Abstract
Introduction
Tobacco demand (i.e., relative value attributed to a given reinforcer) and delay discounting (i.e., relative preference for smaller immediate rewards over larger delayed rewards) are two behavioral economic processes that are linked to the progression of problematic substance use. These processes have not been studied among those with psychopathology, a vulnerable group of smokers. The current study examined differences in tobacco demand and delay discounting, and their association with smoking topography among smokers with (n=43) and without (n=64) past-year psychopathology.
Method
Adult daily smokers (n = 107, Mage = 43.5; SD = 9.7) participated in a study on “smoking behavior.” Past-year psychological disorders were assessed via a clinician-administered diagnostic assessment. All subjects participated in an ad libitum smoking trial and then completed an assessment of delay discounting (Monetary Choice Questionnaire) and tobacco demand (Cigarette Purchase Task) approximately 45–60 minutes post-smoking.
Results
Smokers with psychopathology, compared to those without, had significantly higher demand intensity and maximum expenditure on tobacco (Omax), but did not differ on other demand indices or delay discounting. Smokers with psychopathology had shorter average inter-puff intervals and shorter time to cigarette completion than smokers without psychopathology. Tobacco demand and delay discounting measures were significantly intercorrelated among smokers with psychopathology, but not those without. Both behavioral economic measures were associated with specific aspects of smoking topography in smokers with psychopathology.
Discussion
The association between tobacco demand and delay discounting is evident among smokers with psychopathology and both measures were most consistently related to smoking behavior.
Keywords: cigarette purchase task, delay discounting, smoking topography, relative value, comorbidity
1. Introduction
Despite reductions in the prevalence in smoking over the past fifty years (United States Department of Health and Human Services, 2014), approximately 36.5 million Americans still smoke which is about 15.1% of the US population (Centers for Disease Control and Prevention, 2016). However, the prevalence of smoking among individuals with a psychological disorder is significantly higher (36.1%) than the general population (Centers for Disease Control and Prevention, 2013; Lasser et al., 2000; McClave et al., 2010) and has remained relatively stable at this rate over recent years (Centers for Disease Control and Prevention, 2013). Increased scholarly efforts have focused on understanding factors contributing to the maintenance of smoking and stagnated cessation rates among this vulnerable sub-set of smokers.
One way to study smoking behavior among those with psychopathology is through a behavioral economics framework. Behavioral economics integrates principles from psychology and economics in an effort to analyze key processes involved in decision-making (Camerer, 1999). This framework has been applied to understand substance use behaviors through the “reinforcer pathology” model (Bickel et al., 2014, 2011). Reinforcer pathology comprises the dual effects of two fundamental processes related to the progression of problematic substance use: (a) persistently elevated value attributed to a given reinforcer and/or (b) the excessive preference for obtaining or consuming a given reinforcer immediately despite long-term consequences (Bickel et al., 2014, 2011). This theoretical model posits that individuals with substance use disorders, dependence, or problematic use may regularly attribute high value to a preferred substance while also exhibiting a desire to obtain and use it instantaneously. Two behavioral economic indices allow for objective evaluation of reinforcer pathology: substance demand and delay discounting (DD).
Substance demand pertains to the perceived value of a given substance (Hursh et al., 2005). Cigarette purchase tasks (CPT) are one way to assess demand for tobacco via examination of hypothetical tobacco consumption at a range of prices (MacKillop et al., 2008). These tasks capture related, yet distinct, aspects of tobacco demand including: intensity (amount of tobacco consumed at zero cost), Pmax (price at maximum expenditure for tobacco), Omax (peak expenditure for tobacco), breakpoint (cost whereby tobacco consumption is suppressed to zero), and elasticity of demand (the degree to which consumption decreases with increasing price). Tobacco demand indices appear to be moderately correlated with tobacco dependence and smoking frequency (MacKillop et al., 2008; Murphy et al., 2011), increase in response to acute nicotine deprivation and cue-induced craving (MacKillop et al., 2012), and are associated with lower motivation for smoking cessation (Murphy et al., 2011). Limited work has examined the impact of psychopathology on tobacco demand. Initial studies indicate that elevated depression symptoms and emotional disorders are associated with higher tobacco demand indices, especially under stress (Dahne et al., 2017a) or nicotine-deprived states (Farris et al., 2017). Other work has found that smokers with schizophrenia had higher intensity of demand, relative to healthy controls, when completing a hypothetical CPT under satiated states (MacKillop and Tidey, 2011). Thus, available data, albeit limited, indicates that smokers with various forms of psychopathology may have volumetric differences (e.g., heavy use) in demand.
DD refers to the propensity to discount future rewards over immediate rewards (MacKillop et al., 2011). For example, when asked to choose between a larger, delayed amount of money (e.g., $100 in 6 months) and an immediate smaller amount of money (e.g., $75 today), the rate at which a participant switches from preferring the smaller-sooner reward to a larger-later reward can be plotted as a function of delay (i.e., discount function), with steeper DD reflecting greater impulsive behavior. The undervaluation of future rewards (steeper DD) is a key characteristic of problematic health behaviors (Amlung et al., 2017, 2016), including cigarette smoking (Amlung et al., 2017). Additionally, steeper DD has been observed in various psychological disorders, including those characterized by impulsivity (hypomania/mania, attention deficit-hyperactivity disorder), disorders of cognitive or executive dysfunction (e.g., schizophrenia), disorders involving future-focused uncertainty/fear (e.g., posttraumatic stress disorder, anxiety disorders, borderline personality disorder; Cáceda et al., 2014; Story et al., 2016). Despite the clear documented link between psychological disorders and DD, limited work has examined the nature of DD among smokers with psychological disorders. Self-reported depression has been found to be related to steeper delay discounting in treatment-seeking pregnant female smokers (Yoon et al., 2007) and adolescents (Imhoff et al., 2014), but not in all cases (Weidberg et al., 2015a). In smokers with schizophrenia, DD was not significantly different from healthy controls (MacKillop and Tidey, 2011), although discounting rate appears to be steeper among current and former smokers with schizophrenia relative to never smokers with schizophrenia (Wing et al., 2012). Thus, some data indicate that psychopathology influences DD in smokers.
