Abstract
Background
We report on the non-operative treatment of Mayo Type II olecranon fractures.
Methods
Fourteen isolated Mayo Type II olecranon fractures were treated non-operatively, followed to discharge, and retrospectively reviewed. Treatment was splinting in extension followed by protected active motion beginning 3 weeks to 4 weeks post-injury. Mayo Elbow Performance Index (MEPI) and Shortened Disabilities of the Arm, Shoulder and Hand (QuickDASH) scores were available in 86% and 64% of cases, respectively. Follow-up radiographs were obtained.
Results
At discharge, the mean (SD) MEPI score was 95 (5). The mean (SD) elbow motion arc was 121° (21°). One patient re-fractured his elbow after discharge by falling on the ice. He recovered after open reduction and internal fixation. One patient (documented Marfan syndrome) developed an asymptomatic non-union. Excepting the patient who fell, no patient received additional care.
Conclusions
In this pilot report, Mayo Type II olecranon fractures were treated non-operatively to discharge. Good to excellent results were obtained in all patients according to the MEPI. Supportive care of these fractures should be comparatively studied. A downside risk to providing supportive care for these fractures was not identified.
Keywords: closed olecranon fracture, MEPI, nonoperative care, QuickDASH, splinting, type 2 olecranon fracture
Introduction
Mayo Type II olecranon fractures that are isolated and closed (Mayo Type II = OTA/AO 21-B1)1 are the most common olecranon fracture.2 Using the Mayo classification, these displaced fractures can be either non-comminuted (subtype A) or comminuted (subtype B). Probably, the majority of these fractures undergo operative treatment.
There is evidence that non-operative treatment of olecranon fractures can be appropriate.3,4 Favourable outcomes from conservative treatment of displaced olecranon fractures are described in low-demand, elderly patients.5,6 Another study documented qualitative results using conservative treatment in complex fractures, defining a good outcome as one in which patients had a loss of flexion/extension of up to 15° and slight or occasional pain.7 We have not identified a study devoted to documenting functional outcomes of isolated Mayo Type II olecranon fractures in a cohort of normal demand patients covering adults of all ages. In the present study, we quantitatively document functional outcomes following conservative treatment of minimally-displaced and displaced Mayo Type II olecranon fractures in adults of all ages. In addition, we detail our treatment protocol.
Materials and methods
We performed a retrospective review (Instititional Review Board approved) to identify all skeletally mature patients who were treated non-operatively for an olecranon fracture from January 2006 through April 2014. Information was abstracted from the medical records, including demographic data, date of birth, date of injury, mechanism of injury, fracture type, complications, any subsequent surgical procedures, comorbidities, and follow-up data. Shortened Disabilities of the Arm, Shoulder and Hand (QuickDASH) Outcome Measure8,9 (Institute for Work & Health, Toronto, Ontario, Canada) scores were entered into the dataset. Radiographs were reviewed. We calculated Mayo Elbow Performance Index (MEPI)8,10 scores as described below.
Data collection
In identified isolated olecranon fractures, radiographs were reviewed to confirm the fracture type in accordance with the Mayo classification. Only Mayo Type II fracture patients underwent further data collection/analyses. We utilized our electronic medical record to obtain data from physician and therapy notes.
Initial care
No attempt was made to randomize or direct a patient’s choice of care. Our routine is to describe all treatment options to the patient enabling the patient to choose their preferred treatment using a shared decision making model.11 Thus, the care delivered was the informed preference of the patient (in one patient with Alzheimer’s, the family guardian chose the care to be rendered). For comparison, during the study time period, 29 patients with isolated closed olecranon fractures were treated operatively (1 Type I, 23 Type II, 5 Type III) (same clinic and same attending surgeons).
Discharge from care
Patients were discharged when fracture healing was complete and/or functional status returned to near baseline. Range of motion, pain, strength, complications and functional disability, and return to pre-injury activities were assessed at follow-up visits. MEPI scores were calculated using records data. Sixty-four percent of patients completed the QuickDASH at discharge.
Outcome instruments employed
MEPI: MEPI (Table 1) allocates points to: pain (n = 35); motion (n = 40); strength (n = 20); and stability (n = 5) (100 possible). Outcome ratings are according to the score achieved: 91 to 100, excellent; 81 to 90, good; 71 to 80, fair; and <70, poor. Rating scores were unavailable for two patients in the series (86% of the patients were assigned a MEPI score). The QuickDASH is a true patient-reported instrument and is validated for the arm but not specific to the elbow. Final scores range between 0 (no disability) to 100 (greatest possible disability). Rating scores were available for nine patients in the series (64%).
