Supplemental Digital Content is available in the text.
Keywords: critical care, intensive care unit, organ donation, palliative care, resource allocation
Abstract
Objectives:
To describe the characteristics, circumstances, change over time, resource use, and outcomes of patients admitted to ICUs in Australia and New Zealand for the purposes of “palliative care of a dying patient” or “potential organ donation,” and compare with actively managed ICU patients.
Design:
A retrospective study of data from the Australian and New Zealand Intensive Care Society Adult Patient Database and a nested cohort analysis of a single center.
Setting:
One hundred seventy-seven ICUs in Australia and New Zealand and a nested analysis of one university-affiliated hospital ICU in Melbourne, VIC, Australia.
Patients:
Three thousand seven hundred “palliative care of a dying patient” and 1,115 “potential organ donation” patients from 2007 to 2016. The nested cohort included 192 patients.
Interventions:
No interventions. Data extracted included patient demographics, diagnoses, length of stay, circumstances, and outcome of admission.
Measurements and Main Results:
ICU admissions for “palliative care of a dying patient” and “potential organ donation” increased from 179 in 2007 to 551 in 2016 and from 44 in 2007 to 174 in 2016 in each respective group, though only the “potential organ donation” cohort showed an increase in proportion of total ICU admissions. Lengths of stay in ICU were a mean of 33.8 hours (median, 17.5; interquartile range, 6.4–38.8) and 44.7 hours (26.6; 16.0–44.6), respectively, compared with 74.2 hours (41.5; 21.7–77.0) in actively managed patients. Hospital mortality was 86.6% and 95.9%, respectively. In the nested cohort of 192 patients, facilitating family discussions about goals of treatment and organ donation represented the most common reason for ICU admission.
Conclusions:
Patients admitted to ICU to manage end-of-life care represent a small proportion of overall ICU admissions, with an increasing proportion of “potential organ donation” admissions. They have shorter ICU lengths of stay than actively managed patients, suggesting resource use for these patients is not disproportionate.
Admission to the ICU usually occurs in the setting of acute illness with organ dysfunction or for monitoring in the perioperative period, with the aim of preventing or reversing acute deterioration and increasing chances of survival (1). Although some patients have treatment limitations in place on admission (2), survival remains the aim of treatment. For those who die, end-of-life care in ICU typically occurs after a trial of active treatment has failed, with the majority of deaths preceded by a decision to withhold or withdraw therapy (3–6).
In contrast, some patients may be admitted to ICU with the known expectation of imminent death. Reasons for such admissions may include facilitation of organ donation (7–10) and provision of palliative care to patients unable to be managed elsewhere. Even though resources may be limited, facilities uniquely available in ICUs may offer benefits to patients at the end of life (11) and may provide a better environment for difficult discussions with families (12).
There is little published information about these patients. Our aim was to determine the characteristics, resource use, and outcomes of patients admitted to Australian and New Zealand ICUs with the intention of managing end-of-life care, including organ donation. We hypothesized that the numbers of patients admitted for “palliative care of a dying patient” or “potential organ donation” had increased over recent years and that these patients consumed a disproportionate amount of resources as measured by mean days in ICU compared with actively managed ICU admissions.
MATERIALS AND METHODS
We conducted a retrospective analysis of prospectively collected binational registry data from the Australian and New Zealand Intensive Care Society (ANZICS) Adult Patient Database (APD) with a nested cohort analysis of patients admitted to one major tertiary metropolitan hospital to further investigate causes and circumstances for ICU admission.
Data Source 1—ANZICS APD
The ANZICS APD is one of four clinical quality registries run by the ANZICS Centre for Outcome and Resource Evaluation (13) and collects patient level data on admissions to adult ICUs in Australia and New Zealand. Since January 2007, the ANZICS APD has recorded treatment goals on admission to ICU in four categories as follows: “full active management,” “treatment limitation order,” “palliative care of a dying patient”, and “potential organ donation”. All ICU admissions between January 1, 2007, and December 31, 2016, were examined. Those without recorded treatment goals on admission to ICU were excluded. All patients whose primary admission was for “palliative care of a dying patient” or for “potential organ donation” were extracted. If the palliative admission to ICU was a readmission episode, this was included but only if the original ICU admission had been for active treatment. Otherwise all readmission episodes were excluded.
Variables extracted included age, diagnosis on admission, comorbidities, Acute Physiology and Chronic Health Evaluation II and III scores, source of hospital and ICU admission, length of ICU and hospital stay, and discharge destination. Outcomes considered included in-hospital mortality rates and the proportion of patients discharged home or to a rehabilitation facility. Length of stay in ICU was the outcome examined for consideration of resource use.
Data Source 2—The Alfred Hospital, Melbourne, VIC, Australia
To obtain additional information about the context and reasons for admission, a nested cohort analysis was undertaken of patients admitted for “palliative care of a dying patient” or “potential organ donation” to the ICU at The Alfred Hospital. The Alfred Hospital is a tertiary-level, university-affiliated hospital in metropolitan Melbourne. The 45-bed ICU facility admits approximately 3,000 patients per year and is the regional referral center for heart and lung transplantation, mechanical circulatory assist devices, burns, cystic fibrosis, HIV, and one of two adult trauma and bone marrow transplantation centers in the state of Victoria. Medical notes, charts, hospital administrative, and ICU databases were examined using a prespecified data abstraction template. Reasons and circumstances for admission to ICU (which were not mutually exclusive) were grouped and reported as number and proportion.