In the current study, we examined the nature of tobacco demand and DD in smokers with various forms of psychopathology (internalizing and externalizing disorders) versus those without. Despite heterogeneity in disorders, common underlying factors (e.g., high levels of emotional distress, poor coping with negative distress states, difficulties with emotion regulation) promote and maintain both internalizing and externalizing disorders (e.g., substance use, eating disorders, anxiety disorders, mood disorders; Mennin et al., 2007; Tice et al., 2001). Thus, we aimed to explore these associations among smokers with various forms of psychopathology. Specifically, among non-treatment seeking daily smokers, we examined differences in demand and DD among smokers with and without past-year psychopathology, following approximately 60 minutes of smoking deprivation. This assessment window allowed for the onset of tobacco craving, which can occur within 30 minutes of not smoking (Hendricks et al., 2006). Based on the existing literature, it was hypothesized that smokers with psychopathology would exhibit elevated demand and steeper DD. Additionally, we explored the associations between demand and DD as a function of psychopathology status and their association with smoking topography, a behavioral index of smoking reinforcement.
2. Material and Methods
2.1 Participants
Non-treatment seeking adult daily smokers were recruited for an experimental study on “smoking behavior” (Farris and Zvolensky, 2016). Community-recruited individuals who were between 18–65 years of age, reported smoking 10 or more cigarettes per day for at least one year, and smoked within the first 30 minutes of waking in the morning, were invited for a baseline assessment to determine eligibility for the experimental study (Farris and Zvolensky, 2016). Participants were excluded from participation during an initial telephone screen if they reported frequent drinking (≥ 9 standard drinks/week), illicit drug use (≥ 3 days/week), unstable medical conditions, or current psychotic symptoms. The current study is a secondary analysis of data from participants who completed the baseline assessment (n = 126), regardless of eligibility for the experimental phase of the study.
2.2 Measures
2.2.1 Demographic Characteristics
Demographic characteristics were assessed via self-report. The Financial Strain Questionnaire (Pearlin et al., 1981), which was adapted from an economic strain measure, was used as a proxy for income. The FSQ, is an 8-item self-reported measure that assesses perceived difficulty affording clothes, leisure activities, car, furniture, and other necessities (i.e., medical care, housing). Items that are rated on a scale from 1 to 3 (e.g., “I have enough money”, “I have somewhat enough money”, “I don’t have enough money”). Monetary status at the end of the month is also assessed using a similar scaling (1 = some money left over, 3 = no money left over). Items are summed to derive a total financial strain index, with higher scores indicating greater strain (possible range 8–24).
2.2.2 Smoking History
The Smoking History Questionnaire (SHQ; Brown et al., 2002), a 30-item self-report measure, was used to gather information about smoking history to establish pattern of cigarette use per eligibility criteria (e.g., daily use). A Carbon Monoxide (CO) Analysis, using the Vitalograph Breath Co carbon monoxide monitor, was conducted to measure the amount of CO (in parts per million [ppm]) in an expired breath sample. The Timeline Follow-Back Interview (Brown et al., 1998) is a calendar-based assessment of substance use, which was used to document frequency, quantity, and patterns of tobacco use in the past 30 days. The Fagerström Test for Cigarette Dependence (Fagerström, 2012), a 6-item scale that assesses gradations in cigarette dependence, was used to assess the level of physiological dependence on tobacco (range 0–10, with higher scores reflecting higher levels of dependence). The FTCD has adequate internal consistency and is associated with biochemical indicators of smoking (Heatherton et al., 1991; Pomerleau et al., 1994)
2.2.3 Psychopathology Assessment
The Structured Clinical Interview for DSM-IV Disorders-Non-Patient Version (SCID-I/NP; (First et al., 2007), a clinician-administered semi-structured diagnostic assessment, was used to assess the presence of past-year psychopathology based on the DSM-IV-TR diagnostic guidelines. Diagnostic assessments were conducted by highly-trained post-baccalaureate research assistants. In the current study, all diagnostic assessments were audio-recorded and 100% of cases were supervised for diagnostic accuracy. A random 20% of recordings were subjected to blinded inter-rater reliability review by a doctoral-level clinical psychology graduate student. No cases of diagnostic disagreement were noted.
2.2.4 Tobacco Demand
The Cigarette Purchase Task (MacKillop et al., 2008) was used to assess the relative value of tobacco. The CPT is based on progressive-ratio operant schedules wherein participants self-report their cigarette consumption under various levels of price, and has been previously validated (MacKillop et al., 2008; Murphy et al., 2011). A state version of the CPT (Hitsman et al., 2008) was used in the current study. Participants were provided with the following task instructions: “Imagine that you could smoke RIGHT NOW. The following questions ask how many cigarettes you would consume if they cost various amounts of money. Assume the available cigarettes are your favorite brand. Assume that you have the same income/savings that you have now and NO ACCESS to any cigarettes or nicotine products other than those offered at these prices. In addition, assume that you would consume cigarettes that you request at this time. You cannot save or stockpile cigarettes for a later date. Be sure to consider each price increment carefully.” The CPT was completed approximately 60 minutes post-smoking, and was administered on the computer where each of the 22 questions/prices were presented one at a time, and read: “How many cigarettes would you smoke RIGHT NOW if they were: Free [$0/pack], 1¢ each [20¢/pack], 5¢ each [$1/pack], 10¢ each [$2/pack], 20¢ each [$4/pack], 30¢ each [$6/pack], 40¢ each [$8/pack], 50¢ each [$10/pack], 60¢ each [$12/pack], 70¢ each [$14/pack], 80¢ each [$16/pack], 90¢ each [$18/pack], $1 each [$20/pack], $2 each [$40/pack], $3 each [$60/pack], $4 each [$80/pack], $5 each [$100/pack], $6 each [$120/pack], $7 each [$140/pack], $8 each [$160/pack], $9 each [$180/pack], $10 each [$200/pack]?”
