Abstract
Background
There are limited data about the extent of DSM-5 substance use disorders (SUDs) among primary care patients.
Method
This study analyzed data from a multisite validation study of a substance use screening instrument conducted in a diverse sample of 2,000 adults aged ≥18 years recruited from five primary care practices in four states. Prevalence and correlates of 12-month DSM-5 SUDs were examined.
Results
Overall, 75.5% of the sample used any substance, including alcohol (62.0%), tobacco (44.1%), or illicit drugs/nonmedical medications (27.9%) in the past 12 months (marijuana 20.8%, cocaine 7.3%, opioids 4.8%, sedatives 4.1%, heroin 3.9%). The prevalence of any 12-month SUD was 36.0% (mild disorder 14.2%, moderate/severe disorder 21.8%): tobacco 25.3% (mild 11.5%, moderate/severe 13.8%); alcohol 13.9% (mild 6.9%, moderate/severe 7.0%); and any illicit/nonmedical drug 14.0% (mild 4.0%, moderate/severe 10.0%). Among past 12-month users, a high proportion of tobacco or drug users met criteria for a disorder: tobacco use disorder 57.4% (26.1% mild, 31.3% moderate/severe) and any drug use disorder 50.2% (14.3% mild, 35.8% moderate/severe); a lower proportion of alcohol users (22.4%) met criteria for alcohol use disorder (11.1% mild, 11.3% moderate/severe). Over 80% of adults with opioid/heroin use disorder met criteria for a moderate/severe disorder. Younger ages, male sex, and low education were associated with increased odds of having SUD.
Conclusion
These findings reveal the high prevalence of SUDs in primary care and underscore the need to identify and address them.
Keywords: Marijuana Use Disorder, Opioid Use Disorder, Primary Care, Substance Use Disorder
1. Introduction
In the era of primary care transformation aimed at improving population health, promoting the integration of substance use screening, substance use disorder (SUD) assessment, and treatment in primary care is a critical topic of research (Shapiro et al., 2013; Substance Abuse and Mental Health Services Administration [SAMHSA], 2016). Substance misuse/SUD is a core risk factor for morbidity and mortality (Johnson et al., 2014; Smith et al., 2015). National survey data estimated that, in 2015, only 11.1% of adults aged ≥18 years that needed SUD treatment received SUD treatment at a specialty facility in the past year (Park-Lee et al., 2016). This substantial treatment gap for SUD requires data about prevalence and correlates of SUDs from primary care to guide integration of SUD services, such as targeted screening and intervention, into primary care (Ducharme et al., 2016).
Integration of SUD services within primary care provides an opportunity to increase identification of SUD and provide treatment to reduce SUD-related healthcare use and morbidity (Shapiro et al., 2013; Tai et al., 2014). However, SUDs are typically under-detected, and treatment is infrequently offered in primary care (CASA, 2000; Tai et al., 2012). Data suggest that primary care providers tend to have inadequate information or training to identify or treat SUDs (CASA, 2000; Hwang et al., 2016). There is a need for increasing SUD research in primary care to inform integration of SUD services (Compton et al., 2015; Crowley and Kirschner, 2015). Prior data from primary care patients frequently focus on substance use only (Manwell et al., 1998; Pilowsky and Wu, 2012). Supported by SAMHSA, a screening, brief intervention, and referral to treatment (SBIRT) program was implemented at multiple settings in 2003 (inpatient, outpatient, emergency department, trauma center) (Madras et al., 2009). This SBIRT program employed various tools (e.g., AUDIT, DAST, CAGE) to screen for substance use. Across 6 sites (N=459,599), 22.7% screened positive for alcohol or drug use, but data on SUD prevalence were not systematically collected (Madras et al., 2009).
