Abstract
Background
Bone-patellar tendon-bone (bone-tendon-bone) and four-strand hamstring tendon grafts (hamstring) are the most commonly utilized autografts for primary anterior cruciate ligament (ACL) reconstruction. Existing clinical trials, registry studies, and meta-analyses offer conflicting opinions regarding the most favorable graft choice.
Questions/purposes
Which graft type for ACL reconstruction (bone-tendon-bone or hamstring) has a higher risk of (1) graft rupture and/or (2) graft laxity?
Methods
We performed a meta-analysis of randomized controlled trials (RCTs), prospective cohort studies, and high-quality national registry studies to compare the outcomes of primary ACL reconstruction with bone-tendon-bone autograft or hamstring autograft. Studies that compared these graft types were identified through a comprehensive search of electronic databases (PubMed, MEDLINE, EMBASE, and the Cochrane Library). Two independent reviewers utilized the Jadad scale for RCT study quality and the Modified Coleman Methodology Score for prospective comparative and registry study quality. The included studies were analyzed for the primary outcome measure of graft rupture with or without revision ACL surgery. In surviving grafts, secondary outcomes of graft laxity were quantified by KT1000/2000™ testing, a positive pivot shift test, and a positive Lachman test. Meta-analysis was performed with Review Manager. A total of 47,613 ACL reconstructions (39,768 bone-tendon-bone and 7845 hamstring) from 14 RCTs, 10 prospective comparative studies, and one high-quality national registry study were included in this meta-analysis. Mean age was 28 years in both groups. Sixty-three percent of patients in the bone-tendon-bone cohort were men versus 57% of patients in the hamstring cohort. Mean followup was 68 ± 55 months.
Results
Two hundred twelve of 7560 (2.80%) bone-tendon-bone grafts ruptured compared with 1123 of 39,510 (2.84%) in the hamstring group (odds ratio = 0.83, 95% confidence interval, 0.72-0.96; p = 0.01). The number needed to treat analysis found that 235 patients would need to be treated with a bone-tendon-bone graft over a hamstring tendon graft to prevent one graft rupture. Instrumented laxity analysis showed that 22% (318 of 1433) of patients in the bone-tendon-bone group had laxity compared with 18% (869 of 4783) in the hamstring tendon group (odds ratio = 0.86; p = 0.16). Pivot shift analysis showed a positive pivot shift in 19% (291 of 1508) of the bone-tendon-bone group compared with 17% (844 of 5062) in the hamstring group (odds ratio = 0.89; p = 0.51). Lachman testing showed a positive Lachman in 25% (71 of 280) of patients receiving bone-tendon-bone grafts compared with 25% (73 of 288) in the hamstring group (odds ratio = 0.96; p = 0.84).
Conclusions
In this meta-analysis of short- to mid-term followup after primary ACL reconstruction, hamstring autografts failed at a higher rate than bone-tendon-bone autografts. However, failure rates were low in each group, the difference observed was small, and we observed few differences between graft types in terms of laxity. Both graft types remain viable options for primary ACL reconstruction, and the difference in failure rate should be one part of a larger conversation with each individual patient about graft selection that should also include potential differences in donor site morbidity, complication rates, and patient-reported outcome measures. Continued prospective collection of patient data will be important going forward as we attempt to further characterize the potential differences in outcomes attributable to graft selection.
Level of Evidence
Level III, therapeutic study.
Electronic supplementary material
The online version of this article (doi:10.1007/s11999-017-5278-9) contains supplementary material, which is available to authorized users.
Keywords: Anterior Cruciate Ligament, Anterior Cruciate Ligament Reconstruction, Pivot Shift, Pivot Shift Testing, Hamstring Graft
Introduction
Anterior cruciate ligament (ACL) rupture is a devastating injury that can lead to recurrent instability, chronic pain, and degenerative changes in the knee [5–8, 42]. Arthroscopic reconstruction is the standard approach, but controversy remains over the most favorable graft selection. The most commonly utilized autografts for ACL reconstruction in the United States are the bone-patellar tendon-bone (bone-tendon-bone) and the four-strand hamstring tendon (hamstring) [13, 43]. Some authors suggest that bone-tendon-bone autograft is the most favorable graft choice because of faster graft incorporation [33], a higher proportion of patients returning to preinjury activity levels [47], and potentially a lower risk of graft rupture [32]. However, others favor hamstring autografts because of lower donor site morbidity, anterior knee pain, extensor strength deficit, and osteoarthritis [11, 27, 32, 39, 42].
Although controversy remains on specific advantages and disadvantages, clearly the most significant adverse outcome after ACL reconstruction is graft rupture and subsequent revision surgery. There have been a number of prospective studies that compared bone-tendon-bone and hamstring that demonstrated similar risk of rupture between the two graft types [2, 4, 21, 30, 38, 40, 41, 46]. A 2014 meta-analysis by Xie et al. [47] effectively summarized the literature before 2013 with roughly 1000 patients in each group and found no difference in the risk of graft rupture.
