Abstract
Background
Family history of addiction is a risk factor for substance use disorders. Delay discounting (DD) is associated with the risk of substance use and dependence, and is predictive of the likelihood of successful abstinence and treatment outcomes; thus, we investigated the extent to which having parents with addiction (parental history of addiction) and number of addicted parents affect DD among individuals in recovery from addiction.
Methods
Data from 177 individuals in recovery from addiction from The International Quit and Recovery Registry (IQRR), an ongoing online data collection program that aims to understand addiction and how people succeed in recovery, were included in the analysis. Participants with no, one, or two parents with addiction were compared on measures of DD using an adjusting-amount task.
Results
Parental history of addiction was significantly associated with delay discounting. After controlling for age and gender, which were significantly different between groups, participants reporting two biological parents with addiction had significantly higher DD rates compared to those reporting one or no parents with addiction.
Conclusions
Participants with two parents with addiction had significantly higher rates of discounting compared to those with no or only one parent with addiction. This information can serve as a foundation to better identify and target important subgroups that need additional or non-traditional intervention strategies to address their larger degree of impulsivity and help maintain abstinence or achieve better treatment outcomes.
Keywords: Addiction, Delay Discounting, Parental History, Recovery from Addiction
1.0 Introduction
Substance dependence is a major public health concern (National Institute on Drug Abuse 2005; Nutt et al., 2006) involving harmful effects for the dependent individuals, their families, communities, and society as a whole (National Institute on Drug Abuse 2011; Nutt et al., 2007). Substance use disorders are among the most common psychiatric disorders starting in young adulthood (National Research Council and Institute of Medicine 2010) that co-occur with other mental and physical health problems, and show a strong familial pattern (Kessler et al., 2005; Sher et al., 2005). Because drug addiction is, in part, a choice between short-term reinforcement from substance use and long-term reinforcement from abstinence, the processes underlying decision-making are important to the success of treatment programs. Behavioral economics, combining psychological and economic principles, has been extensively used to understand the decision-making process in individuals with addiction (Bickel et al., 2014a; Heather and Vuchinich 2003). Delay discounting, one of the most widely studied behavioral economic measures, refers to the subjective change in the value of a reward based on the delay to its receipt (Madden and Bickel 2010).
Individuals with addiction have significantly higher rates of delay discounting compared to healthy controls (Amlung et al., 2016; Bickel et al., 2014b; MacKillop et al., 2011). This finding is robust in most drugs of abuse, including opiates (Madden et al., 1999), alcohol (Mitchell et al., 2005), cocaine (Coffey et al., 2003), and nicotine (Baker et al., 2003). In addition, delay discounting rates are positively associated with the risk of substance use with greater discounting rates reported among individuals exhibiting greater drug consumption and dependence (Fernie et al., 2013; Khurana et al., 2013; MacKillop et al., 2011), and negatively associated with the likelihood of successful abstinence from addiction (Krishnan-Sarin et al., 2007; MacKillop and Kahler 2009; C. Sheffer et al., 2012, 2014; Washio et al., 2011; Yoon et al., 2007).
Several previous studies compared discounting rates in current, ex-, and never substance-dependent individuals. Bickel et al. (1999) compared rates of discounting among current, never, and ex-smokers (reported abstinence from cigarettes for at least one year, and had smoked at least 20 cigarettes daily for at least 5 years prior to quitting) and indicated higher rates of discounting among current smokers but no significant difference between never and ex-smokers (Bickel et al., 1999). Former heroin and amphetamine users (reported that they had previously been a long-term misusers of either amphetamine or heroin) discounted delayed money less than current drug users but more than non-users (Bretteville-Jensen 1999). No significant difference in discounting was found between currently abstinent (reported no cocaine use in the past 30 days) and currently using cocaine-dependent outpatients (Heil et al., 2006). Moreover, rates of discounting by ex-alcohol dependent individuals (reported a lifetime history of alcohol dependence but were not drunk to intoxication for more than 30 days) and ex-smokers (reported abstinence from cigarettes for at least one year, and had smoked at least 20 cigarettes daily for at least 5 years prior to quitting) are intermediate to that of current users and never-users in alcohol dependence (Petry 2001) and cigarette smoking, (Odum et al., 2002) respectively. Interestingly, in individuals with substance dependence, high delay discounting rates may persist even after years of abstinence (Mitchell et al., 2005), suggesting a possible irreversible effect of substance abuse and/or a pre-existing genetic risk (MacKillop 2013; Meyer-Lindenberg et al., 2006; Bickel 2015).
Addiction is heritable such that relatives of addicted individuals are eight times more susceptible to developing an addiction compared to the general population (Merikangas et al., 1998). Recent data indicates that delay discounting is also highly heritable (Anokhin et al., 2011, 2015; Mitchell 2011; Wilhelm and Mitchell 2009). A substantially higher correlation between immediate or delayed choices was found within monozygotic twin pairs compared to dizygotic twin pairs, suggesting the presence of a genetic contribution (Anokhin et al., 2011). In addition, rates of discounting among mothers with nicotine dependence and their children were significantly higher than mothers without nicotine dependence and their children (Reynolds et al., 2009). Few studies, however, have examined the association between delay discounting and family history of addiction. Those that have reported mixed results, with some reporting a positive association (Dougherty et al., 2014; Smith et al., 2015; VanderBroek et al., 2016), some reporting a positive association among women but not men (Petry et al., 2002) and some indicating no association (Herting et al., 2010; Sanchez-Roige et al., 2016). Importantly, these studies compared groups of participants with and without a family or parental history of addiction but did not investigate or report the effect of number of parents with addiction in the family on rates of discounting. Hence, the extent to which delay discounting is affected by the number of parents with a history of addiction remains unknown.
