ABSTRACT
Human papilloma virus (HPV)-induced cervical cancer constitutively expresses viral E6/E7 oncoproteins and is an excellent target for T cell-based immunotherapy. However, not all tumor-infiltrating T cells confer equal benefit to patients, with epithelial T cells being superior to stromal T cells.
To assess whether the epithelial T cell biomarker CD103 could specifically discriminate the beneficial antitumor T cells, association of CD103 with clinicopathological variables and outcome was analyzed in the TCGA cervical cancer data set (n = 304) and by immunohistochemistry (IHC) in an independent cohort (n = 460). Localization of CD103+ cells in the tumor was assessed by immunofluorescence. Furthermore, use of CD103 as a response biomarker was assessed in an in vivo E6/E7+ tumor model.
Our results show that CD103 gene expression was strongly correlated with cytotoxic T cell markers (e.g. CD8/GZMB/PD1) in the TCGA series. In line with this, CD103+ cells in the IHC series co-expressed CD8 and were preferentially located in cervical tumor epithelium. High CD103+ cell infiltration was strongly associated with an improved prognosis in both series, and appeared to be a better predictor of outcome than CD8. Interestingly, the prognostic benefit of CD103 in both series seemed limited to patients receiving radiotherapy. In a preclinical mouse model, HPV E6/E7-targeted therapeutic vaccination in combination with radiotherapy increased the intratumoral number of CD103+ CD8+ T cells, providing a potential mechanistic basis for our results.
In conclusion, CD103 is a promising marker for rapid assessment of tumor-reactive T cell infiltration of cervical cancers and a promising response biomarker for E6/E7-targeted immunotherapy.
KEYWORDS: CD103, cervical cancer, intraepithelial T cells, therapeutic vaccination, tumor-infiltrating lymphocytes
Introduction
Cervical cancer is the most common gynecologic malignancy and the second most common malignancy afflicting women worldwide (globcan). The development of cervical cancer is largely dependent on persistent human papilloma virus (HPV) infections, with HPV16 and 18 being the dominant subtypes.1,2 As a virally-induced cancer, control of cervical cancer development appears at least partly mediated by the immune system,3-5 and multiple studies have demonstrated a clear benefit of T cell infiltration on survival in cervical cancer patients.6-9
The malignant transformation of cervical epithelial cells by HPVs involves integration of viral oncogenes, such as HPV E6 and E7, into the cellular DNA. Subsequent expression of these HPV E6 and E7 proteins inhibits the tumor suppressors p53 and pRb, respectively, resulting in a loss of cell cycle control, proliferation and malignant transformation. Importantly, sustained expression of E6 and/or E7 is required for maintaining a malignant cellular phenotype in this setting.10 E6/E7 therefore represent bona fide cancer-specific antigens that can be targeted for cancer immunotherapy. Indeed, T cell-based therapies targeting E6/E7 have met with clinical success in early trials.11-21 As readout for therapeutic efficacy of these approaches, systemic immune monitoring in the blood is usually used alone, or in combination with monitoring of CD8+ T cell tumor infiltration. Herein, a distinction is frequently made between CD8+ TIL that infiltrate the epithelial cancer nests or TIL that infiltrate the surrounding stroma. This distinction is based on the known need for contact between TIL and cancer cells for efficient induction of cell death, and the observed stronger association of epithelial TIL compared with stromal TIL with regards to patient prognosis.22 However, this approach relies on distinguishing epithelial from stromal regions, a non-trivial feat in many tumors. The identification of a biomarker for identifying tumor-reactive cells would therefore be of substantial benefit.
Recently, we and others have demonstrated that CD103, also known as the αE integrin subunit, delineates prognostically favorable intraepithelial CD8+ tumor-infiltrating lymphocytes (TIL) in endometrial, ovarian, lung and bladder cancer.23-27 In contrast to the prognostic benefit observed for CD8+ TIL,28,29 this survival benefit was also evident when quantifying the total number of CD103+ TIL present within the tumor.23-27 This finding is in line with the proposed restricted expression of CD103 on CD8+ TIL that have infiltrated the tumor epithelium.
The aim of this study was therefore to determine whether expression of CD103 defines the intraepithelial CD8+ TIL in cervical cancer and whether CD103+ TIL are associated with improved prognosis. Further, we explored the mechanistic basis of our findings in a preclinical mouse model and determined whether CD103 infiltration could be used as a response biomarker for therapeutic HPV16 E6/E7-targeted immunotherapy.
Results
Expression of CD103 is an independent prognostic factor in cervical cancer and strongly associated with an immune signature
To investigate the utility of CD103 as a biomarker of an anti-tumor T cell response in cervical cancer, we first analyzed expression of CD103 (ITGAE) mRNA in The Cancer Genome Atlas (TCGA) cervical cancer data set. CD103 gene expression was strongly correlated with the expression of T cell markers (CD3, CD2), exhaustion molecules (PD1, TIGIT), antigen-presenting molecules (HLA-DR, -DQ) and B cell markers (CD19) suggesting that increased CD103 expression defines a group of immunologically “hot” tumors in this cervical cancer cohort (Fig. 1A). High CD103 expression (>median) was associated with younger patient age (49.9 vs. 46.5 years, P = 0.03, t-test) and squamous histology (P = 0.026, Fisher exact test), though no association with disease stage, tumor differentiation or treatment use was observed (Supplementary Table 1). Notably, CD103 expression greater than the median was associated with significantly improved cancer-specific survival both in univariable analysis (Fig. 1B; HR = 0.56, 95%CI = 0.34–0.92, P = 0.02) and after adjusting for disease stage in multivariable analysis (HR = 0.55, 95%CI = 0.32–0.94, P = 0.03) (Supplementary Table 2). By contrast, increased expression of CD8A was not significantly associated with cancer-specific survival in this population (Supplementary Table 2). Exploratory analysis according to treatment modality (surgery vs. radio(chemo)therapy) suggested that the prognostic benefit of increased CD103 expression was observed in patients treated with radiotherapy, but not in patients treated with surgery alone (Fig. 1C (p = 0.015) and 1D (p = 0.47), respectively).
Figure 1.
CD103-associated immune responses and clinical outcome in TCGA cervical cancers. A) Heatmap showing expression of immunologic genes according to tumor histology and ordered by CD103 (ITGAE) expression. RSEM-normalized RNAseq expression data were log2 transformed, mean centered and assigned unit variance. For each gene, the correlation with CD103 expression was calculated by spearman rho. B-D) Kaplan–Meier curves demonstrating cancer survival of patients in the TCGA series dichotomized by median CD103 (ITGAE) expression for the total cohort (B) and according to radiotherapy treatment (C, D) (note that survival data were not available for 13 cases). Comparison between groups was made by the 2-sided log-rank test.
CD103+ TIL are associated with prolonged disease-specific and disease-free survival in cervical cancer patients
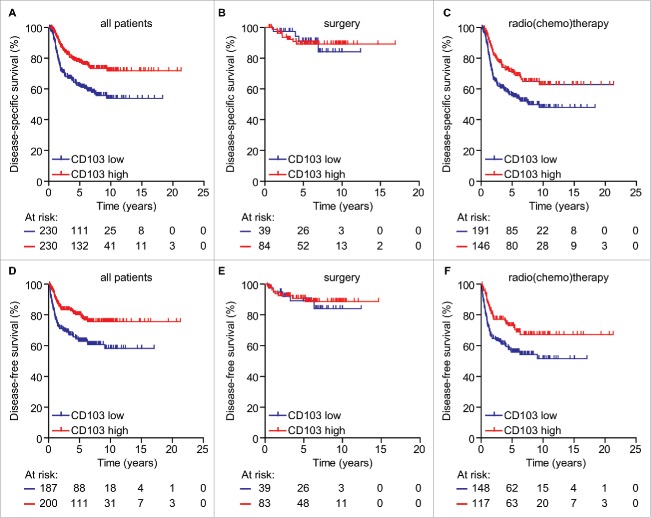
To validate our findings from the TCGA data set, we analyzed infiltration of CD103+ cells by immunohistochemistry (IHC) in an independent cohort of 630 cervical cancer patients. Patients were included for quantification of CD103+ TIL if the tissue microarray (TMA) used contained at least 2 cores with a minimum of 20% tumor. Representative tumor cores were available from 460 patients. Patient and tumor characteristics did not differ between analyzed and excluded patients (data not shown). Table 1 shows the patient and tumor characteristics of the patients eligible for CD103 quantification. Of the 460 included patients, 123 were treated with surgery alone and 337 were treated with radio(chemo)therapy (R(C)T) (alone or in combination with surgery). The surgery cohort consisted of patients diagnosed with Fédération Internationale de Gynécologie Obstétrique (FIGO) stages IB1-IIA. The R(C)T cohort consisted of patients diagnosed with FIGO stages IB1-IVA. The majority of patients in the surgery cohort were diagnosed with FIGO IB1 (n = 86; 69.9%) and the majority of patients in the R(C)T cohort were diagnosed with FIGO stage IIB (n = 112; 33.2%). Of the surgery and R(C)T cohort, 64.2% (n = 79) and 78.9% (n = 266) of tumors were squamous cell carcinomas (SCC) and 17.9% (n = 22) and 13.1% (n = 44) were adenocarcinomas (AC), respectively. The median follow-up time was 5.12 y with a maximum of 21.31 years. Positive staining for CD103+ TIL was equally present in SCC, AC and other subtypes (Supplementary Figure S1A). Interestingly, the median infiltration of CD103+ cells in patients that received radio(chemo)therapy was significantly lower than for patients that received surgery alone (Table 1; median surgery 55 vs. 24 R(C)T; p < 0.0001). Further, within the R(C)T cohort, patients with a higher FIGO stage were characterized by a lower number of CD103+ cells (Table 1; median 38 in IB1 vs. 20 in IIB and 11 in IIIB; p < 0.05 and p < 0.01, respectively). Likewise, adenocarcinomas in the R(C)T cohort were infiltrated less than squamous cell carcinomas (Table 1; median 25 vs. 13; p < 0.05). To analyze survival, patients were dichotomized based on high or low/no infiltration and the cohorts treated with either surgery or radio(chemo)therapy were analyzed together or separately. The cut-off was determined based on median CD103+TIL infiltration of the total cohort and was 29 cells/mm2. Disease-specific survival (DSS) analysis based on infiltration of CD103+ cells revealed a significant improved survival in the total cohort (Fig. 2A; p < 0.0001), a nonsignificant improvement of survival in the cohort treated with surgery only (Fig. 2B; p = 0.9947) and a significant improvement of survival in the radio(chemo)therapy cohort (Fig. 2C; p = 0.0032). Similar results were obtained when determining disease-free survival (Fig. 2D–E; p = 0.0004 for the total cohort, p = 0.7350 for surgery alone, and p = 0.0072 for R(C)T). In analysis of the total cohort, additional prognostic factors were stage (HR = 4.19, p < 0.001), use of radio(chemo)therapy (HR = 1.49, p < 0.001) and tumor diameter (HR = 2.9; p < 0.001) (Supplementary Table 3). In multivariate analysis, stage (HR = 2.43, p < 0.006), use of radio(chemo)therapy (HR = 1.30, p < 0.001) and CD103+ cells (HR = 0.67, p < 0.027) were independent prognostic factors (Supplementary Table 3).