2.2.5 Delay Discounting
The Monetary Choice Questionnaire (Kirby et al., 1999) is a 27-item measure that yields three indices of DD for small, medium, and large-sized rewards. Participants must choose either a smaller, immediate reward (e.g., receive $15 today) or a larger, delayed reward (e.g., receive $35 in 13 days) for each item. To minimize burden while retaining discounting at multiple magnitudes, only the large ($75 – $85) and small ($25 – $35) magnitude items were used in analyses consistent with other studies (MacKillop and Tidey, 2011).
2.2.6 Smoking Topography
The Clinical Research Support System (CReSS; Plowshare Technologies, Borgwaldt KC, Inc., Virginia), specifically the portable CReSS pocket device, was used to assess puff topography. The device has a sterilized flow meter mouthpiece that is connected to a pressure transducer, which converts pressure into a digital signal that is sampled at 1,000Hz. CReSS computer software transforms the signal to a flow rate (mL/s), from which puff topography data are computed. The reliability and acceptability of use of the portable CReSS device is well documented (Blank et al., 2009; Perkins et al., 2012), and is recommended over direct observation (Blank et al., 2009). Puff topography data included: puff volume (amount of CO in mL of smoke inhaled), puff duration (time in seconds inhaled during puff), inter-puff interval (time in seconds between successive puffs), number of puffs, and total time spent smoking (minutes). Puff-level data were averaged to create mean scores.
2.3 Procedure
Participants were screened for potential eligibility by telephone, scheduled for an in-person appointment and instructed to bring their usual brand of cigarettes (at least 2 full cigarettes) to the laboratory. Upon arrival, participants provided a carbon monoxide (CO) analysis of expired breath to verify recency of smoking, completed a diagnostic clinical interview and a series of self-report assessments. Next, all participants completed an ad libitum smoking trial at a standardized point during the baseline assessment (approximately 90 minutes after arrival to the laboratory). Participants were told they could have a ‘smoke break’ during which they were oriented to the portable CReSS device and shown how to use it. The experimenter accompanied the participant outdoors, alongside the laboratory, and informed the participant that he/she would have the opportunity to smoke one cigarette using the device. The participant was told to smoke as usual, and was given as much time as desired. Next, the participants returned inside the laboratory and completed approximately 75 minutes of computerized self-report assessments, which were broken up by two scheduled snack/water breaks (no smoking or caffeine was permitted). The MCQ and CPT were completed at approximately 45 minutes and 60 minutes post-smoking (respectively); thus, all participants were in acute nicotine-deprivation. All participants were compensated $25 for completing the baseline assessment.
2.4 Data Analytic Procedures
Calculations of demand indices were obtained using the following methods. Price elasticity values were generated by fitting individual curves in GraphPad Prism using a exponential demand equation (Koffarnus et al., 2015), Q = Q0 × 10k(e−αQ0C−1), where Q = quantity consumed, Q0 = derived intensity, k = a constant across individuals that denotes the range of the dependent variable (tobacco cigarettes), C = the cost of the commodity, and α = elasticity or the rate constant determining the rate of decline in consumption based on increases in price (i.e., essential value). This is a modification to a prior (Hursh and Silberberg, 2008) exponential demand equation that does not require eliminating or substituting for consumption values of zero. The appropriate k value was determined by subtracting the log10-transformed average consumption at the highest price ($10.00) from the log10-transformed average consumption at the lowest price used in curve fitting ($0.01). The k value used in analyses was 1.743. An R2 value was generated to reflect percentage of variance accounted for by the demand equation (i.e., the adequacy of the fit of the model to the data).
Data cleaning procedures were completed consistent with standard recommendations (Stein et al., 2015). Raw CPT data were examined for outliers using standard scores, with a criterion of Z = 3.29 to retain maximum data. A small number of outliers were detected (1.2%). The outliers were determined to be legitimate high-magnitude values and were recoded as one unit higher than the next lowest non-outlying value between subjects within a single price (Tabachnick and Fidell, 2000). Observed values for intensity, Omax, Pmax, and breakpoint were estimated by directly examining CPT performance. Elasticity of demand was empirically derived using values generated from an exponentiated demand curve model.
Procedures outlined (Kirby, 2000) were used to infer values of the hyperbolic discount parameter (k) from a subject’s choices between immediate and delayed rewards. Consistency values were generated for each subjects’ k parameter to index the percentage of the participants’ choices that did not contradict the discounting function. Only the small and large reward magnitude items were used in this study to maintain consistently with previous work (MacKillop and Tidey, 2011).
All data were examined for distribution normality using histograms. All tobacco demand and MCQ variables were non-normally distributed. A square root transformation was used for intensity, log10 transformation was used for Omax, and cube root transformation was used for Pmax, breakpoint, and elasticity. A square root transformation was used for k values (small, large) on the MCQ. Puff volume, duration, and inter-puff Interval were also non-normally distributed. Puff volume and duration were square-root transformed, and inter-puff interval was log-transformed and then cubic transformed. These transformations were successful in normalizing the data. All transformations improved the distribution substantially.
Primary analyses examined the demand curve indices, k values, and smoking topography by smokers with and without psychopathology. Analysis of covariance (ANCOVA) was used. Any between-group differences on demographic characteristics were entered as covarying factors, consistent with prior work (MacKillop and Tidey, 2011). Next, bivariate zero-order correlations were used to examine the associations between demand curve indices, k values, and smoking topography. The correlations were stratified by psychopathology status to examine the unique associations between indices as a function of psychopathology. Significance was defined as α < .05 for descriptive analyses. Demand curve modeling was conducted using GraphPad Prism 7 and all other analyses were conducted using SPSS 23.0.