Statistical Analysis
The annual prevalence of patients admitted for “palliative care of a dying patient” or “potential organ donation” as a proportion of overall admissions listed in the ANZICS APD over the study period was examined. Characteristics and outcomes of these two groups were compared. Second, a composite group containing both “palliative care of a dying patient” and “potential organ donation” patients was compared with actively managed ICU admissions. Comparison of patients admitted for “palliative care of a dying patient” with those admitted for “potential organ donation” at The Alfred Hospital is also provided in Appendix Table 1 (Supplemental Digital Content 1, http://links.lww.com/CCM/C777).
All data were assessed for normality. Categorical, parametric, and nonparametric data were reported as number (%), mean (sd), or median (interquartile range [IQR]), respectively. Comparisons were undertaken with chi-square, t, or Wilcoxon tests as appropriate depending on distribution of data. Changes over time were assessed by fitting a linear regression line to annual proportions and further verified using the trend modification of the Wilcoxon test. Two-sided p values less than 0.05 were considered statistically significant. All analyses were performed using STATA SE, Version 14 (StataCorp, College Station, TX).
The study was approved by the Alfred Hospital Ethics Committee (number 471/13).
RESULTS
ICU Admissions Throughout Australia and New Zealand (Data Source 1—ANZICS APD)
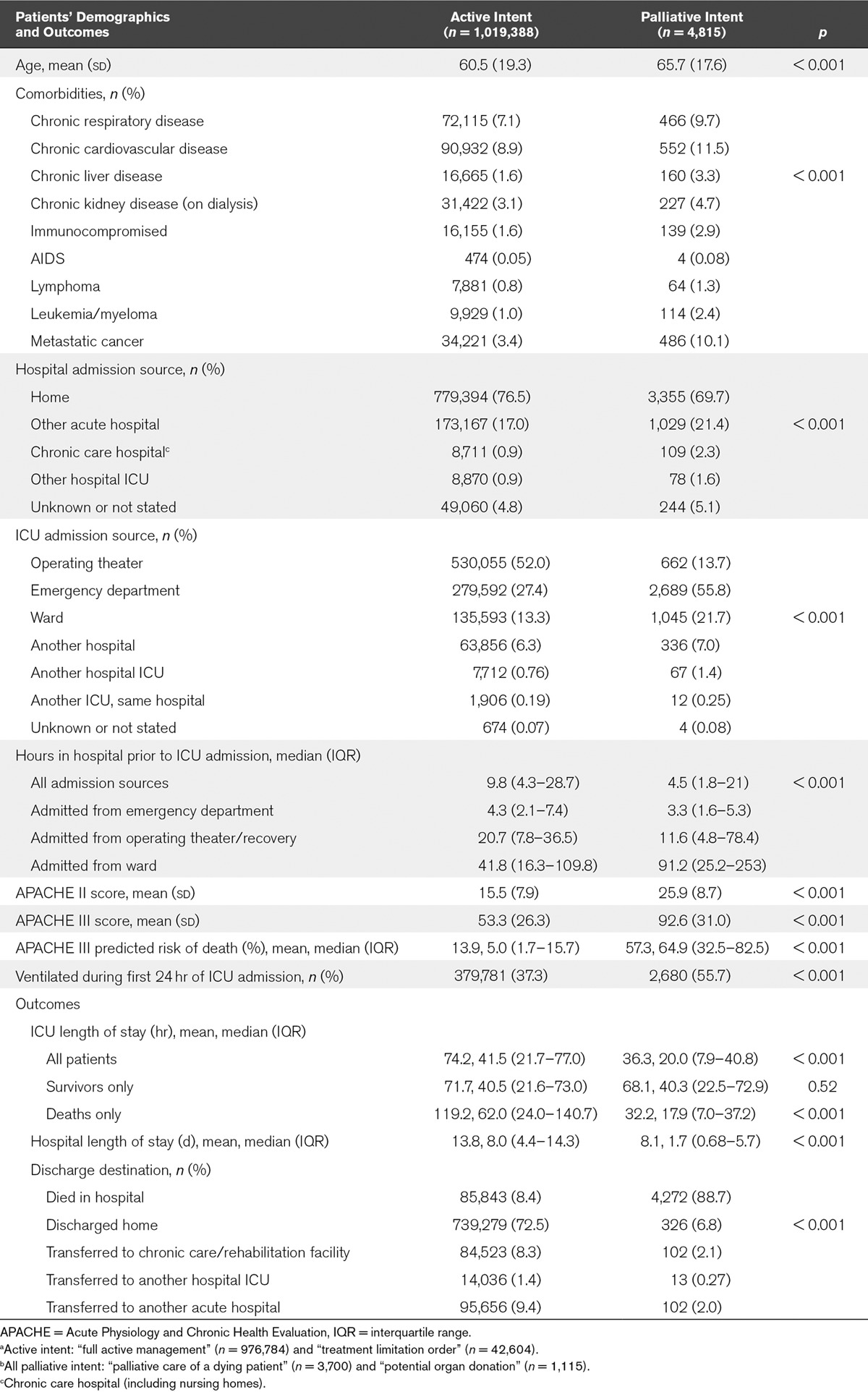
Between January 1, 2007, and December 31, 2016, there were 1,205,153 admissions to 179 ICUs submitted to the ANZICS APD (Appendix Figure 1, Supplemental Digital Content 1, http://links.lww.com/CCM/C777). After exclusion of actively managed readmission episodes, and patients with no treatment goals or hospital outcome listed, there were 1,024,203 ICU admission episodes at 177 ICUs, of whom 3,700 (0.4%) were admitted for “palliative care of a dying patient” and 1,115 (0.1%) for “potential organ donation”. Of these 4,815 patients, 230 (4.8%) had previously had an active admission to ICU. Mortality in each group was 86.6% and 95.9%, respectively, compared to 8.4% in those admitted with active intent. Overall, patients admitted for “palliative care of a dying patient” or for “potential organ donation” had shorter durations of ICU stay (mean hours, 36.3; median, 20.0; IQR, 7.9–40.8) than those admitted with active intent (mean hours, 74.2; median, 41.5; IQR, 21.7–77.0), although survivors in all groups had similar lengths of stay in ICU (Table 1).