Table 1.
Patient characteristics of the IHC cohort.
| Variables N = 460 | Surgery n (%) | CD103 median (range) | (chemo-) RT n (%) | CD103 median (range) | Total n (%) | CD103 median (range) |
|---|---|---|---|---|---|---|
| Patients | 123 (26.7) | 55 (1–367) | 337 (73.3) | 24 (0–256)**** | 460 (100) | 29 (0–367) |
| Age at diagnosis (in years) | ||||||
| Median | 41.2 | 50.7 | 47.7 | |||
| Range | (24.4–84.7) | (20.6–92.0) | (20.6–92.0) | |||
| FIGO stage | ||||||
| IA2 | 0 (0) | 0 (0) | 0 (0) | |||
| IB1 | 86 (69.9) | 52 (1–367) | 77 (22.8) | 38 (0–256) | 163 (35.4) | 50 (0–367) |
| IB2 | 20 (16.3) | 83 (7–286) | 50 (14.8) | 23 (2–204) | 70 (15.2) | 31 (2–286) |
| IIA | 17 (13.8) | 80 (10–203) | 60 (17.8) | 23 (0–215) | 77 (16.7) | 29 (0–215) |
| IIB | 0 (0) | 112 (33.2) | 20 (1–150) | 121 (24.3) | 20 (1–150) | |
| IIIA | 0 (0) | 4 (1.2) | 16 (5–34) | 4 (0.9) | 16 (5–34) | |
| IIIB | 0 (0) | 28 (8.3) | 11 (0–115) | 28 (6.1) | 11 (0–115) | |
| IVA | 0 (0) | 6 (21.8) | 16 (5–43) | 6 (1.3) | 16 (5–43) | |
| Histology | ||||||
| Squamous cell carcinoma | 79 (64.2) | 82 (7–367) | 266 (78.9) | 25 (1–215) | 345 (75.0) | 30 (1–367) |
| Adenocarcinoma | 22 (17.9) | 53 (6–246) | 44 (13.1) | 13 (0–256) | 66 (14.3) | 16 (0–256) |
| Other | 22 (17.9) | 33 (1–186) | 27 (8.0) | 36 (4–199) | 49 (10.7) | 36 (1–286) |
| Grade of differentiation | ||||||
| Good/moderate | 69 (56.1) | 55 (1–367) | 190 (56.4) | 24 (0–215) | 259 (56.3) | 29 ( 0–367) |
| Poor/undifferentiated | 51 (41.5) | 83 (3–303) | 129 (38.3) | 26 (0–256) | 180 (39.1) | 33 (0–304) |
| Unknown | 3 (2.4) | 52 (6–53) | 18 (5.3) | 14 (3–120) | 21 (4.6) | 16 (3–120) |
| Lymphangioinvasion | ||||||
| No | 74 (60.2) | 56 (5–367) | 173 (51.3) | 22 (0–216) | 247 (53.7) | 28 (3–367) |
| Yes | 49 (39.8) | 55 (1–304) | 105 (31.2) | 35 (2–256) | 154 (33.5) | 38 (1–304) |
| Unknown | 0 (0) | 59 (17.5) | 16 (0–128) | 59 (12.8) | 16 (0–128) | |
| Tumor diameter | ||||||
| 0–4 cm | 97 (78.9) | 52 (1–367) | 118 (35.0) | 36 (0–256) | 215 (46.7) | 40 (0–367) |
| ≥ 4 cm | 26 (21.1) | 86 (6–286) | 203 (60.2) | 18 (0–204) | 229 (49.9) | 22 (0–286) |
| Unknown | 0 (0) | 16 (4.7) | 33 (3–128) | 16 (3.5) | 33 (3–128) | |
| Treatment | ||||||
| WM | 123 (100) | 55 (1–367) | ||||
| WM+ post operative RT | 83 (24.6) | 42 (2–256) | ||||
| WM+ Post operative RCT | 14 (4.2)) | 33 (2–84) | ||||
| Primary RT | 115 (34.1) | 22 (0–198) | ||||
| Primary RCT | 125 (37.1) | 16 (0–133) | ||||
| Follow-up (in years) | ||||||
| Median | 5.62 | 4.81 | 5.12 | |||
| Range | (0.53–16.93) | (0.14–21.31) | (0.14–21.31) | |||
| Result last follow-up | ||||||
| No evidence of disease | 109 (88.6) | 77 (3–367) | 168 (49.9) | 29 (0–216) | 227 (60.2) | 38 (0–367) |
| Evidence of disease | 2 (1.6) | 92 (1–184) | 2 (0.6) | 52 (3–102) | 4 (0.9) | 52 (1–184) |
| Death of other disease | 0 (0) | 33 (9.8) | 24 (0–215) | 33 (7.2) | 24 (0–215) | |
| Death of disease | 12 (9.8) | 42 (7–170) | 134 (39.8) | 15 (0–256) | 146 (31.7) | 17 (0–256) |
Abbreviations: FIGO: International Federation of Gynecologists and Obstetricians
WM: Wertheim Meigs RT: Radiotherapy RCT: Radio-chemotherapy
Figure 2.
CD103+ TIL are strongly associated with survival in patients with cervical cancer. A) Disease-specific survival (DSS) of patients within the total cohort according to high or low infiltration of CD103+ cells (p < 0.0001). B) DSS of patients treated with surgery alone with a high or low infiltration of CD103+ cells. C) DSS of patients treated with radio(chemo)therapy and either a high or low infiltration of CD103+ cells. D) Disease-free survival (DFS) of patients within the total cohort according to high or low infiltration of CD103+ cells (p = 0.0004). E) DFS of patients treated with surgery alone with a high or low infiltration of CD103+ cells. F) DFS of patients treated with radio(chemo)therapy and either a high or low infiltration of CD103+ cells. Comparison between groups was made by the 2-sided log-rank test.
CD103 demarcates intraepithelial CD8+ TIL in cervical cancer
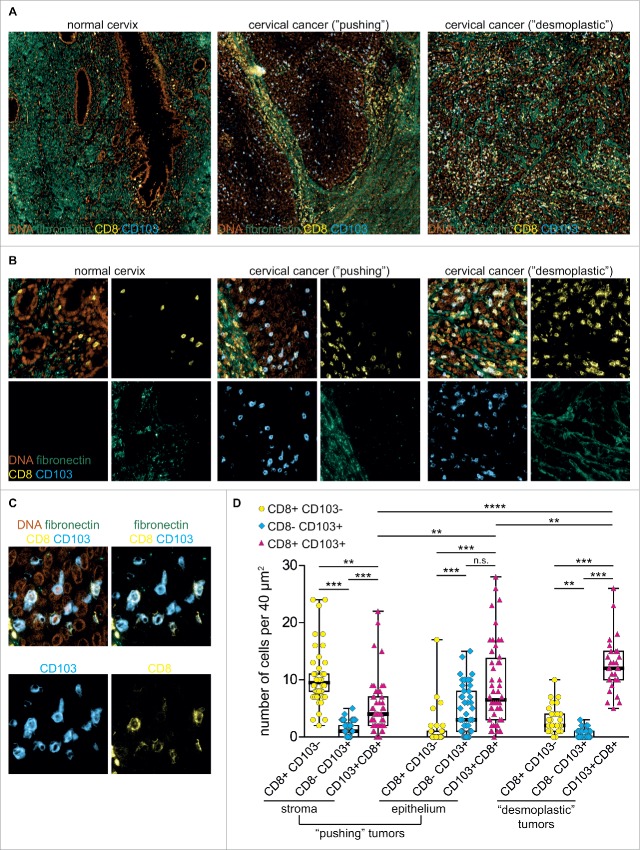
To investigate the localization and the phenotype of CD103+ TIL in cervical cancer, 18 tumors containing high levels of CD103+ TIL were selected, and tumor sections were stained for CD3, CD8, FoxP3, NKp46, fibronectin, DAPI, and CD103. For each section, cell infiltration was quantified for at least three independent regions. When examining the localization of the TIL we noticed different patterns of stromal infiltration into the epithelial areas previously classified as ‘pushing’ tumors and ‘desmoplastic’ tumors.30 Due to their distinctive nature, both types of tumors were subsequently analyzed separately (Fig. 3A).