The purpose of the present study is to compare delay discounting rates from individuals who are registered in the International Quit and Recovery Registry (IQRR), an ongoing online registry seeking to understand the phenotype of recovery, as a function of the number of parental figures who suffer from addiction. We hypothesize that higher rates of discounting will be a graded function of the number of parents with addiction. Given the predictive relation between discounting and successful attempts at drug abstinence reviewed above (Krishnan-Sarin et al., 2007; MacKillop and Kahler 2009; Sheffer et al., 2012, 2014; Washio et al., 2011; Yoon et al., 2007), understanding the effect of parental history and number of parents with addiction on delay discounting rates might better identify those individuals in recovery who may be at greater risk of relapse.
2.0 Methodology
2.1 Participants
Participants were recruited from the IQRR, an online community and registry that was launched in September 2011 and is available internationally through the IQRR website (https://quitandrecovery.org) to adults who are in self-reported recovery from one or more substance or behavioral addictions. The goals of the IQRR include understanding what allows people to succeed in overcoming addiction, tapping the insights of experiences of people who are in recovery, and understanding associations between addiction and decision-making processes. The IQRR also aims to better understand the phenotype of recovery through administration of monthly research assessments. Interested individuals who are in recovery may become IQRR members, called “Recovery Heroes,” by completing a registration process that includes providing general contact information and completing a detailed initial questionnaire concerning socioeconomic demographics, and personal and family history of behavioral addictions and/or substance use. Once registered, IQRR members are encouraged to create a website profile, which allows them to complete any available monthly research assessments.
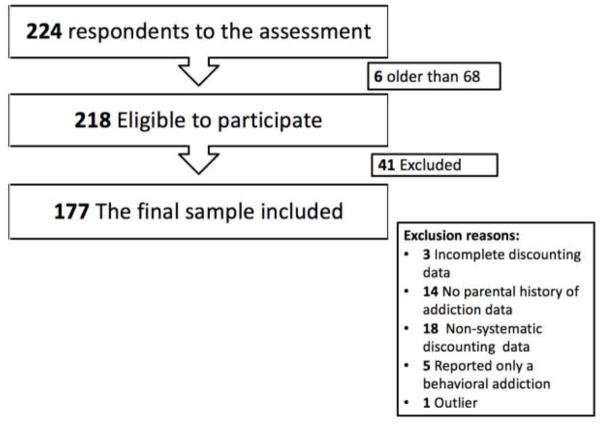
For each monthly research assessment released, participants earn a badge available on their profile and 100 points which is exchangeable for $1.00. The present study concerns data from 224 participants who completed one of the IQRR assessments. Inclusion criteria for the present study required that participants be between the ages of 18 and 68 years (Green et al., 1994, 1999) and self-report recovery from one or more substances. Individuals were excluded (n=41) if they: 1) did not complete the delay discounting task (n=3), 2) did not complete the parental history of addiction questions (n=14), 3) provided nonsystematic delay discounting data (n=18; Johnson and Bickel 2008), and 4) reported a non-substance related primary addiction (e.g., gambling, shopping, viewing pornography, or other; n=5)). These and other inclusion and exclusion criteria were determined by specific responses to the parental history questions and delay discounting items as described in detail below. Figure 1 diagrams that of the 218 participants who were eligible and completed the assessment, 41 were excluded for the present study; thus, the final sample consisted of 177 participants. This study was conducted in compliance with the Institutional Review Board of Virginia Polytechnic Institute and State University.
Fig. 1.
Study sample of substance dependents in recovery respondents to the IQRR assessment.
2.2 Study Measures
To determine the primary addiction of each participant, we used the standard IQRR question, “What was your primary addiction?” with the following choices: a) tranquilizers/depressants; b) prescription pain relievers; c) nicotine; d) cannabis products; e) cocaine; f) stimulants; g) opioids; h) alcohol; i) overeating; j) gambling; k) viewing pornography; l) shopping; or m) other. Examples were provided for each addiction.
To identify parental history of addiction, we used the standard IQRR question from the initial IQRR registrant questionnaire, in which respondents were asked “Do either of your biological parents have any addiction?” with five choices to choose from: “Father, Mother, Neither, both, prefer not to answer”.
Delay discounting was measured using an adjusting-amount task (Du et al., 2002), which presents participants with multiple choices (here, hypothetical monetary rewards) between a relatively larger-delayed reward and a relatively smaller, immediate reward, the magnitude of which is adjusted until the two choices are deemed approximately equal (e.g., an indifference point is reached). Participants in this study were presented with repeated hypothetical choices between $1000 delivered after five discrete delays (1 day, 1 week, 1 month, 6 months, 1 year) or a $500 reward delivered now. Depending on the choice, the amount of the smaller reward was either increased or decreased until reaching an indifference point. Plotting the indifference points at each delay yielded a delay discounting curve that is modeled using this commonly employed hyperbolic discounting function,
| Equation 1 |
where V refers to the value of the delayed reward, A represents the amount of the delayed reward, D is the delay, and k is the estimated index of discounting (Mazur 1987). Larger k values represent higher discounting (i.e., more impulsivity). To reduce the positive skew of the data, which is typical among DD data, estimates of k were transformed using the natural logarithm, ln(k) to perform statistical analyses on rates of delay discounting.