Table 1.
Mayo Elbow Performance Index (MEPI).
| MEPI rating criteria10 | Number of points |
|---|---|
| Pain | |
| None | 35 |
| Mild requiring no medication | 25 |
| Moderate requires medication | 15 |
| Severe to incapacitating | 0 |
| Motion flexion arc (°) | |
| ≥100 | 40 |
| 70 to 99 | 30 |
| 40 to 69 | 15 |
| <40 | 0 |
| Strength of flexion and extension | |
| Normal | 20 |
| Mild loss | 14 |
| Moderate loss | 7 |
| Marked weakness | 0 |
| Stability | |
| Stable | 5 |
| Moderate unstable | 2 |
| Severely unstable | 0 |
Treatment
Elbows were splinted at nearly full extension (5° to 15° short of full extension) in a removable splint fabricated by therapy or a cast. Patients were followed clinically and radiographically every 7 days to 14 days to ensure no displacement of the fracture occurred, until fracture healing. At follow-up examimnations, we ensured via radiographs that no anterior subluxation of the ulnar shaft relative to the trochlea had occurred. Resistance-free active range of motion (AROM) exercises (15 minutes, two to four times each day) were initiated when there was clinical evidence of fracture healing (lack of tenderness to palpation at the fracture site), usually at 3 weeks to 4 weeks post-injury. Note: the single patient with Alzheimer’s remained casted until 4 weeks post-injury. At 3 weeks to 4 weeks post-injury, a supervised therapy program was initiated (active-assisted range of motion, with gravity/resistance eliminated, 15 minutes to 30 minutes, two to four times a day) and the splint was discontinued by 6 weeks. Resistive strengthening with use of a sling between exercise periods began at 6 weeks to 8 weeks post-injury. Between >6 weeks and 12 weeks post-fracture, the patient was encouraged to resume full activity.
Statistical analysis
Descriptive statistics were obtained via Excel (Microsoft Corp., Redmond, WA, USA) and are reported as means (with range and SD). A histogram is used to display age/sex distribution.
Results
This cohort consists of eight men and six women with a mean age of 55 years (range 22 years to 84 years) (mean female age 47 years, mean male age 61 years) (Table 2). The left side was affected in eight cases (57%). One or more comorbidities were present in seven patients (50%): seizure disorder and Parkinson disease (n = 1), Alzheimer disease (n = 1), Marfan syndrome (n = 1), alcohol abuse (n = 2), asthma (n = 1) and contralateral radius fracture (casted) 2 weeks prior to olecranon fracture (n = 1). Mechanisms of injury were: fall from standing height (n = 9; 64%); fall down steps (less than one flight) (n = 1; 7%); slip on ice (n = 1; 7%); bicycle crash (n = 2; 14%); and seizure (n = 1; 7%). The fractures had an average initial displacement of 8.6 mm (range 2 mm to 25 mm; SD 8.9 mm) at presentation.
Table 2.
Olecranon fractures by sex and age.
| Age range (years) (decade) | Number of males | Number of females | |
|---|---|---|---|
| 15 to 20 | 0 | 0 |
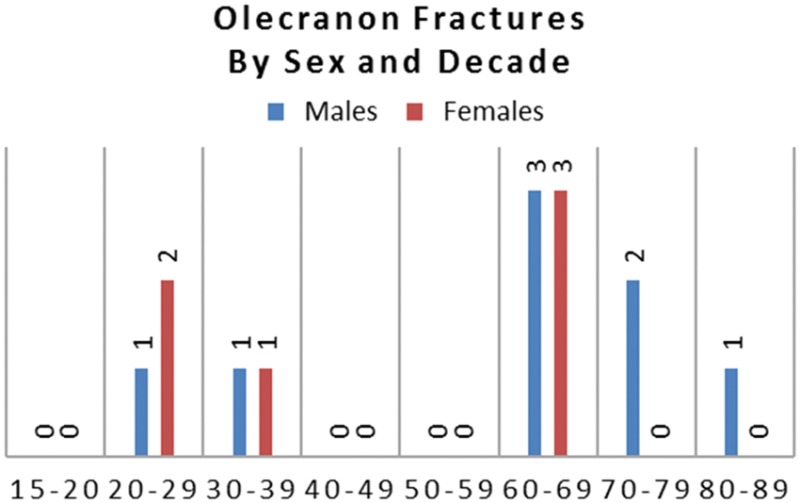
|
| 20 to 29 | 1 | 2 | |
| 30 to 39 | 1 | 1 | |
| 40 to 49 | 0 | 0 | |
| 50 to 59 | 0 | 0 | |
| 60 to 69 | 3 | 3 | |
| 70 to 79 | 2 | 0 | |
| 80 to 89 | 1 | 0 |
Follow-up outcomes (Table 3)
Table 3.