In subsequent years, there have been multiple prospective studies published on this topic [3, 13, 34, 35]. The most notable has been data on greater than 40,000 patients from Scandinavian ACL registries, in which researchers identified a higher risk of rupture/revision for patients receiving hamstring than those receiving bone-tendon-bone [15]. This finding directly contradicts what was reported by Xie et al. in their 2014 meta-analysis [47] and thus raises new questions about failure rate after ACL reconstruction. It remains unclear whether there is an inherent difference in graft type that prior studies have been underpowered to detect or whether the difference found by Gifstad et al. [13] is a uniquely Scandinavian phenomenon that is not generalizable to the orthopaedic community at large.
The goal of this study was to perform an up-to-date meta-analysis, incorporating high-quality evidence from randomized controlled trials (RCTs), prospective comparative studies, and national registries in an attempt to address the aforementioned questions. Specifically, we asked which approach to ACL reconstruction (bone-tendon-bone or hamstring) has a higher risk of (1) graft rupture and/or (2) graft laxity?
Materials and Methods
This study considered for inclusion RCTs, prospective comparative studies, and large national registries with prospective data collection comparing bone-tendon-bone autograft and hamstring autograft in primary ACL reconstruction (Table 1).
Table 1.
Summary of included studies
| Study | Year of publication | Study design | Number of patients | BPTB male | BPTB female | 4SHT male | 4SHT female | BPTB age (years) | 4SHT age (years) | Followup (months) | Lost to followup | Mean MCMS | Median Jadad |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Marder et al. [30] | 1991 | PCS | 80 | 24 | 13 | 26 | 9 | 22 | 24 | 29 | 8 | 73 | |
| Aglietti et al. [1] | 1994 | PCS | 60 | N/A | N/A | N/A | N/A | N/A | N/A | 28 | 3 | 73 | |
| Shaieb et al. [38] | 2002 | RCT | 82 | 26 | 7 | 21 | 16 | 32 | 30 | 33 | 12 | 78 | 3 |
| Aglietti et al. [2] | 2004 | RCT | 120 | 46 | 14 | 46 | 14 | 25 | 25 | 24 | 0 | 78 | 3 |
| Ibrahim et al. [22] | 2005 | PCS | 110 | 40 | 0 | 45 | 0 | 22 | 22 | 81 | 25 | 76 | |
| Laxdal et al. [25] | 2005 | RCT | 79 | 29 | 11 | 28 | 11 | 28 | 26 | 26 | 0 | 84 | 3 |
| Wagner et al. [44] | 2005 | PCS | 110 | 40 | 15 | 40 | 15 | 34 | 31 | 24 | 0 | 82 | |
| Harilainen et al. [16] | 2006 | RCT | 99 | N/A | N/A | N/A | N/A | N/A | N/A | 60 | 16 | 78 | 3 |
| Zaffagnini et al. [48] | 2006 | RCT | 50 | 16 | 9 | 15 | 10 | 31 | 31 | 60 | 0 | 78 | 3 |
| Svensson et al. [40] | 2006 | PCS | 61 | 0 | 28 | 0 | 31 | 28 | 25 | 26 | 2 | 79 | |
| Maletis et al. [28] | 2007 | RCT | 99 | 31 | 15 | 44 | 7 | 27 | 28 | 24 | 2 | 78 | 3 |
| Taylor et al. [41] | 2009 | RCT | 64 | N/A | N/A | N/A | N/A | 22 | 22 | 34 | 11 | 77 | 3 |
| Barenius et al. [4] | 2010 | RCT | 164 | 40 | 38 | 51 | 24 | 33 | 35 | 100 | 11 | 80 | 4 |
| Holm et al. [21] | 2010 | RCT | 72 | 18 | 10 | 15 | 14 | 25 | 27 | 120 | 15 | 85 | 3 |
| Sadoghi et al. [36] | 2011 | PCS | 92 | N/A | N/A | N/A | N/A | 30 | 29 | 24 | 0 | 83 | |
| Wipfler et al. [46] | 2011 | RCT | 62 | 18 | 11 | 15 | 10 | 40 | 34 | 105 | 8 | 77 | 3 |
| Sajovic et al. [37] | 2011 | RCT | 64 | N/A | N/A | N/A | N/A | 27 | 25 | 132 | 2 | 84 | 3.5 |
| Gifstad et al. [14] | 2013 | RCT | 114 | N/A | N/A | N/A | N/A | 27 | 27 | 84 | 12 | 76 | 3 |
| Rahr-Wagner et al. [35] | 2014 | PCS | 70 | ||||||||||
| Gifstad et al. [13] | 2014 | PCS | 45,402 | 4239 | 2497 | 22,132 | 16,534 | N/A | N/A | 36 | 0 | 68 | |
| Leitgeb et al. [26] | 2014 | PCS | 96 | 45 | 11 | 23 | 17 | 28 | 29 | 0 | 82 | ||
| Mohtadi et al. [31] | 2015 | RCT | 220 | N/A | N/A | N/A | N/A | 29 | 29 | 39 | 14 | 79 | 5 |
| Heijne et al. [19] | 2015 | PCS | 68 | 22 | 12 | 14 | 20 | 29 | 30 | 62 | 0 | 81 | |
| Webster et al. [45] | 2016 | RCT | 65 | 16 | 6 | 20 | 5 | 27 | 26 | 180 | 18 | 84 | 5 |
| Thompson et al. [42] | 2016 | PCS | 180 | N/A | N/A | N/A | N/A | 25 | 24 | 240 | 28 | 87 | |
| Totals | 47,613 | 4650 | 2697 | 22,535 | 16,737 | 28 | 28 | 68 | 79 | 3 |
BPTB = bone-patellar tendon-bone; 4SHT = four-strand hamstring tendon; MCMS = Modified Coleman Methodology Score; PCS = prospective cohort study; RCT = randomized controlled trial; N/A = not available.