Figure 3.
CD103 demarcates intraepithelial CD8+ TIL in cervical cancer tissue. A) Representative image of tissue from a normal cervix, from a patient with cervical cancer of the “pushing” type and of a patient with cervical cancer of the “desmoplastic” type stained with DAPI (DNA, orange), anti-CD8 (yellow), anti-CD103 (blue) and anti-fibronectin (green) antibodies. B) Representative images of CD8+ and CD103+ cells in the epithelial or stromal areas of 40 μm2 of tumor tissue. C) Representative single and multichannel images of tumor areas showing co-expression of CD8 and CD103. D) Quantification of single CD8+, single CD103+ or CD8+ CD103+ double-positive cells in the stroma and epithelial areas of the “pushing” tumors or total of the “desmoplastic” tumors. Each data point represents a cell count from a 40μm2 independent region of 18 independent tumors (3–6 in total per tumor section). Groups were compared by ANOVA using a Dunns post-test. *p < 0.05, **p < 0.01, ***p < 0.001.
Fluorescent staining of the pushing tumor type (n = 12) showed that CD103+ TIL were preferentially localized within the tumor epithelium and not within the tumor stroma (Fig. 3A). Furthermore, these intraepithelial CD103+ TIL largely co-expressed CD8 (Fig. 3B). A subset of CD103+ TIL in the pushing tumor type did not express CD8 (Fig. 3C–D). Further analysis of these CD8- CD103+ TIL showed that these cells did express CD3 and could therefore represent CD4+ regulatory T cells (Treg) or natural Killer T cells (NKT) (Supplementary Fig. 2). Interestingly, the CD3+ CD8- CD103+ TIL did not express NKP46 or FoxP3 (Supplementary Figs. 3 and 4, respectively) suggesting a CD3+ CD4+ non-Treg phenotype.
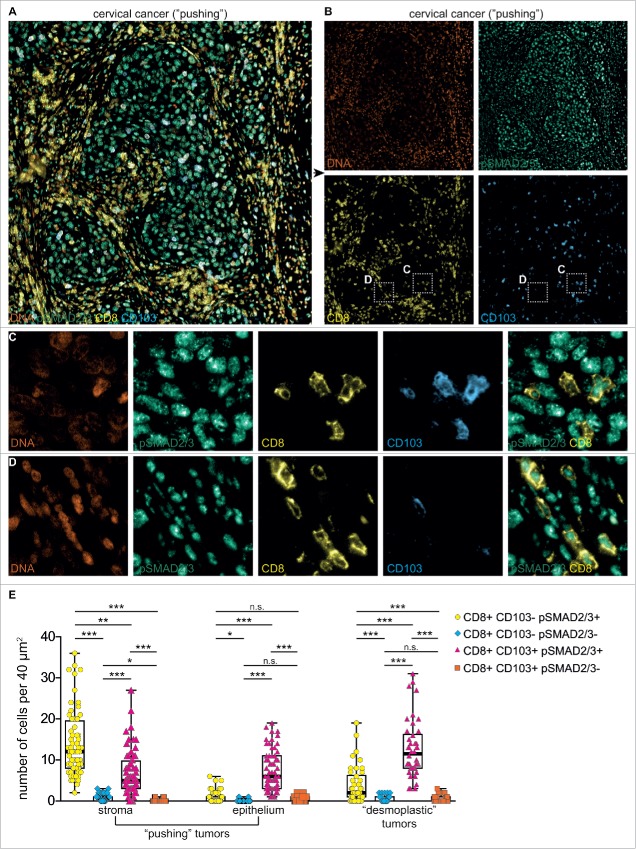
Figure 4.
TGF-β signaling is abundant in cervical cancer tissue. A) Representative image of tissue from a patient with cervical cancer of the “pushing” type stained with DAPI (DNA, orange), anti-CD8 (yellow), anti-CD103 (blue) and anti-pSMAD2/3 (green) antibodies. B) Representative single and multichannel images of the tumor area from A showing predominant localization of CD8+ cells in the pSMAD2/3+ stromal region and CD8+ CD103+ cells in the pSMAD2/3+ epithelial region. Insets represent areas magnified in panels C and D. C-D) Representative images of CD8+ and CD103+ cells in magnified epithelial (C) or stromal areas (D) of tumor tissue as indicated by insets in B. E) Quantification of CD8+, CD103+ and/or pSMAD2/3+ cells in the stroma and epithelial areas of the “pushing” tumors or total of the “desmoplastic” tumors. Each data point represents a cell count from a 40μm2 independent region of 18 independent tumors (3–6 in total per tumor section). Groups were compared by ANOVA using a Dunns post-test. *p < 0.05, **p < 0.01, ***p < 0.001.
Within the desmoplastic tumor type (n = 6), a distinct selection of stromal versus epithelial areas could not be made (Fig. 3A–B). Nevertheless, the desmoplastic tumors contained an even higher percentage of CD8+ CD103+TIL (Fig. 3D). By contrast, single CD8+ or CD103+ cells could barely be detected in these tumors. In healthy cervical tissue, no CD8+ CD103+ cells were detected (Fig. 3A), but epithelial CD8+ CD103- cells and a small number of stromal CD8- CD103+ cells were found. Untransformed stromal cervical tissue surrounding the pushing tumor types was frequently rich in CD8- CD103- cells that expressed NKp46 (data not shown). Taken together, these data demonstrate that CD103+ cells in cervical cancer tissue are predominantly CD8+ T cells, with a minor fraction of CD4+ non-Treg cells. By contrast, CD103+ T cells are largely absent from untransformed epithelium and stroma. In tumor-adjacent stroma, mainly CD103- NK cells are present.
CD103+ TIL in situ are characterized by ongoing TGFbR1-signaling
We and others have demonstrated that CD103 is upregulated on T cells following concomitant T cell and transforming growth factor (TGF)-β receptor (TGFβR) signaling.31-35 Indeed, CD103+, but not CD103-, TIL in high-grade serous ovarian cancer are characterized by nuclear phosphorylated mothers against decapentaplegic homolog 2 and 3 (pSMAD2/3) expression, a hallmark of TGF-β signaling. To confirm signs of active TGF-β signaling in CD103+ TIL from SCC, paraffin-embedded tissue was probed by fluorescent microscopy for simultaneous expression of CD8, CD103 and nuclear pSMAD2/3. SCC tumor islets, the surrounding stroma cells, and CD103- and CD103+ TIL were all characterized by a pronounced nuclear expression of pSMAD2/3 (Fig. 4) suggesting TGFβR1-signaling is highly active in the cervical cancer microenvironment, but not restricted to CD103+ TIL. In healthy cervical tissue, pSMAD2/3 signaling was also abundant in epithelial, stromal, CD8+ and CD103+ cells (Supplementary Fig. 5).
Anti-tumor therapeutic efficacy is mediated by recruitment of CD103+ TIL in vivo
Finally, to determine whether CD103 could also be used as a response biomarker for immunotherapy targeting E6 and E7, we used the E6/E7-transformed TC1 mouse model.36 TC-1 cells are derived from primary epithelial cells of C57BL/6 mice co-transformed with HPV-16 E6 and E7 and c-Ha-ras oncogenes. These cells form tumors composed largely of epithelial cells after subcutaneous injection and should therefore induce CD103 on infiltrating CD8+ T cells. Based on the differential prognostic effects of radiotherapy observed in both the TCGA and IHC series, we also assessed whether radiotherapy synergized with E6/E7-specific antitumor immune responses in vivo using our previously published experimental setup36 (Fig. 5A). In brief, female C57BL/6 mice were challenged with TC1 tumors and treated with a suboptimal immunization regimen of 5 × 106 i.u. semliki forest virus (SFV)eE6,7 immunization 14 days after tumor inoculation with or without radiation. At this dose, immunization alone is insufficient at inducing tumor eradication and synergizes with ionizing radiation. After 22 days mice were killed, tumors were measured and digested.
Figure 5.
Combination immunotherapy targeting HPV E6 and E7 induces accumulation of CD103+ cells in vivo. A) Schematic depiction of the TC1 mouse model. B) Representative flow cytometric plot of a TC1 tumor digest analyzed for expression of CD103 and CD8 within the DAPI-negative live cell population. C) Representative flow cytometric plots of TC1 tumor digests from untreated mice or mice treated with irradiation, a low dose of SFV E6/E7 vaccine, or both analyzed for expression of CD8 and CD103 within the DAPI-negative live cell population. D) Bar graphs representing the absolute number of CD103+ cells per gram of tumor of the experimental groups (n = 3–6). E) Scatter plots representing the number of CD103+ cells per gram of tumor across all groups (n = 3–6). F) Percentage of E7-specific CD8+ T cells across all treatment groups. *p < 0.05.
