Abstract
Depressed adolescents are characterized by negative interpretation biases. Although investigators have used cognitive bias modification for interpretation (CBM-I) to experimentally manipulate interpretation biases in depressed adults, the near- and far-transfer effects are not well understood in adolescents diagnosed with Major Depressive Disorder (MDD). In this study, we extend previous research by investigating the near- and far-transfer effects of 6 sessions of Positive versus Neutral CBM-I on independent measures of interpretation bias (near-transfer effects) and on attention biases and clinical symptoms (far-transfer effects) in a sample of adolescents with MDD (n=46). At post-training, adolescents who received Positive CBM-I interpreted ambiguous scenarios more positively than did participants who received Neutral CBM-I, providing evidence of training effectiveness. There was no evidence, however, of near- or far-transfer effects. These findings raise concerns about the malleability of interpretation biases in adolescent depression and suggest that further work is needed to establish the clinical utility of CBM-I for adolescents with MDD.
Keywords: depression, adolescents, cognitive bias modification, interpretation
Approximately 25% percent of adolescents are diagnosed with Major Depressive Disorder (MDD), and up to 70% of adolescents with MDD will experience recurrent depressive episodes throughout their lifetime (Birmaher, Arbelaez, & Brent, 2002; Kessler & Wang, 2009). Cognitive theories of depression posit not only that negative interpretation biases are present in MDD, but also that they increase risk for the onset, maintenance, and recurrence of depressive episodes (Beck, 1967; Teasdale, 1988). Although investigators have documented the presence of negative interpretation biases in adolescent depression (e.g., Orchard, Pass, & Reynolds, 2016), the causal role of interpretation biases in the maintenance of adolescents’ depressive symptoms is not yet clear.
Recently, researchers have developed cognitive bias modification (CBM) paradigms to test such causal relations. By experimentally altering cognitive biases, investigators have been able to examine the effects on cognitive functioning and clinical symptoms. In a seminal study, Mathews and Mackintosh (2000) developed a cognitive bias modification for interpretation (CBM-I) paradigm designed to train either positive or negative interpretation biases. Participants who received positive CBM-I offered more positive and fewer negative interpretations of new ambiguous scenarios than did participants who received negative CBM-I. The effectiveness of Mathews and Mackintosh’s CBM-I procedure has also been demonstrated in healthy adolescents using a modified version of the scenarios (e.g., Lothmann, Holmes, Chan, Lau, & Lau, 2011). Specifically, adolescents who received positive CBM-I endorsed more positive and fewer negative interpretations of new ambiguous situations than did adolescents who received negative CBM-I.
It is important to note, however, that questions have been raised about the effectiveness of CBM paradigms. For example, several recent meta-analyses concluded that although CBM alters the cognitive bias being trained, the effectiveness of training does not consistently extend to other tasks and has only a small effect, if any, on clinical symptoms (Cristea, Kok, & Cuijpers, 2015; Cristea, Mogoașe, David, & Cuijpers, 2015; Hallion & Ruscio, 2011). Concerns regarding the effectiveness of CBM studies can be conceptualized in terms of the extent of transfer of learning. The distinction between near and far transfer refers to the degree of overlap between training and transfer tasks (Ellis, 1965; Hertel & Mathews, 2011). Whereas CBM often generalizes to other tasks with processing requirements similar to those being trained (near-transfer tasks), the degree of transfer to more distal contexts (far-transfer tasks) is less consistent. Importantly, it is these far-transfer tasks that yield critical insights concerning the relations among cognitive biases, the mechanisms underlying successful CBM-I, and the clinical effects of training.
Researchers have begun to examine near- and far-transfer effects of CBM-I in depressed adults (Blackwell & Holmes, 2010; Lang, Blackwell, Harmer, Davison, & Holmes, 2012). Findings suggest that although interpretation biases can be experimentally manipulated, far-transfer effects are inconsistent, and potentially are related to the number of sessions provided. For example, whereas a single session of CBM-I did not influence depressed mood or affective responses to stress (Yiend et al., 2014), multiple sessions of CBM-I changed memory biases, decreased physiological stress reactivity (Joormann, Waugh, & Gotlib, 2015), and reduced the severity of depressive symptoms (Williams, Blackwell, Mackenzie, Holmes, & Andrews, 2013). An important exception, however, comes from work by Amir, Bomyea, and Beard (2010), who documented that, compared with control participants, individuals who received a single session of positive CBM-I were better able to disengage attention from threatening stimuli post-training, suggesting that the link between interpretation biases and attention biases is particularly robust.