Inclusion criteria were minimum 2-year followup, documentation of graft failure rate (graft rupture or revision ACL reconstruction), and/or documentation of measures of graft laxity in the form of instrumented laxity (KT1000/2000™; MEDmetric Corp, San Diego, CA, USA), pivot shift test, or Lachman test among surviving grafts. Exclusion criteria for studies included case reports, single-center retrospective comparative studies, narrative reviews, or image reviews. Studies were not excluded based on patient demographics or surgical technique. When articles that reported on the same patient group were identified, the most recent data were utilized.
Search Strategy
Search engines utilized were PubMed, Cochrane Library, MEDLINE, and EMBASE. All articles that were not in English were excluded. Further studies were found utilizing the reference lists of the studies initially identified. Search terms included “ACL” or “anterior cruciate ligament” in combination with “hamstring autograft” or “semitendinosus” and “bone tendon bone autograft” or “patellar tendon”.
After duplicates were removed, 136 abstracts were screened. The titles and abstracts of all records retrieved by the search were assessed independently by two authors (BTS, NRJ). Any disagreements were resolved by discussion and arbitration by the three senior authors (KEW, TEH, AJK). After initial screening of these abstracts, two authors (BTS, NRJ) assessed the remaining full-text articles for inclusion in the study (Fig. 1).
Fig. 1.
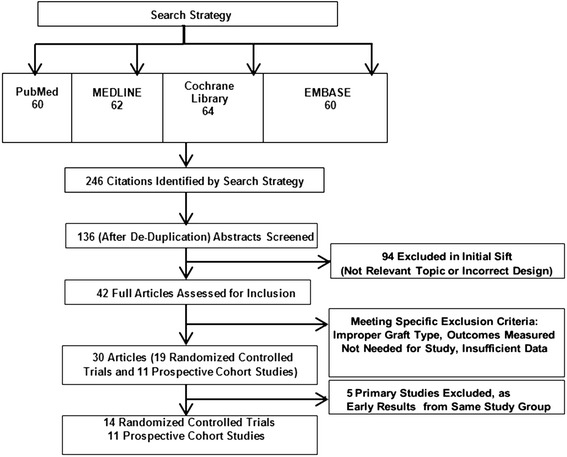
PRISMA diagram shows how the final studies included were obtained. Overall, there were 14 RCTs, 10 prospective cohort studies, and one national registry study.
Studies meeting inclusion criteria were assessed for quality by one of two methods. RCTs were assessed using the Jadad scale [23], whereas prospective comparative studies and registries were assessed using the Modified Coleman Methodology Scores (MCMS) (range, 0–90) [9]. Interrater reliability was assessed with the Pearson correlation coefficient. Values of correlation range from + 1 (perfect positive correlation) to -1 (perfect negative correlation) with a value greater than + 0.7 considered a strong positive correlation. This method has been utilized in the past to assess the validity of interrater reliability when using the MCMS in assessing the quality of articles reviewed [18]. The mean MCMS score of the included studies was 79 ± 5 and the median Jadad for the RCTs included was 3 (range, 3–5) (Table 1). Blinded review of the selected articles was conducted to ensure interrater reliability, and a correlation coefficient of 0.79 was found for MCMS scores and 0.89 for Jadad scores. The majority of studies lost points from their MCMS scores as a result of incomplete followup and the study investigators being the surgeons who performed the operations.
Two authors (BTS, NRJ) independently extracted data from each included study. Any discrepancies were resolved by a third author (KEW). Patient demographics were extracted from each study as well as the number of patients in each study group (bone-tendon-bone versus hamstring). Specific outcomes measured were failure rates (defined as graft rupture or revision ACL reconstruction) in addition to instrumented laxity (positive defined as ≥ 3 mm), pivot shift (positive defined as 1+ or greater), and Lachman test (positive defined as 1+ or greater) in surviving grafts.
Outcomes Measured
There were 47,613 patients from 14 RCTs, 10 prospective comparative studies, and one national registry included in the meta-analysis (Table 1). Mean age for patients who underwent ACL reconstruction with bone-tendon-bone was 28 ± 3 years versus 28 ± 4 years for those who received hamstring autografts. Sixty-three percent of patients in the bone-tendon-bone cohort were men versus 57% of patients in the hamstring cohort. Average followup was 68 ± 55 months for the included studies.
Nineteen studies that included a total of 47,070 (7560 bone-tendon-bone, 39,510 hamstring) patients reported on graft rupture and/or revision ACL reconstruction. Seven studies, including 568 patients (280 bone-tendon-bone, 288 hamstring), reported Lachman test data. Fifteen studies reported data on instrumented laxity as defined by patients with a side-to-side difference of ≥ 3 mm at manual maximum testing with KT1000/2000™. This included 6216 patients (1433 bone-tendon-bone, 4783 hamstring). Overall, 13 studies reported on pivot shift testing and 6570 patients were included (1508 bone-tendon-bone, 5062 hamstring). Pivot shift was denoted as positive if patients had a grade greater than 1+ on physical examination.