2.3 Statistical Analysis
SPSS was used to perform all the statistical analysis (P = 0.05). One participant had a discounting rate that was identified as an outlier using the “'outlier labeling rule” (Hoaglin and Iglewicz 1987), which is based on multiplying the interquartile range (IQR) by a factor of 2.2; hence, this value was removed from all further analysis in this study. Descriptive statistics and chi-square analyses were used to determine the frequencies and associations of sample characteristics with the delay discounting rates and parental history of addiction. As no significant difference in any of the demographics or outcome measures were found between those who answered “Father” or “Mother” to the parental history of addiction question (data not shown), the four groups (both, father, mother, neither) were reclassified into three groups (i.e., both parents, one parent, neither) to ease the analysis and interpretation of the results.
For demographic characteristics (e.g., gender, income, education, marital status, and age), a one-way ANOVA and pearson chi-square analyses were conducted to compare means and frequencies among the parental history of addiction groups. An analysis of covariance was then conducted to compare mean delay discounting rates among the parental history groups, with those demographic factors that differed significantly between groups modeled as covariates (here, participant gender and age). When appropriate, post hoc comparisons were conducted using the Sidak pairwise correction.
3.0 Results
Figure 1 diagrams that of the 224 participants who completed the assessment, 47 were excluded; thus, 177 participants were included in the final analysis. In this final sample, 59 participants (33.3%) did not report a parental history of addiction, 88 (49.7%) reported one addicted parent (62 father, 26 mother), and 30 (16.9%) reported two addicted parents. The mean age (SD) of participants was 47.29 (11.84) for the three groups together (no parental history 49.5 (11.13); one-parent 47.5 (12.13); two parents 41.9 (11.00)). The ANOVAs and pearson chi-square analyses of the continuous and categorical demographic variables, respectively, indicated a significant difference in age [F(2,176) = 4.282, p=0.015] and gender [X2 (2, N=177) = 6.205, p=0.045] among the three parental history groups. Hence, we controlled for these two variables in our final ANCOVA analysis. No other significant differences were found in the sociodemographic variables. Table 1 provides the distributions of the sample characteristics.
Table 1.
Sample characteristics by parental history of addiction (N=177).
| Characteristics | Frequency (%) | |||
|---|---|---|---|---|
|
| ||||
| Neither n=59 | One parent n=88 | Both parents n=30 | P value | |
|
|
||||
| Gender | 0.045* | |||
| Male | 25 (42.4) | 27 (30.7) | 5 (16.7) | |
| Female | 34 (57.6) | 61 (69.3) | 25 (83.3) | |
| Employment | 0.123 | |||
| Employed full-time | 30 (50.8) | 41 (46.6) | 7 (23.3) | |
| Employed part-time | 6 (10.2) | 7 (8.0) | 4 (13.3) | |
| Not currently employed | 5 (8.5) | 11 (12.5) | 8 (26.7) | |
| Retired | 5 (8.5) | 8 (9.1) | 1 (3.3) | |
| Self-employed | 6 (10.2) | 7 (8.0) | 3 (10.0) | |
| Student | 2 (3.4) | 2 (2.3) | 4 (13.3) | |
| Other | 5 (8.5) | 12 (13.6) | 3 (10.0) | |
| Marital Status | 0.219 | |||
| Married | 22 (37.3) | 33 (37.5) | 7 (23.3) | |
| Never married | 10 (10.0) | 17 (19.3) | 9 (30.0) | |
| Divorced | 19 (32.2) | 23 (26.1) | 6 (20.0) | |
| Separated | 1 (1.7) | 5 (5.7) | 1 (3.3) | |
| Unmarried couple living together | 4 (6.8) | 10 (11.4) | 6 (20.0) | |
| Widowed | 3 (5.1) | 0 (0.0) | 1 (3.3) | |
| Education level | 0.380 | |||
| Some high school | 0 (0.0) | 2 (2.3) | 0 (0.0) | |
| High school diploma or equivalency | 5 (8.5) | 9 (10.2) | 5 (16.7) | |
| Some college | 21 (35.6) | 27 (30.7) | 12 (40.0) | |
| Associate degree | 5 (8.5) | 8 (9.1) | 5 (16.7) | |
| Bachelor degree | 20 (33.9) | 30 (34.1) | 4 (13.3) | |
| Master’s degree | 5 (8.5) | 11 (12.5) | 4 (13.3) | |
| Doctoral degree | 3 (5.1) | 1 (1.1) | 0 (0.0) | |
| Primary Addiction | 0.666 | |||
| Alcohol | 32 (54.2) | 53 (60.2) | 14 (46.6) | |
| Cannabis products | 3 (5.1) | 2 (2.2) | 3 (10.0) | |
| Nicotine | 2 (3.4) | 3 (3.4) | 0 (0.0) | |
| Prescription pain relievers | 10 (17.0) | 15 (17.0) | 8 (26.7) | |