3. Results
Of the 126 cases, 11 showed evidence of inconsistent responding across prices on the CPT (i.e., had ≥3 reversals), and 4 cases exhibited constant demand, suggesting low effort during this task. Additionally, 6 cases had low consistency on the MCQ (k ≤ .778) and 2 cases were missing smoking topography data due to equipment malfunction. This results in 19 excluded cases from analyses. The modified exponential demand equation (Koffarnus et al., 2015) provided an excellent fit to the CPT data (R2 = .972) and a good fit to the individual data (median R2 = .847, interquartile range = .763 – .904).
3.1 Sample Characteristics
Participants (n = 107; Mage = 43.5; SD = 9.7; 43.9% female) identified race as Black/African-American (58.9%), white (33.6%), American Indian/Alaska Native (1.9%), Asian (0.9%), or other (4.7%), and 5.6% of participants identified ethnicity as Hispanic. Marital status was reported as: never married (49.5%), divorced/separated (34.5%), married/co-habitating (11.2%), and widowed (4.7%). Approximately half of the sample completed at least some college (57.0%). Employment status was reported as unemployed (39.3%), employed full time (25.2%), employed part time (23.4%), student (3.7%), disabled (7.5%), and retired (0.9%). On average, elevated financial strain was reported (M = 17.2, SD = 5.03).
Smokers with past-year psychopathology (n = 43; 40.2%) met criteria for the following disorders (range 1–4 diagnoses): posttraumatic stress disorder (30.2%), major depressive disorder (23.3%), specific phobia (20.9%), alcohol use disorder (16.3%), social anxiety disorder (16.3%), dysthymic disorder (11.6%), panic disorder with/without agoraphobia (9.3%), cannabis use disorder (9.3%), eating disorder (7.0%), generalized anxiety disorder (4.7%), bipolar disorder I (4.7%), bipolar disorder II (4.7%), obsessive-compulsive disorder (2.3%), psychotic disorder (2.3%), sedative use disorder (2.3%).
3.2 Group Differences
See Table 1 for comparison of demographic and smoking characteristics by smokers with and without psychopathology. Smokers with psychopathology reported significantly greater economic strain (per the FSQ), however did not differ in terms of other demographic characteristics. Regarding smoking behavior, there were no group differences in cigarettes/day, level of tobacco dependence, or use of menthol cigarettes. However, smokers with psychopathology had significantly shorter inter-puff intervals and smoked more quickly, indicated by total time spent smoking, relative to smokers without psychopathology.
Table 1.
Characteristics of smokers with and without psychopathology
| Any Psychopathology(n=43) | No Psychopathology(n=64) | |||
|---|---|---|---|---|
| M (SD)n (%) | M (SD)n (%) | t, x2 | p | |
| Sex (female) | 20 (46.5%) | 57 (42.2%) | .195 | .659 |
| Age | 42.42 (10.18) | 44.27 (9.45) | 0.96 | .339 |
| Race (black) | 26 (60.5%) | 37 (57.8%) | 0.08 | .785 |
| Education (≥part college) | 26 (60.5%) | 35 (54.7%) | 0.35 | .554 |
| Financial strain (FSQ) | 18.65 (4.64) | 16.23 (5.08) | −2.50 | .014* |
| Menthol Cig (yes) | 27 (62.8%) | 37 (57.8%) | 0.27 | .607 |
| Cigs/day | 15.06 (7.01) | 14.84 (5.47) | −0.17 | .863 |
| Tobacco dependence (FTCD) | 4.79 (1.57) | 4.63 (1.45) | −0.56 | .576 |
| Puff Volume (mL) | 65.54 (24.29) | 63.18 (24.35) | −0.50 | .620 |
| Puff Duration (sec) | 1.79 (0.69) | 1.76 (0.60) | −0.037 | .971 |
| Inter-Puff Interval (sec) | 11.55 (4.85) | 14.33 (5.39) | 2.73 | .007** |
| Time/Smoking (min:sec) | 4:28 (1:30) | 5:15 (1:17) | 2.90 | .005** |
| Puff/number | 20.53 (6.93) | 20.42 (7.38) | −0.08 | .937 |
p < .05;
p < .01
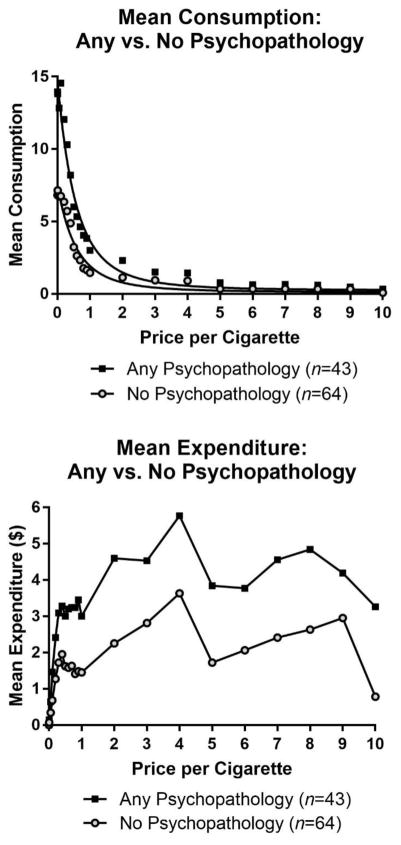
Untransformed indices of CPT and MCQ are presented in Table 2 by psychopathology status. Results indicated that, while covarying for economic strain (FSQ scores), there was a significant difference in demand intensity and Omax. Specifically, smokers with psychopathology had significantly higher consumption when price was unrestricted (intensity) and were willing to expend a significantly higher maximum amount of money for cigarettes (Omax). See Figure 1 for mean consumption and expenditure by psychopathology status on the CPT. There were no observed group differences in discounting of delayed rewards on the MCQ.
Table 2.