Statistical Analysis
Data analysis was performed with Review Manager (Version 5.3; The Cochrane Collaboration, London, UK). Odds ratio was used as summary statistics for dichotomous variables. Odds ratios (ORs) were reported with 95% confidence intervals, and statistical significance was set to a p value of < 0.05. Statistical heterogeneity between included studies was evaluated by the I2 and chi square tests with significance set at p < 0.10. The number needed to treat (NNT) was calculated utilizing observed relative risks and the patient’s expected event rate [12].
Random-effects or fixed-effects models were used depending on heterogeneity of the study. Random-effects modeling was utilized for I2 values of > 25% [20]. A sensitivity analysis was performed by excluding one study in each round and evaluating the influence of any single study on the primary meta-analysis estimate. Subgroup analysis was also performed based on type of study design (RCT versus prospective cohort studies [PCS]) to identify potential differences between bone-tendon-bone and hamstring grafts across trials.
Publication Bias
A funnel plot was created for each outcome measure to determine if there was bias in the studies. These plots showed no evidence of positive outcome bias in any of the outcomes measured and were relatively symmetric (Appendix 1 [Supplemental materials are available with the online version of CORR ®.]).
Results
The meta-analysis found that patients undergoing primary ACL reconstruction with bone-tendon-bone autograft were less likely to experience graft rupture and/or revision ACL reconstruction than patients treated with hamstring autograft (OR, 0.83; 95% confidence interval [CI], 0.72–0.96; p = 0.01) (Fig. 2). A NNT analysis showed that 235 patients would need to be treated with a bone-tendon-bone graft over a hamstring graft to prevent one graft rupture.
Fig. 2.
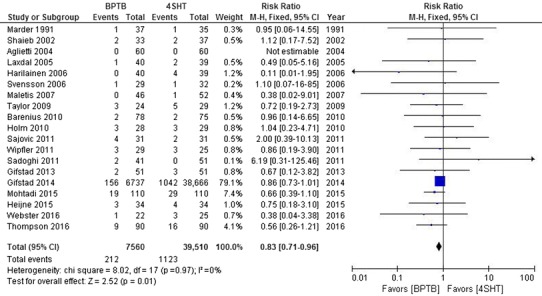
Analysis of failure rate between the studies is demonstrated. OR for graft failure was 0.83 favoring bone-tendon-bone (95% CI, 0.72-0.96; p = 0.01). BPTB = bone-patellar-tendon bone; 4SHT = four-stranded hamstring tendon; M-H = Mantel-Haenszel.
Among patients who did not experience graft rupture or revision, there were no differences observed between the two graft types in any of our secondary analyses of graft laxity. No difference was found based on KT1000/2000™ testing between bone-tendon-bone and hamstring (OR, 0.86; 95% CI, 0.69–1.06; p = 0.16) (Fig. 3), pivot shift testing (OR, 0.89; 95% CI, 0.63–1.25; p = 0.51) (Fig. 4), or Lachman testing (OR, 0.96; 95% CI, 0.67–1.39; p = 0.84) (Fig. 5).
Fig. 3.
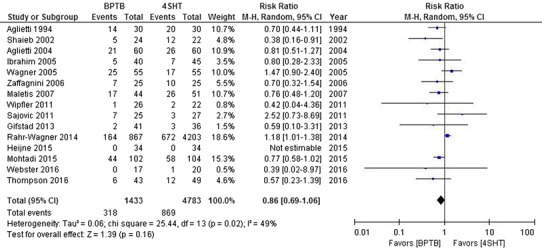
Instrumented laxity was measured by KT1000/2000™. Positive test equals ≥ 3-mm side-to-side difference. No major difference was observed between either group in the study.
Fig. 4.
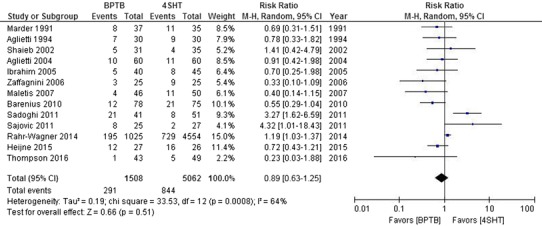
Pivot shift analysis between the studies is shown. No major difference was observed between either group in terms of the study.
Fig. 5.
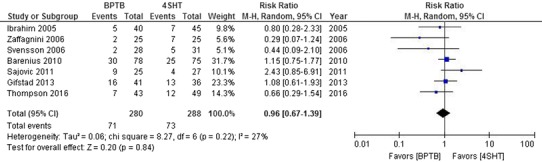
Lachman testing analysis between the studies is shown. No major difference was observed between either group in terms in the study.
A subgroup analysis of the outcomes included in the study was performed according to the type of study design (PCS or RCT). The sole finding of difference was an OR of 0.76 favoring bone-tendon-bone over hamstring when instrumented laxity in RCTs alone was analyzed (95% CI, 0.62-0.92; p = 0.006); there were no differences in terms of Lachman or pivot shift testing (Table 2).
Table 2.