For flow cytometric analysis, TC1 tumor digests were gated on lymphocyte singlets and subsequently on DAPI- live cells (Fig. 5B). Within the TC1 tumor digests, untreated mice showed ∼10% CD8+ CD103+ cells (Fig. 5C–D). Therapeutic SFVeE6/E7 vaccination increased the intratumoral number of CD8+ CD103+ T cells to ∼25%, an effect that further synergized with concomitant irradiation to ∼60% (representative plots in Fig. 5C). Irradiation alone resulted in a ∼10% CD8+ CD103+ T cell infiltration (Fig 5C–D). Within all treatment groups, and independent of the number of infiltrating cells, CD103+ cells were almost exclusively CD8+ T cells (Fig. 5C). As expected, the percentage of infiltrating CD8+ CD103+ T cells across all treatment groups was negatively correlated with tumor weight (Fig. 5E; R2 = 0.53 p = 0.008). Finally, analysis of E7-reactive T cells using E7 H-2Kb dextramer staining revealed E7-specificity to be largely restricted to the CD103+ T cell population (Fig. 5F).
Discussion
In the present study we demonstrate that infiltrating CD103+ T cells are a prognostic factor for survival in cervical cancer patients. By gene expression analysis on tumor samples from cervical cancer patients available within the TCGA data set, we showed that expression of ITGAE, the gene encoding for CD103, correlates with significantly improved survival. This prognostic benefit of CD103-expressing T cells was confirmed in an independent cohort of 460 cervical cancer patients by immunohistochemical analysis of CD103+ TIL in FFPE-tumor cores. Furthermore, we show that CD103 is a marker for intraepithelial CD8+ T cells in cervical cancer. Finally, we demonstrate that CD103 holds considerable promise as both a predictive and response biomarker for radiotherapy and/or E6/E7-targeted immunotherapy.
Our results in the cervical cancer cohorts are in line with earlier findings on the localization and prognostic influence of CD103+ TIL in endometrial, ovarian, bladder and lung cancer. However, in contrast to other malignancies, infiltration of cervical cancers was related to the type of treatment patients received and the stage of disease. Patients that were treated with radio(chemo)therapy alone or in combination with surgery had fewer infiltrating CD103+ TIL compared with patients that qualified for surgical treatment alone. Moreover, within the radio(chemo)therapy group, patients that presented with a higher stage of disease were characterized by even lower numbers of CD103+ TIL when compared with patients with lower FIGO stages. This strongly suggests an interference of T cells and tumor cells where an equilibrium is reached in the early stages of disease, whereas larger tumors have escaped immune control by T cells and advanced stages of the disease are able to develop.37 As a result, patients with immunological ‘hot’ tumors generally present with an early stage of disease, whereas patients with immunological ‘cold’ tumors show a more aggressive disease with indications for primary (locally advanced disease) or adjuvant radio(chemo)therapy treatment (e.g., positive resection margins after surgery or positive lymph nodes).
In addition to the reduced number of infiltrating cells in clinically more aggressive cancers, analysis of the TCGA cervical cancer data set shows that ITGAE expression is not only strongly associated with the common T cell genes such as CD8A, but more importantly also with T cell activation and exhaustion markers such as CD137, CTLA4, PD1, and PDL1. This suggests that these patients may be candidates for additional adjuvant therapy with immune checkpoint inhibitors such as antibodies targeting CTLA-4 (ipilimumab) or PD-1 (nivolumab/pembroluzimab). In patients with melanoma and non-small cell lung cancer in particular, immune checkpoint inhibitors have met with considerable clinical success. In these malignancies, responses to immune checkpoint inhibitors have been strongly linked to the presence of neo-antigens in cancer cells (particularly those expressed across lesions) that provide a true tumor-specific target for T cells for which tolerance has likely not been established.38,39 In cervical cancer, the constitutive expression and the viral nature of E6/E7 oncoproteins in malignant cells is likely to provide a similar strong and non-tolerant target for T cell recognition that may be exploited with immune checkpoint inhibitors.
One caveat herein may be the poor infiltration of these tumors by immune cells. Indeed, as discussed above, aggressive tumors at higher stages of the disease show relatively poor infiltration by CD103+ TIL that may preclude effective responses to checkpoint inhibition. In one melanoma trial, a high number of preexisting T cells was a determinant for subsequent responses to therapy with anti-PD1 antibody pembroluzimab. In the absence of a strong T cell response, additional therapeutic strategies may therefore be required to pre-condition these patients for therapy with checkpoint inhibitors.40 One promising approach is the use of therapeutic vaccins targeting the E6/E7 oncoproteins. Indeed, several clinical trials have demonstrated promising results in cervical intraepithelial neoplasia (CIN) and cervical cancer patients treated with therapeutic E6/E7 targeted vaccines.11,16,18,19,41 In one study using a therapeutic DNA vaccine, 7 out of 9 CIN 3 patients showed complete regression and viral clearance within 36 weeks of follow up.16 In a randomized, double-blind, placebo-controlled trial in CIN2/3 patients, 49.5% of the DNA vaccine recipients showed regression of the disease vs. 30.6% in the control group.11 These promising results may eventually lead to a change in treatment strategy for CIN 2/3, in which therapeutic vaccination could represents a non-surgical option.
In this work, we similarly demonstrate that an E6/E7-targeted SFV vaccine can induce accumulation of CD103+ T cells in tumors in vivo, an effect that synergized with radiotherapy. SFV E6/E7 vaccination therefore not only promotes systemic immune responses, but T cells induced by this vaccination effectively penetrate the tumor lesion and engage the epithelial cells present, resulting in CD103 upregulation. Importantly, all infiltrating cells in this model were CD8+, in line with the phenotype observed in the human setting.
With regards to this phenotype and ontogeny of CD103+ TIL in human tumors the literature remains diverse. In the gut, CD103 has been described to be expressed on Intra-epithelial Lymphocytes (IEL), characterized by a CD8αα+ phenotype.42,43 In NSCLC the phenotype of CD103+ TIL has been described as tissue-resident memory T cells (characterized by a CD69+ CD62L− CD28− CD27+ CD45RA+ CD45RO+ CCR7- phenotype).24 In endometrial cancer CD103+ TIL were of heterogenous memory phenotypes,34 and in HGSC, CD103+TIL were classical CD3+ CD56- TCRab+ CD8ab+ CD4- T cells, also with heterogeneous differentiation status.35 While we demonstrate dominant CD8 co-expression in cervical cancer, the precise differentiation status has not been investigated. We hypothesize that, as the cervix functions as a barrier against pathogens, CD103 tissue-resident memory T cells may also be present. However, in the context of tumor-specific (E6/E7-directed) immune responses, the majority of CD103+ TIL are likely recruited as a result of an adaptive immune response. Within cervical cancer tumor slides, we also show that CD103+ CD8- TIL expressed CD3 but were negative for NkP46 and FoxP3, suggesting a CD4 but not a NKT cell nor a Treg origin.
Interestingly, when analyzing the fluorescent images of the tumor tissue we noticed different patterns of stromal infiltration into the epithelial areas, namely a pushing and desmoplastic type.30 The pushing tumor type was characterized by a distinct separation of epithelial and stromal areas. Whereas in the desmoplastic tumor type, a separation between stromal vs. epithelial areas could not be made. The desmoplastic tumor type has been described in literature as a more invasive tumor, but the exact consequences of this remains unclear. Interestingly, we observed that the desmoplastic tumors contained an even higher percentage of CD8+ CD103+TIL when compared with the pushing type. This might suggest that the desmoplastic tumors are more accessible to infiltration of CD8+ T cells which then engage the epithelial tumor cells and upregulate CD103 after T cell receptor (TCR) activation.
In line with this hypothesis, our data strongly suggests that upregulation of CD103 in cervical cancer is mainly the result of TCR signaling upon cancer cell contact. It has been well established that ITGAE (CD103) expression is induced by dual TCR and TGFβR1 activation.32,33,44 In HGSC, we have further shown that CD103+, but not CD103-, TIL are characterized by nuclear pSMAD2/3 expression, a hallmark of TGF-β signaling.35 In contrast to HGSC tissue, the total tumor microenvironment in cervical cancer tissue was rich in pSMAD2/3 expression and no differences in expression between epithelial and stromal areas were observed. This TGF-β rich microenvironment might be explained by the E6/E7-dependent ontogeny of cervical cancer. HPV-16 E6 and E7 oncoproteins have been shown to directly regulate the TGF-β1 promoter in cervical tumor cells through a specific DNA sequence motif in the TGF-β1 core promoter.45 It is thought the upregulation of TGF-β facilitates the development of cervical neoplasia after E6/E7 integration by promoting genomic instability in the infected epithelial cells.46 As a consequence, the immune environment is rich in TGF-β expression likely rendering T cell contact with the cancer cell as the key determinant of CD103 induction. CD103 may therefore represent an excellent biomarker for tumor-reactive T cells in cervical cancers that could be quantified in a rapid manner without having to account for epithelial vs. stromal compartments. It is tempting to speculate that the same may therefore hold true for other types of HPV-mediated cancers, such as head and neck squamous cell carcinoma (HNSCC). Indeed, TGF-β is overexpressed in ∼80% of HNSCC cases47 and likely produced by both cancer cells, stroma, and/or infiltration immune cells (reviewed in Yang et al.48) It will be interesting to assess whether differences exist between CD103+ cells infiltration in HPV-positive vs. HPV-negative HNSCC tumors, as has been reported for CD8+ cells.49
This use of CD103 as an easy-to-use biomarker for assessing immune responses against cervical cancer is supported by our in vivo data that demonstrate increased infiltration of TC1 tumors by CD103+ CD8+ cells upon treatment with a synergizing combination of HPV E6/E7 vaccination and radiotherapy. Indeed, an inverse correlation exists between the number of CD103+ cells in the tumor digest and the size of the tumor. With the clinical advent of therapeutic E6/E7-based vaccination strategies, CD103 may be incorporated both for patient selection and for monitoring early therapy responses in the tumor by biopsy. Of note, clues for synergistic effects on tumor control for radiation and E6/E7-targeted therapy in the human setting were also found in this study. In particular, the prognostic benefit of CD103+ cell infiltration in both the TCGA and IHC data sets were found within the group of patients that received adjuvant radio(chemo)therapy within 6 months of surgical intervention, but not in patients that received surgery alone. Assuming infiltrating T cells in most patients react against E6/E7 proteins to a certain extent, it is tempting to speculate that the pre-existing immune responses are augmented by the radiotherapy, similar to what was observed in the animal model. Future studies on clinical vaccination in combination with radiotherapy therefore appear warranted in this patient population.