Behavioral economic measures by psychopathology status
| Any Psychopathology(n=43) | No Psychopathology(n=64) | |||||
|---|---|---|---|---|---|---|
| M | SEM | M | SEM | F | p | |
| Intensity | 13.73 | 2.02 | 6.96 | 1.64 | 6.80 | .023* |
| Omax | 11.75 | 2.65 | 5.75 | 2.16 | 5.10 | .026* |
| Pmax | 2.22 | 0.41 | 1.50 | 0.33 | 1.44 | .233 |
| Breakpoint | 2.71 | 0.46 | 2.30 | 0.38 | 1.02 | .314 |
| Elasticity | 0.24 | 0.14 | 0.43 | 0.11 | 2.46 | .120 |
| Small k | 0.07 | 0.01 | 0.09 | 0.01 | 1.32 | .253 |
| Large k | 0.04 | 0.01 | 0.06 | 0.01 | 1.05 | .309 |
p < .05;
p < .01;
non-transformed adjusted means are presented controlling for FSQ
Figure 1.
Mean Consumption and Expenditure stratified by Psychopathology status
3.3 Exploratory Correlational Analyses
To characterize overlap among demand, delayed discounting, and smoking topography, a correlation matrix stratified by psychopathology status is presented in Table 3.
Table 3.
Correlations between behavioral economic measures and smoking topography by psychopathology status
| Intensity | Omax | Pmax | Breakpoint | Elasticity | DD Small | DD large | Puff Volume | Puff Duration | IPI | Time Smoke | # of Puffs | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intensity | -- | .681** | .224† | .306* | −.322** | −.105 | −.156 | −.200 | −.160 | −.250* | −.032 | .237† |
| Omax | .589** | -- | .700** | .727** | −.715** | .035 | −.004 | −.149 | −.175 | −.205 | −.002 | .264* |
| Pmax | .119 | .683** | -- | .927** | −.584** | .061 | .039 | .021 | .014 | −.071 | −.025 | .079 |
| Breakpoint | .276† | .746** | .777** | -- | −.636** | .034 | .009 | .031 | .076 | .030 | −.009 | −.082 |
| Elasticity | −.431** | −.769** | −.415** | −.535** | -- | .029 | −.005 | .089 | .152 | .105 | .070 | −.127 |
| DD Small k | .098 | .157 | .275† | .207 | −.059 | -- | .757** | .077 | −.089 | −.015 | −.114 | .068 |
| DD large k | .148 | .351* | .364* | .368* | −.221 | .754** | -- | .022 | −.040 | .138 | −.059 | −.099 |
| Puff Volume | .144 | −.040 | −.066 | −.033 | .083 | −.115 | −.020 | -- | .730** | .166 | −.235† | −.399** |
| Puff Duration | −.045 | −.246 | −.061 | −.099 | .241 | .227 | .227 | .594** | -- | .167 | −.244† | −.478** |
| IPI | .001 | −.337* | −.326* | −.399** | .335* | .109 | −.124 | .254 | .463** | -- | .462** | −.706** |
| Time Smoke | .013 | −.316* | −.316* | −.385* | .302* | −.040 | −.166 | .258† | .274† | .687** | -- | .221† |
| # of Puffs | .002 | .092 | .071 | .106 | −.140 | −.371* | −.192 | −.079 | −.431** | −.507** | .149 | -- |
Note: Above diagonal = smokers without psychopathology; Below diagonal = smokers with psychopathology; bolded values reflect significant associations between CPT, MCQ, and Topography.
p < .10
p < .05;
p < .01
3.3.1 Smokers without Psychopathology
Among smokers without psychopathology (n=64), tobacco demand and DD indices were not significantly related. Demand intensity was significantly negatively correlated with inter-puff interval (r[62] = −.25, p = .046) and positively correlated with number of puffs at a trend level (r = .24[62], p = .059). Additionally, Omax was significantly positively correlated with number of puffs (r[62] = .26, p = .035). After controlling for FTND scores, the correlations between demand intensity with inter-puff interval (r[61] = −.19, p = .137) and number of puffs (r[61] = .20, p = .124) were non-significant, and the correlation between Omax and number of puffs approached significance (r[61] = .23, p = .067).
3.3.2 Smokers with Psychopathology
Among smokers with psychopathology (n=43), there were several observed significant associations between demand and DD indices. Specifically, Omax, Pmax, and breakpoint were significantly positively correlated with large k, indicating steeper DD (large delayed rewards). After controlling for FTND, all correlations remained significant: Omax (r[40] = .35, p = .024); Pmax (r[40] = .37, p = .017); and breakpoint (r[40] = .37, p = .017). Additionally, Pmax was positively correlated with small k, reflecting steeper discounting of small delayed rewards, which was significant at a trend level (r[41] = .28, p = .074; r[40] = .28, p = .073). Demand indices were significantly correlated with smoking topography indices. Omax, Pmax, breakpoint were significantly negatively associated with inter-puff interval and elasticity was significantly positively associated with inter-puff interval. These correlations remained significant after controlling for FTND scores: Omax (r[40] = −.33, p = .031); Pmax (r[40] = −.33, p = .034); breakpoint (r[40] = −.40, p = .009); elasticity (r[40] = .34, p = .030). Omax, Pmax, breakpoint were also significantly negatively associated with time spent smoking and elasticity was significantly positively associated with time spent smoking. These associations remained significant after controlling for FTND scores: Omax (r[40] = −.34, p = .030); Pmax (r[40] = −.32, p = .042); breakpoint (r[40] = −.39, p = .011); and elasticity approached significance (r[40] = .30, p = .051). In addition, small k was significantly negatively correlated with number of puffs (r[41] = −.37, p = .014; r[40] = −.39, p = .010).