Subgroup analysis
| Outcome measure | Type of study | Number of studies | Number of patients | Test for heterogeneity (p value) | Statistical model | Risk ratio (95% CI) |
p value |
|---|---|---|---|---|---|---|---|
| Failure rate | RCT | 13 | 1194 | 0.91 | Fixed | 0.72 (0.51–1.02) | 0.06 |
| PCS | 6 | 45,876 | 0.72 | Fixed | 0.85 (0.73–1.0) | 0.05 | |
| Instrumented laxity | RCT | 9 | 731 | 0.58 | Fixed | 0.76 (0.62–0.92) | 0.006 |
| PCS | 6 | 5485 | 0.08 | Random | 1.00 (0.73–1.36) | 0.98 | |
| Pivot shift | RCT | 6 | 537 | 0.05 | Random | 0.77 (0.42–1.41) | 0.40 |
| PCS | 7 | 6033 | 0.008 | Random | 0.99 (0.66–1.51) | 0.98 | |
| Lachman testing | RCT | 4 | 332 | 0.14 | Random | 1.12 (0.68–1.84) | 0.67 |
| PCS | 3 | 236 | 0.83 | Fixed | 0.66 (0.36–1.21) | 0.18 |
Value < 1 favors bone-patellar tendon-bone; CI = confidence interval; RCT = randomized controlled trial; PCS = prospective cohort study.
Discussion
Graft rupture is a feared complication after ACL reconstruction, because revision surgery often results in inferior patient-reported outcome measures, increased laxity with pivot shift testing, and increased rates of tibiofemoral arthritis [15]. Although bone-tendon-bone and hamstring autograft are common graft choices, the available evidence is mixed on which graft type is associated with a higher risk of graft rupture and revision ACL reconstruction. A recent large Scandiavian registry study [13] reported a higher risk of graft rupture with hamstring than bone-tendon-bone, but a prior meta-analysis [47] found no difference between graft types. The goals of this study were to utilize the statistical power of a meta-analysis to compare the risk of graft rupture/revision and metrics of graft laxity between graft types. We found a small increased risk of graft rupture/revision in the hamstring group when compared with the bone-tendon-bone group. The NNT was calculated at 235, meaning that 235 patients would need to be treated with bone-tendon-bone rather than hamstring to prevent one rupture. We observed few differences between graft types in terms of graft laxity reported by the primary source studies.
We interpret this study in light of several limitations. First, most of the patients included in this study came from the Scandinavian registry studies and those results factor heavily into the results of the current study. Although the methodology for a registry study is not as rigorous as that of an RCT, the data were collected longitudinally, and the authors have published on the validity of their registry [15]. The inclusion of these data was critical to this study as we attempted to determine whether the results of the registry studies would hold up in the setting of a larger meta-analysis. Second, this study was designed to investigate differences in the risk of graft rupture between the two graft types without considering clinical outcome scores and knee function. This fact keeps the study clear and focused but precludes its use in isolation when a clinician debates the merits of bone-tendon-bone versus hamstring autograft. We believe that the small increased risk of graft rupture observed in this meta-analysis should be only one aspect of a larger discussion with patients regarding optimal graft choice. Another limitation is that the nature of a meta-analysis is such that the authors can only analyze and interpret the data available in light of heterogeneous reporting of data across studies. This fact limits the number of patients available for analysis within the individual outcomes studied but does not alter the validity of the results. Lastly, the relatively short-term minimum followup in some of the included studies prevents us from evaluation of the long-term outcomes between graft types.
In this study, patients who received bone-tendon-bone autograft had a reduced risk of graft failure compared with those receiving hamstring autograft at a minimum 2-year followup with a NNT of 235 patients. These data support the recent findings from the Scandinavian ACL registries [3, 13, 34, 35] and by Maletis et al. in their retrospective registry review [29]. However, the observed difference in this study was small and clinicians must weigh the clinical importance of this finding while also considering differences in donor site morbidity, patient-reported outcome metrics, and knee function scores. All of these areas represent opportunities for continued research.
Secondary outcome measures of graft laxity included KT1000/2000™ instrumented laxity testing, pivot shift test, and the Lachman test. Instrumented laxity testing favored bone-tendon-bone when including RCTs in isolation; however, on examination of the entire cohort, none of these measures was found to be different between groups in the current study. This is in contrast to the meta-analysis by Xie et al. [47] that reported that pivot shift testing favored bone-tendon-bone and the Cochrane review by Mohtadi et al. [32] in which they found all three of these factors favored bone-tendon-bone. The absence of a difference in graft laxity between groups in this study indicates that previously observed differences might have been the result of sampling bias or recent improvements in surgical technique. Newer generation fixation devices for hamstring ACL reconstruction are designed to allow for more anatomic tunnel placement without compromising load to failure [10, 17]. The routine pretensioning of hamstring grafts also may contribute to less graft laxity regardless of graft type [24].