Mayo Type II – closed care olecranon fractures (results by sex)
| Sex | Mean age (years) | Subtype A/B | Mean fracture displacement (mm) (range) | Mean days to discharge | Mean MEPI | Mean QuickDASH | Complications |
|---|---|---|---|---|---|---|---|
| Male (n = 8) | 61 | 7/1 | 6.8 (2.0 to 25.0) | 70 | 99 (n = 7) | 18 (n = 6) | One re-fracture (new fall) |
| Female (n = 6) | 47 | 5/1 | 7.2 (2.1 to 20.0) | 80 | 91 (n = 5) | 6 (n = 3) | None |
MEPI, Mayo Elbow Performance Index; QuickDASH, Shortened Disabilities of the Arm, Shoulder and Hand.
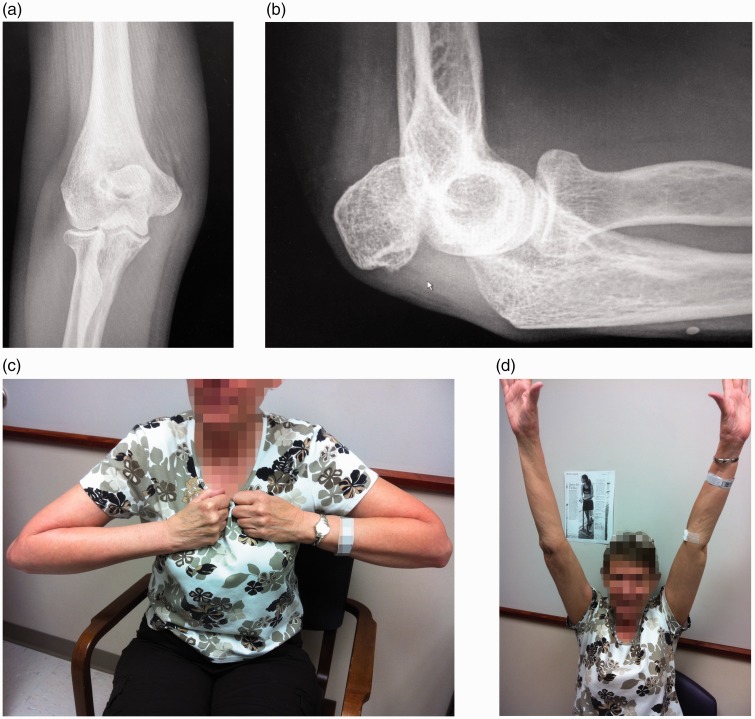
Mean (SD) discharge was 73 days (26 days). The mean (SD) MEPI score was 96 points (range 86 points to 100 points). The mean (SD) QuickDASH score was 12 (22). The mean (SD) elbow motion arc was 121° (21°). Mean (SD) elbow flexion was to 130° (19°). Mean (SD) elbow extension was 9° of flexion (11°). The mean (SD) forearm rotation arc was 175° (8°). Two patients did not have sufficient information in their charts to calculate the MEPI score. Notably, a QuickDASH and MEPI were obtained for the patient with Marfan syndrome who had a painless and functional non-union of the fracture at final follow-up (Figure 1). All of the patients included in this report were successfully returned to pre-morbid activity, with none known to have received subsequent care (excepting the re-fracture noted below).
Figure 1.
Patient 1. (a) Follow-up anteroposterior (AP) radiograph showing maintenance of ulnohumeral stability. (b) Follow-up lateral radiograph showing non-union of olecranon with no anterior translation of the ulnohumeral joint. (c) At 6 weeks post-fracture, the patient has full painless flexion (affected side is patient’s right, opposite to watch). (d) Same conditions as (c), with elbow in full painless extension.