Despite the promise of using CBM-I for depressed adults, there is little research examining CBM-I in depressed adolescents. This is particularly surprising given the formulation that CBM procedures have the potential to “drive powerful, long-lasting benefits” when administered at a younger age (Lau, 2013, p. 614). To date, only one study has examined CBM-I in youth with depressive symptoms. Micco, Henin, and Hirshfeld-Becker (2014) examined the effectiveness of four-sessions of positive versus neutral CBM-I in a sample of 14- to 21-year-old adolescents and young adults with symptoms of depression. Surprisingly, participants who received positive and neutral CBM-I did not differ in their pre- to post-training changes in interpretation biases or depressive symptoms; participants who received positive CBM-I did, however, report greater improvement in negative cognitions than those who received neutral CBM-I. Although this study is an important first step toward testing the effectiveness of CBM-I in depressed youth, the authors (1) included both adolescents (youth younger than 18 years) and young adults (youth aged 18 to 25; Simpson & Kettyle, 2008), thereby preventing us from determining whether these results would be observed in an exclusively adolescent sample; and (2) recruited youth with depressive symptoms, only 62% of whom met criteria for MDD. Moreover, because Micco et al. failed to find training-group differences in pre- to post-training changes in interpretation bias, it is difficult to interpret their findings regarding transfer effects. Thus, there has not yet been a valid test of the near- and far-transfer effects of CBM-I in adolescents diagnosed with MDD.
Given the potential benefits of CBM-I for adolescents (Lau, 2013), the present study was designed to examine near- and far-transfer effects of CBM-I in adolescents diagnosed with MDD. Depressed adolescents completed sessions of either positive or neutral CBM-I every other day over the course of 2 weeks, and we examined the effects of training on independent measures of interpretation biases (near-transfer effects) and on attention biases and clinical symptoms (far-transfer effects). We expected that participants who received positive CBM-I would exhibit more positive interpretation biases post-training than would participants who received neutral CBM-I. Moreover, we expected that the beneficial effects of training would transfer to other measures of interpretation biases, to attention biases, and to clinical symptoms, such that participants who received positive CBM-I would experience greater improvement in interpretation biases, attention biases, and depressive symptoms from pre- to post-training.
Method
Participants
Adolescents ages 13–17 years who met criteria for MDD were recruited through the Pediatric Mood Disorders Program in the Department of Psychiatry and Behavioral Sciences at Stanford University and through online advertisements. None of the adolescents reported major medical complications, head trauma, learning disorders, bipolar disorder, or an alcohol or substance use disorder within the past six months, and all were fluent in English. We screened approximately 115 individuals for initial inclusion and exclusion criteria with a telephone interview and invited 71 to the laboratory for further assessments. Of those, 49 were eligible for participation, and all but three participants returned for the post-training session; thus, we analyzed data from 46 adolescents diagnosed with MDD.
Previous studies that have used the CBM-I protocol utilized in the current study in a similar population (Joormann et al., 2015; Lothmann et al., 2011) reported effect sizes averaging d = 1.09. Power calculations based on the average effect size indicated that 20 participants per group were required to reach a power of 0.95 (ANOVA; Faul, Erdfelder, Lang, & Buchner, 2007; Howell, 2002), suggesting that the present sample was sufficiently powered to detect the expected effects.
Clinical Assessment
The Kiddie Schedule for Affective Disorders and Schizophrenia (Kaufman et al., 1997) is a structured clinical interview developed to determine DSM diagnoses. The KSADS was administered in the lab to the adolescents and their mothers (about their child) to confirm the adolescents’ diagnostic status. An independent rater who was blind to group membership listened to 20% of the diagnostic interviews; the diagnosis of MDD was confirmed in all cases (Κ = 1.0).
Interpretation Training
The CBM-I procedure used in the current study is described in detail in Mathews and Mackintosh (2000) and in Joormann et al. (2015). In the training phase, participants were exposed to ambiguous scenarios that ended with a word fragment that disambiguated the scenario in a positive or neutral direction.
To increase the ecological validity of training, the scenarios presented by Mathews and Mackintosh (2000) were adapted to include topics more relevant to adolescents. For example:
Having finished painting your room, you invite friends to come over and see it. As they walk into your room, you can see that they are surprised. Their reactions are one of (ple-s-re [pleasure]/cur–s-ty [curiosity]).
Scenarios were piloted by adolescents (n = 4) to confirm that they were age appropriate and that the disambiguated scenario would be classified as the intended valence. Scenarios that did not meet these criteria were eliminated or edited, as appropriate. Immediately after viewing each scenario, participants completed a comprehension question (e.g., “Did your friends like what you had done?”) that served to test whether the participants had read the scenario and to reinforce the valence of the scenario. Participants completed eight completely randomized blocks of 13 scenarios: eight training scenarios, two probe scenarios, and three filler scenarios. We created two versions of the task, each with unique scenarios, and asked participants to alternate between them at home, every other day, until they had completed six trainings. Given the nature of the computer-training task, participants were required to complete each training session in one sitting.
After completing the at-home trainings, participants returned to the laboratory to complete the Test Phase, during which they completed 20 novel ambiguous scenarios. Test scenarios were identical in structure to the training scenarios but the word fragment maintained the ambiguity of the scenario. Following a brief filler task (digit span), participants completed the interpretation test, in which they were presented with the title of each scenario and were asked to rate four sentences according to their similarity to the meaning of the original scenario (1 = very different to 4 = very similar). For each scenario, there were four sentence types: positive targets, negative targets, positive foils, and negative foils. Target sentences reflected participants’ interpretation of the scenario. Foil sentences were included to assess broader valence effects of the training.