TABLE 1.
Comparison of “Active Intent”a and “All Palliative Intent”b Cohorts From the Australian and New Zealand Intensive Care Society Adult Patient Database
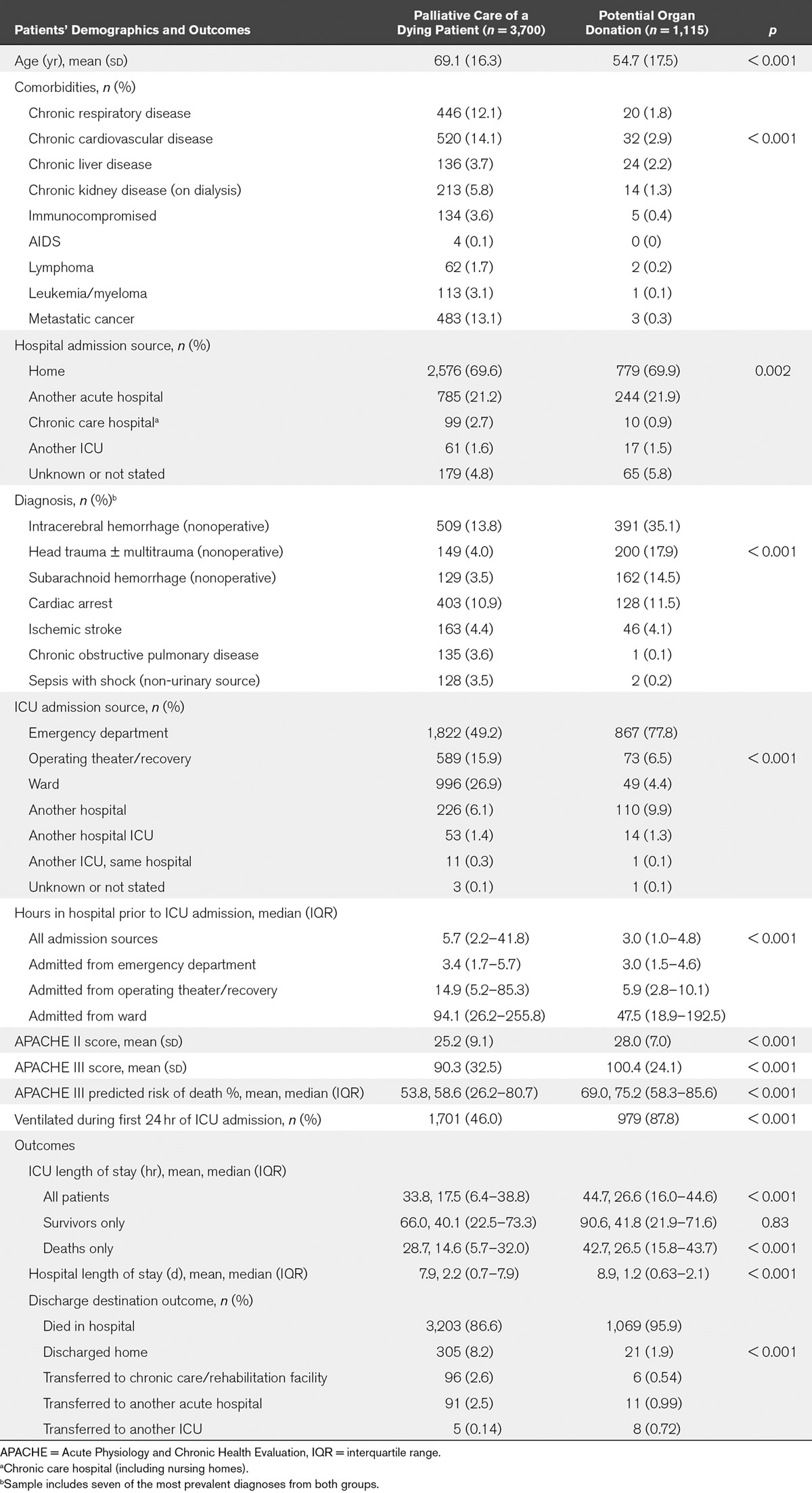
Although there was an increase in absolute numbers, the proportion of all ICU patients admitted for “palliative care of a dying patient” showed no change over the study period (179 [0.34%] in 2007, 551 [0.40%] in 2016; p = 0.75). However, there was an increase in both absolute number and proportion of ICU patients admitted for “potential organ donation” (44 [0.08%] in 2007, 174 [0.13%] in 2016; p < 0.001) (Fig. 1). Patients admitted for “potential organ donation” were younger, had fewer comorbidities, and were more commonly admitted due to neurologic conditions compared with the “palliative care of a dying patient” cohort (Table 2). Although inhospital mortality was high, 305 (8.2%) and 21 (1.9%) patients were recorded as discharged home in the “palliative care of a dying patient” and “potential organ donation” groups, respectively, as well as 96 (2.6%) and six (0.54%) patients transferred to a chronic care/rehabilitation facility, respectively.