4. Discussion
Among community-recruited daily smokers, two indices of tobacco demand were significantly higher among smokers with psychopathology versus those without: demand intensity (hypothetical tobacco consumption when price is unrestricted) and Omax (peak expenditure for tobacco). No group differences were evident in Pmax, breakpoint, or elasticity. These findings provide unique evidence that smokers with psychopathology in nicotine-deprived states have greater amplitude of tobacco demand (i.e., value of greater amounts of tobacco) relative to smokers without psychopathology, but not persistence of demand (Bidwell et al., 2012; O’Connor et al., 2016), which compliments prior work in depression and serious mental illness that examine demand under stress-induced and nicotine-sated states (Dahne et al., 2017b; MacKillop and Tidey, 2011). Additionally, contrary to our hypothesis, DD did not significantly differ in smokers with and without psychopathology. Similar non-significant differences have been noted among smokers with and without with self-reported depression (Weidberg et al., 2015a) or schizophrenia (MacKillop and Tidey, 2011), although other studies have reported steeper DD in smokers with self-reported depression versus smokers without (Imhoff et al., 2014; Yoon et al., 2007). Inconsistencies in this literature may be related to method variance (e.g., self-reported versus diagnostic assessment of psychopathology). More research in smokers is warranted to better understand how psychopathology may impact DD, given evidence of steeper (impulsive) DD in various forms of psychopathology (Cáceda et al., 2014; Story et al., 2016). Alternative forms of discounting (e.g., excessive probability discounting) should also be explored to better understand the nature of immediate tobacco preference despite known long-term consequences.
Significant associations between demand indices and DD were only evident in smokers with psychopathology. Specifically, in those with psychopathology, three demand indices (Omax, Pmax, and breakpoint) were positively associated with greater impulsive DD (large rewards). Moreover, in smokers with psychopathology, demand indices (Omax, Pmax, breakpoint, inelasticity) were negatively associated with smoking topography (inter-puff interval and time spent smoking) and DD (small rewards) was also negatively associated with puff count. These effects were significant after adjusting for level of tobacco dependence. In contrast, in smokers without psychopathology, demand intensity and Omax were significantly negatively inter-puff interval and puff count, respectively, although these effects were non-significant after adjusting for level of tobacco dependence. Moreover, DD was not associated with smoking topography. Overall, the patterning in findings suggest that among smokers with psychopathology: (a) higher demand and DD are significantly inter-related; (b) tobacco demand is associated with actual tobacco consumption, and (c) steeper DD (persistent preference for small-sooner reward) is associated with lower tobacco consumption, although finding warrants replication especially considering the non-significant associations between discounting of large delayed rewards.
There are several limitations to address. First, all data were cross-sectional, therefore, it is unknown whether demand and DD causally contribute to smoking topography. Second, we assessed past-year psychopathology, and as a result, the lifetime disorders that naturally remitted or were successfully treated were not captured. Additionally, it is possible certain disorder-specific effects were undetectable based evaluation of psychological disorders as one group. It should be noted that internalizing disorders were more heavily represented than externalizing disorders in the sample, likely a result of the initial telephone screening procedures. Third, the sample size was small and consequently did not permit examination of demand and DD across specific psychological disorders, which may limit the specificity of the current findings based on the heterogeneity of disorders. It is possible that certain disorder-specific effects were undetectable in the current study based on the grouping of all psychological disorders into one group. Fourth, we excluded data from the CPT where participants displayed ≥ 3 reversals (n =11) and data from the MCQ where k consistency was ≤ .778 (n=6), potentially reflecting invalid responding. Reversals may have occurred from misunderstanding directions, limited cognitive functioning, or may be an artifact based on administration of the CPT and MCQ: items were presented one at a time rather than all at once.
Taken together, the reinforcer pathology model (Bickel et al., 2014) may be particularly relevant to the maintenance of smoking in those with psychopathology, especially in the context of nicotine-deprivation. Higher demand and steeper DD are related to poorer substance use treatment outcomes (MacKillop and Kahler, 2009; MacKillop and Murphy, 2007), yet are malleable in treatment. For example, interventions that enhance future time orientation (Sheffer et al., 2016) and present-focused attention/mindfulness (Ashe et al., 2015) or provide contingent reinforcement (Weidberg et al., 2015b) appear to reduce DD. Additionally, brief motivational (Dennhardt et al., 2015) or personalized feedback interventions (Murphy et al., 2015) reduce the rewarding value of substances. Smokers with psychopathology may benefit from pre-cessation intervention that specifically targets (reduce) tobacco demand and DD, whereby increasing ability to manage withdrawal-induced urge and craving to tobacco that onset following a quit attempt. More work is needed to understand aspects of demand and DD, and their interplay in smokers with specific forms of psychopathology, to inform their influence on tobacco consumption, motivational factors for continued use, and cessation behavior.
Highlights.
Smokers with psychopathology versus without had significantly higher tobacco demand
There were no differences in delay discounting by psychopathology status
Tobacco demand and DD were intercorrelated only in smokers with psychopathology
The reinforcer pathology framework may apply to the psychopathology-smoking link
Acknowledgments
Research Funding
This research was supported by a pre-doctoral National Research Service Award from the National Institute of Drug Abuse (F31-DA035564) awarded to the first author. The research described in this paper was also supported in part by a grant to the first author from the American Psychological Association. The first author is currently supported by a training grant from the National Health, Lung, and Blood Institute (T32-HL076134-11). Data analysis and manuscript preparation was supported in part by a grant from the National Institute on Drug Abuse to the second author (K01-DA039311). The funding sources had no other role other than financial support.
Footnotes
Contributors
Drs. Farris and Zvolensky developed the parent study, and Drs. Farris and Aston designed the current secondary investigation. Drs. Farris and Aston managed the literature searches and summaries of previous related work and completed statistical analyses. All authors contributed to and have approved the final manuscript.