CBM-I effectiveness was determined based on participants’ similarity ratings of positive versus negative sentences during the Test Phase (Mathews & Mackintosh, 2000). We restricted our analysis to scenarios for which participants answered the comprehension question correctly given that inaccurate responses on this basic comprehension question indicated that participants had not accurately read or did not recall the scenario; this procedure excluded 11.96% of the scenarios, which did not differ significantly by group, F(1, 43) < 1.00, p>.05.
We also examined participants’ adherence to the at-home training protocol by examining (1) the total number of training sessions completed, regardless of day; (2) the number of training sessions completed on separate days, as was instructed; and (3) participants’ accuracy on the comprehension questions.
Near Transfer: Independent Measures of Interpretation Bias
Scrambled sentences
The scrambled sentences task (SST; Wenzlaff, 1993) was one of two measures of interpretation bias that participants completed at pre- and post-training. In the SST, participants were given 3 minutes to unscramble 20 scrambled sentences. For each sentence, participants were asked to use five of the six words to create a grammatically correct sentence. Importantly, the task constrained participants to create either a positive or a negative sentence. For example, “looks the future bright very dismal” could be unscrambled to read, “the future looks very bright” (positive) or “the future looks very dismal” (negative). Two parallel versions were created with different scrambled sentences, and each was presented in a counterbalanced order at pre- or post-training.
Performance on the SST was evaluated based on the number of positive sentences created as a proportion of the total number of grammatically correct positive and negative sentences completed. Sentences were scored by two individuals who were blind to training condition, and discrepancies in scoring were reconciled by a study author (CE). Grammatically incorrect sentences comprised 12.07% of sentences at pre-training and 11.20% at post-training; the number of grammatically incorrect sentences did not differ significantly between participants who received Positive and Neutral CBM-I at pre-training or post-training, Fs(1, 43) < 1.00, all p > .05.
Blended words
Participants also completed the blended words task (Dearing & Gotlib, 2009). In this task, participants listened to ambiguous auditory stimuli that were constructed by acoustically blending two words that differed by only one phoneme (e.g., sad-sand). After listening to each stimulus, participants indicated which word they heard. The blended words task consisted of 10 negative-neutral (e.g., sad-sand) and 10 positive-neutral (e.g., joy-boy) test stimuli, and 20 control stimuli. Control stimuli were non-blended neutral (n = 10), negative (n=5), or positive (n=5) words. Neutral control stimuli were presented with either a positive or negative alternative. Negative and positive control stimuli were presented with a neutral alternative. Two parallel versions of the task were created with different word pairs, and each was presented in a counterbalanced order at pre- or post-training.
Although the primary dependent variable of the blended words task is participants’ performance on ambiguous test trials (Dearing & Gotlib, 2009), performance on unambiguous control trials allows us to assess general task performance because these trials have a clear right and wrong answer. Performance on the unambiguous control trials was evaluated based on percentage of items answered correctly for each of the four control conditions. Performance on the ambiguous test trials was determined by the percentage of trials on which participants reported hearing the emotional versus the neutral word.
Far-Transfer: Clinical Symptoms and Attention Biases
Attention biases
The dot-probe task was used to assess subliminal and supraliminal biases in attention. Pictures of 12 actors (6 female; 6 male), each displaying happy, sad, angry, and neutral expressions, were selected from the MacArthur Network Face Stimuli Set. Each of the emotional expressions was paired with the neutral expression of the same actor, creating 36 picture pairs. The picture pair was selected at random for each of the six trial types, which varied based on the valence of the picture pair (happy, sad, angry) and presentation duration (subliminal, supraliminal), for a total of 192 trials.
Each trial started with a 1,000 ms display of a black fixation cross in the middle of a white screen. Next, a picture pair was presented. In the subliminal condition, the picture pair was presented for 17 ms followed by a black-screen mask for 68ms; in the supraliminal condition, the picture pair was presented for 1,500 ms. The emotional expression appeared on the right and the left side of the screen with equal probability. Finally, a small black dot was presented with equal probability on the left or the right of the screen, in the location where one of the pictures had been. The dot remained on the screen until participants indicated its location.
Subliminal and supraliminal attentional bias scores were calculated based on the formulas presented by Mogg, Bradley, and Williams (1995). Consistent with previous research (e.g., Joormann & Gotlib, 2007), we restricted our analyses to accurate trials on which participants’ reaction times (RTs) were greater than 100 ms and less than 1,000 ms. We computed average RTs for each emotion type and probe location, and calculated attentional bias scores for each emotional expression. Attentional bias scores reflect the attention-capturing quality of emotional faces. Positive values of this bias indicate attention toward the emotional face relative to a matched neutral face; negative values indicate attention away from the emotional face relative to the neutral face.
Depressive symptoms
Severity of participants’ depressive symptoms was assessed with the 10-item version of the self-report Children’s Depression Inventory (CDI; Kovacs, 1985) and the 17-item interviewer-administered Children’s Depression Rating Scale-Revised (CDRS-R; Poznanski & Mokros, 1996), which was conducted by an experimenter who was blind to training group. Both of these measures have been documented to have strong psychometric properties (Kovacs, 1985; Mayes, Bernstein, Haley, Kennard, & Emslie, 2010). In the current sample, the CDI demonstrated acceptable internal consistency at pre-training (α = .86) and post-training (α = .84); similarly, the CDRS-R demonstrated acceptable internal consistency at pre-training (α = .70) and post-training (α = .78).