Figure 1.
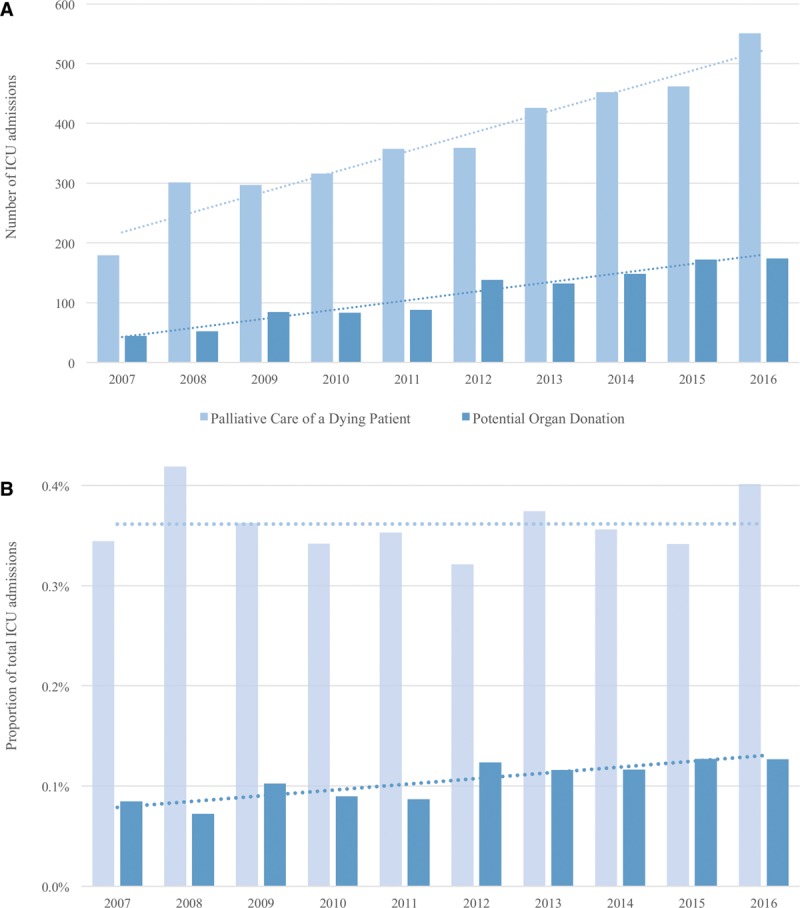
Annual prevalence (A) and proportion (B) of “palliative care of a dying patient” and “potential organ donation” admissions to ICU per year, 2007–2016 in the Australian and New Zealand Intensive Care Society Adult Patient Database. p value less than 0.001 for change in proportion over time in “potential organ donation” cohort. p value 0.75 for change in proportion over time in “palliative care of a dying patient” cohort.
TABLE 2.
Comparison of “Palliative Care of a Dying Patient” and “Potential Organ Donation” Cohorts—Demographics and Outcomes from the Australian and New Zealand Intensive Care Society Adult Patient Database
ICU Admissions at The Alfred Hospital, Melbourne, VIC, Australia (Data Source 2)
Two hundred twenty patients at The Alfred Hospital were listed as having been admitted for “palliative care of a dying patient” or “potential organ donation”. Two patients initially coded as “potential organ donation” were considered to have had active treatment, although organ donation was later considered in both cases. Both subsequently died in ICU. Twenty-six admissions initially coded as “palliative care of a dying patient” were considered to have had full active treatment (nine patients) or active treatment with limitations (17 patients). Of these, 77% (20/26) subsequently died. This left 192 patients in whom circumstances and reasons for admission were examined.
Patients admitted to The Alfred ICU for “potential organ donation” were younger and more commonly admitted from the emergency department when compared with those admitted for “palliative care of a dying patient”. Median duration of stay in ICU was less than 24 hours in both groups. All 116 patients admitted for “potential organ donation” died in ICU. One (1.3%) of the 76 admissions for “palliative care of a dying patient” was discharged alive to an aged care facility (Appendix Table 1, Supplemental Digital Content 2, http://links.lww.com/CCM/C778).