| Stimulants | 9 (15.3) | 14 (15.9) | 5 (16.7) | |
| Tranquilizers/Depressants | 3 (5.0) | 1 (1.1) | 0 (0.0) | |
| Income | 0.510 | |||
| Less than $30,000 | 18 (30.5) | 25 (28.4) | 15 (50.0) | |
| $30,000 – $49,999 | 10 (16.9) | 19 (21.6) | 5 (16.7) | |
| $50,000 – $69,999 | 9 (15.3) | 15 (17.0) | 2 (6.7) | |
| $70,000 – $89,999 | 5 (8.5) | 4 (4.5) | 0 (0.0) | |
| $90,000 – $149,999 | 7 (11.9) | 15 (17.0) | 3 (10.0) | |
| $150,000 and above | 4 (6.8) | 3 (3.4) | 1 (3.3) | |
| Prefer not to answer | 6 (10.2) | 7 (8.0) | 4 (13.3) | |
| Smoking Status | 0.719 | |||
| No | 40 (67.8) | 65 (73.9) | 21 (70.0) | |
| Yes | 19 (32.2) | 23 (26.1) | 9 (30.0) | |
| Delay Discounting | ||||
| Ln(k) (Mean (SD)) | −6.41 (2.01) | −6.25 (2.04) | −5.02 (1.47) | 0.004 |
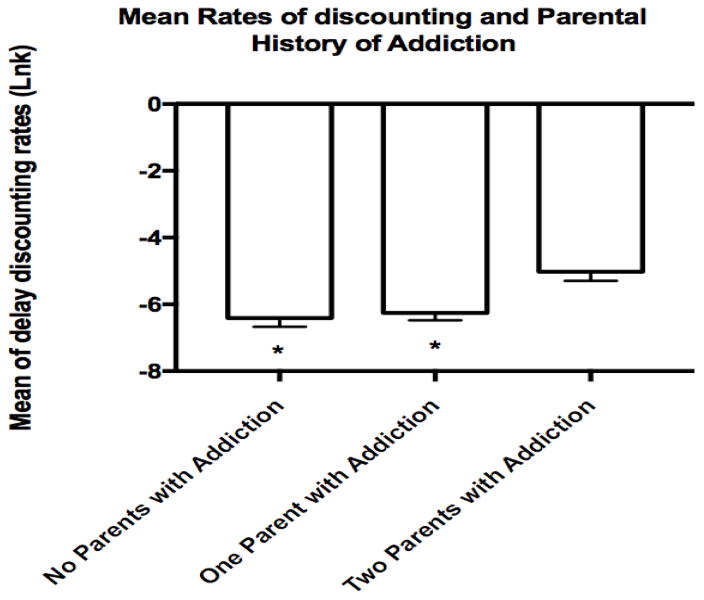
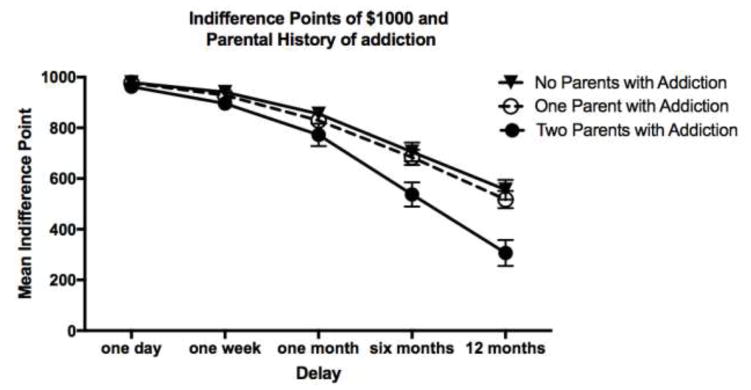
The mean (M) rates of delay discounting (lnk) for participants with two addicted parents (M = -5.02, SD = 1.47) was significantly higher (p=0.014) than the neither parents with addiction (M = −6.41, SD = 2.01) and the one parent with addiction (M = −6.25, SD = 2.04) groups (see Figure 2). The indifference point at each delay is presented in Figure 3.
Fig. 2.
The mean (M) delay discounting rates (lnk) for participants with two parents with addiction compared to those with one parent or no parents with addiction groups. *p<0.05 Compared to “Both parents” group
Error bars represent standard error.
Fig. 3.
The mean delay discounting indifference points of $1000 calculated for each of the five points of time used in the adjusted amount discounting (1 day, 1 week, 1 month, 6 months, 1 year).
Error bars represent standard error.
Analysis of variance (ANOVA) showed a main effect of parental history on rates of delay discounting (F(2,176) = 5.593, p = 0.004. Due to differences in age and gender between groups, an ANCOVA with a between-subjects factor of parental history of addiction (i.e., both parents, one parent, neither parent) and covariates of age and gender was conducted and revealed a main effect of parental history on delay discounting rates [F(2, 171) = 3.820 p= 0.024], and age, [F(1, 171) = 6.780, p= 0.010], but not gender [F(1, 171) = 0.020, p= 0.886]. Pairwise comparisons using the Sidak test indicated that participants who had two parents with addiction had significantly higher discounting rates compared to those who had one parent with addiction (p=0.036) or neither parent with addiction (p=0.032) groups after controlling for age and gender.
4.0 Discussion
To our knowledge, this study is the first to investigate the differences in delay discounting rates as a function of number of addicted parents (i.e., neither, one parent, two parents) among individuals in recovery from addiction. We report greater delay discounting in those with two addicted parents, compared to one or none. Other demographic variables such as smoking status, income, marital status, and education did not significantly contribute to differences in rates of discounting; and above all, when the influence of gender and age were controlled, the parental history of addiction continued to predict discounting rates. In contrast with our hypothesis no significant difference in discounting rates were observed between those who have one addicted parent compared to those who have no addicted parents. Below, we discuss two main points related to these findings.
First, as rates of delay discounting are higher across individuals with many developmental and psychiatric disorders (Barkley et al., 2001; Rounds et al., 2007; Scheres et al., 2010; Wilson et al., 2010; Yoon et al., 2007), our findings of significant effect of parental addiction on rates of discounting among individuals in recovery from addiction are consistent with previous studies examining the effect of family/parental addiction on the risk of many negative outcomes among offspring, including emotional, social, and behavioral problems (Lander et al., 2013) in addition to abnormal cognitive functioning such as shorter attention span, hyperactivity (Steinhausen et al., 1984), higher impulsiveness, aggressiveness (Stanger et al., 1999), and Attention Deficit Hyperactivity Disorder (ADHD) (Sundquist et al., 2014) with findings indicating higher risk among individuals with family/parental history compared to controls (Wilens 1994).
