.1 Most fractures are simple transverse intra-articular fractures that occur from standing height falls; however, higher energy injuries may result in substantial articular comminution or be part of a more complex fracture dislocation pattern.1
The most common mechanism of fracture is a direct blow to the elbow, followed by avulsion fractures and less commonly, stress fractures. Olecranon osteotomy performed for access to the distal humerus is a further reason where fixation of the olecranon might be necessary.1,2
Surgical fixation of an olecranon fracture is indicated if there is extensor mechanism weakness, intra-articular displacement or instability of the ulnohumeral joint. Contraindications include lower demand patients with poor soft tissue and bone quality. In this group, satisfactory results have been achieved with non-operative treatment.3
Regardless of the mechanism, the goals of surgery are: (i) to achieve anatomic reduction of the greater sigmoid notch of the ulna; (ii) neutralize the displacing force of the triceps; (iii) permit early range of motion; and (iv) avoid complications or re-operation.
Commonly used techniques include tension band wire fixation, plate fixation and, more recently, intramedullary fixation. The most common complication associated with all olecranon fracture surgery is prominence of metalwork causing discomfort, wound breakdown and/or re-operation for removal of hardware. This has been reported to be as high as 75% for tension band wiring and 50% for plate fixation.2,4–6
To try and address the problems related to prominent hardware and re-operation, we have developed a novel technique utilizing a high strength, braided suture without kirschner wires that reduces the incidence of prominent hardware without compromising mechanical stability.
Indications
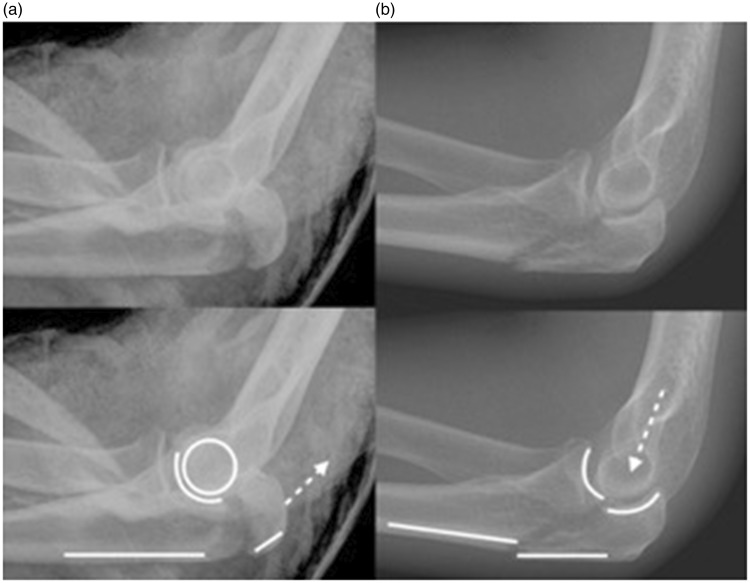
This technique is routinely used by the authors for fixation of simple, transverse olecranon fractures and chevron osteotomies performed for distal humeral access (Fig. 1a).
Figure 1.
(a) A typical transverse olecranon fracture treated using the suture technique. There is no translation of the dorsal cortex of the ulna and the ulnohumeral joint is congruent. The direction of force (dotted arrow) is in the line of the triceps. (b) Ulnohumeral instability following an olecranon fracture. Note the ulnohumeral incongruity and step in the dorsal cortex of the ulna created by translation of the proximal fragment relative to the ulna shaft. The dotted arrow indicates the direction of force. Plate fixation is advocated for this fracture.
In addition, it is used to augment plate fixation of comminuted proximal ulna fractures where there is a risk of proximal fragment ‘escape’ from the construct.
It is also used for smaller avulsion fractures of the olecranon that are normally difficult to secure with metalwork and may have been treated by fragment excision and triceps advancement in the past.
A further indication is in paediatric olecranon fractures where placement of metalwork is even less desirable.
These indications comprise over 75% of all olecranon fractures.2
Contraindications
The suture fixation technique employs a tension band principle, and therefore is not suitable for fractures with significant articular comminution, multi-fragmentary fractures, and fractures that extend distal to the greater sigmoid notch.