Taken together, we demonstrate here for the first time that CD103 is a suitable marker for rapid unbiased assessment of prognostically beneficial CD8+ T cell infiltration of cervical cancers and might be used as a response biomarker for E6/E7-targeted immunotherapy alone or in combination with radiotherapy.
Methods
TCGA data and analysis
TCGA RSEM normalized50 RNAseq and clinical data were downloaded from FireBrowse (http://firebrowse.org) on August 22nd, 2016. After removal of normal tissue controls and technical duplicates, 304 cervical cancer cases were informative for this study. RNAseq data were log2 transformed before further analysis. The expression of CD103 (ITGAE) relative to that of other immune markers51 was visualized by means of a heatmap using GENE-E (Broad Institute). For analysis of CD103 expression with clinicopathological variables and patient survival, cases were dichotomized according to median CD103 expression. Analyses of clinical outcome excluded 13 patients for whom survival data were not available. For the exploratory analyses of the relationship between CD103 expression, radiotherapy treatment and clinical outcome, we excluded cases in which radiotherapy was given ≥ 6 months after diagnosis, to avoid misclassification of patients irradiated after disease recurrence.
Patient selection for the immunohistochemical series
Clinicopathological characteristics of cervical cancer patients treated within the University Medical Center Groningen were prospectively stored in a database since January 1980. As described by Maduro et al,52 a separate anonymized database was retrieved containing all patients with stage IA2-IVA cervical cancer. Patients were treated between January 1980 and December 2004 with either surgery or radiotherapy depending on stage of disease and/or results of surgical outcome. We categorized patients into two groups based on their treatment modality, namely surgery or radio(chemo)therapy. The treatment modality was considered surgery in those patients in whom a radical hysterectomy combined with pelvic lymph node dissection was performed (first choice of treatment in early stage disease). The treatment modality was considered radio(chemo)therapy (first choice of treatment in locally advanced disease) if patients received radiotherapy or radio-chemotherapy, even if a surgical procedure was performed, as is the case in e.g., patients where positive nodes are detected after primary hysterectomy/lymph node dissection. Patients were selected if sufficient formalin-fixed, paraffin-embedded (FFPE) tissue was available for tissue microarray (TMA) construction. For the construction of the TMA, only pretreatment biopsies were used. Follow up data was collected up to April 2012. According to Dutch law, no approval from our institutional review board was needed.
Tissue microarray (TMA) construction
From the patients meeting the inclusion criteria, a TMA was constructed as described previously.53 In brief, cancer nests were determined by a gynecologic pathologist based on H&E staining. Triplicate 1mm2 cores were randomly selected from cancer nests and placed in a recipient paraffin block by a tissue microarrayer (Beecher instruments). After insertion of cores, recipient blocks were placed at 37°C for 15 minutes to maximize tissue adhesion to the wax. The paraffin block was sliced into 4µm sections and placed on APES-coated slides (Starfrost).
Immunohistochemical analysis of CD103± TIL infiltration
TMA sections were dewaxed in xylene and rehydrated using degraded concentrations of ethanol to distilled water. Antigen retrieval was initiated using a preheated 10 mM citrate buffer (pH6), endogenous peroxidase activity was blocked by submerging of sections in a 0.45% H2O2 solution. Sections were incubated in a blocking buffer (1% human AB serum in 1% BSA/PBS solution), followed by an avidin/biotin block. Afterwards, sections were incubated with rabbit-anti human CD103 mAb (anti-αEβ7-integrin, Abcam, ab129202, 1:200 in blocking buffer) and incubated at 4°C overnight. Slides were incubated with a peroxidase-labeled polymer (Envision+ anti-rabbit Dako) and a Biotin Tyramide working solution according to the manufacturer's instructions (TSA Kit Perkin Elmer, NEL700A001KT). Subsequently, slides were incubated with streptavidin-HRP (dilution: 1:100) (TSA kit, Perkin Elmer) and specific signal visualized by 3,3′diaminobenzidin (DAB). Slides were counterstained with hematoxylin.
The total number of positively stained CD103+ cells was counted per core and the percentage of tumor/stromal surface was estimated. Patients were included if at least 2 cores contained >20% tumor epithelium. All slides were counted manually by 2 individuals that were blinded for clinicopathological data. The 2 individual scores were compared and differences in counts of over 10% were reanalyzed until consensus was reached. Cell count was re-calculated per 1 mm2 (i.e. the surface of one core).
Immunofluorescent analysis of CD103+ TIL localization and phenotype
Preparation, antigen retrieval and incubation with primary CD103 antibody of full tumor slides was performed as described in immunohistochemistry (IHC). Sections were subsequently incubated with Envision-HRP anti-rabbit followed by fluorophore tyramide stock solution:amplification diluents (TSA KIT Perkin Elmer,1:50) according to the manufacturer's instructions. Slides were incubated overnight at 4°C with either biotinylated rabbit anti-fibronectin (Abcam, ab6584 1:50 in blocking buffer) or rabbit anti-phospho-SMAD2/3 Mab (cell signaling, Ser 465/467 #3101, 1:50 in blocking buffer), and either mouse anti-human CD8 (DAKO, clone C8/144B, M710301–2, 1:25 in blocking buffer), anti-NKp46 (R&D Systems, ab1850, 1:25 in blocking buffer), anti-CD3 (Abcam, ab11089, 1:25 in blocking buffer) or anti-FoxP3 (Abcam, ab20034, 1:50 in blocking buffer) antibodies. Sections were subsequently incubated with goat-anti-mouse Alexa Fluor 555 (Life Technologies, Eugene,1:150) and streptavidin dylight 488 (Life Technologies, 1:150) Nuclei were visualized with DAPI. Sections were embedded in prolong Diamond anti-fade mounting medium (Life Technologies, Eugene) and scanned using a TissueFaxs imaging system (TissueGnostics). Processed channels were merged using Adobe Photoshop. On each slide 3 to 6 representative epithelial and 3 to 6 stromal areas of 40 μm2 were selected based on DAPI staining. Within each area, single-positive (CD103-CD8+ or CD103+CD8-) cells as well as double-positive (CD103+CD8+) cells were counted manually.
Mice
Specified pathogen-free female C57BL/6 mice were used at 8 to 12 weeks of age at the onset of the experiment. They were purchased from Harlan CPB (Zeist, The Netherlands) and kept according to institute guidelines. All animal experiments were approved by the local Animal Experimentation Ethical Committee.
Tumor inoculation, local tumor irradiation and rSFV immunization
TC-1 cells were a kind gift from Dr. Cornelis J. Melief and Dr. Rienk Offringa (Leiden University Medical Center, The Netherlands). The TC-1 cell line was generated from C57Bl/6 primary lung epithelial cells with a retroviral vector expressing HPV16 E6E7. All cells were cultured as described before.54 Mice were inoculated subcutaneously in the neck with 2 × 104 TC-1 cells suspended in 0.2 mL Hank's Balanced Salt Solution (Invitrogen,). Fourteen days after injection of TC-1, mice were locally irradiated with 7 Gy and/or semliki forest virus (SFV)eE6,7 immunization. Radiation was performed using X-RAD 320 Biological Irradiator (Precision X-Ray) with a delivery rate of 1.64 Gy/min. Immunization was performed intramuscularly with a dose of 5 × 106 i.u. of SFVeE6,7 and boosted twice with a one-week interval (day 14 and 21) as a suboptimal immunization regimen. Control mice were injected intramuscularly with PBS. Tumors were isolated 22 days after TC-1 inoculation.
Tumor digestion and flow cytometry analysis
Tumors isolated from mice were processed as previous described(51). In brief, pre-warmed Collagenase A (Roche) solution was used for digestion and tumors were homogenized using the gentle MACStm Dissociator (Miltenyi Biotec). Tumors cells were further stained with PeCy7-anti-CD8 (eBioscience, clone 53–6.7, 25–5273–41) and FITC-anti-CD103 (BD Biosciences, clone 2E7, 333155). For the dextramer staining, cell suspensions were first washed twice in FACS buffer (PBS containing 0.5% bovine serum albumin) and stained with PE-H-2Db E749–57 dextramers (Immudex, Copenhagen, Denmark) for 10 min at room temperature. Subsequently, the cells were stained with PE-Cy7-anti-CD8a Ab and FITC-anti-CD103 Ab. To exclude dead cells, cells were stained with Zombie Violet™ (Biolegend, 423113).