Second, our results are consistent with findings from studies examining the effect of number of parents with addiction and the negative outcomes on offspring which indicated stronger association among those who have two addicted parents compared to one or none (Earls et al., 1988; Yoon et al., 2013). For example, greater risk for social competence deficits in children from families with two alcohol-dependent parents when compared to children from families with one alcohol-dependent parent has been reported (Hussong et al., 2005). Moreover, children with two alcohol-dependent parents exhibited greater risk for internalizing (i.e., negative behaviors that are targeted toward the self, such as anxiety and depression) and externalizing (i.e., negative behaviors that are targeted toward others such as delinquency and aggression) symptoms (Hussong et al., 2007, 2008) compared to children with one alcoholic parent. However, consistent with our findings, parent-reported internalizing and externalizing symptoms for children with one alcohol-dependent parent did not significantly differ from controls (Hussong et al., 2007, 2008), suggesting that having only one addicted parent may minimize risk of social and emotional problems for children with parental history of addiction.
This study supports and furthers the role of delay discounting as a behavioral marker of addiction (Bickel et al., 2014b) by supporting an association between discounting rates and parental history of addiction. This association may be due to biological and genetic processes that underlie addiction, parental behavioral changes caused by the addiction, and/or gene-environment interactions between these processes. Identification of the specific mechanism(s) underlying our findings awaits further investigation. Nonetheless, our findings are corroborated by prior work on cigarette smoking. Specifically, in a study examining delay discounting among mothers with and without nicotine dependence and their children (Reynolds et al., 2009) smoking mothers and their children had significantly higher rates of discounting compared to non-smoking mothers and their children, suggesting that delay discounting may function as a behavioral risk factor for adolescent cigarette smoking that precedes any significant nicotine use. However, in order to reach firm well-founded conclusions future work assessing the relationship between family history and discounting that aim to understand and explain reasons of inconsistency in findings from the current study and some previous ones of significant association (Dougherty et al., 2014; Smith et al., 2015; VanderBroek et al., 2016) compared to other findings of no association ( Herting et al., 2010; Sanchez-Roige et al., 2016) is needed. In addition, investigating other risk factors that might alter rates of discounting as a function of abstinence such as cessation duration, severity of addiction, and the presence of any ongoing secondary addictions and how they can affect the relationship between rates of discounting, having a family history of addiction and recovery might be beneficial.
This study has both strengths and weaknesses. Using the IQRR that represents different groups of individuals in recovery from substance dependence provides a valuable image of the association between parental history of addiction and delay discounting rates in this specific population. However, one of the limitations of this study was using the online-based assessment, which limited our sample to include only those individuals in recovery who use technology and an email address. Future studies that include individuals with substance dependence in recovery who do not have or use technology might be necessary to identify the specific effect of parental history on delay discounting rates, since differences in demographics, if they exist, might be quite important. In addition, this study did not address all parental, personal, or environmental factors that may affect the relationship between parental history of addiction, rates of discounting, and developing negative outcomes. For example, the study did not collect data about the co-occurring parental psychopathology (Solis et al., 2012), the parents’ status of recovery (Hussong et al., 2012; Solis et al., 2012), the severity of addiction, any ongoing use for other problematic substances, cessation duration, stress levels, type of parental addiction, and whether participants were raised by their addicted parents or not. As those factors may alter rates of discounting and its association with family history, future research that includes assessing these factors might be necessary to better understand the relation between parental history of addiction and delay discounting rates. Finally, the IQRR is a self-reported survey, which might be subject to some potential sources of bias such as social desirability bias and recall bias. However, self-reporting about parental history of substance use has been validated in prior studies (Andreasen 1986; Ellingson et al., 2010; Sher and Descutner 1986).
5.0 Conclusion
Delay discounting rates are significantly associated with parental history of addiction, specifically the number of addicted parents in individuals in recovery from addiction. Participants who had two addicted parents displayed significantly higher rates of discounting compared to those who had no or only one parent with addiction. This information can serve as a foundation to better identify and target important subgroups that need additional or non-traditional intervention strategies to address their larger degree of impulsivity and help achieve better treatment outcomes.
Highlights.
Delay discounting is significantly associated with parental history of addiction.
Participants with two parents with addiction have the highest discounting rates.
No difference in discounting among those with one or no parents with addiction.
Gender of parent with addiction is not associated with discounting in offspring.
Acknowledgments
Role of Funding Source
Nothing declared.
This work was supported by the Virginia Tech Carilion Research Institute and NIH/NIDA [grant number R01DA039456, 2014]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency. The funding agency played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit this article for publication.
Footnotes
Contributors
Athamneh analyzed and interpreted the data, and wrote the manuscript; Stein provided expertise in the analysis and interpretation of findings and edited the manuscript; Quisenberry contributed to the data collection and edited the manuscript; Pope contributed to the interpretation of findings and edited the manuscript; Bickel conceptualized the study, provided expertise in the analysis and interpretation of findings and edited the manuscript. All authors have read and approved of the final version of the manuscript before submission to the journal.