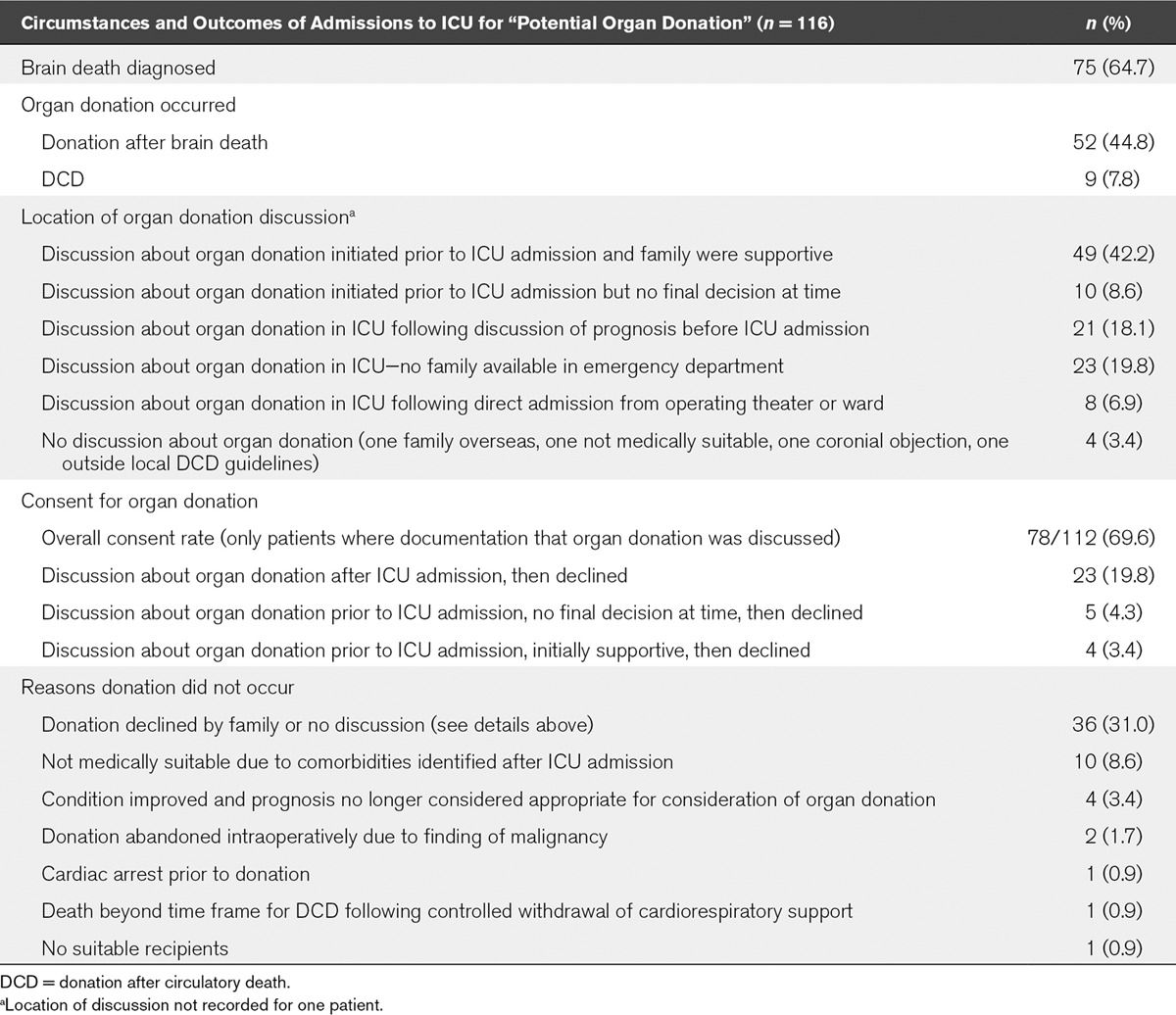
Reasons for and Circumstances of Admission to The Alfred Hospital ICU
The most common reason for admission to ICU for palliative care of a dying patient was to allow time for arrival of family members or to facilitate further discussions about goals of treatment (Table 3). A common factor was the requirement for ongoing management of invasive mechanical ventilation initiated outside ICU (68 patients, 89.5%). Of the 116 admissions for “potential organ donation”, successful organ donation occurred in 61 patients (52.6%) (Table 4). The most common reason that donation did not eventuate was that family declined to proceed, though in four cases, the patient’s condition improved so that organ donation was no longer considered appropriate. All these patients subsequently died in ICU.
TABLE 3.