While national surveys show mixed findings, some data suggest an increase in problem marijuana use or disorder (Hasin et al., 2015; Grucza et al., 2016; Wu et al., 2016a). Additionally, the U.S. is experiencing an opioid overdose epidemic (Rudd et al., 2016). SUD data from the newer DSM-5 are needed to inform research and integrated SUD care in primary care (APA, 2013). Supported by National Drug Abuse Treatment Clinical Trials Network, the Tobacco, Alcohol, Prescription Medication, and Other Substance Use Tool (TAPS Tool) study enrolled 2,000 adults to develop a combined screen and brief assessment tool in detecting problem substance use (Wu et al., 2016b). The sample of the TAPS Tool study, drawn from 5 primary care practices, provides an opportunity for examining SUDs in primary care. We examine prevalence and correlates of 12-month SUDs. Among individuals who reported 12-month substance use, we determine conditional prevalence and correlates of SUDs. The latter determines the probability of SUDs and intervention needs among recent users.
2. Methods
2.1. Study Sample
The TAPS Tool study recruited 2,000 adults from five primary care practices to develop a tool to screen patients for substance use and assess problem use (McNeely et al., 2016). Eligible patients were adults aged ≥18 years who were able to provide consent, comprehend spoken English, and self-administer the Tool on an iPad. Participants were recruited from four sites (Federally Qualified Health Center [FQHC] in Baltimore, Maryland; university-based practice in New York City, New York; university-based practice in Richmond, Virginia; two non-FQHC and non-academic primary care practices in Kannapolis, North Carolina). Sites were selected to include academic and non-academic practices that served a sufficient number of patients across urban and suburban areas.
Participants were enrolled between August, 2014 and April, 2015. Participants were paid $20 for completing survey assessments. All sites conducted recruitment procedures consistently (Wu et al., 2016b). Research assistants consecutively approached each patient in the waiting area for eligibility and obtained verbal consent. Of 14,171 individuals approached, 12% declined screening, and 88% were assessed for eligibility; 52% of them were excluded due to ineligibility (not a clinic patient [n=2,884]; language [n=2,142]; previously enrolled [n=1,042], age<18 [n=278], or other reason [n=172]). A total of 2,057 adults (35% of eligible adults) were enrolled in the study; 2,000 participants completed the study.
2.2. Study Variables
The analysis was based on 12-month substance use (illicit/nonmedical use) and SUDs (tobacco, alcohol, marijuana/hashish, cocaine/crack, methamphetamines, heroin, Rx opioids, stimulants, sedatives, hallucinogens, inhalants, other drugs) from the modified Composite International Diagnostic Interview, Second Edition, Substance Abuse Module (CIDI) (Compton et al., 1996; Cottler, 2000). These SUD data were collected by face-to-face interview with a research assistant, in a private room. The CIDI has been widely used in research to assess SUDs based on DSM-IV (APA, 2000). In the modified CIDI, existing CIDI items were mapped onto 12-month DSM-5 SUDs by omitting the item on legal problems and including the CIDI item on craving to examine DSM-5 SUDs (McNeely et al., 2016). Based on DSM-5 (APA, 2013), SUD was defined as meeting ≥2 DSM criteria for a given substance; mild SUD was defined as meeting 2–3 criteria; and moderate/severe SUD was defined as meeting ≥4 criteria. Self-reported age, sex, race/ethnicity, education, marital status, and employment status were examined as correlates of SUDs; age groups were chosen to be consistent with national survey’s grouping (Wu et al., 2016a). Other demographic data were not collected.
2.3. Data analysis
We analyzed demographic distribution of the sample. Prevalence of SUDs in the sample and among 12-month substance users was calculated. Demographic differences in SUD were estimated by conducting separate logistic regression analyses (SUD vs. no), controlling for site effects. Due to the low SUD prevalence for some drugs, analyses were focused on tobacco, alcohol, marijuana, and a composite ‘any drug’ category. Analyses were conducted with Stata (StataCorp, 2013).
3. Results
3.1. Sociodemographics (Site-Level Data: Supplementary Table 11)
The mean age of the sample was 46.0 years (SD=14.7 years). Women (56.2%) outnumbered men (43.7%). Over one-half of participants were African-American (55.6%). About 12% were Hispanic. Over one-third were employed. Nearly one-half had never been married. Forty-eight percent had not attended college.