Conflict of Interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amlung M, Petker T, Jackson J, Balodis I, MacKillop J. Steep discounting of delayed monetary and food rewards in obesity: A meta-analysis. Psychol Med. 2016;46:2423–34. doi: 10.1017/S0033291716000866. [DOI] [PubMed] [Google Scholar]
- Amlung M, Vedelago L, Acker J, Balodis I, Mackillop J. Steep delay discounting and addictive behavior: A meta-analysis of continuous associations. Addiction. 2017;112:51–62. doi: 10.1111/add.13535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashe ML, Newman MG, Wilson SJ. Delay discounting and the use of mindful attention versus distraction in the treatment of drug addiction: A conceptual review. J Exp Anal Behav. 2015;103:234–248. doi: 10.1002/jeab.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Jarmolowicz DP, Mueller ET, Gatchalian KM. The behavioral economics and neuroeconomics of reinforcer pathologies: Implications for etiology and treatment of addiction. Curr Psychiatry Rep. 2011;13:406–415. doi: 10.1007/s11920-011-0215-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, Murphy JG. The behavioral economics of substance use disorders: Reinforcement pathologies and their repair. Annu Rev Clin Psychol. 2014;10:641–77. doi: 10.1146/annurev-clinpsy-032813-153724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bidwell LC, MacKillop J, Murphy JG, Tidey JW, Colby SM. Latent factor structure of a behavioral economic cigarette demand curve in adolescent smokers. Addict Behav. 2012;37:1257–1263. doi: 10.1016/j.addbeh.2012.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blank MD, Disharoon S, Eissenberg T. Comparison of methods for measurement of smoking behavior: mouthpiece-based computerized devices versus direct observation. Nicotine Tob Res. 2009;11:896–903. doi: 10.1093/ntr/ntp083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Burgess ES, Sales SD, Whiteley JA, Evans DM, Miller IW. Reliability and validity of a smoking timeline follow-back interview. Psychol Addict Behav. 1998;12:101–112. doi: 10.1037/0893-164X.12.2.101. [DOI] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. J Abnorm Psychol. 2002;111:180–5. [PubMed] [Google Scholar]
- Cáceda R, Nemeroff CB, Harvey PD. Toward an understanding of decision making in severe mental illness. J Neuropsychiatry Clin Neurosci. 2014;26:196–213. doi: 10.1176/appi.neuropsych.12110268. doi: http://dx.doi.org/10.1176/appi.neuropsych.12110268. [DOI] [PubMed] [Google Scholar]
- Camerer C. Behavioral economics: Reunifying psychology and economics. Proc Natl Acad Sci. 1999;96:10575–10577. doi: 10.1073/pnas.96.19.10575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Current cigarette smoking among adults - United States, 2005–2015. MMWR Morb Mortal Wkly Rep. 2016;65:1205–1211. doi: 10.15585/mmwr.mm6544a2. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Vital signs: Current cigarette smoking among adults aged ≥18 years with mental illness — United States, 2009–2011. MMWR Morb Mortal Wkly Rep. 2013;62:81–87. [PMC free article] [PubMed] [Google Scholar]
- Dahne J, Murphy JG, MacPherson L. Depressive symptoms and cigarette demand as a function of induced stress. Nicotine Tob Res. 2017a;19:49–58. doi: 10.1093/ntr/ntw145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahne J, Murphy JG, MacPherson L. Depressive symptoms and cigarette demand as a function of induced stress. Nicotine Tob Res. 2017b;19:49–58. doi: 10.1093/ntr/ntw145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennhardt AA, Yurasek AM, Murphy JG. Change in delay discounting and substance reward value following a brief alcohol and drug use intervention. J Exp Anal Behav. 2015;103:125–140. doi: 10.1002/jeab.121. [DOI] [PubMed] [Google Scholar]
- Fagerström KO. Determinants of tobacco use and renaming the FTND to the Fagerström Test for Cigarette Dependence. Nicotine Tob Res. 2012;14:75–78. doi: 10.1093/ntr/ntr137. [DOI] [PubMed] [Google Scholar]
- Farris SG, Aston ER, Zvolensky MJ, Abrantes AM, Metrik J. Psychopathology and tobacco demand. Drug Alcohol Depend. 2017;177:59–66. doi: 10.1016/j.drugalcdep.2017.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farris SG, Zvolensky MJ. An experimental test of the effect of acute anxious arousal and anxiety sensitivity on negative reinforcement smoking. J Psychopharmacol. 2016;30:641–53. doi: 10.1177/0269881116642880. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient edition. Biometrics Research, New York State Psychiatric Insititue; New York, NY: 2007. [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hendricks PS, Ditre JW, Drobes DJ, Brandon TH. The early time course of smoking withdrawal effects. Psychopharmacology (Berl) 2006;187:385–396. doi: 10.1007/s00213-006-0429-9. [DOI] [PubMed] [Google Scholar]
- Hitsman B, MacKillop J, Lingford-Hughes A, Williams TM, Ahmad F, Adams S, Nutt DJ, Munafò MR. Effects of acute tyrosine/phenylalanine depletion on the selective processing of smoking-related cues and the relative value of cigarettes in smokers. Psychopharmacology (Berl) 2008;196:611–21. doi: 10.1007/s00213-007-0995-5. [DOI] [PubMed] [Google Scholar]
- Hursh SR, Galuska CM, Winger G, Woods JH. The economics of drug abuse: A quantitative assessment of drug demand. Mol Interv. 2005;5:20–28. doi: 10.1124/mi.5.1.6. [DOI] [PubMed] [Google Scholar]
- Hursh SR, Silberberg A. Economic demand and essential value. Psychol Rev. 2008;115:186–198. doi: 10.1037/0033-295X.115.1.186. [DOI] [PubMed] [Google Scholar]
- Imhoff S, Harris M, Weiser J, Reynolds B. Delay discounting by depressed and non-depressed adolescent smokers and non-smokers. Drug Alcohol Depend. 2014;135:152–155. doi: 10.1016/j.drugalcdep.2013.11.014. [DOI] [PubMed] [Google Scholar]