Reasons for and Circumstances of Admission for “Palliative Care of a Dying Patient” to the ICU at The Alfred Hospital (75 Patientsa)
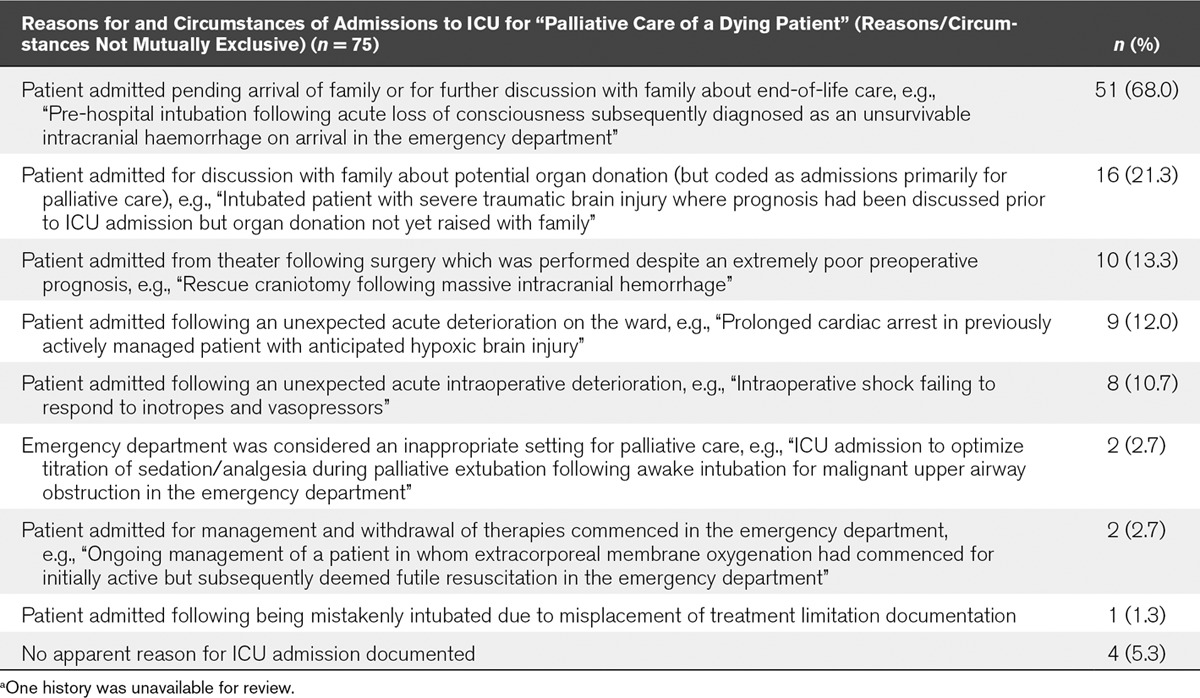
TABLE 4.
Circumstances and Outcomes of Admissions for “Potential Organ Donation” to the ICU at The Alfred Hospital (116 Patients)
DISCUSSION
Patients whose goal of admission to ICU was to facilitate end-of-life care comprised a small proportion of all ICU admissions. They had shorter ICU stays than actively managed patients suggesting that ICU resource use was not disproportionate, as initially hypothesized. Although mortality was expectedly high, survivors were occasionally identified. Over the 10-year period, there was an increasing proportion of ICU admissions admitted for “potential organ donation”, although the proportion admitted specifically for “palliative care of a dying patient” remained constant.
Relationship to Previous Studies and Implications of Study Findings
Palliative care is recognized as an essential component of intensive care medicine (11, 14, 15). ICU may be a more appropriate setting for palliative care in certain cases, for example, where aggressive symptom control is required during withdrawal of mechanical ventilation (16), aided by higher nurse-to-patient ratios (11), or for family considerations (12). However, there is limited literature describing patients admitted to ICU specifically for palliative care, with current literature more focused on palliative management following failed active treatment.
In the nested cohort study, the most common reason for ICU admission for “palliative care of a dying patient” was to enable communication with the patient’s family about goals of care, after ICU therapies had already been initiated. Family communication is considered a vital aspect of ICU and end-of-life care, and is rated as one of the most important aspects of ICU care by families (15, 17–20). When life-sustaining treatments are withdrawn, most patients die quickly (21–23). Their continuation affords family members an opportunity to be with loved ones and facilitates discussion about end-of-life care (12, 14). The ICU may be a better environment to provide this care than emergency departments which are potentially busy, lack privacy, comfort, and space for family members, and have competing time pressures for staff (12, 24).
In our study, patients admitted for “palliative care of a dying patient” or “potential organ donation” had shorter ICU and hospital stays than those admitted for active management. Although information on therapies provided in the ICU were not available, it is possible that they also required less costly treatment, through lower use of antibiotics, infusions, and organ supports such as renal replacement therapy (25). Although we cannot determine whether clinicians could have managed these patients outside the ICU, the infrequent but consistent occurrence of ICU admission over the 10 years examined suggests clinicians may consider it an appropriate use of resources in certain situations. It may also reflect existing local practices shaped by available resources inside and outside the ICU.
In our study, admissions for “potential organ donation” increased as a proportion of overall ICU admissions. The study period coincided with improved funding and legislative support for the donation sector in Australia (26) which likely increased awareness among clinicians and the community, leading to improved identification of potential donors. ICU admission of potential organ donors may yield more quality-adjusted life-years per ICU bed-day for the community compared with expected benefits for ICU patients expected to survive (10). A significant group of unrealized potential organ donors in Australia are those with imminent brain death who have treatment withdrawn outside the ICU (27). Our study demonstrated that most families were supportive of potential organ donation when it was discussed prior to admission and that admission to ICU for “palliative care of a dying patient” also facilitated discussion about organ donation in over 20% of patients. Thus, our study potentially supports ICU admission for consideration of organ donation as an effective use of scarce resources.