Potential Covariates
Anxiety was assessed via the 39-item Multidimensional Anxiety Scale for Children (MASC; March, Parker, Sullivan, Stallings, & Conners, 1997), which demonstrated acceptable internal consistency (α = .90). In addition, the Wechsler Intelligence Scale for Children–III (WISC-III; Wechsler, 1991) vocabulary subtest was administered to ensure that any group differences in the processing of emotional information were not a function of differences in verbal ability.
Procedure
This study was approved by the Stanford University Institutional Review Board. After providing informed consent, participants completed the KSADS and self-report questionnaires. Eligible participants were invited to return to the laboratory for their pre-training session within one week of their diagnostic evaluation. At pre-training, participants completed the CDRS-R interview, SST, blended words task, dot-probe task, and self-report questionnaires. The CBM-I procedure was then described to participants. They completed the first training task that day and the next five sessions at home, every other day, for two weeks. Participants were assigned to receive either Positive or Neutral CBM-I using stratified randomization, controlling for gender (Suresh, 2011), and they were given a laptop to take home with the trainings for their assigned condition. Participants and experimenters were blind to participants’ assigned condition. After training, participants returned to the laboratory for their post-training session. At post-training, participants completed the CBM-I test phase. In addition, participants completed an alternate version of the SST, an alternate version of the blended words task, the dot-probe task, self-report questionnaires, the CDRS-R interview, and the vocabulary test. Participants were paid $25 per hour for their participation in the study.
Results
Participant Characteristics
Participants’ demographic and clinical characteristics are presented in Table 1. Adolescents who received Positive CBM-I did not differ significantly from adolescents who received Neutral CBM-I with respect to the proportion of females, χ2(1, N = 46) < 1.00, ethnicity, χ2(2, N = 46) = 5.57, duration of their depressive episode, t(41) < 1.00, CDI scores, t(44) < 1.00, CDRS-R scores, t(44) < 1.00, severity of anxiety symptoms, t(44) < 1.00, proportion taking prescribed psychotropic medication, χ2(1, N = 46) < 1.00, proportion with a comorbid psychiatric disorder, χ2(1, N = 46) = 2.99, or WISC-III vocabulary subtest scale scores, t(44) = 1.23, all p > .05; however, adolescents who received Positive CBM-I were older than were adolescents who received Neutral CBM-I, t(44) = 3.16, p = .003. Thus, age at pre-training was included as a covariate in all analyses.
Table 1.
Participant Characteristics
| Variable | Neutral CBM-I (N = 22) |
Positive CBM- I (N = 24) |
|---|---|---|
| Baseline age, M(SD) | 14.59 (1.18) | 15.67 (1.13) |
| Female, % | 72.73% | 79.17% |
| Duration depressive episode (months) | 13.99 (13.54) | 18.78 (19.94) |
| Caucasian, % | 59.09% | 66.67% |
| Taking psychotropic medication, % | 54.55% | 41.67% |
| Comorbid psychiatric diagnosis, % | 58.33% | 81.81% |
| # trainings completed, M(SD) | 5.41 (1.18) | 5.13 (1.54) |
| # trainings completed separate days, M(SD) | 5.14 (1.32) | 4.58 (1.72) |
| % Training Accuracy, M(SD) | 96.46 (5.92) | 98.40 (1.01) |
| CDI, M(SD) | ||
| Pre-training | 26.55 (7.80) | 24.46 (7.65) |
| Post-training | 27.05 (8.07) | 24.62 (6.88) |
| CDRS-R, M(SD) | ||
| Pre-training | 52.23 (12.74) | 55.29 (9.39) |
| Post-training | 50.55 (9.85) | 51.33 (14.54) |
| MASC, M(SD) | 53.68 (19.34) | 53.75 (15.82) |
| WISC-III Vocabulary | 51.77 (5.26) | 49.67 (6.27) |
Note. CMB-I = Cognitive Bias Modification for Interpretation; CDI=Children’s Depression Inventory-Short Form; CDRS-R=Children’s Depression Rating Scale-Revised; MASC=Multidimensional Anxiety Scale for Children; WISC-III=Wechsler Intelligence Scale for Children Vocabulary Subtest
Interpretation Training
Adherence with the CBM-I protocol was good. Out of the six training sessions scheduled, adolescents completed an average of 5.26 training sessions (SD = 1.37) and an average of 4.85 training sessions on separate days (SD = 1.55). Participants’ performance on the comprehension questions also suggested good compliance with the training protocol. Overall, participants correctly answered 97.47% of the comprehension questions. Importantly, participants who received Positive CBM-I did not differ significantly from participants who received Neutral CBM-I with respect to the total number of trainings completed, F(1, 43) = 0.58, p > .05, the number of training sessions completed on separate days, F(1, 43) = 1.37, p > .05, or the number of comprehension questions answered correctly, F(1, 43) = 1.90, p > .05.