One patient received subsequent operative treatment. He had been discharged from active care. At 3 months, he fell on ice and re-fractured the olecranon. The ulnohumeral joint remained stable. Open reduction and internal fixation (ORIF) was performed and he fully recovered.
Measureable direct cost associated with our non-operative regimen was $2319 in 2014 US dollars (average dollars billed). We did not include any costs associated with work modification/compensation.
Discussion
Currently, the preferred treatment of olecranon fractures is surgery. Indeed, when reviewing treatment alternatives, Hak and Galloday12 did not include non-operative care as an option. However, as noted at the outset, studies have described non-operative care of this fracture in select patients.3–5 To our knowledge, this is the first study to expand the age where such care can be considered to include all adult patients. Our results demonstrate that non-operative treatment of Type II olecranon fractures can yield excellent and good outcomes (as defined by the MEPI) in patients of both sexes and across the adult age range. In patients with more complex fractures, surgery is still our preferred treatment method as described by Ring et al.13 As related to managing these fractures in patients with comorbidities, we note that successful management of Type II olecranon fractures in the presence of comorbidities is possible.
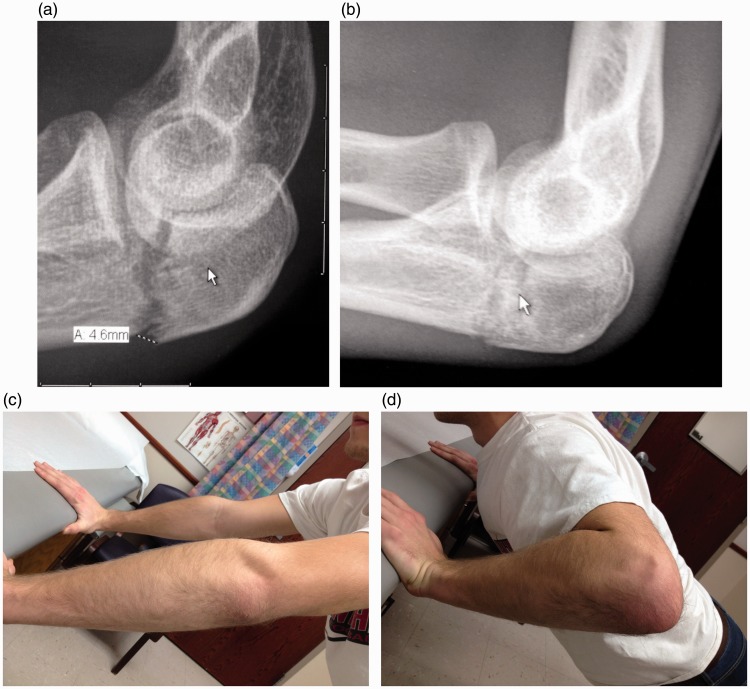
In our patients, non-operative treatment was a successful treatment strategy as it relates to regaining useful function (Figures 1 and 2). In addition to recovering function, our patients realized at least two added benefits. First, the chance of a surgical complication with non-operative care was zero. Second, because care did not require the insertion of orthopedic hardware, there were no orthopedic hardware complications. By comparison, in one study, ORIF of olecranon fractures required removal in 81% of patients.14
Figure 2.
Patient 2. (a) Initial lateral plain film radiograph demonstrates a Type II olecranon fracture. (b) Subsequent lateral plain film radiograph at 4 weeks demonstrates callus formation and healing of the fracture. (c) At 6 weeks post-fracture, the patient was able to do push-ups against resistance (elbow extended, affected side towards the camera). (d) Same conditions as (c), with elbow in flexion.
Nonsurgical treatment has disadvantages. Close follow-up is required. Failure to properly follow the patient could lead to late identification of an unstable elbow. Therefore, patients/caregivers must be vigilant. Notably, our cohort included one patient with dementia who repeatedly removed his splint (after initial casting) when not being observed; despite this behavior, the patient still had a good outcome. Another disadvantage of nonsurgical treatment is the potential of a re-fracture. We saw this with one patient who then required surgical fixation. Whether this complication is more or less frequent than would be seen with ORIF of the same fracture would require a large comparative study. Finally, the frequency of this treatment leading to non-union cannot be determined from this small sample. One patient in this study developed a non-union. This specific patient has documented Marfan syndrome without other co-morbidities (i.e. tobacco use disorder). Despite developing a non-union the patient maintained a stable ulnohumeral joint, a full painless active range of motion, and her MEPI and QuickDASH scores were excellent (Figure 1).