Most importantly, the technique is not advocated for fractures with associated ulnohumeral instability (Fig. 1b), namely trans-olecranon fracture dislocations and Monteggia variants that affect the olecranon.
Surgical technique
Set-up
The patient is placed in the lateral decubitus position under general anaesthesia with a high arm tourniquet. The arm is placed over a lateral support, which allows unimpeded full extension of the elbow. The fluoroscopy unit is brought in from the opposite side of the table perpendicular to the long axis of the arm. Lateral imaging is achieved by elevating the arm slightly and coronal imaging is obtained by rotating the arm at the shoulder.
Prophylactic antibiotics are administered prior to inflation of the tourniquet.
Surgical approach
A posterior midline longitudinal incision is made skirting radially around the point of the elbow. Full thickness skin and subcutaneous flaps are raised with care taken not to perform excessive undermining of the tissues. The ulna nerve is not routinely identified or decompressed. The fracture is exposed and thoroughly cleared of debris. Care is taken to identify the fracture ends by removing a few millimeters of soft tissue to aid anatomic reduction of the cortical surfaces. Sub-periosteal elevation of the soft tissue from the medial and lateral aspect of the ulna shaft is performed to allow placement of a transverse drill hole.
Reduction and fixation
Direct reduction of the fracture is performed using a large fragment pointed reduction clamp. The clamp provides inter-fragmentary compression. A unicortical 2.5-mm drill hole made on the dorsal surface of the ulna and angulated slightly proximal aids secure positioning of the clamp and prevents slippage prior to final fracture fixation. Satisfactory reduction of the articular surface is confirmed under fluoroscopy before proceeding with suture fixation.
Levered retractors are placed around the ulna and a transverse 2.5-mm drill hole is made distal to the level of the ulnohumeral joint and at least 15 mm from the fracture line. This hole is made from medial to lateral to minimize risk of injury to the ulna nerve and should be anterior enough to provide at least a 10-mm dorsal bone bridge. With the fracture reduced, a synthetic braided number 2 Orthocord suture (De Puy Synthes, West Chester, PA, USA) with a needle attached is passed through the transverse drill hole from lateral to medial. This ensures the final knot will lie on the lateral aspect of the ulna. Orthocord is preferred because it is partially resorbed (62% polydioxanone), which gives it superior handling properties and allows space for tissue ingrowth and load sharing.
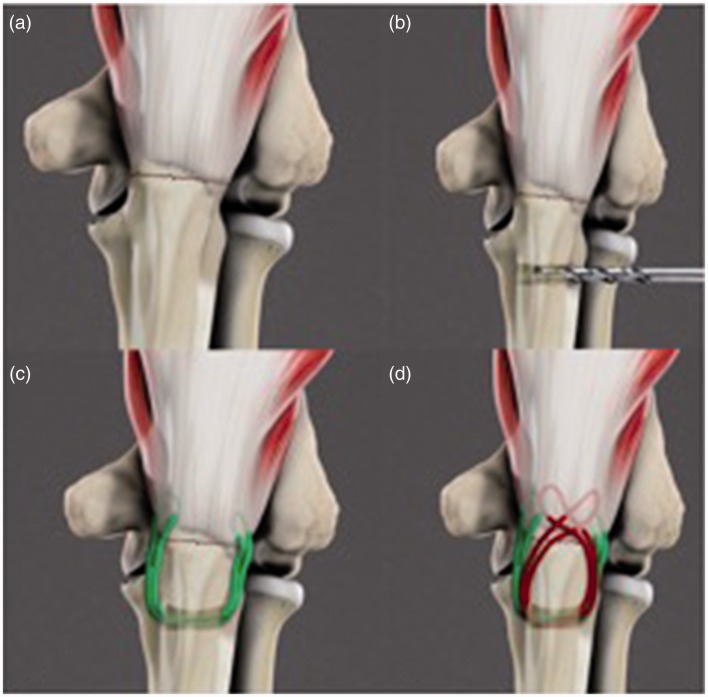
A simple horizontal grasping stitch is placed the triceps where it inserts onto the medial aspect of the proximal fragment. This suture is then brought back through the transverse drill hole from medial to lateral and then passed through the triceps tendon on the lateral aspect of the proximal fragment in the same fashion. This creates a tensionable suture loop in the long axis of the ulna, replicating the action of intra-medullary kirschner wires. Pulling on both sutures ends maximizes compression across the fracture site and a surgeon’s knot is tied on the lateral aspect of the ulna. A second Orthocord is passed through the transverse hole from lateral to medial but is brought obliguely over the dorsal surface of the ulna and a horizontal grasp is placed in the triceps tendon on the lateral aspect of the proximal fragment. The suture is then passed back through the transverse tunnel from medial to lateral and brought obliquely over the ulna to grasp the medial triceps. The two free ends of the suture are then tied to each other on the lateral aspect of the ulna (Figure 2). This second suture provides a figure of eight tension band along the dorsal aspect of the ulna (Figure 3).