To examine the effects of CBM-I on participants’ performance during the Test Phase, we conducted a Training Group (Positive CBM-I, Neutral CBM-I) by Sentence Type (target, foil) by Sentence Valence (positive, negative) repeated-measures ANOVA on sentence ratings. This ANOVA yielded a significant interaction of Sentence Valence and Training Group, F(1, 43) = 6.66, p = .013, η2 = .134, 90% CI [0.016 – .289]. Follow-up tests revealed that, compared with adolescents who received Neutral CBM-I, adolescents who received Positive CBM-I endorsed more positive sentences (targets and foils) as similar to the original scenario, F(1,43) = 6.21, p = .017, η2 = .126, 90% CI [0.013 – .280]. The two training groups did not differ in their similarity ratings for negative sentences (targets and foils), F(1, 43) = 0.03, p = .874, η2 = .001, 90% CI [0.000 – .028]. No other main or interaction effects were significant, all F(1, 43) < 2.04, all p > .05.
Near Transfer: Independent Interpretation Bias Measures
Scrambled sentences
To examine whether CBM-I transferred to other, independent, measures of interpretation bias, we examined group differences in participants’ performance on the SST and blended words task (see Table 1 of the online supplemental materials). The two-way Training Group (Positive CBM-I, Neutral CBM-I) by Training Time (pre-training, post-training) repeated-measures ANOVA on percentage of positive sentences yielded no significant main or interaction effects, all F(1, 43) < 1.90, all p > .05.
Blended words
Before analyzing group differences in performance on the ambiguous test trials, the primary dependent variable of the blended words task (Dearing & Gotlib, 2009), we analyzed participants’ responses to the unambiguous control trials (see Table 1 of the online supplemental materials). We conducted a Training Group (Positive IBT, Neutral IBT) by Control Stimuli Type (neutral-positive pairs, neutral-negative pairs, positive-neutral pairs, and negative-neutral pairs) by Training Time (pre-training, post-training) repeated-measures ANOVA on the percent accuracy scores. This ANOVA yielded a significant main effect of Control Stimuli Type, F(3, 105) = 3.31, p = .023, η2 = .086, 90% CI [0.007 – .160], with participants being more accurate on neutral-positive pairs than positive-neutral pairs, F(1, 36) = 6.20, p = .018, η2 = 0.147, 90% CI [0.015 – .316], and more accurate on negative-neutral pairs than neutral-positive pairs, F(1, 36) = 5.12, p = .030, η2 = 0.125, 90% CI [0.007 – .291]. There was also a significant interaction of Training Group and Training Time, F(1, 35) = 6.37, p = .016, η2 = 0.15, 90% CI [0.016 – .325]. At pre-training, participants who received Positive and Neutral IBT did not differ significantly in their accuracy, F(1, 35) = 0.01, p = .583, η2 = 0.009, 90% CI [0.000 – .011]. At post-training, however, participants who received Positive IBT were more accurate than were participants who received Neutral IBT, F(1, 35) = 4.53, p = .040, η2 = .115, 90% CI [0.003 – .282]. No other main or interaction effects were significant, all F(1, 41) < 1.90, ps > .05, η2 < .051.
We next analyzed group differences in performance on the ambiguous test trials (Dearing & Gotlib, 2009; see Table 1 of the supplemental materials). We conducted a three-way Training Group (Positive CBM-I, Neutral CBM-I) by Test Stimuli Type (negative-neutral blend, positive-neutral blend) by Training Time (pre-training, post-training) repeated-measures ANOVA on the percent of test stimuli for which participants endorsed hearing the emotional versus neutral word. It yielded no significant main or interaction effects, all F(1, 35) < 3.73, all p > .05.
Far Transfer: Clinical Symptoms and Attentional Biases
Attentional biases
Attentional bias scores are presented in Table 2 of the supplemental materials. To test the effects of Positive versus Neutral CBM-I on attention to angry, happy, and sad emotional expressions, we conducted a four-way Training Group (Positive CBM-I, Neutral CBM-I) by Presentation Duration (subliminal, supraliminal) by Emotion (angry, happy, sad) by Training Time (pre-training, post-training) repeated-measures ANOVA on attentional bias scores. This ANOVA yielded a main effect of Training Time, F(1, 43) = 5.75, p = .021, η2 = .118, 90% CI [0.010 – .270]. Participants attended more to the emotional face relative to the neutral face at pre-training than at post-training. No other main or interactive effects were significant, all F < 2.97, all p > .09.
Clinical symptoms
We also tested whether CBM-I reduced adolescents’ depressive symptoms by conducting a two-way Training Group (Positive CBM-I, Neutral CBM-I) by Training Time (pre-training, post-training) repeated-measures multivariate analysis of variance (MANOVA) on CDI and CDRS-R scores. This MANOVA yielded no significant main or interaction effects, all F(2,42) < 1.87, all p > .05.