3.2. 12-Month Substance Use (Site-Level Data: Supplementary Table 21)
Overall, 75.5% of participants reported 12-month substance use, including alcohol (62.0%), tobacco (44.1%), and illicit/nonmedical drugs (27.9%). Of the drugs, marijuana use had the highest prevalence (20.8%), followed by cocaine (7.3%), Rx opioids (4.8%), sedatives (4.1%), and heroin (3.9%). The prevalence of nonmedical Rx medication use was 7.4%. The prevalence of opioid/heroin use was 7.3%.
3.3. 12-Month SUD (Supplementary Table 32)
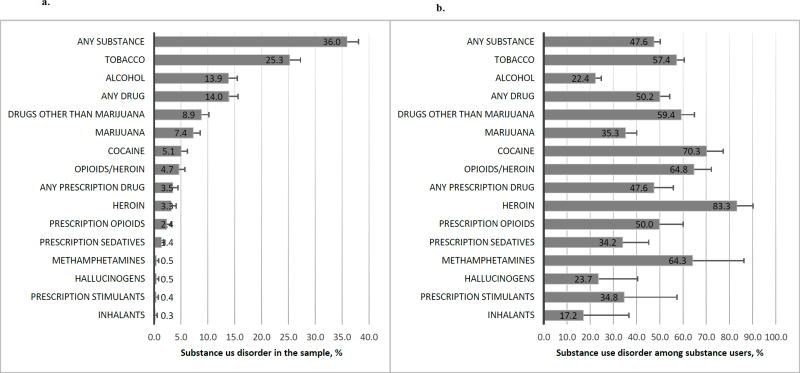
Overall, 36.0% met criteria for any 12-month SUD (14.2% mild disorder, 21.8% moderate/severe disorder): tobacco 25.3%, alcohol 13.9%, and any drug 14.0% (Figure 1a). The prevalence of drug use disorder (DUD) was 7.4% for marijuana, 5.1% for cocaine, 3.3% for heroin, 2.4% for Rx opioids, 1.4% for sedatives, and 3.5% for any Rx medication. Among 12-month substance users, 47.6% met criteria for any 12-month SUD (18.8% mild, 28.8% moderate/severe): tobacco 57.4%, alcohol 22.4%, and any drug 50.2% (Figure 1b).
Figure 1.
a. Prevalence of past 12-month substance use disorders in the total sample: Error bars represent the upper bound of 95% confidence intervals. Detailed results can be found in Supplementary Table 33.
b. Conditional prevalence of past 12-month substance use disorders among past 12-month substance users: Error bars represent the upper bound of 95% confidence intervals. Detailed results can be found in Supplementary Table 33.
3.4. Correlates of 12-Month SUD (Table 1)
Table 1.
Adjusted logistic regressions of correlates of past 12-month substance use disorders in the total sample and among past 12-month substance users
| In the total Sample | Among past 12-month substance users | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 12–month use disorder | Tobacco | Alcohol | Any Drug | Marijuana | Tobacco | Alcohol | Any Drug | Marijuana |
|
| ||||||||
| Adjusted odds ratio* | AOR 95% CI | AOR 95% CI | AOR 95% CI | AOR 95% CI | AOR 95% CI | AOR 95% CI | AOR 95% CI | AOR 95% CI |
|
| ||||||||
| Age in years (vs. 18–25) | ||||||||
| 26–34 | 1.22 0.78–1.90 | 1.26 0.74–2.13 | 1.25 0.75–2.07 | 0.93 0.54–1.60 | 1.30 0.76–2.23 | 1.31 0.76–2.25 | 1.63 0.85–3.10 | 1.72 0.86–3.45 |
| 35–49 | 1.22 0.80–1.86 | 0.68 0.40–1.16 | 0.54 0.32–0.90 | 0.26 0.14–0.48 | 1.48 0.88–2.48 | 0.91 0.52–1.58 | 0.86 0.45–1.66 | 0.50 0.23–1.08 |
| 50–64 | 0.99 0.64–1.54 | 0.69 0.40–1.18 | 0.33 0.19–0.57 | 0.11 0.05–0.21 | 1.34 0.78–2.33 | 1.05 0.59–1.87 | 0.67 0.32–1.37 | 0.19 0.08–0.47 |
| 65+ | 0.38 0.19–0.76 | 0.28 0.11–0.68 | 0.19 0.07–0.50 | 0.03 0.01–0.15 | 0.97 0.39–2.37 | 0.57 0.22–1.50 | 0.74 0.18–3.01 | 0.05 0.01–0.42 |