Figure 2.
Schematic diagram of the suture technique. (a) Transverse olecranon fracture. (b) Creation of transverse tunnel distal to the fracture. (c) Placement of first longitudinal suture loop. (d) placement of second figure of eight suture loop. The knots are not illustrated here but are tied on the lateral aspect of the olecranon.
Figure 3.
In vivo final construct following suture fixation.
Both sutures are tied with the elbow in extension so that they tighten as the elbow is flexed, converting the tension forces on the dorsal aspect of the ulna into compression at the articular surface.
The clamp is removed and stable reduction without gapping of the articular surface is confirmed under fluoroscopy with the elbow fully flexed and extended.
The wound closure is performed in 30° flexion to prevent excessive tension on the suture line as the elbow is flexed postoperatively. Care is taken to close the anconeous fascia over the laterally based knots using a 2-0 absorbable-braided suture. This leaves the Orthocord knots deep to the soft tissues minimizing skin irritation. Further subcutaneous and subcuticular closure is performed in a standard fashion.
Longitudinal steristrips, an absorbant adhesive dressing and a wool and crepe compression bandage is applied. The arm is placed in a sling for comfort.
Rehabilitation
Immediate active range of motion is permitted with an emphasis on regaining full extension. The bulky dressing is reduced at 48 hours and the wound reviewed in clinic at 2 weeks. Heavy or repetitive lifting and axial loading on the arm is avoided for 6 weeks to minimize the triceps force. A further radiographic and clinical review is performed at 6 weeks to 8 weeks, after which the patient is usually discharged to the care of physiotherapy.
Clinical results
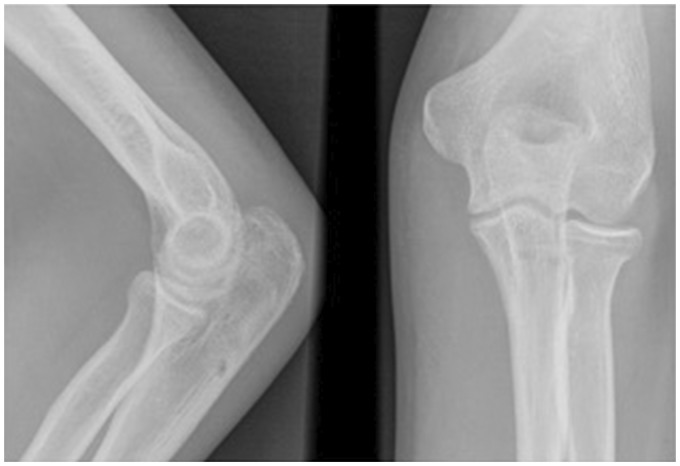
To date, we have performed this procedure on 17 patients with an acute fracture and 11 patients with an olecranon osteotomy. Radiographic union was achieved in all patients at a mean of 6 weeks (5 weeks to 8 weeks) (Figure 4).
Figure 4.
Example of a postoperative X ray demonstrating anatomic articular reduction and bony union at 8 weeks post operatively.
One patient had loss of reduction after fracture of the dorsal cortex of the transverse suture tunnel. This was because of osteoporotic bone and a technical error leaving the bone bridge too small. The result was a malunion with a 5-mm gap at the fracture site. The patient did not require re-operation and had no functional deficit.
All other patients healed with anatomic reduction of the articular surface.