Exploratory Analyses
Previous research suggests that transfer effects are found only when multiple sessions of training are provided. Thus, we conducted exploratory analyses restricted to adolescents who completed more than one training session (Positive CBM-I n = 22, Neutral CBM-I n = 21). Paralleling findings in the full sample, adolescents who received Positive CBM-I interpreted ambiguous scenarios more positively than did participants who received Neutral CBM-I, F(1, 40) = 4.86, p = .033, η2 = .108, 90% CI = [0.005 – .264]; however, we found no near- or far-transfer effects, all p > .05. Given that CBM paradigms are designed to target negative interpretation biases, and that not all depressed adolescents exhibited negative biases, we also conducted exploratory analyses restricted to adolescents with negative interpretation biases at baseline (as measured by performance on either the SST or blended words task; Positive CBM-I n = 22, Neutral CBM-I n = 20). Findings in this subsample also paralleled those documented in the full sample. Finally, given evidence of gender differences in the prevalence of depression and in verbal ability (e.g., Maccoby & Jacklin, 1974), we examined whether both boys and girls exhibited training and transfer effects. Findings obtained separately for boys and girls paralleled the results obtained in the full sample; however, these gender findings should be interpreted with caution given the relatively small number of boys in the Positive CBM-I and Neutral CBM-I conditions.
Discussion
Researchers have documented the effectiveness of CBM-I in depressed adults and youth (e.g., Joormann et al., 2015; Micco et al., 2014). The present study extended this literature by testing the near- and far-transfer effects of CBM-I in adolescents with MDD. Our findings demonstrate that positive interpretation biases can be trained in depressed adolescents, but that the effectiveness of this training is restricted to the task on which participants were trained; in fact, we found no evidence of near- or far-transfer effects. These findings are important in elucidating the degree of malleability of interpretation biases in depressed adolescents and the extent to which training transfers to cognitive and clinical functioning.
Consistent with our expectations, adolescents who received positive CBM-I interpreted ambiguous scenarios as more positive than did participants who received neutral CBM-I. Interestingly, we found group differences in participants’ endorsement of both target and foil sentences, whereas the majority of previous studies with adults found group differences in participants’ endorsement of only target sentences (Joormann et al., 2015; Tran, Siemer, & Joormann, 2011). Foil sentences reflect a more general interpretation of the scenario and, thus, suggest the presence of broader valence effects of the training (Mathews & Mackintosh, 2000).
In contrast to evidence of near- and far-transfer effects in depressed adults (Amir et al., 2010; Lang et al., 2012; Yiend et al., 2014), CBM-I did not transfer to independent measures of interpretation bias (near transfer) or attentional biases (far transfer). Interpreting our results in light of the extant literature raises questions about the potential influence of development on the effectiveness of CBM-I for depression. Adolescence is marked by the maturation of the neural architecture underlying higher-level cognition, including the development of brain structures associated with cognitive biases and emotion regulation (Paus et al., 2008; Sternberg, 2005). Although this period of maturation could offer a valuable window of opportunity for intervention, the neural infrastructure may not yet be in place to facilitate transfer of training. This possibility is consistent with other research documenting no near or far-transfer effects of CBM-I in adolescents (e.g., Fu, Du, Au, & Lau, 2013).
Importantly, CBM-I did not affect depressive symptoms. This finding adds to existing concerns regarding the clinical utility of CBM in both adult (Hallion & Ruscio, 2011) and adolescent samples (Cristea, Mogoașe, et al., 2015), and yet contrasts with the considerable enthusiasm regarding the potential of CBM as an intervention for adolescents with psychopathology. There are several possible explanations for our null results. First, it is possible that although CBM-I effectively changes interpretation biases, interpretation biases are not causally related to adolescents’ depressive symptoms. This explanation, however, is contrary to well-established theoretical models of depression (Beck, 1967; Teasdale, 1988) and to empirical evidence from healthy adolescent samples (e.g., Lothmann et al., 2011). Second, it is possible that although CBM-I effectively changes interpretation biases, alternative methods are needed (e.g., a longer follow-up duration, examination of symptoms after experiencing a stressor) to elicit changes in clinical symptoms. Third, it is also important to consider that, for depressed adolescents, this CBM-I protocol did not change interpretation biases to the extent needed to elicit changes in clinical symptoms. Given the similarity between the training task and the test of bias change, demand characteristics could explain group differences in participants’ performance on the ambiguous scenarios post-test, as has been suggested elsewhere (Cristea, Mogoașe, et al., 2015; Lau, 2013). Thus, it is clear that additional research is needed to establish the clinical utility of CBM-I.
In the current study, participants completed the majority of CBM-I training sessions at home. Although a recent meta-analysis found that the effectiveness of CBM-I trainings administered at home did not differ from those administered in the laboratory or in a mental health facility (Cristea, Mogoașe, et al., 2015), trainings administered in a school setting produced a stronger effect than those administered in any other setting. Thus, it is possible that adolescents would receive additional benefit from CBM-I when administered in settings with more oversight and fewer distractions. Future research should examine more explicitly the effect of training location on training efficacy and transfer.