Survival following withdrawal of life-sustaining treatments in ICU (3, 21, 28, 29) and following referral from the emergency department for organ donation (30) have been previously reported. Initial predictions about prognosis may be unclear, evolve, change, and subsequently be proven wrong, which highlights the potential difficulty of making such decisions at a single point in time (12). In our study, approximately 10% and 2.4% of patients in the “palliative care of a dying patient” and “potential organ donation” groups were listed as either discharged home or to a chronic care/rehabilitation facility, although only one survivor was noted in the nested cohort study from The Alfred Hospital. Survivors spent the same time in ICU as patients admitted for active management. Thus, although there was no evidence of disproportionate resource use in ICU as measured by length of stay, no conclusions about ongoing healthcare requirements for survivors can be determined from this study.
In only one patient from the nested cohort study was there a mistaken intubation with a treatment limitation order in place. Other than this case, the number of avoidable ICU admissions, and potential resources saved, could not be determined. Most patients were admitted following a new diagnosis, often made after institution of ICU therapies, and unrelated to preexisting comorbidities.
Strengths and Limitations
The strengths of our study were the large international database used with a wide sampling of patients over a lengthy period of time, and supplementary in-depth data from a nested cohort study. It is likely representative of and relevant to intensive care practice in Australia and New Zealand. To our knowledge, this is the first study to provide this objective data about admissions for end-of-life care in ICU.
Study limitations include its retrospective nature. The extent and impact of data inaccuracy are unknown. Ten percent of total eligible ICU admissions were excluded due to absence of listed treatment goals. Outcome data were limited, and functional status of survivors was unknown. The extent to which survivors may be explained by miscoding was unknown. It was not possible to determine whether a decision to avoid intubation contributed to the low rate in the “palliative care of a dying patient” cohort. Our nested cohort demonstrated higher rates of intubation, suggesting this may have been a function of the ANZICS data collection method where ventilation status was known only if an arterial blood gas was available. In addition, the greater proportion of ICU admissions coded as “potential organ donation” compared with “palliative care of a dying patient” may limit wider applicability of the findings from the nested cohort.
Although ICU length of stay is strongly correlated with ICU costs (31), no specific information was available about therapies provided in or available outside of the ICU. No inferences can be made about institutions’ potential ability to deliver end-of-life care to patients in whom invasive therapies have already been commenced outside ICU. No information about advanced directives was available. The Alfred Hospital is a trauma, neurosurgical, cardiothoracic transplant, and burns center which may limit generalizability to other ICUs. Lack of definitive criteria for classification is also a limitation. Application of strict criteria within the nested single-center cohort resulted in exclusion of 28 patients in whom we determined active treatment had been provided. High mortality in excluded patients suggested concerns about futility were present at ICU admission. Overlap also appeared to exist between “palliative care of a dying patient” and “potential organ donation” cohorts. Separation into distinct groups was dependent on arbitrary classification by the treating doctor.
Future Studies
Potential areas of future study should consider therapies needed to care for these patients, functional and dependency status of survivors, as well as whether the ICU is best suited to deliver this care from humanistic and economic perspectives, or if therapies already initiated can be delivered in non-ICU settings.
CONCLUSIONS
Patients admitted to ICU for “palliative care of a dying patient” or “potential organ donation” represent a small proportion of ICU admissions. Despite increases in absolute numbers, only the “potential organ donation” cohort showed an increasing proportion of total ICU admissions. Both groups have short lengths of stay in ICU and do not appear to use more ICU resources than actively managed patients. Facilitating family discussion about goals of treatment and organ donation represented the most common need for intensive care admission.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Dr. Anderson is a Hospital Medical Director for organ donation at The Alfred Hospital in Victoria. Prof. Pilcher is a medical advisor for DonateLife in Victoria. The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Adhikari NK, Fowler RA, Bhagwanjee S, et al. Critical care and the global burden of critical illness in adults. Lancet 2010; 376:1339–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Godfrey G, Pilcher D, Hilton A, et al. Treatment limitations at admission to intensive care units in Australia and New Zealand: Prevalence, outcomes, and resource use. Crit Care Med 2012; 40:2082–2089. [DOI] [PubMed] [Google Scholar]
- 3.Cook D, Rocker G, Marshall J, et al. ; Level of Care Study Investigators and the Canadian Critical Care Trials Group: Withdrawal of mechanical ventilation in anticipation of death in the intensive care unit. N Engl J Med 2003; 349:1123–1132. [DOI] [PubMed] [Google Scholar]