Statistics
Differences in cell count were determined by a Mann-Whitney U, Kruskall-Wallis, ANOVA or t-test. Disease-specific survival (DSS) and disease-free survival (DFS) were analyzed using a Kaplan-Meier function; differences in survival were assessed by log Rank test. DSS was defined as date of diagnosis to date of death due to disease. DFS was defined as date of diagnosis to date of recurrence or date of death of disease, in case no recurrence was reported previously. Differences in DSS and DFS according to clinicopathologic characteristics and to infiltration of CD103+ TIL were analyzed using the Cox regression analyses. Variables with a p-value <0.05 in the univariate analyses were included in the multivariate analyses. Significance was defined as a p-value of <0.05, all tests were performed 2-sided. Statistics were performed using SPSS software version 22.0 (SPSS inc.), Stata (StataCorp,) or GraphPad Prism (GraphPad Software inc.).
Supplementary Material
Disclosure of potential conflicts of interest
HW Nijman and T Daemen have a financial ownership interest in ViciniVax and may financially benefit if the company is successful in marketing its product related to this research. The terms of this arrangement have been reviewed and approved by the University of Groningen.
Acknowledgments
This work was supported by Dutch Cancer Society/Alpe d'Huzes grant UMG 2014−6719 to MB and a Jan Kornelis de Cock Stichting grant to FLK. DNC is supported by a Clinician Scientist Award from the Academy of Medical Sciences / Health Foundation, and has received funding from the Oxford Cancer Center, University of Oxford. Part of the work has been performed at the UMCG Imaging and Microscopy Center (UMIC), which is sponsored by NWO-grants 40–00506–98–9021 and 175–010–2009–023. The authors would like to thank Klaas Sjollema for his technical assistance.
Funding
This work was supported by Dutch Cancer Society/Alpe d'Huzes under grant UMCG 2014−6719 to MB; Jan Kornelis de Cock Stichting under grants to FLK and FAE. DNC is supported by a Clinician Scientist Award from the Academy of Medical Sciences / Health Foundation, and has received funding from the Oxford Cancer Center, University of Oxford. Part of the work has been performed at the UMCG Imaging and Microscopy Center (UMIC), which is sponsored by NWO-grants 40–00506–98–9021 and 175–010–2009–023.
References
- 1.Kjaer SK, van den Brule AJ, Paull G, Svare EI, Sherman ME, Thomsen BL, Suntum M, Bock JE, Poll PA, Meijer CJ. Type specific persistence of high risk human papillomavirus (HPV) as indicator of high grade cervical squamous intraepithelial lesions in young women: population based prospective follow up study. BMJ [Internet] 2002. [cited 2015October8]; 325:572. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=124551&tool=pmcentrez&rendertype=abstract; PMID:12228133; https://doi.org/ 10.1136/bmj.325.7364.572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Remmink AJ, Walboomers JM, Helmerhorst TJ, Voorhorst FJ, Rozendaal L, Risse EK, Meijer CJ, Kenemans P. The presence of persistent high-risk HPV genotypes in dysplastic cervical lesions is associated with progressive disease: natural history up to 36 months. Int J Cancer [Internet] 1995. [cited 2015August26]; 61:306-11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/7729939; PMID:7729939; https://doi.org/ 10.1002/ijc.2910610305 [DOI] [PubMed] [Google Scholar]
- 3.Kalinski P, Mailliard RB, Giermasz A, Zeh HJ, Basse P, Bartlett DL, Kirkwood JM, Lotze MT, Herberman RB. Natural killer-dendritic cell cross-talk in cancer immunotherapy. Expert Opin Biol Ther [Internet] 2005. [cited 2016January11]; 5:1303-15. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16197336; PMID:16197336; https://doi.org/ 10.1517/14712598.5.10.1303 [DOI] [PubMed] [Google Scholar]
- 4.Blankenstein T, Qin Z. The role of IFN-gamma in tumor transplantation immunity and inhibition of chemical carcinogenesis. Curr Opin Immunol [Internet] 2003. [cited 2016January11]; 15:148-54. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12633663; PMID:12633663; https://doi.org/ 10.1016/S0952-7915(03)00007-4 [DOI] [PubMed] [Google Scholar]
- 5.Mellman I, Coukos G, Dranoff G. Cancer immunotherapy comes of age. Nature [Internet] 2011. [cited 2014July9]; 480:480-9. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3967235&tool=pmcentrez&rendertype=abstract; PMID:22193102; https://doi.org/ 10.1038/nature10673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gorter A, Prins F, van Diepen M, Punt S, van der Burg SH. The tumor area occupied by Tbet+ cells in deeply invading cervical cancer predicts clinical outcome. J Transl Med [Internet] 2015. [cited 2016September14]; 13:295. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26357849; PMID:26357849; https://doi.org/ 10.1186/s12967-015-0664-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Vos van Steenwijk PJ, Ramwadhdoebe TH, Goedemans R, Doorduijn EM, van Ham JJ, Gorter A, van Hall T, Kuijjer ML, van Poelgeest MI, van der Burg SH, et al.. Tumor-infiltrating CD14-positive myeloid cells and CD8-positive T-cells prolong survival in patients with cervical carcinoma. Int J cancer [Internet] 2013. [cited 2016September14]; 133:2884-94. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23740735; PMID:23740735 [DOI] [PubMed] [Google Scholar]
- 8.Sasagawa T, Takagi H, Makinoda S. Immune responses against human papillomavirus (HPV) infection and evasion of host defense in cervical cancer. J Infect Chemother [Internet] 2012. [cited 2016January11]; 18:807-15. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23117294; PMID:23117294; https://doi.org/ 10.1007/s10156-012-0485-5 [DOI] [PubMed] [Google Scholar]
- 9.Steele JC, Mann CH, Rookes S, Rollason T, Murphy D, Freeth MG, Gallimore PH, Roberts S. T-cell responses to human papillomavirus type 16 among women with different grades of cervical neoplasia. Br J Cancer [Internet] 2005. [cited 2016January11]; 93:248-59. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2361543&tool=pmcentrez&rendertype=abstract; PMID:15986031; https://doi.org/ 10.1038/sj.bjc.6602679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nasseri M, Gage JR, Lorincz A, Wettstein FO. Human papillomavirus type 16 immortalized cervical keratinocytes contain transcripts encoding E6, E7, and E2 initiated at the P97 promoter and express high levels of E7. Virology [Internet] 1991. [cited 2016January11]; 184:131-40. Available from: http://www.ncbi.nlm.nih.gov/pubmed/1651587; PMID:1651587; https://doi.org/ 10.1016/0042-6822(91)90829-Z [DOI] [PubMed] [Google Scholar]
- 11.Trimble CL, Morrow MP, Kraynyak KA, Shen X, Dallas M, Yan J, Edwards L, Parker RL, Denny L, Giffear M, et al.. Safety, efficacy, and immunogenicity of VGX-3100, a therapeutic synthetic DNA vaccine targeting human papillomavirus 16 and 18 E6 and E7 proteins for cervical intraepithelial neoplasia 2/3: a randomised, double-blind, placebo-controlled phase 2b trial. Lancet (London, England) [Internet] 2015. [cited 2015September22]; 386(10008):2078-88; Available from: http://www.ncbi.nlm.nih.gov/pubmed/26386540; https://doi.org/ 10.1016/S0140-6736(15)00239-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stevanović S, Draper LM, Langhan MM, Campbell TE, Kwong ML, Wunderlich JR, Dudley ME, Yang JC, Sherry RM, Kammula US, et al.. Complete regression of metastatic cervical cancer after treatment with human papillomavirus-targeted tumor-infiltrating T cells. J Clin Oncol [Internet] 2015. [cited 2015September9]; 33:1543-50. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25823737; PMID:25823737; https://doi.org/ 10.1200/JCO.2014.58.9093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maldonado L, Teague JE, Morrow MP, Jotova I, Wu TC, Wang C, Desmarais C, Boyer JD, Tycko B, Robins HS, et al.. Intramuscular therapeutic vaccination targeting HPV16 induces T cell responses that localize in mucosal lesions. Sci Transl Med [Internet] 2014. [cited 2015July4]; 6:221ra13. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4086631&tool=pmcentrez&rendertype=abstract; PMID:24477000; https://doi.org/ 10.1126/scitranslmed.3007323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kawana K, Adachi K, Kojima S, Taguchi A, Tomio K, Yamashita A, Nishida H, Nagasaka K, Arimoto T, Yokoyama T, et al.. Oral vaccination against HPV E7 for treatment of cervical intraepithelial neoplasia grade 3 (CIN3) elicits E7-specific mucosal immunity in the cervix of CIN3 patients. Vaccine [Internet] 2014. [cited 2015September16]; 32:6233-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25258102; PMID:25258102; https://doi.org/ 10.1016/j.vaccine.2014.09.020 [DOI] [PubMed] [Google Scholar]