|
| ||||||||
| Sex (vs. male) | ||||||||
| Female | 0.59 0.47–0.74 | 0.43 0.32–0.57 | 0.44 0.33–0.59 | 0.50 0.35–0.74 | 0.99 0.73–1.33 | 0.50 0.37–0.68 | 0.80 0.54–1.20 | 0.95 0.58–1.56 |
|
| ||||||||
| Race (vs. white) | ||||||||
| African-American/Black | 0.71 0.56–0.92 | 0.77 0.56–1.05 | 0.96 0.69–1.34 | 1.25 0.80–1.93 | 0.83 0.60–1.15 | 0.83 0.59–1.16 | 1.16 0.76–1.77 | 1.33 0.79–2.24 |
| Other | 0.47 0.30–0.72 | 0.65 0.39–1.08 | 0.70 0.42–1.17 | 0.59 0.30–1.18 | 0.62 0.35–1.09 | 0.71 0.41–1.22 | 0.95 0.48–1.88 | 0.64 0.28–1.45 |
|
| ||||||||
| Ethnicity (vs. non-Hispanic) | ||||||||
| Hispanic | 0.83 0.56–1.23 | 1.04 0.66–1.66 | 1.32 0.84–2.07 | 1.42 0.80–2.54 | 0.95 0.56–1.63 | 1.04 0.63–1.72 | 1.17 0.63–2.18 | 1.43 0.70–2.95 |
|
| ||||||||
| Employment (vs. unemployed) | ||||||||
| Employed | 0.66 0.49–0.90 | 0.75 0.52–1.08 | 0.47 0.32–0.68 | 0.63 0.38–1.03 | 0.92 0.62–1.35 | 0.69 0.47–1.02 | 0.51 0.30–0.85 | 0.75 0.41–1.40 |
| Retired | 1.22 0.70–2.13 | 1.01 0.50–2.03 | 0.28 0.10–0.80 | 1.34 0.39–4.58 | 1.35 0.65–2.79 | 0.93 0.44–1.98 | 0.16 0.04–0.62 | 2.45 0.44–13.82 |
| Disabled | 1.36 1.00–1.85 | 0.80 0.55–1.18 | 1.07 0.74–1.55 | 1.26 0.74–2.13 | 1.81 1.21–2.73 | 0.93 0.61–1.41 | 0.91 0.53–1.56 | 1.84 0.88–3.82 |
| Other | 0.94 0.63–1.42 | 0.73 0.43–1.23 | 0.84 0.51–1.37 | 1.01 0.56–1.85 | 1.25 0.74–2.13 | 0.82 0.47–1.43 | 0.85 0.44–1.64 | 1.37 0.63–2.96 |
|
| ||||||||
| Marital status (vs. married/living with partner) | ||||||||
| Separated/divorced/widowed | 1.24 0.91–1.69 | 1.12 0.73–1.71 | 1.13 0.73–1.75 | 1.05 0.56–1.95 | 0.86 0.56–1.31 | 1.02 0.65–1.60 | 1.27 0.71–2.27 | 0.88 0.41–1.87 |
| Never married | 1.30 0.98–1.74 | 1.49 1.02–2.16 | 1.33 0.91–1.95 | 1.34 0.80–2.23 | 0.85 0.58–1.25 | 1.40 0.94–2.08 | 1.27 0.77–2.10 | 1.29 0.69–2.39 |
|
| ||||||||
| Education (vs. less than high school) | ||||||||
| High school/GED | 0.82 0.61–1.11 | 0.72 0.49–1.04 | 0.95 0.66–1.36 | 0.84 0.52–1.37 | 1.03 0.70–1.50 | 0.59 0.39–0.89 | 1.01 0.60–1.69 | 1.18 0.63–2.21 |
| Some college/associate degree | 0.83 0.61–1.12 | 0.74 0.50–1.07 | 0.68 0.46–1.00 | 0.56 0.33–0.94 | 1.20 0.81–1.77 | 0.56 0.37–0.84 | 0.64 0.38–1.08 | 0.60 0.32–1.15 |
| Bachelor/graduate degree | 0.34 0.23–0.51 | 0.51 0.32–0.82 | 0.30 0.18–0.51 | 0.45 0.24–0.87 | 0.73 0.44–1.21 | 0.41 0.24–0.68 | 0.35 0.17–0.69 | 0.64 0.28–1.46 |
Each adjusted binary logistic regression model included variables listed in the first column and controlled for study location (state). Less than 1% of the total sample and past 12-month substance users was not included due to missing data.