Conflict of Interest
Dr. Bickel is a principal in HealthSim, LLC
None of the other authors have any conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amlung M, Vedelago L, Acker J, Balodis I, Mackillop J. Steep delay discounting and addictive behavior: A meta-analysis of continuous associations. Addiction. 2016;112:51–62. doi: 10.1111/add.13535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreasen N. The family history approach to diagnosis. Arch Gen Psychiatry. 1986;43:421. doi: 10.1001/archpsyc.1986.01800050019002. [DOI] [PubMed] [Google Scholar]
- Anokhin AP, Golosheykin S, Grant JD, Heath AC. Heritability of delay discounting in adolescence: A longitudinal twin study. Behav Genet. 2011;41:175–83. doi: 10.1007/s10519-010-9384-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anokhin AP, Grant JD, Mulligan RC, Heath AC. The genetics of impulsivity: Evidence for the heritability of delay discounting. Biol Psychiatry. 2015;77:887–94. doi: 10.1016/j.biopsych.2014.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker F, Johnson MW, Bickel WK. Delay discounting in current and never-before cigarette smokers: Similarities and differences across commodity, sign, and magnitude. J Abnorm Psychol. 2003;112:382–92. doi: 10.1037/0021-843x.112.3.382. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Edwards G, Laneri M, Fletcher K, Metevia L. Executive functioning, temporal discounting, and sense of time in adolescents with attention deficit hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD) J Abnorm Child Psychol. 2001;29:541–56. doi: 10.1023/a:1012233310098. [DOI] [PubMed] [Google Scholar]
- Bickel WK. Discounting of delayed rewards as an endophenotype. Biol Psychiatry. 2015;77:846–47. doi: 10.1016/j.biopsych.2015.03.003. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, Murphy JG. The behavioral economics of substance use disorders: reinforcement pathologies and their repair. Ann Rev Clin Psychol. 2014a;10:641–77. doi: 10.1146/annurev-clinpsy-032813-153724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Koffarnus MN, Moody L, Wilson AG. The behavioral- and neuro-economic process of temporal discounting: A candidate behavioral marker of addiction. Neuropharmacology. 2014b;76:518–27. doi: 10.1016/j.neuropharm.2013.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Odum AL, Madden GJ. Impulsivity and cigarette smoking: Delay discounting in current, never, and ex-smokers. Psychopharmacology. 1999;146:447–54. doi: 10.1007/pl00005490. [DOI] [PubMed] [Google Scholar]
- Bretteville-Jensen AL. Addiction and discounting. J Health Econ. 1999;18:393–407. doi: 10.1016/s0167-6296(98)00057-5. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Gudleski GD, Saladin ME, Brady KT. Impulsivity and rapid discounting of delayed hypothetical rewards in cocaine-dependent individuals. Exp Clin Psychopharmacol. 2003;11:18–25. doi: 10.1037//1064-1297.11.1.18. [DOI] [PubMed] [Google Scholar]
- Dougherty DM, Charles NE, Mathias CW, Ryan SR, Olvera RL, Liang Y, Acheson A. Delay discounting differentiates pre-adolescents at high and low risk for substance use disorders based on family history. Drug Alcohol Depend. 2014;143:105–11. doi: 10.1016/j.drugalcdep.2014.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du W, Green L, Myerson J. Cross-cultural comparisons of discounting delayed and probabilistic rewards. Psychol Rec. 2002;52:479. [Google Scholar]
- Earls F, Reich W, Jung KG, Cloninger CR. Psychopathology in children of alcoholic and antisocial parents. Alcohol Clin Exp Res. 1988;12:481–87. doi: 10.1111/j.1530-0277.1988.tb00230.x. [DOI] [PubMed] [Google Scholar]
- Ellingson JM, Slutske WS, Martin NG. The reliability and validity of the family history method for assessing pathological gambling and gambling involvement. Psychol Addict Behav. 2010;24:292–99. doi: 10.1037/a0018126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernie G, Peeters M, Gullo MJ, Christiansen P, Cole JC, Sumnall H, Field M. Multiple behavioural impulsivity tasks predict prospective alcohol involvement in adolescents. Addiction. 2013;108:1916–23. doi: 10.1111/add.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green L, Fry AF, Myerson J. Discounting of delayed rewards: A life-span comparison. Psychol Sci. 1994;5:33–36. [Google Scholar]
- Green L, Myerson J, Ostaszewski P. Discounting of delayed rewards across the life span: Age differences in individual discounting functions. Behav Process. 1999;46:89–96. doi: 10.1016/S0376-6357(99)00021-2. [DOI] [PubMed] [Google Scholar]
- Heather N, Vuchinich RE. Choice, Behavioural Economics and Addiction. Elsevier; 2003. [Google Scholar]
- Heil SH, Johnson MW, Higgins ST, Bickel WK. Delay discounting in currently using and currently abstinent cocaine-dependent outpatients and non-drug-using matched controls. Addict Behav. 2006;31:1290–94. doi: 10.1016/j.addbeh.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Herting MM, Schwartz D, Mitchell SH, Nagel BJ. Delay discounting behavior and white matter microstructure abnormalities in youth with a family history of alcoholism. Alcohol Clin Exp Res. 2010;34:1590–1602. doi: 10.1111/j.1530-0277.2010.01244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoaglin DC, Iglewicz B. Fine-tuning some resistant rules for outlier labeling. J Am Stat Assoc. 1987;82:1147. [Google Scholar]