In this meta-analysis of short- to mid-term followup after primary ACL reconstruction, hamstring autografts failed at a higher rate than bone-tendon-bone autografts. However, failure rates were low in each group, the difference observed was small, and the grafts performed similarly in metrics of graft laxity. Both graft types remain viable options for primary ACL reconstruction, and the difference in failure rate should be one part of a larger conversation with each individual patient about graft selection that should also include potential differences in donor site morbidity, complication rates, and patient-reported outcome measures. Continued prospective collection of patient data will be important going forward as we attempt to further characterize the potential differences in outcomes attributable to graft selection.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Footnotes
Funded by the National Institutes of Health (R01 AR056259-06; TEH). One of the authors (KEW) is on the Editorial or Governing Board of the Journal of Sports Science and Medicine and received research support from Smith & Nephew, Inc (Andover, MA, USA). One of the authors (AJK) is on the Editorial or Governing Board of the American Journal of Sports Medicine; is a paid consultant for Arthrex Inc (Naples, FL, USA); received research support from the Arthritis Foundation, Ceterix Orthopaedics (Fremont, CA, USA), and Histogenics Corp (Waltham, MA, USA); and is a Board or Committee Member of the International Cartilage Repair Society, Minnesota Orthopedic Society, and the Musculoskeletal Transplantation Foundation.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Mayo Clinic, Rochester, Rochester, MN, USA; and the School of Allied Health, La Trobe University, Melbourne, Australia.
References
- 1.Aglietti P, Buzzi R, Zaccherotti G, De Biase P. Patellar tendon versus doubled semitendinosus and gracilis tendons for anterior cruciate ligament reconstruction. Am J Sports Med. 1994;22:211–217; discussion 217–218. [DOI] [PubMed]
- 2.Aglietti P, Giron F, Buzzi R, Biddau F, Sasso F. Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Joint Surg Am. 2004;86:2143–2155. doi: 10.2106/00004623-200410000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Andernord D, Bjornsson H, Petzold M, Eriksson BI, Forssblad M, Karlsson J, Samuelsson K. Surgical predictors of early revision surgery after anterior cruciate ligament reconstruction: results from the Swedish National Knee Ligament Register on 13,102 patients. Am J Sports Med. 2014;42:1574–1582. doi: 10.1177/0363546514531396. [DOI] [PubMed] [Google Scholar]
- 4.Barenius B, Nordlander M, Ponzer S, Tidermark J, Eriksson K. Quality of life and clinical outcome after anterior cruciate ligament reconstruction using patellar tendon graft or quadrupled semitendinosus graft: an 8-year follow-up of a randomized controlled trial. Am J Sports Med. 2010;38:1533–1541. doi: 10.1177/0363546510369549. [DOI] [PubMed] [Google Scholar]
- 5.Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE. Treatment of anterior cruciate ligament injuries, part 1. Am J Sports Med. 2005;33:1579–1602. doi: 10.1177/0363546505279913. [DOI] [PubMed] [Google Scholar]
- 6.Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE. Treatment of anterior cruciate ligament injuries, part 2. Am J Sports Med. 2005;33:1751–1767. doi: 10.1177/0363546505279922. [DOI] [PubMed] [Google Scholar]
- 7.Church S, Keating JF. Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br. 2005;87:1639–1642. doi: 10.1302/0301-620X.87B12.16916. [DOI] [PubMed] [Google Scholar]
- 8.Cohen M, Amaro JT, Ejnisman B, Carvalho RT, Nakano KK, Peccin MS, Teixeira R, Laurino CF, Abdalla RJ. Anterior cruciate ligament reconstruction after 10 to 15 years: association between meniscectomy and osteoarthrosis. Arthroscopy. 2007;23:629–634. doi: 10.1016/j.arthro.2007.03.094. [DOI] [PubMed] [Google Scholar]
- 9.Cowan J, Lozano-Calderon S, Ring D. Quality of prospective controlled randomized trials. Analysis of trials of treatment for lateral epicondylitis as an example. J Bone Joint Surg Am. 2007;89:1693–1699. doi: 10.2106/JBJS.F.00858. [DOI] [PubMed] [Google Scholar]
- 10.Flanigan DC, Kanneganti P, Quinn DP, Litsky AS. Comparison of ACL fixation devices using cadaveric grafts. J Knee Surg. 2011;24:175–180. doi: 10.1055/s-0031-1284728. [DOI] [PubMed] [Google Scholar]
- 11.Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR., Jr Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31:2–11. doi: 10.1177/03635465030310011501. [DOI] [PubMed] [Google Scholar]
- 12.Freemantle N, Geddes J. Understanding and interpreting systematic reviews and meta-analyses. Part 2: meta-analyses. Evidence Based. Mental Health. 1998;1:102–104. [Google Scholar]
- 13.Gifstad T, Foss OA, Engebretsen L, Lind M, Forssblad M, Albrektsen G, Drogset JO. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014;42:2319–2328. doi: 10.1177/0363546514548164. [DOI] [PubMed] [Google Scholar]
- 14.Gifstad T, Sole A, Strand T, Uppheim G, Grontvedt T, Drogset JO. Long-term follow-up of patellar tendon grafts or hamstring tendon grafts in endoscopic ACL reconstructions. Knee Surg Sports Traumatol Arthrosc. 2013;21:576–583. doi: 10.1007/s00167-012-1947-0. [DOI] [PubMed] [Google Scholar]