AOR: adjusted odds ratio. CI: confidence interval. Boldface: p<0.05.
3.4.1 Correlates of SUD in the Sample
Ages 65+ (vs. ages 18–25), female sex, and bachelor/graduate degree (vs. <high school) were associated with lower odds of SUD (tobacco, alcohol, marijuana, any drug). Ages 35–49 and ages 50–64 (vs. ages 18–25) were associated with lower odds of DUD (drug, marijuana). African-American and other race (vs. white race) and employment (vs. unemployment) were associated with decreased odds of tobacco use disorder. Being never-married (vs. being married/cohabiting) was associated with increased odds of alcohol use disorder (AUD). Employment and retirement (vs. unemployment) was associated with lower odds of DUD.
3.4.2 Correlates of SUD Among 12-Month Users
Among tobacco users, being disabled (vs. being unemployed) was associated with increased odds of tobacco use disorder. Among alcohol users, female sex and more education (vs. <high school) were associated with lower odds of AUD. Among drug users, being employed or retired (vs. being unemployed) and bachelor/graduate degree (vs. < high school) were associated with lower odds of DUD. Among marijuana users, ages 50–64 and ages 65+ (vs. aged 18–25) were associated with lower odds of marijuana use disorder.
4. Discussion
Given the national movement toward the integration of primary care and SUD treatment, these findings have implications for clinical practice. 12-month SUDs were prevalent (any SUD: 36.0%) among primary care patients in this sample. Overall, 50% of illicit/nonmedical drug users met criteria for any DUD; over 80% of those with cocaine or opioid/heroin use disorder had a moderate/severe disorder. The findings of prevalent SUDs highlight a need to improve primary care providers’ training and willingness to provide screening and treatment for SUDs (CASA, 2000; Mannelli and Wu, 2016).
The 12-month prevalence of DSM-IV AUD and any DUD among adults in the 2015 National Survey of Drug Use and Health (NSDUH) was 6.2% and 2.8%, respectively (CBHSQ, 2016). The 12-month prevalence of DSM-5 AUD and any DUD among adults in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC)-III was 13.9% and 3.9%, respectively (Grant et al., 2015, 2016). In this sample, the 12-month prevalence of DSM-5 AUD and any DUD was 13.9% and 14.0%, respectively. Although NSDUH used DSM-IV criteria (abuse/dependence), and we used DSM-5 criteria (≥2 criteria), the difference appears to be related to comparatively high prevalence of drug use among primary care patients in this sample. Methodological differences (setting, interview mode, contextual effect) complicate the comparison of our results with those from other survey or clinical trial samples (Grucza et al., 2016). The latter often includes active substance users only (e.g., Bernstein et al., 2015). The sample for this study included primary care patients regardless of substance use to allow analysis of prevalence and correlates of SUDs. The SAMHSA-supported SBIRT program found that 22.7% screened positive for alcohol or drug use (Madras et al., 2009). In this sample, 27.9% reported drug use and 62.0% endorsed alcohol use in the past year. Thus, prevalence of problem substance use may be elevated in healthcare settings (Pilowsky and Wu, 2012).
By distinguishing between mild and moderate/severe use disorders, we found that 71% of adults with any DUD were moderate/severe cases. The analysis of conditional prevalence revealed that 65% of opioid/heroin users met criteria for opioid/heroin use disorder. These findings suggest the presence of potentially high-level but overlooked SUD treatment needs. Given the opioid overdose epidemic and availability of medication-assisted treatment for opioid use disorder, it is critical to develop the infrastructure, including training for primary care physicians, to treat opioid use disorder (Stein et al., 2016).