There are additional limitations to the present study. Notably, we had a small cohort consisting of fourteen patients. The study probably suffers from inherent selection bias by both surgeons and patients. That is, the patients who chose non-operative care may be attitudinally different when compared to those choosing surgery, and this difference would impact their acceptance of outcome. Also, not being a prospective study, our follow-up was limited to data collected prior to discharge from active care.
We began the present study after several patients who had declined operative intervention of their closed Type II olecranon fractures recovered excellent function after non-operative care alone. We did not convert our process to a prospective study largely as a result of inertia. Having collected the patients we are reporting on, we consider that a prospective multicentre study of this treatment would be appropriate. We believe this based upon our experience. But, we have also considered why this intra-articular fracture may be amenable to a treatment method that runs counter to current practice. Based on our reading, these results rely on: (i) retained ligament support and (ii) retained dynamic muscle support.
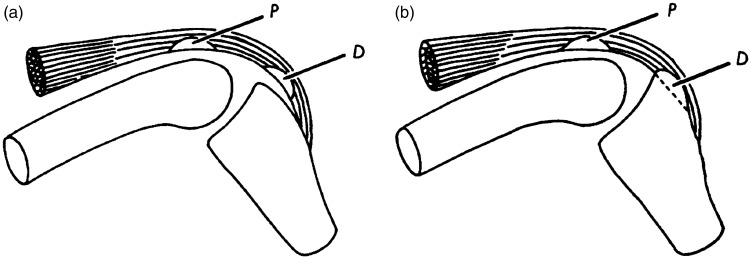
The olecranon does not arise as a single bony element. Rather, it is a fusion of what phylogenetically is a sesamoid bone. Barnett and Lewis15 described the nature of the sesamoid olecranon in avians and the tree shrew, proposing that the olecranon may have evolved into a traction epiphysis (Figure 3). In humans, a fusion streak persists between the more distal olecranon and the proximal ‘traction epiphysis’ (a term introduced by Parsons in 190416).17 This streak consistently appears near halfway between proximal and distal olecranon margin. Fractures proximal to this streak (50% or less) are described as possibly amenable to non-operative care in select patients, whereas fractures more distal (greater than 50%) are assumed to be unstable thus requiring surgery.18
Figure 3.
(a) Proximal (p) and distal (d) sesamoids related to a hypothetical joint. (b) Conversion of distal sesamoid into a traction epiphysis. Reporoduced with permission.15
As we learn more about genetic development, it is interesting to note that the HOX11 homeobox gene controls development of the zeugopod (forearm) and that absence of these genes in a mouse embryo model results in the development of an incomplete olecranon similar to that seen in avian species described above.19 From our perspective, the critical point of this information related to our proposed treatment is that ligaments are attached medially and laterally distal to this ‘50% line’.16 The potential added ulnohumeral stability of a fused olecranon appears to be an evolutionary development.
In addition to the instantaneous stability afforded the ulnohumeral joint by way of bone and ligament anatomy, a study by Molinear et al.20 suggests that the anconeus can dynamically stabilize the ulnohumeral joint against varus rotational loads.20 Similarly, Park and Ahmad21 previously described the importance of the flexor-pronator muscle group as it relates to dynamically stabilizing the ulnohumeral joint against valgus loads.21
Ultimately, no single fact explains why a Type II olecranon fracture may be more amenable to closed care than has recently been taught. However, we consider that a combination of the above information provides a foundation from which our results can be considered.
In the present study, we report on non-operative care of Type II olecranon fractures in adults of all ages. We treated a near equal number of men and women. In the cases for which a MEPI score was available, the outcome was rated as excellent or good. The MEPI rating was independent of displacement. Outcome ratings were independent of patient age and the outcomes were comparable for men and women in the cohort. In this cohort, the recorded patient comorbidities were not predictive of outcome.
Conclusions
Non-operative treatment of Mayo Type II olecranon fractures may be successful. Our results are consistent with those from more limited studies but extend the age range for which such treatment of displaced olecranon fractures can be considered.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent
IRB Study Track ID: 0907M69141. As a retrospective study, no patient consent was required.