- 15.Grassi A, Ardern CL, Marcheggiani Muccioli GM, Neri MP, Marcacci M, Zaffagnini S. Does revision ACL reconstruction measure up to primary surgery? A meta-analysis comparing patient-reported and clinician-reported outcomes, and radiographic results. Br J Sports Med. 2016;50:716–724. doi: 10.1136/bjsports-2015-094948. [DOI] [PubMed] [Google Scholar]
- 16.Harilainen A, Linko E, Sandelin J. Randomized prospective study of ACL reconstruction with interference screw fixation in patellar tendon autografts versus femoral metal plate suspension and tibial post fixation in hamstring tendon autografts: 5-year clinical and radiological follow-up results. Knee Surg Sports Traumatol Arthrosc. 2006;14:517–528. doi: 10.1007/s00167-006-0059-0. [DOI] [PubMed] [Google Scholar]
- 17.Harilainen A, Sandelin J. A prospective comparison of 3 hamstring ACL fixation devices–Rigidfix, BioScrew, and Intrafix–randomized into 4 groups with 2 years of follow-up. Am J Sports Med. 2009;37:699–706. doi: 10.1177/0363546508328109. [DOI] [PubMed] [Google Scholar]
- 18.Harris JD, Erickson BJ, Cvetanovich GL, Abrams GD, McCormick FM, Gupta AK, Verma NN, Bach BR, Jr, Cole BJ. Development of a valid and reliable knee articular cartilage condition-specific study methodological quality score. Orthop J Sports Med. 2014;2:2325967113512606. doi: 10.1177/2325967113512606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heijne A, Hagstromer M, Werner S. A two- and five-year follow-up of clinical outcome after ACL reconstruction using BPTB or hamstring tendon grafts: a prospective intervention outcome study. Knee Surg Sports Traumatol Arthrosc. 2015;23:799–807. doi: 10.1007/s00167-013-2727-1. [DOI] [PubMed] [Google Scholar]
- 20.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holm I, Oiestad BE, Risberg MA, Aune AK. No difference in knee function or prevalence of osteoarthritis after reconstruction of the anterior cruciate ligament with 4-strand hamstring autograft versus patellar tendon-bone autograft: a randomized study with 10-year follow-up. Am J Sports Med. 2010;38:448–454. doi: 10.1177/0363546509350301. [DOI] [PubMed] [Google Scholar]
- 22.Ibrahim SA, Al-Kussary IM, Al-Misfer AR, Al-Mutairi HQ, Ghafar SA, El Noor TA. Clinical evaluation of arthroscopically assisted anterior cruciate ligament reconstruction: patellar tendon versus gracilis and semitendinosus autograft. Arthroscopy. 2005;21:412–417. doi: 10.1016/j.arthro.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 23.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 24.Jisa KA, Williams BT, Jaglowski JR, Turnbull TL, LaPrade RF, Wijdicks CA. Lack of consensus regarding pretensioning and preconditioning protocols for soft tissue graft reconstruction of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2016;24:2884–2891. doi: 10.1007/s00167-015-3530-y. [DOI] [PubMed] [Google Scholar]
- 25.Laxdal G, Kartus J, Hansson L, Heidvall M, Ejerhed L, Karlsson J. A prospective randomized comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:34–42. doi: 10.1016/j.arthro.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 26.Leitgeb J, Kottstorfer J, Schuster R, Kovar FM, Platzer P, Aldrian S. Primary anterior cruciate ligament reconstruction in athletes: a 5-year follow up comparing patellar tendon versus hamstring tendon autograft. Wien Klin Wochenschr. 2014;126:397–402. doi: 10.1007/s00508-014-0550-4. [DOI] [PubMed] [Google Scholar]
- 27.Li S, Chen Y, Lin Z, Cui W, Zhao J, Su W. A systematic review of randomized controlled clinical trials comparing hamstring autografts versus bone-patellar tendon-bone autografts for the reconstruction of the anterior cruciate ligament. Arch Orthop Trauma Surg. 2012;132:1287–1297. doi: 10.1007/s00402-012-1532-5. [DOI] [PubMed] [Google Scholar]
- 28.Maletis GB, Cameron SL, Tengan JJ, Burchette RJ. A prospective randomized study of anterior cruciate ligament reconstruction: a comparison of patellar tendon and quadruple-strand semitendinosus/gracilis tendons fixed with bioabsorbable interference screws. Am J Sports Med. 2007;35:384–394. doi: 10.1177/0363546506294361. [DOI] [PubMed] [Google Scholar]
- 29.Maletis GB, Inacio MC, Desmond JL, Funahashi TT. Reconstruction of the anterior cruciate ligament: association of graft choice with increased risk of early revision. Bone Joint J. 2013;95:623–628. doi: 10.1302/0301-620X.95B5.30872. [DOI] [PubMed] [Google Scholar]
- 30.Marder RA, Raskind JR, Carroll M. Prospective evaluation of arthroscopically assisted anterior cruciate ligament reconstruction. Patellar tendon versus semitendinosus and gracilis tendons. Am J Sports Med. 1991;19:478–484. doi: 10.1177/036354659101900510. [DOI] [PubMed] [Google Scholar]
- 31.Mohtadi N, Chan D, Barber R, Oddone Paolucci E. A randomized clinical trial comparing patellar tendon, hamstring tendon, and double-bundle ACL reconstructions: patient-reported and clinical outcomes at a minimal 2-year follow-up. Clin J Sport Med. 2015;25:321–331. doi: 10.1097/JSM.0000000000000165. [DOI] [PubMed] [Google Scholar]