One further patient developed heterotopic ossification following fixation of a distal humerus fracture after an olecranon osteotomy had been performed. The osteotomy healed anatomically and the heterotopic ossification was adjacent to the distal humerus rather than the proximal ulna.
There have been no other instances of late articular displacement or gapping at the fracture site. No patients have required removal of their sutures or re-operation related to the olecranon fracture. There have been no wound-related complications.
Discussion
Our experience of using suture fixation to stabilize simple olecranon fractures has been positive with no re-operations or wound complications and only one instance of fracture gapping caused by a technical error. All patients treated have had good or excellent functional outcomes with minimal loss of motion.
The technical pearls for performing this procedure successfully are outlined in Table 1.
Table 1.
Technical pearls.
| Technical Pearls | Rationale |
|---|---|
| Use a non-absorbable braided suture | Has similar strength and fatigue properties to steel wire therefore will not elongate significantly under load |
| Compress and reduce the fracture with a pointed reduction clamp | The suture will maintain compression once the clamp is removed and act as a tension band but is not used as a reduction tool |
| Maintain at least a 10-mm bone bridge between the dorsal ulna cortex and the transverse drill hole | Aligns suture parallel to the the long axis of the ulna shaft and minimizes the risk of tunnel fracture |
| Ensure grasping bites in the triceps are as close to bone as possible | Ensures closer suture contact with bone which improves construct stability |
| Use two separate sutures and tie two knots | Results in more sutures crossing the fracture site in different orientations and acts as a fail safe if one suture loosens |
| Tighten the sutures and tie the knots with the elbow extended | Generates compressive forces at the fracture site when the elbow is flexed and minimizes slack in the system |
| Tie the knots on the lateral aspect of the ulna and bury them underneath anconeus during closure | Avoids knots close to the ulna nerve and prevents knot prominence through the skin |
A potential concern with using braided sutures is whether they can resist the high tensile load imparted by the triceps; however, braided sutures have been tested in vitro and in vivo where they have been shown to match the tensile strength and fatigue properties of stainless steel wires.7,8
Based on our results, suture fixation is now the mainstay of treatment for all simple olecranon fractures and we no longer perform the traditional tension band wiring technique using steel wires for any fractures. If the fracture is not amenable to suture fixation, we advocate plating.
The results presented are from a two centre experience; however, the technique has gained popularity and we feel comfortable recommending it to fellow surgeons. We are in the process of performing a prospective comparative study to further assess the technique.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical review and patient consent
All patients consented to collection of outcome scores used as part of this publication.
References
- 1.Duckworth AD, Clement ND, Aitken SA, et al. The epidemiology of fractures of the proximal ulna. Injury 2012; 43: 343–346. [DOI] [PubMed] [Google Scholar]
- 2.Brolin TJ, Throckmorton T. Olecranon fractures. Hand Clinics 2015; 31: 581–590. [DOI] [PubMed] [Google Scholar]
- 3.Duckworth AD, Bugler KE, Clement ND, et al. Non-operative management of displaced olecranon fractures in low-demand elderly patients. The Journal of Bone and Joint Surgery 2014; 96: 67–72. [DOI] [PubMed] [Google Scholar]
- 4.Snoddy MC, Lang MF, An TJ, et al. Olecranon fractures: factors influencing re-operation. International Orthopaedics (SICOT) 2014; 38: 1711–1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Macko D, Szabo RM. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg Am 1985; 67: 1396–1401. [PubMed] [Google Scholar]
- 6.Buijze G, Kloen P. Clinical evaluation of locking compression plate fixation for comminuted olecranon fractures. The Journal of Bone and Joint Surgery 2009; 91: 2416–2420. [DOI] [PubMed] [Google Scholar]
- 7.Carofino BC, Santangelo SA, Kabadi M, et al. Olecranon fractures repaired with FiberWire or metal wire tension banding: a biomechanical comparison. Arthroscopy 2007; 23: 964–970. [DOI] [PubMed] [Google Scholar]
- 8.Wright PB, Kosmopoulos V, Coté RE, et al. FiberWire is superior in strength to stainless steel wire for tension band fixation of transverse patellar fractures. Injury 2009; 40: 1200–1203. [DOI] [PubMed] [Google Scholar]