- 15.Rosales R, López-Contreras M, Rosales C, Magallanes-Molina J-R, Gonzalez-Vergara R, Arroyo-Cazarez JM, Ricardez-Arenas A, Del Follo-Valencia A, Padilla-Arriaga S, Guerrero MV, et al.. Regression of human papillomavirus intraepithelial lesions is induced by MVA E2 therapeutic vaccine. Hum Gene Ther [Internet] 2014. [cited 2015September16]; 25:1035-49. Available from: http://online.liebertpub.com/doi/abs/10.1089/hum.2014.024; PMID:25275724; https://doi.org/ 10.1089/hum.2014.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim TJ, Jin HT, Hur SY, Yang HG, Seo YB, Hong SR, Lee CW, Kim S, Woo JW, Park KS, et al.. Clearance of persistent HPV infection and cervical lesion by therapeutic DNA vaccine in CIN3 patients. Nat Commun [Internet] 2014. [cited 2015July21]; 5:5317. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=4220493&tool=pmcentrez&rendertype=abstract; PMID:25354725; https://doi.org/ 10.1038/ncomms6317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trimble CL, Peng S, Kos F, Gravitt P, Viscidi R, Sugar E, Pardoll D, Wu TC. A phase I trial of a human papillomavirus DNA vaccine for HPV16+ cervical intraepithelial neoplasia 2/3. Clin Cancer Res [Internet] 2009. [cited 2015September15]; 15:361-7. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2865676&tool=pmcentrez&rendertype=abstract; PMID:19118066; https://doi.org/ 10.1158/1078-0432.CCR-08-1725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Vos van Steenwijk PJ, Ramwadhdoebe TH, Löwik MJ, van der Minne CE, Berends-van der Meer DM, Fathers LM, Valentijn AR, Oostendorp J, Fleuren GJ, Hellebrekers BW, et al.. A placebo-controlled randomized HPV16 synthetic long-peptide vaccination study in women with high-grade cervical squamous intraepithelial lesions. Cancer Immunol Immunother [Internet] 2012. [cited 2015September15]; 61:1485-92. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3427705&tool=pmcentrez&rendertype=abstract; PMID:22684521; https://doi.org/ 10.1007/s00262-012-1292-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Poelgeest MI, Welters MJ, van Esch EM, Stynenbosch LF, Kerpershoek G, van Persijn van Meerten EL, van den Hende M, Löwik MJ, Berends-van der Meer DM, Fathers LM, et al.. HPV16 synthetic long peptide (HPV16-SLP) vaccination therapy of patients with advanced or recurrent HPV16-induced gynecological carcinoma, a phase II trial. J Transl Med [Internet] 2013. [cited 2015September15]; 11:88. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3623745&tool=pmcentrez&rendertype=abstract; PMID:23557172; https://doi.org/ 10.1186/1479-5876-11-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kenter GG, Welters MJ, Valentijn AR, Lowik MJ, Berends-van der Meer DM, Vloon AP, Drijfhout JW, Wafelman AR, Oostendorp J, Fleuren GJ, et al.. Phase I immunotherapeutic trial with long peptides spanning the E6 and E7 sequences of high-risk human papillomavirus 16 in end-stage cervical cancer patients shows low toxicity and robust immunogenicity. Clin Cancer Res [Internet] 2008. [cited 2015July4]; 14:169-77. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18172268; PMID:18172268; https://doi.org/ 10.1158/1078-0432.CCR-07-1881 [DOI] [PubMed] [Google Scholar]
- 21.Borysiewicz LK, Fiander A, Nimako M, Man S, Wilkinson GW, Westmoreland D, Evans AS, Adams M, Stacey SN, Boursnell ME, et al.. A recombinant vaccinia virus encoding human papillomavirus types 16 and 18, E6 and E7 proteins as immunotherapy for cervical cancer. Lancet (London, England) [Internet] 1996. [cited 2015October8]; 347:1523-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/8684105; PMID:8684105; https://doi.org/ 10.1016/S0140-6736(96)90674-1 [DOI] [PubMed] [Google Scholar]
- 22.Piersma SJ, Jordanova ES, van Poelgeest MI, Kwappenberg KM, van der Hulst JM, Drijfhout JW, Melief CJ, Kenter GG, Fleuren GJ, Offringa R, et al.. High number of intraepithelial CD8+ tumor-infiltrating lymphocytes is associated with the absence of lymph node metastases in patients with large early-stage cervical cancer. Cancer Res [Internet] 2007. [cited 2016September14]; 67:354-61. Available from: http://www.ncbi.nlm.nih.gov/pubmed/17210718; PMID:17210718; https://doi.org/ 10.1158/0008-5472.CAN-06-3388 [DOI] [PubMed] [Google Scholar]
- 23.Wang B, Wu S, Zeng H, Liu Z, Dong W, He W, Chen X, Dong X, Zheng L, Lin T, et al.. CD103+ Tumor Infiltrating Lymphocytes Predict a Favorable Prognosis in Urothelial Cell Carcinoma of the Bladder. J Urol [Internet] 2015. [cited 2016March22]; 194:556-62. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25752441; PMID:25752441; https://doi.org/ 10.1016/j.juro.2015.02.2941 [DOI] [PubMed] [Google Scholar]
- 24.Djenidi F, Adam J, Goubar A, Durgeau A, Meurice G, de Montpréville V, Validire P, Besse B, Mami-Chouaib F. CD8+CD103+ tumor-infiltrating lymphocytes are tumor-specific tissue-resident memory T cells and a prognostic factor for survival in lung cancer patients. J Immunol [Internet] 2015. [cited 2016March22]; 194:3475-86. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25725111; PMID:25725111; https://doi.org/ 10.4049/jimmunol.1402711 [DOI] [PubMed] [Google Scholar]
- 25.Workel HH, Komdeur FL, Wouters MC, Plat A, Klip HG, Eggink FA, Wisman GB, Arts HJ, Oonk MH, Mourits MJ, et al.. CD103 defines intraepithelial CD8+ PD1+ tumour-infiltrating lymphocytes of prognostic significance in endometrial adenocarcinoma. Eur J Cancer 2016; 60:1-11; PMID:27038842; https://doi.org/ 10.1016/j.ejca.2016.02.026 [DOI] [PubMed] [Google Scholar]
- 26.Webb JR, Milne K, Nelson BH. PD-1 and CD103 Are Widely Coexpressed on Prognostically Favorable Intraepithelial CD8 T Cells in Human Ovarian Cancer. Cancer Immunol Res [Internet] 2015; 3:926-35. Available from: http://cancerimmunolres.aacrjournals.org/cgi/doi/10.1158/2326-6066.CIR-14-0239; PMID:25957117; https://doi.org/ 10.1158/2326-6066.CIR-14-0239 [DOI] [PubMed] [Google Scholar]
- 27.Webb JR, Milne K, Watson P, Deleeuw RJ, Nelson BH. Tumor-infiltrating lymphocytes expressing the tissue resident memory marker CD103 are associated with increased survival in high-grade serous ovarian cancer. Clin Cancer Res [Internet] 2014. [cited 2016March22]; 20:434-44. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24190978; PMID:24190978; https://doi.org/ 10.1158/1078-0432.CCR-13-1877 [DOI] [PubMed] [Google Scholar]
- 28.Chao HT, Wang PH, Tseng JY, Lai CR, Chiang SC, Yuan CC. Lymphocyte-infiltrated FIGO Stage IIB squamous cell carcinoma of the cervix is a prominent factor for disease-free survival. Eur J Gynaecol Oncol [Internet] 1999. [cited 2016September14]; 20:136-40. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10376433; PMID:10376433 [PubMed] [Google Scholar]
- 29.Bethwaite PB, Holloway LJ, Thornton A, Delahunt B. Infiltration by immunocompetent cells in early stage invasive carcinoma of the uterine cervix: a prognostic study. Pathology [Internet] 1996. [cited 2016September14]; 28:321-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/9007950; PMID:9007950; https://doi.org/ 10.1080/00313029600169274 [DOI] [PubMed] [Google Scholar]
- 30.Ronnett BM. Endocervical adenocarcinoma: selected diagnostic challenges. Mod Pathol [Internet] 2016; 29 Suppl 1:S12-28. Available from: https://doi.org/10.1038/modpathol.2015.131; PMID:26715171; https://doi.org/ 10.1038/modpathol.2015.131 [DOI] [PubMed] [Google Scholar]
- 31.Massagué J, Blain SW, Lo RS. TGFbeta signaling in growth control, cancer, and heritable disorders. Cell [Internet] 2000. [cited 2016March22]; 103:295-309. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11057902; PMID:11057902; https://doi.org/ 10.1016/S0092-8674(00)00121-5 [DOI] [PubMed] [Google Scholar]
- 32.Mokrani M, Klibi J, Bluteau D, Bismuth G, Mami-Chouaib F. Smad and NFAT pathways cooperate to induce CD103 expression in human CD8 T lymphocytes. J Immunol [Internet] 2014. [cited 2016March22]; 192:2471-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24477908; PMID:24477908; https://doi.org/ 10.4049/jimmunol.1302192 [DOI] [PubMed] [Google Scholar]
- 33.Boutet M, Gauthier L, Leclerc M, Gros G, De Montpreville V, Théret N, Donnadieu E, Mami-Chouaib F. TGF-β signaling intersects with CD103 integrin signaling to promote T lymphocyte accumulation and antitumor activity in the lung tumor microenvironment. Cancer Res [Internet] 2016. [cited 2016March22]; 76(7):1757-69; Available from: http://www.ncbi.nlm.nih.gov/pubmed/26921343; PMID:26921343; https://doi.org/ 10.1158/0008-5472.CAN-15-1545 [DOI] [PubMed] [Google Scholar]
- 34.Workel HH, Komdeur FL, Wouters MC, Plat A, Klip HG, Eggink FA, Wisman GB, Arts HJ, Oonk MH, Mourits MJ, et al.. CD103 defines intraepithelial CD8+ PD1+ tumour-infiltrating lymphocytes of prognostic significance in endometrial adenocarcinoma. Eur J Cancer [Internet] 2016. [cited 2016April4]; 60:1-11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27038842; PMID:27038842; https://doi.org/ 10.1016/j.ejca.2016.02.026 [DOI] [PubMed] [Google Scholar]