- Hussong AM, Wirth RJ, Edwards MC, Curran PJ, Chassin LA, Zucker RA. Externalizing symptoms among children of alcoholic parents: Entry points for an antisocial pathway to alcoholism. J Abnorm Psychol. 2007;116:529–42. doi: 10.1037/0021-843X.116.3.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Flora DB, Curran PJ, Chassin LA, Zucker RA. Defining risk heterogeneity for internalizing symptoms among children of alcoholic parents. Dev Psychopathol. 2008;20:165–93. doi: 10.1017/S0954579408000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Huang W, Serrano D, Curran PJ, Chassin LA. Testing whether and when parent alcoholism uniquely affects various forms of adolescent substance use. J Abnorm Child Psychol. 2012;40:1265–76. doi: 10.1007/s10802-012-9662-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Zucker RA, Wong MM, Fitzgerald HE, Puttler LI. Social competence in children of alcoholic parents over time. Dev Psychol. 2005;41:747–59. doi: 10.1037/0012-1649.41.5.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. An algorithm for identifying nonsystematic delay-discounting data. Exp Clin Psychopharmacol. 2008;16:264–74. doi: 10.1037/1064-1297.16.3.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month dsm-iv disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khurana A, Romer D, Betancourt LM, Brodsky NL, Giannetta JM, Hurt H. Working memory ability predicts trajectories of early alcohol use in adolescents: The mediational role of impulsivity. Addiction. 2013;108:506–15. doi: 10.1111/add.12001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Brady R, Duhig AM, Smith A, Liss T, McFetridge A, Cavallo DA, Carroll KM, Potenza MN. Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug Alcohol Depend. 2007;88:79–82. doi: 10.1016/j.drugalcdep.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lander L, Howsare J, Byrne M. The impact of substance use disorders on families and children: From theory to practice. Soc Work Public Health. 2013;28:194–205. doi: 10.1080/19371918.2013.759005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J. Integrating behavioral economics and behavioral genetics: Delayed reward discounting as an endophenotype for addictive disorders. J Exp Anal Behav. 2013;99:14–31. doi: 10.1002/jeab.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, Munafò MR. Delayed reward discounting and addictive behavior: A meta-analysis. Psychopharmacology. 2011;216:305–21. doi: 10.1007/s00213-011-2229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Kahler CW. Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug Alcohol Depend. 2009;104:197–203. doi: 10.1016/j.drugalcdep.2009.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden GJ, Bickel WK, Jacobs EA. Discounting of delayed rewards in opioid-dependent outpatients: Exponential or hyperbolic discounting functions? Exp Clin Psychopharmacol. 1999;7:284–93. doi: 10.1037//1064-1297.7.3.284. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Bickel WK. Impulsivity: The Behavioral and Neurological Science of Discounting. Amer Psychological Assn 2010 [Google Scholar]
- Mazur JE. An Adjusting Procedure for Studying Delayed Reinforcement. Commons. 1987:55–73. [Google Scholar]
- Merikangas KR, Marilyn S, Stevens DE, Joseph G, Preisig MA, Brenda F, Heping Z, O’Malley SS, Rounsaville BJ. Familial transmission of substance use disorders. Arch Gen Psychiatry. 1998;55:973. doi: 10.1001/archpsyc.55.11.973. [DOI] [PubMed] [Google Scholar]
- Meyer-Lindenberg A, Weinberger DR. Intermediate phenotypes and genetic mechanisms of psychiatric disorders. Nature Rev Neurosci. 2006;7:818–27. doi: 10.1038/nrn1993. [DOI] [PubMed] [Google Scholar]
- Mitchell JM, Fields HL, D’Esposito M, Boettiger CA. Impulsive responding in alcoholics. Alcohol Clin Exp Res. 2005;29:2158–69. doi: 10.1097/01.alc.0000191755.63639.4a. [DOI] [PubMed] [Google Scholar]
- Mitchell SH. The genetic basis of delay discounting and its genetic relationship to alcohol dependence. Behav Process. 2011;87:10–17. doi: 10.1016/j.beproc.2011.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse (NIDA), and National Institutes of Health. Understanding Drug Abuse and Addiction. [accessed 09.02.2017];NIDA InfoFacts. 2011 https://www.drugabuse.gov/publications/drugfacts/understanding-drug-use-addiction.
- National Institute on Drug Abuse (NIDA) [accessed 09.02.2017];Drug Abuse and Addiction: One of America’s Most Challenging Public Health Problems. 2005 http://archives.drugabuse.gov/about/welcome/aboutdrugabuse/magnitude/
- O’Connell Mary Ellen, Boat Thomas, Warner Kenneth E., editors. National Research Council. Preventing Mental, Emotional, and Behavioral Disorders Among Young People: Progress and Possibilities. National Academies Press; Washington, DC: 2010. [PubMed] [Google Scholar]
- Nutt DJ, Robbins TW, Stimson GV, Ince M, Jackson A. Drugs and the Future: Brain Science, Addiction and Society. Academic Press; 2006. [Google Scholar]
- Nutt D, King LA, Saulsbury W, Blakemore C. Development of a rational scale to assess the harm of drugs of potential misuse. Lancet. 2007;369:1047–53. doi: 10.1016/S0140-6736(07)60464-4. [DOI] [PubMed] [Google Scholar]
- Odum AL, Madden GJ, Bickel WK. Discounting of delayed health gains and losses by current, never-and ex-smokers of cigarettes. Nicotine Tob Res. 2002;4:295–303. doi: 10.1080/14622200210141257. Ntr.oxfordjournals.org. http://ntr.oxfordjournals.org/content/4/3/295.short. [DOI] [PubMed] [Google Scholar]