- Kirby KN. Instructions for inferring discount rates from choices between immediate and delayed rewards 2000 [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. J Exp Psychol. 1999;128:78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Koffarnus MN, Franck CT, Stein JS, Bickel WK. A modified exponential behavioral economic demand model to better describe consumption data. Exp Clin Psychopharmacol. 2015;23:504–12. doi: 10.1037/pha0000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. J Am Med Assoc. 2000;284:2606–10. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, Munafò MR. Delayed reward discounting and addictive behavior: A meta-analysis. Psychopharmacology (Berl) 2011;216:305–321. doi: 10.1007/s00213-011-2229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Few LR, Murphy JG, Wier LM, Acker J, Murphy C, Stojek M, Carrigan M, Chaloupka F. High-resolution behavioral economic analysis of cigarette demand to inform tax policy. Addiction. 2012;107:2191–200. doi: 10.1111/j.1360-0443.2012.03991.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Kahler CW. Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug Alcohol Depend. 2009;104:197–203. doi: 10.1016/j.drugalcdep.2009.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Murphy JG. A behavioral economic measure of demand for alcohol predicts brief intervention outcomes. Drug Alcohol Depend. 2007;89:227–233. doi: 10.1016/j.drugalcdep.2007.01.002. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Murphy JG, Ray LA, Eisenberg DTA, Lisman SA, Lum JK, Wilson DS. Further validation of a cigarette purchase task for assessing the relative reinforcing efficacy of nicotine in college smokers. Exp Clin Psychopharmacol. 2008;16:57–65. doi: 10.1037/1064-1297.16.1.57. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Tidey JW. Cigarette demand and delayed reward discounting in nicotine-dependent individuals with schizophrenia and controls: An initial study. Psychopharmacology (Berl) 2011;216:91–9. doi: 10.1007/s00213-011-2185-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClave AK, McKnight-Eily LR, Davis SP, Dube SR. Smoking characteristics of adults with selected lifetime mental illnesses: Results From the 2007 National Health Interview Survey. Am J Public Health. 2010;100:2464–2472. doi: 10.2105/AJPH.2009.188136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mennin DS, Holaway RM, Fresco DM, Moore MT, Heimberg RG. Delineating components of emotion and its dysregulation in anxiety and mood psychopathology. Behav Ther. 2007;38:284–302. doi: 10.1016/j.beth.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Yurasek AM, Skidmore JR, Martens MP, MacKillop J, McDevitt-Murphy ME. Behavioral economic predictors of brief alcohol intervention outcomes. J Consult Clin Psychol. 2015;83:1033–43. doi: 10.1037/ccp0000032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, MacKillop J, Tidey JW, Brazil LA, Colby SM. Validity of a demand curve measure of nicotine reinforcement with adolescent smokers. Drug Alcohol Depend. 2011;113:207–14. doi: 10.1016/j.drugalcdep.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor RJ, Heckman BW, Adkison SE, Rees VW, Hatsukami DK, Bickel WK, Cummings KM. Persistence and amplitude of cigarette demand in relation to quit intentions and attempts. Psychopharmacology (Berl) 2016;233:2365–2371. doi: 10.1007/s00213-016-4286-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. J Health Soc Behav. 1981;22:337–56. [PubMed] [Google Scholar]
- Perkins KA, Karelitz JL, Giedgowd GE, Conklin CA. The reliability of puff topography and subjective responses during ad lib smoking of a single cigarette. Nicotine Tob Res. 2012;14:490–4. doi: 10.1093/ntr/ntr150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomerleau CS, Carton SM, Lutzke ML, Flessland KA, Pomerleau OF. Reliability of the Fagerstrom Tolerance Questionnaire and the Fagerstrom Test for Nicotine Dependence. Addict Behav. 1994;19:33–9. doi: 10.1016/0306-4603(94)90049-3. [DOI] [PubMed] [Google Scholar]
- Sheffer CE, Mackillop J, Fernandez A, Christensen D, Bickel WK, Johnson MW, Panissidi L, Pittman J, Franck CT, Williams J, Mathew M. Initial examination of priming tasks to decrease delay discounting. Behav Processes. 2016;128:144–152. doi: 10.1016/j.beproc.2016.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein JS, Koffarnus MN, Snider SE, Quisenberry AJ, Bickel WK. Identification and management of nonsystematic purchase task data: Towards best practice. Exp Clin Psychopharmacol. 2015;23:337–386. doi: 10.14574/ojrnhc.v14i1.276.Using. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Story GW, Moutoussis M, Dolan RJ. A computational analysis of aberrant delay discounting in psychiatric disorders. Front Psychol. 2016;6 doi: 10.3389/fpsyg.2015.01948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4. Allyn and Bacon; Boston, MA: 2000. [Google Scholar]
- Tice DM, Bratslavsky E, Baumeister RF. Emotional distress regulation takes precedence over impulse control: If you feel bad, do it! J Pers Soc Psychol. 2001;80:53–67. [PubMed] [Google Scholar]
- United States Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress A Report of the Surgeon General. A Rep Surg Gen 2014 [Google Scholar]
- Weidberg S, Garcia-Rodriguez O, Yoon JH, Secades-Villa R. Interaction of depressive symptoms and smoking abstinence on delay discounting rates. Psychol Addict Behav. 2015a;29:1041–1047. doi: 10.1037/adb0000073. [DOI] [PubMed] [Google Scholar]
- Weidberg S, Landes RD, García-Rodríguez O, Yoon JH, Secades-Villa R. Interaction effect of contingency management and sex on delay-discounting changes among treatment-seeking smokers. Exp Clin Psychopharmacol. 2015b;23:361–368. doi: 10.1037/pha0000043. [DOI] [PubMed] [Google Scholar]
- Wing VC, Moss TG, Rabin RA, George TP. Effects of cigarette smoking status on delay discounting in schizophrenia and healthy controls. Addict Behav. 2012;37:67–72. doi: 10.1016/j.addbeh.2011.08.012. [DOI] [PubMed] [Google Scholar]
- Yoon JH, Higgins ST, Heil SH, Sugarbaker RJ, Thomas CS, Badger GJ. Delay discounting predicts postpartum relapse to cigarette smoking among pregnant women. Exp Clin Psychopharmacol. 2007;15:176–86. doi: 10.1037/1064-1297.15.2.186. [DOI] [PubMed] [Google Scholar]