- 4.Sprung CL, Cohen SL, Sjokvist P, et al. ; Ethicus Study Group: End-of-life practices in European intensive care units: The Ethicus Study. JAMA 2003; 290:790–797. [DOI] [PubMed] [Google Scholar]
- 5.Brieva JL, Cooray P, Rowley M. Withholding and withdrawal of life-sustaining therapies in intensive care: An Australian experience. Crit Care Resusc 2009; 11:266–268. [PubMed] [Google Scholar]
- 6.Prendergast TJ, Luce JM. Increasing incidence of withholding and withdrawal of life support from the critically ill. Am J Respir Crit Care Med 1997; 155:15–20. [DOI] [PubMed] [Google Scholar]
- 7.British Medical Association: Building on Progress: Where Next for Organ Donation Policy in the UK? 2012. Available at: http://www.bma.org.uk/-/media/files/pdfs/working%20for%20change/improving%20health/organdonation_buildingonprogressfebruary2012.pdf. Accessed November 1, 2015
- 8.Opdam HI, Silvester W. Identifying the potential organ donor: An audit of hospital deaths. Intensive Care Med 2004; 30:1390–1397. [DOI] [PubMed] [Google Scholar]
- 9.Bendorf A, Kerridge IH, Stewart C. Intimacy or utility? Organ donation and the choice between palliation and ventilation. Crit Care 2013; 17:316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nunnink L, Cook DA. Palliative ICU beds for potential organ donors: An effective use of resources based on quality-adjusted life-years gained. Crit Care Resusc 2016; 18:37–42. [PubMed] [Google Scholar]
- 11.Nelson JE, Danis M. End-of-life care in the intensive care unit: Where are we now? Crit Care Med 2001; 29:N2–N9. [DOI] [PubMed] [Google Scholar]
- 12.Manara A, Thomas I, Harding R. A case for stopping the early withdrawal of life sustaining therapies in patients with devastating brain injuries. J Intensive Care Soc 2016; 17:295–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Australian and New Zealand Intensive Care Society Centre for Outcome and Resource Evaluation Annual Report 2014/15. 2016Melbourne, VIC, ANZICS. [Google Scholar]
- 14.Faber-Langendoen K, Lanken PN. Dying patients in the intensive care unit: Forgoing treatment, maintaining care. Ann Intern Med 2000; 133:886–893. [DOI] [PubMed] [Google Scholar]
- 15.Truog RD, Campbell ML, Curtis JR, et al. ; American Academy of Critical Care Medicine: Recommendations for end-of-life care in the intensive care unit: A consensus statement by the American College [corrected] of Critical Care Medicine. Crit Care Med 2008; 36:953–963. [DOI] [PubMed] [Google Scholar]
- 16.American Thoracic Society: Fair allocation of intensive care resources. Am J Resp Crit Care Med 1997; 156:1282–1301. [DOI] [PubMed] [Google Scholar]
- 17.Heyland DK, Rocker GM, Dodek PM, et al. Family satisfaction with care in the intensive care unit: Results of a multiple center study. Crit Care Med 2002; 30:1413–1418. [DOI] [PubMed] [Google Scholar]
- 18.Lautrette A, Darmon M, Megarbane B, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med 2007; 356:469–478. [DOI] [PubMed] [Google Scholar]
- 19.Nelson JE, Puntillo KA, Pronovost PJ, et al. In their own words: Patients and families define high-quality palliative care in the intensive care unit. Crit Care Med 2010; 38:808–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Curtis JR, Patrick DL, Shannon SE, et al. The family conference as a focus to improve communication about end-of-life care in the intensive care unit: Opportunities for improvement. Crit Care Med 2001; 29:N26–N33. [DOI] [PubMed] [Google Scholar]
- 21.Coleman NL, Brieva JL, Crowfoot E. Prediction of death after withdrawal of life-sustaining treatments. Crit Care Resusc 2008; 10:278–284. [PubMed] [Google Scholar]
- 22.DeVita MA, Brooks MM, Zawistowski C, et al. Donors after cardiac death: Validation of identification criteria (DVIC) study for predictors of rapid death. Am J Transplant 2008; 8:432–441. [DOI] [PubMed] [Google Scholar]
- 23.Keenan SP, Busche KD, Chen LM, et al. A retrospective review of a large cohort of patients undergoing the process of withholding or withdrawal of life support. Crit Care Med 1997; 25:1324–1331. [DOI] [PubMed] [Google Scholar]
- 24.Forero R, McDonnell G, Gallego B, et al. A literature review on care at the end-of-life in the emergency department. Emerg Med Int 2012; 2012:486516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Campbell ML, Guzman JA. Impact of a proactive approach to improve end-of-life care in a medical ICU. Chest 2003; 123:266–271. [DOI] [PubMed] [Google Scholar]
- 26.Australian Organ and Tissue Donation and Transplantation Authority Act 2008. Vol. 2008122 . Available at: https://www.legislation.gov.au/Details/C2008A00122. Accessed August 7, 2017 [Google Scholar]
- 27.Opdam HI, Silvester W. Potential for organ donation in Victoria: An audit of hospital deaths. Med J Aust 2006; 185:250–254. [DOI] [PubMed] [Google Scholar]
- 28.Azoulay E, Metnitz B, Sprung CL, et al. ; SAPS 3 Investigators: End-of-life practices in 282 intensive care units: Data from the SAPS 3 database. Intensive Care Med 2009; 35:623–630. [DOI] [PubMed] [Google Scholar]
- 29.Nolin T, Andersson R. Withdrawal of medical treatment in the ICU. A cohort study of 318 cases during 1994-2000. Acta Anaesthesiol Scand 2003; 47:501–507. [DOI] [PubMed] [Google Scholar]
- 30.Michael GE, O’Connor RE. The importance of emergency medicine in organ donation: Successful donation is more likely when potential donors are referred from the emergency department. Acad Emerg Med 2009; 16:850–858. [DOI] [PubMed] [Google Scholar]
- 31.Graf J, Graf C, Janssens U. Analysis of resource use and cost-generating factors in a German medical intensive care unit employing the Therapeutic Intervention Scoring System (TISS-28). Intensive Care Med 2002; 28:324–331. [DOI] [PubMed] [Google Scholar]