Limitations of this study include: a cross-sectional design, self-report data (recall/reporting bias), and inability to assess differences in sociodemographic correlates among specific DUDs. Our sample is not representative of primary care patient populations. It was limited to clinics of primary care in the Eastern U.S. Eligible respondents include those that were able to comprehend spoken English and self-administer the assessment on an iPad. Further, substance users may be frequent utilizers of medical care; as such they may be disproportionately captured in this study. Nonetheless, recruitment was conducted consistently in all sites that specified procedures for screening every patient in the waiting room for eligibility to mitigate selection bias. This study also has notable strengths. It included a large sample to produce new data for DSM-5 SUDs among primary care patients. Prior multisite studies were based on data collected 10+ years ago (Madras et al., 2009). The sample includes patients recruited from multiple regions. Results tend to reflect up-to-date SUD estimates in this setting. Patients’ substance use varied by location (Madras et al., 2009); it is important to study SUDs in diverse samples from multiple regions.
In conclusion, SUD is prevalent among primary care patients in this sample. To improve integration of SUD assessment and treatment into primary care, research is needed to inform primary care physicians’ willingness to use validated tools for screening substance misuse, identify effective approaches for addressing SUDs in medical settings, and engage patients into SUD treatment (Kim et al., 2016; Loheswaran et al., 2015; Saitz et al., 2014).
Supplementary Material
Highlights.
There are limited data of DSM-5 substance use disorders (SUDs) in primary care.
Past-year illicit or nonmedical drug use was common (28%) in primary care patients.
Over 1 in 3 (36%) adult primary care patients had a DSM-5 SUD.
About 5% of primary care patients had opioid/heroin use disorder in the past year.
The majority of adults with SUD had a moderate/severe use disorder.
Acknowledgments
All study procedures of the TAPS Tool Study were approved by local Institutional Review Boards (ClinicalTrials.gov Identifier: NCT02110693). The secondary data analysis of this manuscript was approved by the Duke University Health System Institutional Review Board for Clinical Investigations (Pro00071131). The authors thank all research participants, participating practices, and all research staff and investigators for their efforts and support for the TAPS Tool study (Leah Bouk, Kimberly Roseman, Carla Kingsbury, Melissa Johnston, Amina Chaudhry, Jack Chally, Courtney Nordeck, Kevin O’Grady, Anjalee Sharma, Laurie Cathers, Dace Svikis, Kate Polak, David Pomm, Patsy Novo, Linnea Russell, Luke Sleiter, Saima Mili, Phoebe Gauthier, Jacquie King, Aimee Wahle, Colleen Allen, Anne Hassell, Eve Jelstrom, Robert Lindblad, Lauren Yesko, Patrice Yohannes, Alex Borbely).
Role of the funding source
This work was made possible by research support from the National Institutes of Health (UG1DA040317, U10DA013727, UG1DA013034, UG1DA013035, R01MD007658, and R01DA019623). The sponsoring agencies have no further role in the study design and analysis, the writing of the report, or the decision to submit the paper for publication. The opinions expressed in this paper are solely those of the authors and do not represent the official position of the U.S. government. G. Subramaniam has had no programmatic responsibilities for R01MD007658 and R01DA019623.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Author Disclosures
Contributors
LT Wu led the study design and statistical analysis for this manuscript, conducted literature review, and drafted the manuscripts. H Zhu conducted data analyses under the supervision and guidance of LT Wu. RP Schwartz, LT Wu, and J McNeely were Principal Investigators of the data source (The TAPS Tool). G Subramaniam was a scientific protocol coordinator and collaborator under the cooperative agreement. G Sharma and P VanVeldhuisen were statistical investigators of the TAPS Tool. KT Brady was Principal Investigator of Southern Consortium Node. All authors contributed to revisions and interpretations of the findings that resulted in the final manuscript. All authors approved of the final manuscript.
Conflicts of Interest
The authors have no conflict of interest to disclose.