- 32.Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011;9:CD005960. [DOI] [PMC free article] [PubMed]
- 33.Papageorgiou CD, Ma CB, Abramowitch SD, Clineff TD, Woo SL. A multidisciplinary study of the healing of an intraarticular anterior cruciate ligament graft in a goat model. Am J Sports Med. 2001;29:620–626. doi: 10.1177/03635465010290051501. [DOI] [PubMed] [Google Scholar]
- 34.Persson A, Fjeldsgaard K, Gjertsen JE, Kjellsen AB, Engebretsen L, Hole RM, Fevang JM. Increased risk of revision with hamstring tendon grafts compared with patellar tendon grafts after anterior cruciate ligament reconstruction: a study of 12,643 patients from the Norwegian Cruciate Ligament Registry, 2004-2012. Am J Sports Med. 2014;42:285–291. doi: 10.1177/0363546513511419. [DOI] [PubMed] [Google Scholar]
- 35.Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M. Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the Danish Registry of Knee Ligament Reconstruction. Am J Sports Med. 2014;42:278–284. doi: 10.1177/0363546513509220. [DOI] [PubMed] [Google Scholar]
- 36.Sadoghi P, Muller PE, Jansson V, van Griensven M, Kropfl A, Fischmeister MF. Reconstruction of the anterior cruciate ligament: a clinical comparison of bone-patellar tendon-bone single bundle versus semitendinosus and gracilis double bundle technique. Int Orthop. 2011;35:127–133. doi: 10.1007/s00264-010-1037-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sajovic M, Strahovnik A, Dernovsek MZ, Skaza K. Quality of life and clinical outcome comparison of semitendinosus and gracilis tendon versus patellar tendon autografts for anterior cruciate ligament reconstruction: an 11-year follow-up of a randomized controlled trial. Am J Sports Med. 2011;39:2161–2169. doi: 10.1177/0363546511411702. [DOI] [PubMed] [Google Scholar]
- 38.Shaieb MD, Kan DM, Chang SK, Marumoto JM, Richardson AB. A prospective randomized comparison of patellar tendon versus semitendinosus and gracilis tendon autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30:214–220. doi: 10.1177/03635465020300021201. [DOI] [PubMed] [Google Scholar]
- 39.Sugimoto D, Myer GD, McKeon JM, Hewett TE. Evaluation of the effectiveness of neuromuscular training to reduce anterior cruciate ligament injury in female athletes: a critical review of relative risk reduction and numbers-needed-to-treat analyses. Br J Sports Med. 2012;46:979–988. doi: 10.1136/bjsports-2011-090895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Svensson M, Sernert N, Ejerhed L, Karlsson J, Kartus JT. A prospective comparison of bone-patellar tendon-bone and hamstring grafts for anterior cruciate ligament reconstruction in female patients. Knee Surg Sports Traumatol Arthrosc. 2006;14:278–286. doi: 10.1007/s00167-005-0708-8. [DOI] [PubMed] [Google Scholar]
- 41.Taylor DC, DeBerardino TM, Nelson BJ, Duffey M, Tenuta J, Stoneman PD, Sturdivant RX, Mountcastle S. Patellar tendon versus hamstring tendon autografts for anterior cruciate ligament reconstruction: a randomized controlled trial using similar femoral and tibial fixation methods. Am J Sports Med. 2009;37:1946–1957. doi: 10.1177/0363546509339577. [DOI] [PubMed] [Google Scholar]
- 42.Thompson SM, Salmon LJ, Waller A, Linklater J, Roe JP, Pinczewski LA. Twenty-year outcome of a longitudinal prospective evaluation of isolated endoscopic anterior cruciate ligament reconstruction with patellar tendon or hamstring autograft. Am J Sports Med. 2016;44:2579–2588. doi: 10.1177/0363546516655333. [DOI] [PubMed] [Google Scholar]
- 43.Tibor L, Chan PH, Funahashi TT, Wyatt R, Maletis GB, Inacio MC. Surgical technique trends in primary ACL reconstruction from 2007 to 2014. J Bone Joint Surg Am. 2016;98:1079–1089. doi: 10.2106/JBJS.15.00881. [DOI] [PubMed] [Google Scholar]
- 44.Wagner M, Kaab MJ, Schallock J, Haas NP, Weiler A. Hamstring tendon versus patellar tendon anterior cruciate ligament reconstruction using biodegradable interference fit fixation: a prospective matched-group analysis. Am J Sports Med. 2005;33:1327–1336. doi: 10.1177/0363546504273488. [DOI] [PubMed] [Google Scholar]
- 45.Webster KE, Feller JA, Hartnett N, Leigh WB, Richmond AK. Comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction: a 15-year follow-up of a randomized controlled trial. Am J Sports Med. 2016;44:83–90. doi: 10.1177/0363546515611886. [DOI] [PubMed] [Google Scholar]
- 46.Wipfler B, Donner S, Zechmann CM, Springer J, Siebold R, Paessler HH. Anterior cruciate ligament reconstruction using patellar tendon versus hamstring tendon: a prospective comparative study with 9-year follow-up. Arthroscopy. 2011;27:653–665. doi: 10.1016/j.arthro.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 47.Xie X, Liu X, Chen Z, Yu Y, Peng S, Li Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015;22:100–110. doi: 10.1016/j.knee.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 48.Zaffagnini S, Marcacci M, Lo Presti M, Giordano G, Iacono F, Neri MP. Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surg Sports Traumatol Arthrosc. 2006;14:1060–1069. doi: 10.1007/s00167-006-0130-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