- Petry NM, Kirby KN, Kranzler HR. Effects of gender and family history of alcohol dependence on a behavioral task of impulsivity in healthy subjects. J Stud Alcohol. 2002;63:83–90. [PubMed] [Google Scholar]
- Petry NM. Delay discounting of money and alcohol in actively using alcoholics, Currently abstinent alcoholics, and controls. Psychopharmacology. 2001;154:243–50. doi: 10.1007/s002130000638. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Leraas K, Collins C, Melanko S. Delay discounting by the children of smokers and nonsmokers. Drug Alcohol Depend. 2009;99:350–53. doi: 10.1016/j.drugalcdep.2008.07.015. [DOI] [PubMed] [Google Scholar]
- Rounds JS, Beck JG, Grant DM. Is the delay discounting paradigm useful in understanding social anxiety? Behav Res Ther. 2007;45:729–35. doi: 10.1016/j.brat.2006.06.007. [DOI] [PubMed] [Google Scholar]
- Sanchez-Roige S, Stephens DN, Theodora D. Heightened impulsivity: Associated with family history of alcohol misuse, and a consequence of alcohol intake. Alcohol Clin Exp Res. 2016;40:2208–17. doi: 10.1111/acer.13184. [DOI] [PubMed] [Google Scholar]
- Scheres A, Tontsch C, Thoeny AL, Kaczkurkin A. Temporal reward discounting in attention-deficit/hyperactivity disorder: The contribution of symptom domains, reward magnitude, and session length. Biol Psychiatry. 2010;67:641–48. doi: 10.1016/j.biopsych.2009.10.033. [DOI] [PubMed] [Google Scholar]
- Sheffer C, MacKillop J, McGeary J, Landes R, Carter L, Yi R, Jones B, Christensen D, Stitzer M, Jackson L, Bickel W. Delay discounting, locus of control, and cognitive impulsiveness independently predict tobacco dependence treatment outcomes in a highly dependent, lower socioeconomic group of smokers. Am J Addict. 2012;21:221–32. doi: 10.1111/j.1521-0391.2012.00224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheffer CE, Christensen DR, Landes R, Carter LP, Jackson L, Bickel WK. Delay discounting rates: A strong prognostic indicator of smoking relapse. Addict Behav. 2014;39:1682–89. doi: 10.1016/j.addbeh.2014.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher KJ, Grekin ER, Williams NA. The development of alcohol use disorders. Ann Rev Clin Psychol. 2005;1:493–523. doi: 10.1146/annurev.clinpsy.1.102803.144107. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Descutner C. Reports of paternal alcoholism: Reliability across siblings. Addict Behav. 1986;11:25–30. doi: 10.1016/0306-4603(86)90005-5. [DOI] [PubMed] [Google Scholar]
- Smith CT, Steel EA, Parrish MH, Kelm MK, Boettiger CA. Intertemporal choice behavior in emerging adults and adults: effects of age interact with alcohol use and family history status. Front Hum Neurosci. 2015;9:627. doi: 10.3389/fnhum.2015.00627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solis JM, Shadur JM, Burns AR, Hussong AM. Understanding the diverse needs of children whose parents abuse substances. Curr Drug Abuse Rev. 2012;5:135–47. doi: 10.2174/1874473711205020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanger C, Higgins ST, Bickel WK, Elk R, Grabowski J, Schmitz J, Amass L, Kirby KC, Seracini AM. Behavioral and emotional problems among children of cocaine- and opiate-dependent parents. J Am Acad Child Adolesc Psychiatry. 1999;38:421–28. doi: 10.1097/00004583-199904000-00015. [DOI] [PubMed] [Google Scholar]
- Steinhausen HC, Göbel D, Nestler V. Psychopathology in the offspring of alcoholic parents. J Am Acad Child Psychiatry. 1984;23:465–71. doi: 10.1016/s0002-7138(09)60326-5. [DOI] [PubMed] [Google Scholar]
- Sundquist J, Sundquist K, Ji J. Autism and attention-deficit/hyperactivity disorder among individuals with a family history of alcohol use disorders. eLife. 2014;3:e02917. doi: 10.7554/eLife.02917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderBroek L, Acker J, Palmer AA, de Wit H, MacKillop J. Interrelationships among parental family history of substance misuse, delay discounting, and personal substance use. Psychopharmacol. 2016;233:39–48. doi: 10.1007/s00213-015-4074-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washio Y, Higgins ST, Heil SH, McKerchar TL, Badger GJ, Skelly JM, Dantona RL. Delay discounting is associated with treatment response among cocaine-dependent outpatients. Exp Clin Psychopharmacol. 2011;19:243–48. doi: 10.1037/a0023617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilens TE. The child and adolescent offspring of drug- and alcohol-dependent parents. Curr Opin Psychiatry. 1994;7:319–23. [Google Scholar]
- Wilhelm CJ, Mitchell SH. Strain differences in delay discounting using inbred rats. Genes Brain Behav. 2009;8:426–34. doi: 10.1111/j.1601-183X.2009.00484.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson VB, Mitchell SH, Musser ED, Schmitt CF, Nigg JT. Delay discounting of reward in ADHD: Application in young children. J Child Psychol Psychiatry Allied Discipl. 2010;52:256–64. doi: 10.1111/j.1469-7610.2010.02347.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon G, Westermeyer J, Kuskowski MA, Nesheim L. Impact of the number of parents with alcohol use disorder on alcohol use disorder in offspring: A population-based study. J Clin Psychiatry. 2013;74:795–801. doi: 10.4088/JCP.13m08350. [DOI] [PubMed] [Google Scholar]
- Yoon JH, Higgins ST, Heil SH, Sugarbaker RJ, ThomaS CS, Badger GJ. Delay discounting predicts postpartum relapse to cigarette smoking among pregnant women. Exp Clin Psychopharmacol. 2007;15:176–86. doi: 10.1037/1064-1297.15.2.186. [DOI] [PubMed] [Google Scholar]