References
- American Psychiatric Association (APA) Diagnostic and Statistical Manual. 4. Washington, DC: American Psychiatric Press; 2000. text revision. [Google Scholar]
- American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders. Fifth. American Psychiatric Association; Arlington, VA: 2013. [Google Scholar]
- Bernstein J, Cheng DM, Wang N, Trilla C, Samet J, Saitz R. Recreational drug use among primary care patients: Implications of a positive self-report. Ann. Fam. Med. 2015;13:257–260. doi: 10.1370/afm.1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CASA Columbia. Missed opportunity: National survey of primary care physicians and patients on substance abuse. The National Center on Substance Abuse at Columbia University; New York: 2000. [accessed 10.12.16]. http://www.casacolumbia.org/addiction-research/reports/national-survey-primary-care-physicians-patients-substance-abuse. [Google Scholar]
- Center for Behavioral Health Statistics and Quality (CBHSQ) 2015 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2016. [accessed 10.12.16]. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf. [Google Scholar]
- Compton WM, Cottler LB, Dorsey KB, Spitznagel EL, Magera DE. Comparing assessments of DSM-IV substance dependence disorders using CIDI-SAM and SCAN. Drug Alcohol Depend. 1996;41:179–187. doi: 10.1016/0376-8716(96)01249-5. [DOI] [PubMed] [Google Scholar]
- Compton WM, Blanco C, Wargo EM. Integrating addiction services into general medicine. JAMA. 2015;314:2401–2402. doi: 10.1001/jama.2015.12741. [DOI] [PubMed] [Google Scholar]
- Cottler LB. Department of Psychiatry. Washington University School of Medicine; St Louis, MO: 2000. Composite International Diagnostic Interview - Substance Abuse Module (SAM) [Google Scholar]
- Crowley RA, Kirschner N Health and Public Policy Committee of the American College of Physicians. The integration of care for mental health, substance abuse, and other behavioral health conditions into primary care: Executive summary of an American College of Physicians position paper. Ann. Intern. Med. 2015;163:298–299. doi: 10.7326/M15-0510. [DOI] [PubMed] [Google Scholar]
- Ducharme LJ, Chandler RK, Harris AHS. Implementing effective substance abuse treatments in general medical settings: Mapping the research terrain. J. Subst. Abuse Treat. 2016;60:110–118. doi: 10.1016/j.jsat.2015.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, Hasin DS. Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry. 2015;72:757–766. doi: 10.1001/jamapsychiatry.2015.0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, Zhang H, Smith SM, Pickering RP, Huang B, Hasin DS. Epidemiology of DSM-5 drug use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions–III. JAMA Psychiatry. 2016;73:39–47. doi: 10.1001/jamapsychiatry.2015.2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grucza RA, Agrawal A, Krauss MJ, Cavazos-Rehg PA, Bierut LJ. Recent trends in the prevalence of marijuana use and associated disorders in the United States. JAMA Psychiatry. 2016;73:300–301. doi: 10.1001/jamapsychiatry.2015.3111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, Jung J, Pickering RP, Ruan WJ, Smith SM, Huang B, Grant BF. Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA Psychiatry. 2015;72:1235–1242. doi: 10.1001/jamapsychiatry.2015.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang CS, Turner LW, Kruszewski SP, Kolodny A, Alexander GC. Primary care physicians’ knowledge and attitudes regarding prescription opioid abuse and diversion. Clin. J. Pain. 2016;32:279–284. doi: 10.1097/AJP.0000000000000268. [DOI] [PubMed] [Google Scholar]
- Johnson NB, Hayes LD, Brown K, Hoo EC, Ethier KA Centers for Disease Control and Prevention (CDC) CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors—United States, 2005-2013. MMWR Suppl. 2014;63:3–27. [PubMed] [Google Scholar]
- Kim TW, Bernstein J, Cheng DM, Lloyd-Travaglini C, Samet JH, Palfai TP, Saitz R. Receipt of addiction treatment as a consequence of a brief intervention for drug use in primary care: A randomized trial. Addiction. 2016 doi: 10.1111/add.13701. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loheswaran G, Soklaridis S, Selby P, Le Foll B. Screening and treatment for alcohol, tobacco and opioid use disorders: a survey of family physicians across Ontario. PloS One. 2015:10. doi: 10.1371/journal.pone.0124402. http://doi.org/10.1371/journal.pone.0124402. [DOI] [PMC free article] [PubMed]
- Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, Clark HW. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: Comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99:280–295. doi: 10.1016/j.drugalcdep.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannelli P, Wu LT. Primary care for opioid use disorder. Subst. Abuse Rehabil. 2016;2016:107–109. doi: 10.2147/SAR.S69715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manwell LB, Fleming MF, Johnson K, Barry KL. Tobacco, alcohol, and drug use in a primary care sample: 90-day prevalence and associated factors. J. Addict. Dis. 1998;17:67–81. doi: 10.1300/J069v17n01_07. [DOI] [PubMed] [Google Scholar]
- McNeely J, Wu LT, Subramaniam G, Sharma G, Cathers LA, Svikis D, Sleiter L, Russell L, Nordeck C, Sharma A, O'grady KE, Bouk LB, Cushing C, Wahle A, Schwartz RP. Performance of the Tobacco, Alcohol, Prescription Medication, and Other Substance Use (TAPS) tool for substance use screening in primary care patients. Ann. Intern. Med. 2016;165:690–699. doi: 10.7326/M16-0317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park-Lee E, Lipari RN, Hedden SL, Copello EAP, Kroutil LA. Receipt of services for substance use and mental health issues among adults: Results from the 2015 National Survey on Drug Use and Health. 2016 [PubMed] [Google Scholar]
- Pilowsky DJ, Wu LT. Screening for alcohol and drug use disorders among adults in primary care: A review. Subst. Abuse Rehabil. 2012;3:25–34. doi: 10.2147/SAR.S30057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths - United States, 2000–2014. MMWR. 2016;64:1378–1382. doi: 10.15585/mmwr.mm6450a3. [DOI] [PubMed] [Google Scholar]
- Saitz R, Palfai TP, Cheng DM, Alford DP, Bernstein JA, Lloyd-Travaglini CA, Meli SM, Chaisson CE, Samet JH. Screening and brief intervention for drug use in primary care: The ASPIRE randomized clinical trial. JAMA. 2014;312:502–513. doi: 10.1001/jama.2014.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro B, Coffa D, McCance-Katz EF. A primary care approach to substance misuse. Am. Fam. Physician. 2013;88:113–121. [PubMed] [Google Scholar]
- Smith MW, Stocks C, Santora PB. Hospital readmission rates and emergency department visits for mental health and substance abuse conditions. Community Ment. Health J. 2015;51:190–197. doi: 10.1007/s10597-014-9784-x. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 13. StataCorp LP; College Station, TX: 2013. [Google Scholar]
- Stein BD, Sorbero M, Dick AW, Pacula RL, Burns RM, Gordon AJ. Physician capacity to treat opioid use disorder with buprenorphine-assisted treatment. JAMA. 2016;316:1211–1212. doi: 10.1001/jama.2016.10542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) [accessed 15.01.16];Primary care in behavioral health. 2016 http://www.integration.samhsa.gov/integrated-care-models/primary-care-in-behavioral-health.
- Tai B, Wu LT, Clark HW. Electronic health records: Essential tools in integrating substance abuse treatment with primary care. Subst. Abuse Rehabil. 2012;3:1–8. doi: 10.2147/SAR.S22575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tai B, Sparenborg S, Ghitza UE, Liu D. Expanding the National Drug Abuse Treatment Clinical Trials Network to address the management of substance use disorders in general medical settings. Subst. Abuse Rehabil. 2014;5:75–80. doi: 10.2147/SAR.S66538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, Zhu H, Swartz MS. Trends in cannabis use disorders among racial/ethnic population groups in the United States. Drug Alcohol Depend. 2016a;165:181–190. doi: 10.1016/j.drugalcdep.2016.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu LT, McNeely J, Subramaniam GA, Sharma G, VanVeldhuisen P, Schwartz RP. Design of the NIDA clinical trials network validation study of tobacco, alcohol, prescription medications, and substance use/misuse (TAPS) tool. Contemp. Clin. Trials. 2016b;50:90–97. doi: 10.1016/j.cct.2016.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.