- 35.Komdeur FL, Wouters MCA, Workel HH, Tijans AM, Terwindt ALJ, Brunekreeft KL, Plat A, Klip HG, Eggink FA, Leffers N, et al.. CD103+ intraepithelial T cells in high-grade serous ovarian cancer are phenotypically diverse TCRαβ+ CD8αβ+ T cells that can be targeted for cancer immunotherapy. Oncotarget [Internet] 2016. [cited 2016September23]; 7(46):75130-44; Available from: http://www.ncbi.nlm.nih.gov/pubmed/27650547; PMID:27650547; https://doi.org/ 10.18632/oncotarget.12077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Draghiciu O, Boerma A, Hoogeboom BN, Nijman HW, Daemen T. A rationally designed combined treatment with an alphavirus-based cancer vaccine, sunitinib and low-dose tumor irradiation completely blocks tumor development. Oncoimmunology [Internet] 2015. [cited 2017March30]; 4:e1029699. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26451295; PMID:26451295; https://doi.org/ 10.1080/2162402X.2015.1029699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dunn GP, Old LJ, Schreiber RD. The immunobiology of cancer immunosurveillance and immunoediting. Immunity [Internet] 2004. [cited 2016September14]; 21:137-48. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15308095; PMID:15308095; https://doi.org/ 10.1016/j.immuni.2004.07.017 [DOI] [PubMed] [Google Scholar]
- 38.Van Allen EM, Miao D, Schilling B, Shukla SA, Blank C, Zimmer L, Sucker A, Hillen U, Geukes Foppen MH, Goldinger SM, et al.. Genomic correlates of response to CTLA-4 blockade in metastatic melanoma. Science [Internet] 2015. [cited 2016September15]; 350:207-11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26359337; PMID:26359337; https://doi.org/ 10.1126/science.aad0095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McGranahan N, Furness AJS, Rosenthal R, Ramskov S, Lyngaa R, Saini SK, Jamal-Hanjani M, Wilson GA, Birkbak NJ, Hiley CT, et al.. Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science [Internet] 2016. [cited 2016September15]; 351:1463-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26940869; PMID:26940869; https://doi.org/ 10.1126/science.aaf1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tumeh PC, Harview CL, Yearley JH, Shintaku IP, Taylor EJM, Robert L, Chmielowski B, Spasic M, Henry G, Ciobanu V, et al.. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature [Internet] 2014. [cited 2016September16]; 515:568-71. Available from: http://www.nature.com/doifinder/10.1038/nature13954; PMID:25428505; https://doi.org/ 10.1038/nature13954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.de Vos van Steenwijk PJ, van Poelgeest MI, Ramwadhdoebe TH, Löwik MJ, Berends-van der Meer DM, van der Minne CE, Loof NM, Stynenbosch LF, Fathers LM, Valentijn AR, et al.. The long-term immune response after HPV16 peptide vaccination in women with low-grade pre-malignant disorders of the uterine cervix: a placebo-controlled phase II study. Cancer Immunol Immunother [Internet] 2014. [cited 2015July21]; 63:147-60. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24233343; PMID:24233343; https://doi.org/ 10.1007/s00262-013-1499-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Woo JC, Roccabianca P, van Stijn A, Moore PF. Characterization of a feline homologue of the alphaE integrin subunit (CD103) reveals high specificity for intra-epithelial lymphocytes. Vet Immunol Immunopathol [Internet] 2002. [cited 2016September14]; 85:9-22. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11867163; PMID:11867163; https://doi.org/ 10.1016/S0165-2427(01)00394-4 [DOI] [PubMed] [Google Scholar]
- 43.Konkel JE, Maruyama T, Carpenter AC, Xiong Y, Zamarron BF, Hall BE, Kulkarni AB, Zhang P, Bosselut R, Chen W. Control of the development of CD8αα+ intestinal intraepithelial lymphocytes by TGF-β. Nat Immunol [Internet] 2011. [cited 2016March22]; 12:312-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21297643; PMID:21297643; https://doi.org/ 10.1038/ni.1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mackay LK, Rahimpour A, Ma JZ, Collins N, Stock AT, Hafon M-L, Vega-Ramos J, Lauzurica P, Mueller SN, Stefanovic T, et al.. The developmental pathway for CD103(+)CD8+ tissue-resident memory T cells of skin. Nat Immunol [Internet] 2013. [cited 2016March22]; 14:1294-301. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24162776; PMID:24162776; https://doi.org/ 10.1038/ni.2744 [DOI] [PubMed] [Google Scholar]
- 45.Peralta-Zaragoza O, Bermúdez-Morales V, Gutiérrez-Xicotencatl L, Alcocer-González J, Recillas-Targa F, Madrid-Marina V. E6 and E7 oncoproteins from human papillomavirus type 16 induce activation of human transforming growth factor beta1 promoter throughout Sp1 recognition sequence. Viral Immunol [Internet] 2006. [cited 2016September15]; 19:468-80. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16987065; PMID:16987065; https://doi.org/ 10.1089/vim.2006.19.468 [DOI] [PubMed] [Google Scholar]
- 46.Deng W, Tsao SW, Kwok YK, Wong E, Huang XR, Liu S, Tsang CM, Ngan HYS, Cheung ANY, Lan HY, et al.. Transforming growth factor beta1 promotes chromosomal instability in human papillomavirus 16 E6E7-infected cervical epithelial cells. Cancer Res [Internet] 2008. [cited 2016September15]; 68:7200-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18757436; PMID:18757436; https://doi.org/ 10.1158/0008-5472.CAN-07-6569 [DOI] [PubMed] [Google Scholar]
- 47.Lu S-L, Reh D, Li AG, Woods J, Corless CL, Kulesz-Martin M, Wang XJ. Overexpression of transforming growth factor 1 in Head and Neck Epithelia Results in Inflammation, Angiogenesis, and Epithelial Hyperproliferation. Cancer Res [Internet] 2004. [cited 2017March30]; 64:4405-10. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15231647; PMID:15231647; https://doi.org/ 10.1158/0008-5472.CAN-04-1032 [DOI] [PubMed] [Google Scholar]
- 48.Yang L, Moses HL. Transforming Growth Factor : Tumor Suppressor or Promoter? Are Host Immune Cells the Answer? Cancer Res [Internet] 2008. [cited 2017March30]; 68:9107-11. Available from: http://cancerres.aacrjournals.org/cgi/doi/10.1158/0008-5472.CAN-08-2556; PMID:19010878; https://doi.org/ 10.1158/0008-5472.CAN-08-2556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Partlová S, Bouček J, Kloudová K, Lukešová E, Zábrodský M, Grega M, Fučíková J, Truxová I, Tachezy R, Špíšek R, et al.. Distinct patterns of intratumoral immune cell infiltrates in patients with HPV-associated compared to non-virally induced head and neck squamous cell carcinoma. Oncoimmunology [Internet] 2015. [cited 2017March30]; 4:e965570. Available from: http://www.tandfonline.com/doi/full/10.4161/21624011.2014.965570; PMID:25949860; https://doi.org/ 10.4161/21624011.2014.965570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li B, Dewey CN. RSEM: accurate transcript quantification from RNA-Seq data with or without a reference genome. BMC Bioinformatics [Internet] 2011. [cited 2016September14]; 12:323. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21816040; PMID:21816040; https://doi.org/ 10.1186/1471-2105-12-323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.van Gool IC, Eggink FA, Freeman-Mills L, Stelloo E, Marchi E, de Bruyn M, Palles C, Nout RA, de Kroon CD, Osse EM, et al.. POLE Proofreading Mutations Elicit an Antitumor Immune Response in Endometrial Cancer. Clin Cancer Res [Internet] 2015. [cited 2016September23]; 21:3347-55. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25878334; PMID:25878334; https://doi.org/ 10.1158/1078-0432.CCR-15-0057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maduro JH, Noordhuis MG, ten Hoor KA, Pras E, Arts HJ, Eijsink JJ, Hollema H, Mom CH, de Jong S, de Vries EG, et al.. The prognostic value of TRAIL and its death receptors in cervical cancer. Int J Radiat Oncol Biol Phys [Internet] 2009. [cited 2016September14]; 75:203-11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19695437; PMID:19695437; https://doi.org/ 10.1016/j.ijrobp.2009.03.071 [DOI] [PubMed] [Google Scholar]
- 53.Noordhuis MG, Eijsink JJ, Ten Hoor KA, Roossink F, Hollema H, Arts HJ, Pras E, Maduro JH, Reyners AK, de Bock GH, et al.. Expression of epidermal growth factor receptor (EGFR) and activated EGFR predict poor response to (chemo)radiation and survival in cervical cancer. Clin Cancer Res [Internet] 2009. [cited 2016September14]; 15:7389-97. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19920104; PMID:19920104; https://doi.org/ 10.1158/1078-0432.CCR-09-1149 [DOI] [PubMed] [Google Scholar]
- 54.Daemen T, Riezebos-Brilman A, Regts J, Dontje B, van der Zee A, Wilschut J. Superior therapeutic efficacy of alphavirus-mediated immunization against human papilloma virus type 16 antigens in a murine tumour model: effects of the route of immunization. Antivir Ther [Internet] 2004. [cited 2015October14]; 9:733-42. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15535411; PMID:15535411 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.