We should note three limitations of the current study. First, we did not include a no-training control condition, which would have allowed us to examine naturally occurring changes in cognitive biases and clinical symptoms over time. It is possible that, in the absence of training, cognitive biases and depressive symptoms would have worsened, and positive CBM-I might have minimized this deterioration in functioning. Second, we did not include a healthy control group. Given that researchers have documented the effectiveness of CBM-I in healthy controls (Lothmann et al., 2011) and the presence of interpretation biases in depression (Orchard et al., 2016), this control group was not essential or central to the goals of the current study. Finally, for ethical reasons we used a neutral, instead of a negative, CBM-I comparison condition. Neutral CBM-I may have provided a low-level positive training, thereby masking group differences and offering an alternative explanation for the null results documented here.
Despite these limitations, our results add to concerns regarding the effectiveness of CBM and call into question the utility of CMB-I for adolescents with MDD. Given the potential benefits of CBM procedures for youth, we hope that these findings encourage investigators to conduct additional research on alternative CBM-I protocols for depressed adolescents.
Supplementary Material
Figure 1.
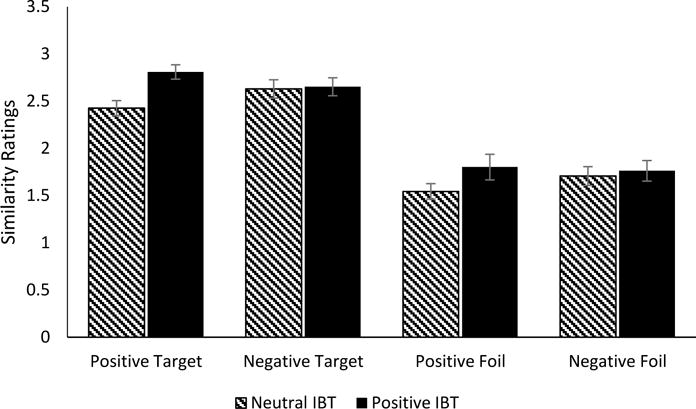
Interpretation training data. Similarity ratings by sentence valence (positive, negative) for those in the Neutral versus Positive CBM-I condition. Error bars indicate +/= 1 SE.
Acknowledgments
This study was funded by National Institute of Mental Health (NIMH) Grants R21-MH101545 (to IHG), F32-MH102013 (JLM), and K23-MH085919 (MKS) and the Brain & Behavior Research Foundation (formerly NARSAD; Young Investigator Award 22337 to JLM and Distinguished Investigator Award to IHG).
Footnotes
Conflict of Interest
The authors declare that they have no conflicts of interest.
References
- Amir N, Bomyea J, Beard C. The effect of single-session interpretation modification on attention bias in socially anxious individuals. Journal of Anxiety Disorders. 2010;24:178–182. doi: 10.1016/j.janxdis.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT. Depression: Clinical, experimental, and theoretical aspects. New York: Hoeber Medical Division; 1967. [Google Scholar]
- Birmaher B, Arbelaez C, Brent D. Course and outcome of child and adolescent major depressive disorder. Child and Adolescent Psychiatric Clinics of North America. 2002;11:619–37. doi: 10.1016/s1056-4993(02)00011-1. [DOI] [PubMed] [Google Scholar]
- Blackwell SE, Holmes EA. Modifying interpretation and imagination in clinical depression: A single case series using cognitive bias modification. Applied Cognitive Psychology. 2010;24:338–350. doi: 10.1002/acp.1680. [DOI] [Google Scholar]
- Cristea IA, Kok RN, Cuijpers P. Efficacy of cognitive bias modification interventions in anxiety and depression: Meta-analysis. British Journal of Psychiatry. 2015;206:7–16. doi: 10.1192/bjp.bp.114.146761. [DOI] [PubMed] [Google Scholar]
- Cristea IA, Mogoașe C, David D, Cuijpers P. Practitioner review: Cognitive bias modification for mental health problems in children and adolescents: A meta-analysis. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2015;56:723–34. doi: 10.1111/jcpp.12383. [DOI] [PubMed] [Google Scholar]
- Dearing KF, Gotlib IH. Interpretation of ambiguous information in girls at risk for depression. Journal of Abnormal Child Psychology. 2009;37:79–91. doi: 10.1007/s10802-008-9259-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis HC. The transfer of learning. Princeton, NJ: Macmillan; 1965. [Google Scholar]
- Faul F, Erdfelder E, Lang AGG, Buchner A. G * Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Fu X, Du Y, Au S, Lau JYF. Reducing negative interpretations in adolescents with anxiety disorders: A preliminary study investigating the effects of a single session of cognitive bias modification training. Developmental Cognitive Neuroscience. 2013;4:29–37. doi: 10.1016/j.dcn.2012.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallion LS, Ruscio AM. A Meta-analysis of the effect of cognitive bias modification on anxiety and depression. Psychological Bulletin. 2011;137:940–958. doi: 10.1037/a0024355. [DOI] [PubMed] [Google Scholar]
- Hertel PT, Mathews A. Cognitive bias modification: Past perspectives, current findings, and future applications. Perspectives on Psychological Science. 2011;6:521–536. doi: 10.1177/1745691611421205. [DOI] [PubMed] [Google Scholar]
- Howell DC. Statistical methods for psychology. 5th. Pacific Grove, CA: Duxbury; 2002. [Google Scholar]
- Joormann J, Gotlib IH. Selective attention to emotional faces following recovery from depression. Journal of Abnormal Psychology. 2007;116:80–5. doi: 10.1037/0021-843X.116.1.80. [DOI] [PubMed] [Google Scholar]