Level of Evidence
Therapeutic Level IV
References
- 1.Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium 2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 2007; 21(10 Suppl): S1–S133. [DOI] [PubMed] [Google Scholar]
- 2.Duckworth AD, Clement ND, Aitken SA, Court-Brown CM, McQueen MM. The epidemiology of fractures of the proximal ulna. Injury 2012; 43: 343–46. [DOI] [PubMed] [Google Scholar]
- 3.Eriksson E, Sahlin O, Sandahl U. Late results of conservative and surgical treatment of fracture of the olecranon. Acta Chir Scand 1957; 113: 153–166. [PubMed] [Google Scholar]
- 4.Lou I. Olecranon fractures treated in the Orthopaedic Hospital, Copenhagen 1936–47; a follow-up examination. Acta Orthop Scand 1949; 19: 166–179. [DOI] [PubMed] [Google Scholar]
- 5.Duckworth AD, Bugler KE, Clement ND, Court-Brown CM, McQueen MM. Nonoperative management of displaced olecranon fractures in low-demand elderly patients. J Bone Joint Surg Am 2014; 96: 67–72. [DOI] [PubMed] [Google Scholar]
- 6.Gallucci GL, Piuzzi NS, Slullitel PA, et al. Non-surgical functional treatment for displaced olecranon fractures in the elderly. Bone Joint J 2014; 96B: 530–534. [DOI] [PubMed] [Google Scholar]
- 7.Parker MJ, Richmond PW, Andrew TA, Bewes PC. A review of displaced olecranon fractures treated conservatively. J R Coll Surg Edinb 1990; 35: 392–394. [PubMed] [Google Scholar]
- 8.Morrey B, An K, Chao E. Functional evaluation of the elbow. In: Morrey B. (ed). The elbow and its disorders, 2nd ed Philadelphia, PA: WB Saunders, 1993, pp. 86–97. [Google Scholar]
- 9.Longo UG, Franceschi F, Loppini M, Maffulli N, Denaro V. Rating systems for evaluation of the elbow. Br Med Bull 2008; 87: 131–161. [DOI] [PubMed] [Google Scholar]
- 10.Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am 1989; 71: 1348–1354. [PubMed] [Google Scholar]
- 11.Elwyn G, Frosch D, Thomson R, et al. Shared decision making: A model for clinical practice. J Gen Intern Med 2012; 27: 1361–1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hak DJ, Golladay GJ. Olecranon fractures: Treatment options. J Am Acad Orthop Surg 2000; 8: 266–275. [DOI] [PubMed] [Google Scholar]
- 13.Martin JA, Regehr G, Reznick R, et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg 1997; 84: 273–278. [DOI] [PubMed] [Google Scholar]
- 14.Chalidis BE, Sachinis NC, Samoladas EP, Dimitriou CG, Pournaras JD. Is tension band wiring technique the ‘gold standard’ for the treatment of olecranon fractures? A long term functional outcome study. J Orthop Surg Res 2008; 3: 9–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barnett CH, Lewis OJ. The evolution of some traction epiphyses in birds and mammals. J Anat 1958; 92: 593–601. [PMC free article] [PubMed] [Google Scholar]
- 16.Parsons FG. Observations on traction epiphyses. J Anat Physiol 1904; 38: 248–258. [PMC free article] [PubMed] [Google Scholar]
- 17.Malagelada F, Dalmau-Pasto M, Vega J, Golanó P. Elbow Anatomy. In: Doral MN, Karlsson J. (eds). Sports injuries: prevention, diagnosis, treatment and rehabilitation, Berlin: Springer, 2014, pp. 1–30. [Google Scholar]
- 18.Wiegand L, Bernstein J, Ahn J. Fractures in brief: olecranon fractures. Clin Orthop Relat Res 2012; 470: 3637–3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koyama E, Yasuda T, Minugh-Purvis N, et al. Hox11 genes establish synovial joint organization and phylogenetic characteristics in developing mouse zeugopod skeletal elements. Development 2010; 137: 3795–3800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Molinier F, Laffosse J-M, Bouali O, Tricoire J-L, Moscovici J. The anconeus, an active lateral ligament of the elbow: new anatomical arguments. Surg Radiol Anat 2011; 33: 617–621. [DOI] [PubMed] [Google Scholar]
- 21.Park MC, Ahmad CS. Dynamic contributions of the flexor-pronator mass to elbow valgus stability. J Bone Joint Surg Am 2004; 86A: 2268–2274. [DOI] [PubMed] [Google Scholar]