- Joormann J, Waugh CE, Gotlib IH. Cognitive bias modification for interpretation in major depression: Effects on memory and stress reactivity. Clinical Psychological Science. 2015;3:126–139. doi: 10.1177/2167702614560748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Ryan ND. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Wang PS. Epidemiology of depression. In: Gotlib Ian H, Hammen CL., editors. Handbook of depression. New York: Guilford; 2009. pp. 5–22. [Google Scholar]
- Kovacs M. The Children’s Depression, Inventory (CDI) Psychopharmacology Bulletin. 1985;21:995–998. doi: 10.3724/SP.J.1041.2015.01004. [DOI] [PubMed] [Google Scholar]
- Lang TJ, Blackwell SE, Harmer CJ, Davison P, Holmes EA. Cognitive bias modification using mental imagery for depression: developing a novel computerized intervention to change negative thinking styles. European Journal of Personality. 2012;26:145–157. doi: 10.1002/per.855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau JYF. Cognitive bias modification of interpretations: A viable treatment for child and adolescent anxiety? Behaviour Research and Therapy. 2013;51:614–622. doi: 10.1016/j.brat.2013.07.001. [DOI] [PubMed] [Google Scholar]
- Lothmann C, Holmes EA, Chan SWYY, Lau JYFF, Lau JYFF. Cognitive bias modification training in adolescents: Effects on interpretation biases and mood. Journal of Child Psychology and Psychiatry and Allied Disciplines. 2011;52:24–32. doi: 10.1111/j.1469-7610.2010.02286.x. [DOI] [PubMed] [Google Scholar]
- Maccoby EE, Jacklin CN. The psychology of sex differences. Vol. 1. Stanford: Stanford University Press; 1974. [Google Scholar]
- March JS, Parker JDA, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- Mathews A, Mackintosh B. Induced emotional interpretation bias and anxiety. Journal of Abnormal Psychology. 2000;109:602–615. doi: 10.1037/0021-843X.109.4.602. [DOI] [PubMed] [Google Scholar]
- Mayes TL, Bernstein IH, Haley CL, Kennard BD, Emslie GJ. Psychometric properties of the Children’s Depression Rating Scale-Revised in adolescents. Journal of Child and Adolescent Psychopharmacology. 2010;20:513–6. doi: 10.1089/cap.2010.0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micco JA, Henin A, Hirshfeld-Becker DR. Efficacy of interpretation bias modification in depressed adolescents and young adults. Cognitive Therapy and Research. 2014;38:89–102. doi: 10.1007/s10608-013-9578-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mogg K, Bradley BP, Williams R. Attentional bias in anxiety and depression: The role of awareness. British Journal of Clinical Psychology. 1995;34:17–36. doi: 10.1111/j.2044-8260.1995.tb01434.x. [DOI] [PubMed] [Google Scholar]
- Orchard F, Pass L, Reynolds S. “It was all my fault”; Negative interpretation bias in depressed adolescents. Journal of Abnormal Child Psychology. 2016;44:991–998. doi: 10.1007/s10802-015-0092-x. [DOI] [PubMed] [Google Scholar]
- Simpson R, Kettyle W. MIT Young adult development project. 2008 Retrieved from http://hrweb.mit.edu/worklife/youngadult/
- Suresh K. An overview of randomization techniques: An unbiased assessment of outcome in clinical research. Journal of Human Reproductive Sciences. 2011;4:8–11. doi: 10.4103/0974-1208.82352. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Teasdale J. Cognitive vulnerability to persistent depression. Cognition & Emotion. 1988;2:247–274. doi: 10.1080/02699938808410927. [DOI] [Google Scholar]
- Tran TB, Siemer M, Joormann J. Implicit interpretation biases affect emotional vulnerability: A training study. Cognition & Emotion. 2011;25:546–558. doi: 10.1080/02699931.2010.532393. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Intelligence Scale for Children-III. San Antonio, TX: The Psychological Corporation; 1991. [Google Scholar]
- Wenzlaff RM. The mental control of depression: Psychological obstacles to emotional well-being. In: Wegner DM, Pennebaker JW, editors. Handbook of mental control. Englewood Cliffs, NJ: Prentice Hall; 1993. pp. 239–257. [Google Scholar]
- Williams AD, Blackwell SE, Mackenzie A, Holmes EA, Andrews G. Combining imagination and reason in the treatment of depression: A randomized controlled trial of internet-based cognitive-bias modification and internet-CBT for depression. Journal of Consulting and Clinical Psychology. 2013;81:793–799. doi: 10.1037/a0033247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yiend J, Lee JS, Tekes S, Atkins L, Mathews A, Vrinten M, Shergill S. Modifying interpretation in a clinically depressed sample using “cognitive bias modification-errors”: A double blind randomised controlled trial. Cognitive Therapy and Research. 2014;38:146–159. doi: 10.1007/s10608-013-9571-y. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


